Acute Liver Failure - PBworks
advertisement
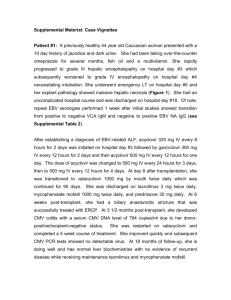
Acute Liver Failure 30 year old woman presents to hospital with a two day history of nausea, vomiting, and right upper quadrant pain. She has been healthy and denies any medication use. She recently traveled to Vietnam where she twisted her ankle while bungee jumping. The pain has been well controlled with over the counter and natural remedies. On examination, she is slightly confused to date and in moderate distress from the pain. Vital signs are: 123/41, heart rate 109, respiratory rate 24, and saturations 95% on room air. She is has diffuse abdominal tenderness and palpable liver edge with a scleral icterus. What is the most likely cause of this patient’s presentation? What are the common etiologies of acute liver failure? – Consider: A – acetaminophen, hepatitis A, autoimmune B – hepatitis B C – cryptogenic, hepatitis C D – hepatitis D E – esoteric causes such as Wilson’s and Budd-Chiari F – fatty infiltration such as fatty liver of pregnancy and Reye Initial bloodwork comes back: – ALT 3826, AST 4826, TBili 59, Alk Phos 283,INR 4.2, creatinine 436, pH 7.31 What in the history gives us clues to the cause? – Travel: hepatitis virus? – Over the counter drugs: acetaminophen? – Natural remedies: drug or toxin? – Childbearing age: fatty liver of pregnancy? Obtaining further history, her family tells you that she has been vaccinated against hepatitis B because she is a lab tech, she is not pregnant but do not know what medications and remedies she takes. You take the history from the family because the patient is rapidly becoming unresponsive. What is the definition of fulminant hepatic failure? – Severe acute liver injury with impaired synthetic function and encephalopathy in a person with a normal liver or well-compensated liver disease. What are the grades of encephalopathy? The patient has become completely unresponsive with posturing to stimulation. You rapidly intubate and resuscitate her and obtain an urgent CT scan. Head CT What has happened? How do you grade hepatic encephalopathy? Grade Mental Status Asterixis EEG I Euphoria/depression Mild confusion Slurred speech Disordered sleep Yes/No Usually normal II Lethargy Moderate confusion Yes Abnormal III Marked confusion Incoherent Sleeping but arousable Yes Abnormal IV Coma No Abnormal How do you treat hepatic encephalopathy with and without intracranial hypertension? What is the role for intracranial monitoring in this case? After appropriate resuscitation and treatment, the patient is more stable. The family approaches you for more information. They want to know whether she is going to need liver transplant. What do you tell them and how do you know? Acetaminophen-induced disease Arterial pH <7.3 (irrespective of the grade of encephalopathy) OR Grade III or IV encephalopathy AND Prothrombin time >100 seconds AND Serum creatinine >3.4mg/dL (301 µmol/L) All other causes of fulminant hepatic failure Prothrombin time >100 seconds (irrespective of the grade of encephalopathy) OR Any three of the following variables (irrespective of the grade of encephalopathy) 1. Age <10 years or >40 years 2. Etiology: non-A, non-B hepatitis, halothane hepatitis, idiosyncratic drug reactions 3. Duration of jaundice before onset of encephalopathy >7 days 4. Prothrombin time >50 seconds 5. Serum bilirubin >18 mg/dL (308 µmol/L) •By the way, what are some of the drugs that can cause fulminant hepatic failure? Acetaminophen Alcohol Amiodarone Carbon tetrachloride Dideoxyinosine Gold Halothane Isoniazid Ketoconazole MAO inhibitors Methyldopa NSAIDs Phenytoin Poison mushrooms (Amanita phalloides) Propylthiouracil Rifampin Sulfonamides Tetracycline Tricyclic antidepressants Valproic acid Next patient 68 year old man with known chronic liver dysfunction from NASH. He presents to his family doctor with increasing confusion. He admits the patient to hospital and consults you because of persisting fevers. On assessment, he is febrile, slightly jaundiced with signs of chronic liver disease and abdominal tenderness. Blood cultures come back positive for E. coli What is the most likely problem? How is the diagnosis of spontaneous bacterial peritonitis made? A paracentesis reveals a WBC count of 375 cells/mL with 95% PMNs. What is the appropriate treatment of spontaneous bacterial peritonitis? The next day, the patient feels better but his urine output has been poor. His creatinine is 242, last level 6 months ago was 109. What are the possible causes of this problem? – Consider: Volume depletion from paracentesis Abdominal compartment syndrome ATN from nephrotoxins such as aminoglycosides Interstitial nephritis from B-lactams Hepatorenal syndrome How would you investigate this? There is no change in renal function after fluid challenges and his urine sodium is < 10 mmol/L. What is the criteria for hepatorenal syndrome? What is the pathophysiology behind hepatorenal syndrome? The diagnosis of HRS is confirmed. The family asks you what this means. He has refused transplant workup and long term dialysis. What do you tell the family? What is the role of albumin in HRS? What is the role of vasopressors such as midodrine/octreotide or levophed/vasopressin in HRS? Questions??