Itchy Rash

welcome
Patient itch/
Itchy Rash
Prof. DOULAT RAI BAJAJ
FCPS, MCPS
Professor & Chairman
Dept. of Dermatology
LUMHS
Goals of Presentation
At the end of presentation you would be able to:
1.
Clinically evaluate a patient with itch or itchy rash
2.
Make a working diagnosis
3.
Manage it at the best
How to Evaluate?
History
Examination
Lab investigations
History:
Age of patient
I nfant/child :
Atopic Dermatitis
Scabies, Pediculosis
Infantile seb. dermatitis psoriasis
Mastocytosis
Insect bites (papular urticaria)
Urticaria
Age of patient: Young adult
Specific dermatoses: Atopic Dermatitis, Contact
Dermatitis, Psoriasis, P. Rosea, lichen simplex chronicus, Prurigo,
Infections: Scabies, body lice, Yeast & fungal infections (tineas, P. versicolor)….
Hypersensitivity reactions: urticaria, Dermatitis herpetiformis
Miscellaneous: cut. Lymphoma, psychogenic……
History:
Old age:
Dermatitis Herpetiformis
Xerosis psoriasis
Aging of skin
Drug reactions,
Systemic diseases
History:
Acute vs Chronic
Acute: scabies, pediculosis, drugs, insect bites, urticaria
Chronic : AD, ACD, Psoriasis, LSC, prurigo, systemic diseases
Gender : pregnancy associated dermatoses
Family history: Scabies, pediculosis, psoriasis,
AD,
History:
Presence of Systemic Disease:
Renal: CRF, Pt on dialysis
Endocrine: DM, hypo-and hyperthyroidism,
Liver Disease
Malignancies: any internal malignancy
AIDS:
Hematological: Polycythmia, anaemia
Psychogenic
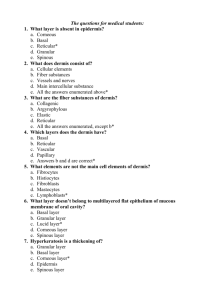
Examination:
Type of lesion: macule/patch, papule/plaque, nodule, vesicle/bullae, pustule, erosion/ulcer ..
Sites and Distribution:
Shape: annular, discoid, polygonal, arcuate…
Pattern: discrete, grouped, linear, segmental, dermatomal
Colour, consistency, margins etc
Secondary features: crust, scale, excoriation ,
Investigations:
Woods’ light examination
Scrappings for fungal infections
Skin Biopsy:
Atopic Dermatitis
ATOPIC DERMATITIS
“ATOPY” is a genetically determined tendency to produce increased amounts of reagens (IgE), in response to allergens.
Clinically manifested by :
ASTHMA
HAY FEVER
ATOPIC DERMATITIS
IgG
IgM
IgA
IgD
IgE
Macropha ge
IL-1
T cell IL-4
Antigen
IMMUNITY
Plasma cell
B cell
Antigen
ALLERGY
Macrophage
IL-1
T cell IL-4
IgE
Plasma cell
B cell
Major features (must have 4)
Pruritus
Early age of onset
Typical morphology and distribution
Infants & Children: Face & extensors
Adults: Flexureal lichenification & linearity
Chronic course
Personal or family history of atopy (asthma, rhinoconjuctivitis, dermatitis).
Minor features
Dryness of skin
Ichthyosis , palmar hyperlinearity/keratosis pilaris
Hand/foot dermatitis
Lip dermatitis
Nipple eczema
Increased cutaneous infections e.g. Staph. aureus &
H.Simplex)
Common Clinical Features:
Itching
Erythematous Macules, Papules, vesicles
Eczema with crusting, Lichenification,
Excoriation
Dry skin
Secondary infection
ACUTE vs Chronic AD
Acute AD
Redness
Swelling
Papules
Vesicles
Exudation
Cracking
Chronic AD
Less vesiculation/ exudation
More Thickening, pigmentation &
Lichenification (due to rubbing & scratching)
Fissures
Scratch marks
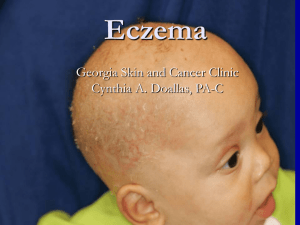
Infantile/childhood AD
Red Itchy scaly lesions on scalp, cheeks, wrists & trunk
Diaper area spared
Extensor aspects of limbs
(begins to Crawl)
Irritable & restlessness
Crusts
Pustules
Adult AD
Lichenified, pigmented papules, plaques scattered all over body
Bothering itch
Prominent infra-orbital crease
General dry skin
Sebhorroic Dermatitis
Seb. Derm
Characterized by:
Erythematous scaly plaques
Greasy scaling
yellow crusted patches & plaques
There is very minimal itch (vs AD)
Age of onset:
Below 06 months: infantile SD
After puberty: adult SD
Sites:
Infantile SD:
Scalp (Cradle Cap),
Face & Neck (eye brows, Ears & sides of neck).
Trunk & Flexures, starting in napkin area.
Adult SD :
Scalp
Forehead
Face: Eyebrows, Nasolabial folds, ear canals, behind pinnae,
Trunk: sternal area, interscapular region & flexures
Contact Dermatitis
1.
2.
Irritant Contact Dermatitis
Allergic Contact Dermatitis
Irritant Contact Dermatitis
Non-allergic reaction of the skin caused by exposure to irritating substance
Any person can develop ICD if concentration & duration of contact sufficient
About 80% of occupational dermatitis is irritant in nature
C/F: Erythema, Edema, Vesiculation, Weeping
ALLERGIC CONTACT DERMATITIS
Immunologically-mediated, Delayed (type IV) hypersensitivity
Occurs in persons already sensitized
Not dose related, Not restricted to area of contact
C/F: erythema, edema, papules, papulovesicles
it is difficult to distinguish C/F of ACD from irritant or constitutional dermatoses(AD, SD)
Common sensitizer:
1.
2.
3.
4.
5.
Hair dyes
Nickel, Chromate, cobalt
Leather, Rubber
Topical Drugs: neomycin, gentamicin, lignocaine
Plants
Pathogenesis ACD
Dry scaly dermatitis
ACD due to items in pocket
LEATHER
ADHESIVE TAPE
PLANTS
Tatoos causing ACD
TREATMENT
Treatment Principles
Avoid known triggers
Moisturize, moisturize, moisturize
Itch Control
Topical corticosteroids
Other topical therapies
Systemic therapy
Avoid Irritants
Allergen avoidance during pregnancy and or infancy (mild benefit shown from avoiding cow’s milk, eggs, and dust mites)
Big Five: dryness, dust mites, animal dander, cigarette smoke, wool
Others include water and chemicals
Dry Skin Care
Baths and showers not hot and short
Mild soap (Dove) – best to avoid alkali soaps
Blot dry and immediately moisturize (skin should still be slightly damp)
Creams and ointments better than lotions and oils
Itch Control
Avoid topical antihistamines
Products containing menthol, camphor & weak conc: of phenol may be helpful
Cool compresses
Avoid hot/sweaty conditions
Antihistamines
In children generally sedating AH used. No role of non-sedating AH in children with AD
A combination of sedating & non-sedating AH indicated in adults with eczema.
For AD : Zonalon=topical doxepin – qid for maximum of eight days. Never occlude, some systemic absorption, very sedating, risk of ACD
TOPICAL STEROIDS
Steroid
1.
2.
3.
4.
5.
6.
7.
8.
Potency
Vehicle
Amount
Site
Clinical stage of eczema
Weather
Duration of treatment
Disease
Super Potent Potent
Clobetasol propionate 0.05%
(dermovate)
Fluticasone propionate
(cutivate)
Amcinonide
Diflucortolone valerate (volog) Mometasone Furoate
(hivate)
Flucinolone acetonide 0.2% Betamethasone dipropionate (diprolene)
Halcinonide
Betamethasone valerate
0.1% (betnovate )
Triamcinolone acetonide
(kenacomb)
Moderate
Potent
Betamethason valerate
0.025%
Mild
Hydrocortisone
Prednicarbate
Methyl prednisolone acetate 0.25%
Flucinolone acetonide
0.0025%
Desonide (desone)
Methylprednisolone aceponate 0.1% (advantan )
Other Topical Therapies
Tar
Salicylic acid
Topical Tacrolimus, pimecrolimus
Antimicrobials
Antibiotics for culture proven infections
Ketoconazole for head and neck based atopic dermatitis (reduce yeast counts)
Phototherapy
UVB
Narrow Band UVB
UVA/PUVA
Sunlight
Other Therapies
Leukotriene Inhibitors do not work
Oral cromolyn sodium results conflicting
Interferon gamma daily s/c inj. helps
Cyclosporine
Azathioprine
Hydroxychloroquine
Some Specific Types of
Eczema
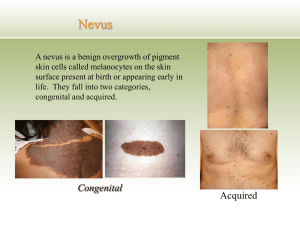
Discoid/Nummular eczema
Circular or oval plaques
A clearly demarcated edge
Related to atopy, emotional stress, bacterial infection
Usually lesions dry.
Exudative ones always associated with bacterial infections.
Treatment : Emollients, topical steroids, antibacterials
Lichen Simplex Chronicus
An eczematous dermatosis characterized by
Lichenified plaques, usually 1-2 in number
Typical sites: nape of neck, scrotum, wrists
skin thickened, pigmented with prominent skin markings
Associated with atopy, emotional stress
Tr: Superpotent steroids with keratolytic agents.
I/L steroid injections
LSC
Nodular Prurigo
Characterized clinically by chronic, intensely itchy papules & nodules
lesions range from small papules to hard nodules, 1 –3 cm in diameter, with a raised, warty surface.
The early lesion is red later becoming pigmented.
Tr: superpotent steroids, oral steroids, UVB,
PUVA, thalidomide
Pompholyx
Pompholyx is characterized by the
sudden onset of clear vesicles over hands.
Symptoms : No erythema, less pruritus but more heat and prickling sensation.
Sites : sides and dorsa of fingers & hands
Vesicles may become confluent and present as large bullae, especially on feet.
Itching may be severe, preceding the eruption of vesicles
Pityriasis Rosea (P. rosea)
An acute, self-limiting disease, probably infective in origin, affecting mainly children and young adults.
The first lesion is “ Herald patch ” a large circular, sharply defined eryhematous patch with fine scales on thigh/trunk.
This is followed by an eruption of discrete oval lesions, dull pink in colour, covered by fine, dry, silvery scales forming a collarette at edges.
The centre tends to clear and assumes a wrinkled, atrophic appearance.
The lesions appear in crops.
P.Rosea contd…….
The lesions tend occur in ‘chrismas tree’ pattern along the rib cage.
There are usually no symptoms. Some pts. have mild to moderate pruritus
Tr: The common asymptomatic, self-limiting cases require no treatment . If itch is severe or the appearance distressing, a topical steroid
(moderate potent) or UVB can be helpful .
Asteototic Eczema
Eczema developing in dry skin
Seen on legs, arms and hands.
Tends to be more marked in the winter and in elderly people.
Skin is dry, scaly showing a criss-cross skin markings. Finger pulps are dry and cracked; retaining a prolonged depression after pressure
(‘parchment pulps’).
Associated with hypothyroidism, zinc deficiency, diuretic use and cimetidine use
Pityriasis alba
A mild eczema in which hypopigmentation is the most conspicuous feature. (NO CALCIUM Deficiency
Predominantly seen in children b/w ages of 3 -16 ys.
The individual lesion is circular, oval or irregular hypopigmented patch with NOT well defined edges.
Lesions often slightly erythematous & have fine scale
Common sites : cheeks & around the mouth & chin
Less commonly on neck, arms, shoulders & trunk.
D/D: vitiligo, P. versicolor, PIH
Tr : mild steroids, emollients
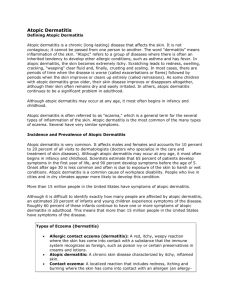
SUMMARY
Disease
Irritant CD
Typical morphology
Sharply demarcated macular erythema, little vesiculation
Exzematous, scaly edematous plaques with vesiculation
Diagnostic clues
More burning less itch, only at area of contact
Allergic CD
Atopic
Dermatitis
Sebhorroic dermatitis
Eczematous, honey-crusted scaly plaques, lichenified in chronic cases
Greasy scaly papules, minimal itch
Pruritis, primary lesion at area of contact
,
Flexural areas, neck predominance
Hair bearing areas, glabella, nasolabial folds
Xerotic/asteot ic eczema
Crackled parchment like patches, no edema, no vesiculation
Lower legs
Nummular
/discoid eczema
Pompholyx
Coin-shaped, well demarcated, scaly or weepy plaques, bilateral, symetrical, kissing lesions
Arms, legs, dorsal hands
Deep seated papulo-vesicles on palmar plantar surfaces, volar edges
Palms, soles, typical dorsal involvement
Conclusions
Eczema management rests on three pillars: avoid irritants, moisturize, topical management
Use steroids to quiet a flare then switch to a nonsteroidal therapy
Treating hot spots can prolong remissions
Control itch!
THANK YOU
This presentation is available on www.lumhs.edu.pk/DFHC/html