Head to Toe Skin Assessment
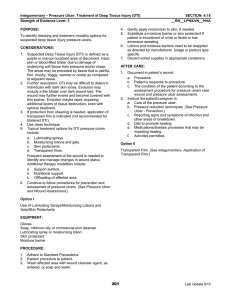
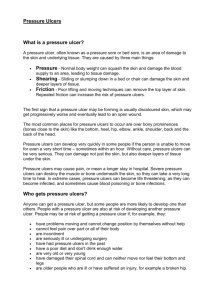
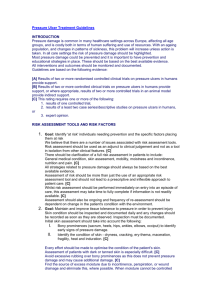
advertisement

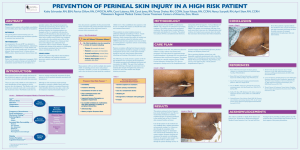
Head to Toe Skin Assessment Karen R. Brown BS, RN, CWS Wound/Ostomy Specialist Objectives: Describe essentials for maintenance of healthy skin Discuss pressure ulcer risk assessment tools Describe appropriate documentation of skin assessment SKIN ASSESSMENTS Each square inch of human skin consists of twenty feet of blood vessels A large amount of the dust in you home is actually dead skin Humans shed about 600,000 particles of skin every hour about 1.5 pounds a year. By 70 years of age, an average person will have lost 105 pounds of skin. A large amount of the dust in you home is actually dead skin Skin Facts Skin assessment important in the prevention of pressure ulcers, IAD, MADS,Intertrigo, etc. A complete skin assessment should include: Assessing for localized heat Edema Induration (hardness) Excessive moisture Skin Assessment Skin Care is important to protect the skin from breakdown: Not massaging skin Not turning the patient back onto a still reddened surface from previous pressure loading Not vigorously rubbing skin that is at risk for skin breakdown SKIN ASSESSMENT What tools do we use? Eyes Hands Ears excellent history taking and data gathering Braden Scale Nutrition Assessment Tool CONFINED TO BED/CHAIR Preventative Actions Look at skin at least once a day. Bathe only when needed for comfort or cleanliness. Prevent dry skin. Immobility/decreased mobility For a person in a chair: 1. Change position every hour or as often as possible. 2. Use foam, gel, or air cushion to relieve pressure. • Reduce friction by: Lifting, rather than dragging, when repositioning. Using cornstarch on skin. • Involve physical therapy as needed. SKIN ASSESSMENT Donuts are for eating Not sitting on NO DONUT SHAPED CUSHIONS Change position at least every 2 hours. Use a special mattress that contains foam, air, gel, or water. Raise the head of bed as little and for as short as a time as possible. For a Bed Bound Patient Loss of Bowel or Bladder Control Clean skin as soon as soiled with urine or stool. • Assess and treat urine leaks. • If moisture cannot be controlled: 1. Use absorbent pads and/or briefs with a quick-drying surface. 2. Protect skin with a cream or ointment. Poor Nutrition Eat a balanced diet. • If a normal diet is not possible, talk to health care provider about food supplements Lowered Mental Awareness Choose preventative actions for the person with lowered mental awareness. For example, if the person is chairbound, refer to the specific preventative actions outlined in Risk Factor 1. Support Surfaces SKIN ASSESSMENT DOCUMENTATION SKIN ASSESSMENT SKIN FOLDS DOCUMENT PRESENCE OF: MOISTURE RASH CANDIDA LESIONS 2007 Medline Industries, Inc. Xerosis is a dermatosis exhibited as dry scaly skin with or without erythema (redness) and pruritus (itching) xerosis Caused by epidermal water loss Loss of natural moisturization factors LOCATION: Usually lower legs Sometimes trunk and hands xerosis Clinically looks like Scaling, flaking skin Dull, white color and increased skin markings DOCUMENT changes in skin color excess skin moisture skin turgor changes in skin texture SKIN ASSESSMENT DOCUMENT ULCER LOCATIONS OVER BONY PROMINENCES HISTORY OF PREVIOUS ULCERATIONS SKIN ASSESSMENT PALPATE FOR WARMTH, TENDERNESS, BOGGINESS EDEMA DOCUMENT EVERY DETAIL ASSESS MEDICAL DEVICES DOCUMENT TYPE OF DEVICE LOCATION TYPE OF SECUREMENT DEVICE ASSESS MEDICAL DEVICES TUBE SITE EROSION HYPERGRANULATION TISSUE BARIATRIC SKIN ASSESSMENT incontinence-related dermatitis secondary to inability to perform personal hygiene, pressure ulcers (including sites other than bony prominences), venous Insufficiency/ulceration, and/or lymphedema. BARIATRIC SKIN ASSESSMENT The bariatric patient may not be able to clean the perineal area well enough or maybe not at all. BARIATRIC SKIN ASSESSMENT Pressure ulcers not over bony prominences Increased propensity for venous ulcers with or without lymphedema Malnourishment INCONTINENCE ASSOCIATED DERMATITIS (IAD) Incontinenceassociated dermatitis is a common problem affecting as many as half of the patients with urinary or fecal incontinence who are managed with absorptive products. SKIN CARE PROTOCOLS Clean after soiling and at routine intervals Avoid hot water Use mild cleansers non- irritating and non-drying agents Use moisturizers for dry skin Use barrier ointments/ sprays Powder bedpans SKIN CARE PROTOCOL Use heel/elbow protectors or socks Use lift sheets or pads to move patient Limit head elevation to 30 degrees and use knee gatch if available Use overhead trapeze (prevent dragging patient up in bed) Use footboards Use light weight clothing and covers (layering is best) Minimize environmental factors leading to drying such as low humidity/exposure to cold References Gray M, Ratliff C, Donovan A. Perineal skin care for the incontinent patient. Adv Skin Wound Care. 2002;15:170-179. Ghadially R. Aging and the epidermal permeability barrier: implications for contact dermatitis. Am J Contact Dermat. 1998;9(3):162-169. Brown DS. Perineal dermatitis risk factors: clinical validation of a conceptual framework. Ostomy Wound Manag.1995;41(10):46-48, 50, 52-53. European Pressure Ulcer Advisory Panel and National Pressure Ulcer. Treatment of pressure ulcers: Quick Reference Guide. Washington DC: National Pressure Ulcer Advisory Panel; 2009. References Portable Instructional Education (PIE). Home Health Care 1st Edition. (CD) Wound Ostomy and Continence Nurses Society, WOCN National Office, Mt. Laurel, NJ; 2008.