Eczema “The boiling over of the skin”
advertisement

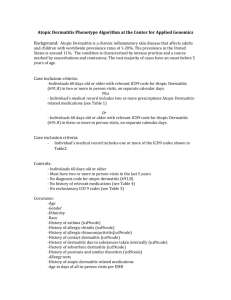
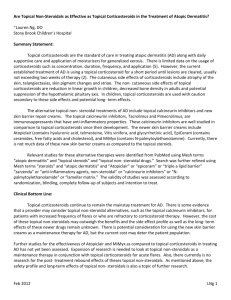
Eczema Georgia Skin and Cancer Clinic Cynthia A. Doallas, PA-C Eczema (Atopic Dermatitis) the most common inflammatory skin condition most confusing skin ailment for both patients and their nondermatologic health care providers Atopic dermatitis is the most common type of eczema. It is a chronic, inflammatory, itchy skin condition with unpredictable course of flares and remissions. It effects 5% to 10% of the United States population. Most cases begin in childhood (often in infancy); however may start any age The disease frequently remits spontaneously-reportedly in 40% to 50% of children- but it may return in adolescence or adulthood and possibly persist for a lifetime. Typically families are advised that children “will grow out of eczema” . Atopic dermatitis is an inherited Type I hypersensitivity disorder of the skin. It is usually associated with personal or family history of hay fever, asthma, allergic rhinitis or sinusitis. M Grandfather M. Grandmother MOM P. Grandfather P. Grandmother DAD BABY Normal Skin Skin of Acute Eczema Eczematous epidermis contains intercellular an intracellular fluid that appears in a sponge-like formation (spongiosis); Vasodilatation of the dermis occurs, resulting in the clinical manifestation of ACUTE eczema. Acute Eczema Appears as “itchy” erythematous patches, plaques, or papules that may develop into vesicular lesions, or may continue as a less nonvesicular, erythematous eruption. Chronic Eczema Later, the epidermis will thicken (acanthosis) and retain parakeratosis, resulting in an overabundance of cellular infiltrate in the dermis. These changes account for the scale and lichenification of CHRONIC eczema. The epidermis shows hyperkeratosis, acanthosis, and a prominent granular layer. There is liquefaction degeneration at the dermal-epidermal interface. Chronic Eczema (aka: Chronic eczematous dermatitis) Has a hallmark lichenification (plaque with an exaggeration or hypertrophy of the normal skin markings). Scale and hemorrhagic crusts can result from scratched or drying vesicles. Older lesions exhibit hypo or hyper pigmentation. Severity Atopic dermatitis can present with a wide spectrum of severity. mild, recurrent, localized itchy rash on “dry” skin or more severe, extensive eruption that can be accompanied by unremitting pruritus, sleepless nights, secondary cutaneous bacterial infections, and/or embarrassing lichenification. Effects Psychosocial problems, such as poor self-image, anger, and frustration may lead to depression and social isolation. What to look for…. The character and distribution of the skin rash tends to vary according to the patient’s age. Any or all manifestations of atopic dermatitis may exist in a single patient. The different phases of atopic dermatitis are not always clearly distinct. Infantile Phase Childhood Phase Adolescent and Adult Phase Infantile Phase (patients 2 months to 2 years of age) Eruption may become generalized, in most cases it first manifests with severe “cradle cap” or severe intertriginous rashes (groin, neck, axillae). As the patient approaches age 2 years, the flexor creases become involved. Lesions consist of scaly, red, and occasionally oozing plaques that tend to be symmetric. Occurs on the scalp face, particularly cheeks neck chest extensor extremities Childhood Phase (patients aged 2 years to 12 years of age) These patients tend to be less acute and lesions less exudative than those seen in infancy. Inflamed lesions become lichenified (especially in Asian and African-American patients) secondary to chronic rubbing and scratching. Lesions tend to occur symmetrically, with characteristic distribution in the flexural folds. Occurs on the: Antecubital and popliteal fossae Neck, wrists, and ankles May occur on the eyelids, lips, scalp, and postauricular areas Adolescent and Adult Phase (patients 12 years and older) Post inflammatory hyper or hypo pigmented changes tend to be seen. The appearance of atopic dermatitis may change to a more poorly defined, itchy, erythematous rash, possibly with papules and/or plaques. Lichenified plaques of atopic dermatitis are typically less well demarcated than are the plaques seen in psoriasis. These plaques tend to blend into surrounding normal skin. Clinical Aspects Clues to diagnosing Atopic Dermatitis: Persistent Xerosis, or dry, “sensitive” skin. “Allergic Shiners”-this refers to the darkened or tanned coloring in the periorbital areas. Hyperlinear palmar creases Follicular eczema (most common in AfricanAmerican patients) Ichthyosis vulgaris Keratosis Pilaris Possible Complications Pruritus (itching) may interfere with sleep. Pruritis is increased by repeated scratching and rubbing, which leads to lichenification, oozing, and secondary bacterial infection. Secondary infection with Staphylococcus aureus may trigger relapse of atopic dermatitis. Differential Diagnosis Diagnosis of atopic dermatitis is generally not difficult, especially in patients with atopic history. The following should be considered or excluded: Contact Dermatitis Determine whether the patient was exposed to a substance that could cause contact dermatitis. The location of the lesions may suggest an external cause. Differential Diagnosis Psoriasis Lesions are generally in extensor locations (elbows, knees, and other large joints) rather than the flexor creases. May be palmar or plantar as seen in this image. Patients typically have a positive family history of psoriasis. Psoriasis is less pruritic than eczema, lesions tend to be clearly demarcated from normal surrounding skin, and the scale of psoriasis tends to be thicker in appearance. However, psoriasis may at times be clinically indistinguishable from atopic dermatitis Differential Diagnosis Tinea A positive KOH test or fungal culture result will confirm (remember, an unresolved eczematous-like rash, worsening with topical corticosteroids could be tinea) Once I diagnosis it, how do I treat it? Topical Corticosteroid Therapy General Principles: Application of an appropriately chosen topical steroid will usually bring prompt improvement in a patient with atopic dermatitis. Topical Steroids should be used only as short-term therapy. (Two weeks on, two weeks off unless severe flare). They should not be used for prevention of future lesions or for cosmetic concerns, such as post inflammatory hyperpigmentation “Stronger” is often preferable to “Longer” in the use of topical steroids, because long-term application is more often associated with side effects. Topical Steroids can be used in conjunction with “Wet wrap Usage”. When the condition is under control, the frequency of application and the potency should be reduced. Low potency steroids should be used to treat the face and body folds. Wet Wraps and Moisturizers Combination Therapies to be used with Topical Steroid Topical Immunomodulator Therapy (six-week intervals) Tacrolimus (Protopic) 0.03% or 0.1% ointment (age-dependent) Pimecrolimus (Elidel) 1% cream Other Therapeutic Measures Antihistamines prn Benadryl Atarax or Cyproheptadine, Palgic and other H-1 blockers Minimal Mild, moisturizing soaps (i.e. Vani, Dove, Cera Ve Fragrance-free regimine Oils/Moisturizers Derma-Smoothe FS Robathol Olive Crisco Lard Vanicream, Cera Ve Mimyx, Atopiclair, Hylira Avoidance Irritants: Recommend non-irritant fabric, such as cotton. Wool may induce itching Overheating and sweating: Excess dryness or humidity should be avoided. An air conditioner or humidifier in a child’s bedroom may help to avoid the dramatic changes in climate that may trigger outbreaks. Allergens: Environmental elimination of airborne substances may bring lasting relief. Severe cases In severe patients that failed oral and tropical corticosteriods consider Cellcept. Points to Remember Topical Steroids should be applied only to inflamed skin (active disease). When Topical Steroids are applied immediately after bathing their penetration and potency are increased. Low-potency topical steroids are recommended for use on the face and in skin folds. There are primarily two causes of eczema: Outside (contact dermatitis) Inside (atopic dermatitis) Patients and their parents, caregivers, and teachers should be educated on the manifestations and management of atopic dermatitis The National Eczema Association can be contacted at (503) 228-4430 or www.eczema-assn.org Thank you for your attention Questions?