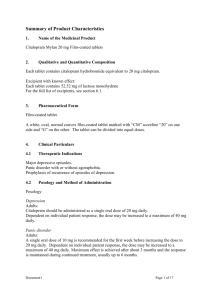
Citalopram/Escitalopram flowchart
advertisement
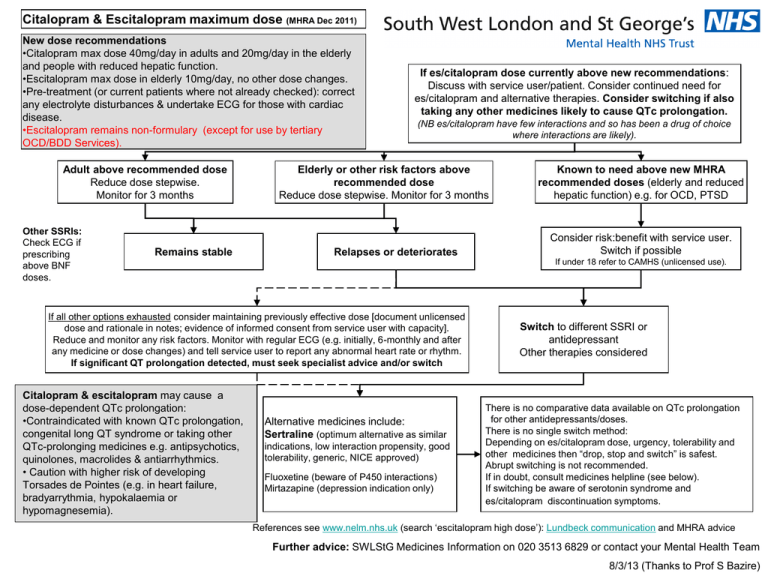
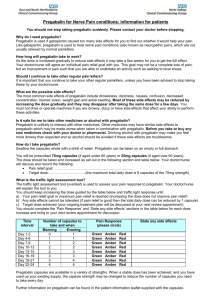
Citalopram & Escitalopram maximum dose (MHRA Dec 2011) New dose recommendations •Citalopram max dose 40mg/day in adults and 20mg/day in the elderly and people with reduced hepatic function. •Escitalopram max dose in elderly 10mg/day, no other dose changes. •Pre-treatment (or current patients where not already checked): correct any electrolyte disturbances & undertake ECG for those with cardiac disease. •Escitalopram remains non-formulary (except for use by tertiary OCD/BDD Services). Adult above recommended dose Reduce dose stepwise. Monitor for 3 months Other SSRIs: Check ECG if prescribing above BNF doses. Remains stable If es/citalopram dose currently above new recommendations: Discuss with service user/patient. Consider continued need for es/citalopram and alternative therapies. Consider switching if also taking any other medicines likely to cause QTc prolongation. (NB es/citalopram have few interactions and so has been a drug of choice where interactions are likely). Elderly or other risk factors above recommended dose Reduce dose stepwise. Monitor for 3 months Relapses or deteriorates Consider risk:benefit with service user. Switch if possible If under 18 refer to CAMHS (unlicensed use). If all other options exhausted consider maintaining previously effective dose [document unlicensed dose and rationale in notes; evidence of informed consent from service user with capacity]. Reduce and monitor any risk factors. Monitor with regular ECG (e.g. initially, 6-monthly and after any medicine or dose changes) and tell service user to report any abnormal heart rate or rhythm. If significant QT prolongation detected, must seek specialist advice and/or switch Citalopram & escitalopram may cause a dose-dependent QTc prolongation: •Contraindicated with known QTc prolongation, congenital long QT syndrome or taking other QTc-prolonging medicines e.g. antipsychotics, quinolones, macrolides & antiarrhythmics. • Caution with higher risk of developing Torsades de Pointes (e.g. in heart failure, bradyarrythmia, hypokalaemia or hypomagnesemia). Known to need above new MHRA recommended doses (elderly and reduced hepatic function) e.g. for OCD, PTSD Alternative medicines include: Sertraline (optimum alternative as similar indications, low interaction propensity, good tolerability, generic, NICE approved) Fluoxetine (beware of P450 interactions) Mirtazapine (depression indication only) Switch to different SSRI or antidepressant Other therapies considered There is no comparative data available on QTc prolongation for other antidepressants/doses. There is no single switch method: Depending on es/citalopram dose, urgency, tolerability and other medicines then “drop, stop and switch” is safest. Abrupt switching is not recommended. If in doubt, consult medicines helpline (see below). If switching be aware of serotonin syndrome and es/citalopram discontinuation symptoms. References see www.nelm.nhs.uk (search ‘escitalopram high dose’): Lundbeck communication and MHRA advice Further advice: SWLStG Medicines Information on 020 3513 6829 or contact your Mental Health Team 8/3/13 (Thanks to Prof S Bazire)