Pancreatitis & Hepatic Failure
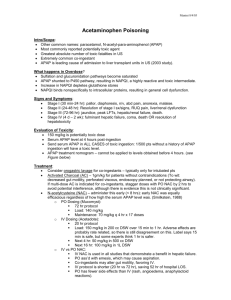
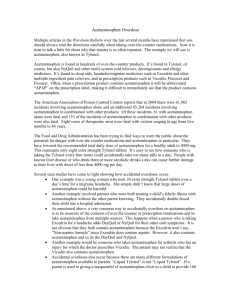
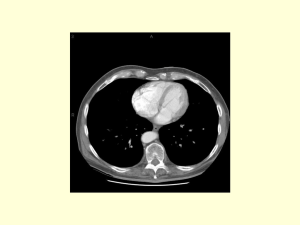
advertisement

Leanna R. Miller, RN, MN, CCRN-CSC, PCCN-CMC, CEN, CNRN, CMSRN, NP Education Specialist LRM Consulting Nashville, TN inflammatory response and potential necrosis of pancreatic endocrine and exocrine cells as the result of premature activation of pancreatic enzymes Presenting Signs & Symptoms pain (upper abdomen) – 95% –edema and distension –chemical burn –release of kinin –obstruction of biliary tree Presenting Signs & Symptoms Acute Abdomen protracted vomiting abdominal tenderness guarding distension tympany Presenting Signs & Symptoms Severe disease –hypovolemic shock –Grey Turner’s sign –Cullen’s sign Diagnostics Serum amylase –elevated during 1st 24 hours after onset of signs –may remain elevated for only 2 days –> 300 mcg/dL Diagnostics Serum lipase –elevates within 24 to 48 hours of disease –remains elevated for 5 - 7 days –can indicate pseudocyst Hypocalcemia –free fatty acid-albumin complexes bind calcium –decreased PTH function Radiographic Studies Computed tomography (CT) – gold standard for diagnosis Complications Pancreatic Abscess • high fever, palpable mass, abdominal tenderness, N & V, leukocytosis & hyperglycemia • surgery required Complications Pancreatic Pseudocyst • abdominal pain, fever, N & V > 1 week • WBC or amylase remains elevated Medical Goals prevent & control shock relieve pain suppress pancreatic stimulation Medical Goals support the patient minimize the occurrence of complications • • • 64 year old woman develops upper abdominal pain late last night. Band-like with radiation to back. Initially not severe, but awoke and had several episodes of non-bloody emesis. The first 8 hours in ED/Hospital the patient required 36 mg MSO4 to control pain. • • • PMHx: HTN, Hyperlipidemia MEDS: Estrace, Plendil SOCIAL: no tobacco or ETOH use • • • • • BP: 94/45 160/90, HR: 76, T: 97.9, GEN: awake alert HEENT: no icterus, mouth is dry CARDIO: ST ABD: no rebound tenderness, no bruising • ABD CT: marked peri-pancreatic fluid, streaking around pancreas, normal enhancement, no clear gallstones, CBD not dilated LABS: • AST/ALT both slightly elevated. • T.bilirubin normal • Amylase 2620 • Lipase 26,625 • Hct normal • WBC 14.8 Ranson’s Criteria • Admission • • • • • Age > 55 WBC > 16,000 Glucose > 200 LDH > 350 AST > 250 • During first 48 hours • • • • • • Hematocrit drop > 10% Serum calcium < 8 Base deficit > 4.0 Increase in BUN > 5 Fluid sequestration > 6L Arterial PO2 < 60 5% mortality risk with <2 signs 15-20% mortality risk with 3-4 signs 40% mortality risk with 5-6 signs 99% mortality risk with >7 signs • • At 36 hrs the patient has increased work of breathing, crackles at bases of lungs. She is 4 liters ahead on fluids. What do you want to do? • “Vigorous intravenous hydration alone is the best available option in the prevention of pancreatic necrosis.” • Pitchhumoni et al. “Mortality in Acute Pancreatitis,” Journal of Clinical Gastroenterology • AGGRESSIVE FLUID RESUSCITATION • May require 250-500 cc/hr for first 48 hrs – 6 L of fluid is sequestered in abdomen alone – Third spacing can consume up to 1/3 of total plasma volume • 1/3 of people die in the first phase 50% of these are associated to ARDS • PULMONARY EDEMA ≠ CHF • How do you know you have resuscitated the patient? • Blood pressure • Heart rate • Urine output • SaO2/ABG’s show good oxygenation and no acidemia • AGGRESSIVE FLUID RESSUCITATION • may create electrolyte imbalances that need to be corrected • may need CVP monitoring (central line) • CXRs help (CHF vs ARDS) • ABGs help (still hypoxic need more fluids?) • 23% of SAP pts get ARF 80% mortality • 0.5 cc/kg/hr urine output is goal (need a Foley) NECROSIS • Starts to occur within 4 days of disease • CT with oral & IV contrast is gold standard • necrotic areas do not enhance • will NOT see it on CT before 48hrs NECROSIS • once diagnosis of necrosis is made mortality jumps • 40-60% get secondary infection • mortality then approaches 80% • • • secondary infection symptoms: • N/V, epigastric pain, distension, fever, elevated WBC diagnosis of sterile vs infected necrosis • CT-guided needle aspiration the most devastating complication and marks the second peak in mortality (@ 2 weeks) SECONDARY INFECTIONS n n What bugs? Gram (-) bacteria cross from gut • • • • • E. coli (35%) Klebsiella (24%) Enterococcus (24%) Staph (14%) Pseudomonas, proteus, strep, enterobacter, bacteroides, anaerobes ANTIOBIOTICS • Controversial • DO decrease incidence of infection in necrosis, but do NOT decrease mortality • Gotta cover multiple bugs • Gotta get into pancreas • If you see necrosis start antibiotics NUTRITION • normal pancreas secretes up to 2 liters/day of secretions • pancreatic stimulation during AP releases proteolytic enzymes autodigestion • oral feeding increases release of secretin and cholecystokinin stimulates pancreas • “rest the pancreas” “NPO” • ENTERAL vs TPN Feedings: • If distal to Ligament of Treitz (nasojejunal tube or J-tube) pancreatic secretion = basal rate • Both started after 48 hours – Easier to restart po feedings – Average length of nutritional support shorter • 7 vs 11 days – Fewer septic complications – $23/day vs $222/day • • NEW THOUGHTS • Meta-analysis of 15 randomized studies: • Compared early vs delayed ENTERAL feedings in 753 critically ill pts • Early was 36 hrs! • Improved: • Wound healing • Host immune function • Preservation of intestinal mucosal integrity • Decreased infections BUT, no decreased mortality Case continues • By 48 hours patient’s abdominal pain is worsening • HR is 140, afebrile, BP normal • Abdomen shows very subtle guarding • WBC: 27.6 • Ca++: 6.6 Case continues • • • • • PO2: 61 Base deficit: 8 BUN rise: 9 LDH: 976 RANSON SCORE: 3 Case continues • Patient transferred to ICU • Central line & Arterial line • Repeat Abdominal CT: new bilateral pleural effusions, pancreas enhanced in tail only. • Patient died 5 weeks after admission SUMMARY • They may look good, but… • Score severity early • Use lots of IVF • Go to ICU early • Early enteral feedings work better Hepatic Failure cirrhosis: –alcoholic with malnutrition –biliary cirrhosis hepatitis hepatatoxins hypoperfusion Hepatic Failure Signs & Symptoms – asterixis – jaundice – obtundation – distended abdomen & ascites – renal failure – GI bleed Hepatic Failure Treatment –encourage rest –limit protein, amino acids & fat –prevent exposure to stress Hepatic Failure Treatment: Monitor –hemodynamic status –serum drug levels –lab tests Hepatic Failure Treatment –monitor EEG –maintain glucose –monitor for ICP Hepatic Failure Treatment –jaundice = vitamin K –thrombocytopenia = folic acid & FFP, platelets –DIC = fibrinogen & heparin Hepatic Failure Treatment for varicies –saline lavage –administer blood –IV vasopressin or somastatin –Sengstaken – Blakemore tube –portacaval shunt On May 3 (approx. 2200 hours) a 35 year old alcoholic male began to take 2-3 acetaminophen 500 mg tablets per hour because of a toothache. He continued this through the night until 0800 hours. What is the recommended therapeutic dose for acetaminophen? • • Adults: 4 grams per day. Children: 75 mg/kg/day to a maximum of 4 grams per day. • • • On May 4,the patient presented to the ED because of his toothache and was discharged home with Tylenol #3. He went home and took 3-4 Tylenol #3 at 0900 hours. At approx. 1100 hours he developed abdominal pain and N/V and returned to the ED. His acetaminophen level was 212 umol/L and his AST was 990 IU/L. How do you interpret these numbers? • • Because it is a chronic ingestion you can not plot it on the nomogram. In instances where it is a chronic ingestion or the time of ingestion is unknown, send an acetaminophen level and an AST(ALT) and if either are elevated start N-acetylcysteine Rumack-Matthew Nomogram • IV NAC is initiated. • How does ethanol affect acetaminophen toxicity? • • • Chronic alcoholics are at increased risk with an acetaminophen overdose. Chronic ethanol consumption induces the cytochrome P450 pathway resulting in increased metabolism through this pathway and therefore increased NAPQI formation. Malnourishment decreases glutathione stores. On May 5 his acetaminophen level was nondetectable and his AST was 22,733 (2305 hours) and his INR was 19. Is his liver failure secondary to chronic alcohol abuse or acetaminophen toxicity? How long would you continue his NAC and why? • • • Aminotransferase elevation in chronic ethanol abuse rarely exceeds 1000 IU/L. It is not unusual for severe acetaminophen toxicity to have elevations in the 10,000’s IU/L. In alcoholics with acetaminophen overdoses and elevated aminotransferases, err on the side of caution and treat with IV NAC. How long would you continue his NAC and why? • Continue IV N-acetylcysteine until his INR is less than 2. • N-acetylcysteine has antioxidant and free radical scavenging effects which have been shown to decrease mortality in fulminant hepatic failure. • When would you transfer this patient to a hospital that could do liver transplants? • What are the indications for a liver transplant? Transfer for transplant consideration! • INR > 5 at anytime. • Metabolic acidosis (pH <7.35 or CO2 <18) • Hypoglycemia. • Renal Failure (creatinine >200 umol/L) • Encephalopathy Indications for Transplant! • pH <7.3 after adequate fluid replacement. • Grade III or IV encephalopathy plus either: • PT >100 seconds • Creatinine > 292 umol/L • The patient was continued on IV Nacetylcysteine and on May 14 his INR was 1.16. • Will this patient have any chronic liver damage from his acetaminophen overdose? • No, patients who recover from an acetaminophen overdose go on to have completely normal liver function with no chronic sequelae