HEALTH EQUITY:
THE INDIAN CONTEXT
Subodh S Gupta
Health Indicators among selected
countries
Country
IMR (per 1000 LB)
MMR (per 100,000
LB
Female Life
Expectancy (yrs)
India
58
259
66.9
China
32
56
74.2
Japan
3
10
86.1
Republic of Korea
3
20
81.5
Indonesia
36
230
69.9
Malaysia
9
41
76.2
Vietnam
27
130
73.5
Bangladesh
52
380
65.1
Nepal
58
740
63.4
Sri Lanka
15
92
77.5
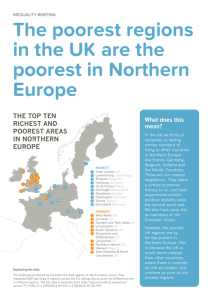
National averages often
mask substantially worse outcomes
for many disadvantaged groups
of population
Infant Mortality Rate according to
wealth quintiles
IMR
80
70
60
50
40
IMR
30
20
10
0
Poorest
Q2
Q3
Q4
Richest
Infant Mortality Rate in different states
according to wealth quintiles
120
100
India
Tamilnadu
Gujarat
Bihar
Uttar Pradesh
Rajasthan
Assam
80
60
40
20
0
Poorest
Q2
Q3
Q4
Richest
Framework for identifying pathways
leading to health inequities
Introduction
The political economy context
The organisational structure and delivery
mechanism
Health financing mechanisms
Coverage patterns
Current status of health and health care
Per Capita Gross Domestic Product
(PPP)
Percent population below poverty line
(GOI data)
The Political Economy Context
Second most populous country
A democratic federal structure; subdivided into states
and Uts; further into districts
Local levels of governance (Panchayat Raj)
Health – a state subject
Alapuzzha in Kerala Vs.
Kishanganj in Bihar
Characteristics of Indian Health System
Complex mixed health system - Tax
based health finance system with small
health insurance sector
- Publicly financed government
health system
- Fee-levying private health sector
Health Expenditure in India
Sources of Health Care Financing in
Different Countries
Financial Protection in Health
Individuals should be able to access health care
when they need it and not be prevented from doing
so by excessive cost.
When they do access health care, they should not
incur costs that prevent them from obtaining other
basic household necessities such as food, education
and shelter.
Catastrophic Health Expenditure
If health expenditures exceed a certain percentage of
household income or capacity to pay, and therefore
drive a household into poverty or prevent a household
from buying other essential items including food and
education.
Twelve percent of households have catastrophic health
expenditure.
About a third of poor households have catastrophic
health expenditure.
Impoverishment due to catastrophic health expenditure
is higher (about half) among middle economic status
households.
Percent of Households Compromising or Postponing
Consumption Decisions after Seeking Inpatient Care
(3 Districts, West Bengal)
Relative Share of Sources of Financing to Pay for
Inpatient Care
(3 Districts, West Bengal)
Percent of Rural Persons with an Illness who could not Seek
Treatment due to Financial Constraints, by Economic Quintile
(3 districts, West Bengal)
Effect of Economic Reforms on Public Health
Increasing unregulated privatisation with little
accountability to patients
Systematic deregulation of drug prices resulting in
skyrocketing prices of drugs
Selective intervention approach instead comprehensive
primary health care
Health Inequity in outcomes
Rural/ Urban/ Urban (slum)
Inter/ Intra state
Socio-economic status
Gender
Caste
Religion
Coverage with health services
according to wealth quintile
100
88.8
90
80
71
70
60
55.3
30
49
46.9
50
40
67.2
33.2
24.4
20
31.8
19.4
58
55.2
49.8
43.5
49.1
34.6
30.6
21.5
13.2
10
10
0
Immunization
Coverage
Skilled Provider Use of modern IFA consumption
at birth
contraceptive
>90
Poorest
Q2
Q3
Q4
Richest
U5 Mortality Rate in different states
according to wealth quintiles
160
140
120
India
Tamilnadu
Gujarat
Bihar
Uttar Pradesh
Rajasthan
Assam
100
80
60
40
20
0
Poorest
Q2
Q3
Q4
Richest
Underweight by Wealth Quintiles
Percent
70
60
50
40
30
57
49
41
34
20
20
10
0
Lowest Second Middle Fourth Highest
Poor
Nutrition as a Contributing
Factor to
Undernutrition
Among
Children
Undernutrition in Children under Age 5
Under-Five
Mortality
INDIA
Under Five Years
Poor nutrition
contributes to 54% of
48 age 5
deaths under
Percent underweight (NCHS/WHO Growth Reference)
Percent
India 2005-06
Bangladesh 2007
Nepal 2006
Niger 2006
Madagascar 2003-4
Ethiopia 2005
Cambodia 2005-06
Mali 2006
Nigeria 2003
Guinea 2005
Malawi 2004
Kenya 2003
Cameroon 2004
Zimbabwe 2005-06
Swaziland 2006-07
DR 2007
Neonatal
deaths
ARI
Contribution to
Under-5 Mortality
Severe malnutrition
11%
Diarrhoea
4
Malaria
41
39
36
32
Mild to moderate
malnutrition
29
43%
Prevalence of
26
underweight higher in India
than in any of the other
40 countries with DHS
surveys in the last 5
years.
Measles
22
20
Other
19
causes
16
7
46
45
44
Trend data provides strong evidence of declines in the sex ratio
of the population age 0-6 and the sex ratio at birth….
Females per 1,000 males
Sex ratio of population age 0-6
934
Sex ratios at birth of live
births and births that have
died
Live
926
918
991
936
NFHS-1
(1992-93)
NFHS-2
(1998-99)
Dead
NFHS-3
(2005-06)
NFHS-1
(1987-91)
1,045
1,011
931
NFHS-2
(1993-97)
910
NFHS-3
(2000-04)
…females are under-represented among births and overrepresented among births that die.
• After the first month of life, girls are more likely to die than boys: The
child mortality rate is 61% higher for girls than for boys.
Child mortality: Deaths between the ages of 1-4 years per
1,000 children surviving to age 1 year
Female
41
Male
28
18
24
9
18
11
Lowest
Second
Middle
Wealth quintile
6
Fourth
5
4
Highest
The three different levels of
government action
First Level: The Macro Level
The level of the government's national budget. Here, the major
concern will be the amount of resources allocated to health,
but an important secondary concern will be the possible
reallocations of budgets to reach poor people better.
Second Level: The Health System Level
Here, the concern will be to put together reforms and improve
incentives to get the system to function better for poor people.
Third Level: The Micro Level
The service delivery level, where the focus will be on how to
implement specific activities to reach poor people.
Work at these three levels is interdependent
Health Financing
Pricing policies that reduce and/or eliminate user
fees for basic services;
Cross-subsidization of health services that benefit
the poor;
Strengthening exemption mechanisms services;
Expanding social insurance to cover informal sector
workers;
Developing community-financing arrangements;
Developing equity funds to pay for the poor
Thank you
Achieving health equity
within a generation is
possible. It is the right thing
to do, and now is the right
time to do it.
- Commission on Social
Determinants of Health