Ortho Post op Pain
advertisement

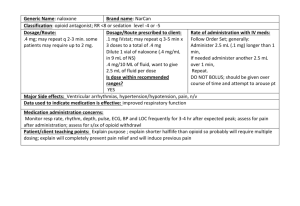
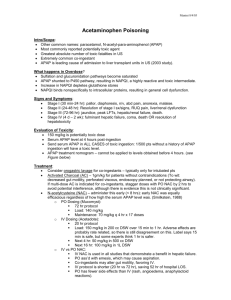
Perioperative Pain Management Using a MultiModal Approach Melanie MacInnis; PharmD, RPh Clinical Pharmacist, HHS/McMaster May 2012 Learning Objectives • After this presentation, the learner should be able to: – Describe the rationale of multimodal analgesia – Understand the role of acetaminophen, NSAIDs and gabapentin in post-operative pain control – Determine patient specific factors for prescribing a multi modal pain control regimen Pain Definitions Pain is defined by IASP as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage”. Analgesia Postop Pain “The major difference between iatrogenic pain and other types of pain is that iatrogenic pain is anticipated. Therefore, the physician has an excellent opportunity to deal with such pain in a planned and expeditious manner.” Brian Goldman, MD The Role of Pain Control in Postoperative Care • Prevent suffering • Hasten recovery • Influence perioperative morbidity • Decrease the development of chronic pain Chronic Pain Medications • • • • • • • • • • • • • Anti-inflammatories (NSAIDs, steroids) Muscle relaxants Benzodiazepines TCAs and other anti-depressants (SSRIs, SNRIs) Anticonvulsants (Gabapentin, Pregabalin, Carbamazepine) Opioids Tramadol IV Anti-arrhythmics (lidocaine, bretylium) Topical formulations (capsaicin, lidocaine, NSAIDs) Alpha 2-agonists (clonidine, guanethedine) Cannabinoids (Nabilone) NMDA antagonists (ketamine, methadone, memantine) Osteoclast inhibitors (calcitonin, alendronate) Opioid Tolerance • Shortened duration and decreased intensity of analgesia, euphoria, sedation, and other CNS effects • Predictable pharmacologic adaptation • Rightward shift in the dose-response curve means increasing amount of drug to maintain the same effects • In general, the higher the daily dose, the greater the degree of tolerance • Individuals requiring >1 mg IV (3 mg PO) morphine per hour for a period of > 1 month are considered to have high-grade tolerance and withdrawal symptoms World Institute of Pain 2005; 5(1): 18-32 Can J Anesth 2006; 53 (12): 1190-99 Problems of Equi-Analgesic Dose Ratios of Opioids • Incomplete cross tolerance occurs during chronic opioid use • Accumulation of active metabolites can influence effect of opioids • The ratios may change according to the direction of opioid switch Strategies for Pain Control • Multimodal analgesia: balanced technique • Determine and continue baseline opioid requirements, in addition to acute pain requirements • Treat contributing co-morbidities, such as anxiety, poor sleep, nausea and constipation • Order pain medications in the acute phase routinely, rather than PRN CNS Drugs 2007; 21(3): 185-211 Multi modal analgesia • Different classes of drugs exert different side effects • Side effects can be dose related • Additive/synergistic • Combinations can provide superior analgesia than either drug alone • Opioid sparing • Improved recovery, shorter hospital stay Acetaminophen • Very weak COX inhibitor – No appreciable anti-inflammatory or NSAID side effects • Liver metabolism • 4g/d in healthy adults • Lower doses: – Liver disease (2g/d) – Alcoholism (2g/d) – Frail elderly (3.2g/d) “Tylenol” • • • • Always confirm with patients Extra strength tylenol ≠ tylenol with codeine PRN vs RTC Acetaminophen as part of multi-modal analgesia minimizes opioid requirements by 20% NSAIDS • Effective for post operative pain • MOA: – Inhibit cyclo-oxygenase (COX) in the periphery and spinal column – Several variants of COX enzyme – Influence platelet function, GI mucosa, and renal function, CV risk – Selecting the COX variant to avoid side effects Adverse effects • Platelet dysfunction – NSAIDs alone not a risk for spinal hematoma • GI ulceration • Nephrotoxicity • Headache, tinnitus, abdominal pain, rash, hyperkalemia, asthma Renal function • Serum creatinine is used as a surrogate • NB: extremes of body weight and nourishment • Baseline SCr and while on NSAID • Also urea nitrogen, I/O • Cockroft Gault • eGFR • SCr = (140-age)(kg) x 0.85 if female (SCr)(72) http://nephron.com/cgi-bin/CGSI.cgi OR www.globalrph.com (from calculators menu select CrCl multi-calc under C) Monitoring for NSAIDs • CBC (plts), SCr, BUN, lytes • Absolute contra-indication – GI ulcer, hx of PUD/GUD; CHF; low platelets; CrCl less than 30ml/min • Relative contraindication – Fracture, GERD, age • Celecoxib: sulfa allergy; only COX-2 selective, 200mg/d max • Ketorolac: only IV product, po • Ibuprofen: suspension, OTC or rx, po • Naproxen: OTC or rx, po or pr NSAIDs + Acetaminophen • • • • • • 21 studies 1909 patients Ibuprofen, diclofenac, ketorolac, aspirin Lower pain scores Lower supplemental analgesic requirements Better global pain relief Anesth Analg 2010; 110:1170-9 NSAIDs + Acetaminophen APAP+NSAID % more effective Pain intensity lessened Analgesic supplementation lessened 64% 37.7% 31.3% 85% 35.0% 38.8% NSAID APAP + NSAID APAP NSAIDs + Acetaminophen • No evidence of increased side effects • If morphine rescue required; higher incidence of N/V Analgesic Efficacy • NNT calculated for at least 50% pain relief over 4-6h compared to placebo • Oral, single dose • Moderate to Severe pain • All are oral unless otherwise specified • Doses in mg Analgesic (mg) NNT Ibuprofen 600 or 800 1.7 Ibuprofen 400 2.5 Acetaminophen 650 + oxycodone 10 (2 Percocet) 2.6 Ketorolac 10 2.6 Naproxen 500 2.7 Morphine 10mg IV 2.9 Ketorolac 30mg IV 3.4 Acetaminophen 500 3.5 Celecoxib 200 3.5 Acetaminophen 1000 (2 Extra Strength Tylenol) 3.8 Acetaminophen 650 + codeine 60 (2 Tylenol #3) 4.2 Acetaminophen 650 (2 Tylenol Plain) 4.6 Acetaminophen 325 + oxycodone 5 (1 Percocet) 5.5 Acetaminophen 325 + codeine 30 (1 Tylenol #3) 5.7 Codeine 60mg 16.7 Gabapentinoids • Gabapentin (Neurontin) and pregabalin (Lyrica) • Enhance the inhibitory pain pathway long term • Impact sodium gated channels of nerves in the periphery • Prevent hyperalgesia postoperatively • Modify transmission of nerve impulses • Can prevent persistent post surgical pain at 3-6 months Gabapentinoids • Role in post-operative treatment is unclear • Can reduce pain intensity and opioid consumption • Optimal dose and duration unknown – Gabapentin: 300-1200mg pre op, post op 100-300mg variety of dosing strategies – Pregabalin: 150-300mg pre-op, post op doses 50mg150mg of durations 24h – 2 weeks • No influence on prevention of PONV Gabapentinoids • • • • Renally eliminated SCr needed baseline and after initiation Dose reduction in renal impairment After long term use needs to be tapered to DC (seizure risk) • In elderly can cause confusion, sedation, dysphoria Take Home Points • Multimodal analgesia can help improve pain control and minimize side effects • Persistent postsurgical pain may be influenced by improved acute pain control • Order routine pain medications initially for moderate to severe pain (rather than PRN) Take Home Points • Patient specific factors need to be considered in prescribing the best post-operative analgesic regimen • Around the clock NSAIDS + acetaminophen are effective and minimize opioid use • The role of gabapentinoids is unclear in post operative pain control Thank you. Questions and Comments.