High_Risk_Antepartum_Nursing_Care_3
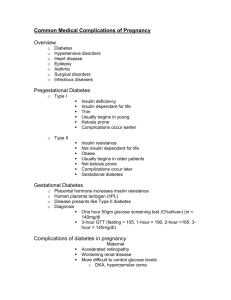
advertisement
Clinical Severe nausea and vomiting Severe dehydration-fluid loss Electrolyte imbalance: Manifestations: Hypokalemia Hyponatremia Ketosis- Ketones in the urine (Ketonuria) Metabolic acidosis Weight loss Bleeding gums Complications: Metabolic acidosis Starvation/malnutrition Acid-base imbalance Maternal death Fetal problems (CNS malformation, IUGR) Termination of pregnancy NURSING IV therapy with replacement of electrolytes and possible TPN. Maintain NPO status for 24-48 hour vomiting has stopped Facilitate the client’s environment- quiet , stress free, and odor free Assess and Monitor: CARE: VS, I&O, Daily wt. Nutritional status, Emotional support. Laboratory studies: CBC, UA, Serum chemistries, and liver function studies Administer antiemetics- Relgan , Zofran, Nursing After vomiting has stopped diet progresses slowly : Care: Clear liquids Bland diet – cold foods first, small servings, without fluid Regular diet Teach client about the disease process, procedures and treatments, diet, medications, and follow up care Provide emotional support Monitor Fetus if ordered. Diabetes Mellitus Cardiac disease or conditions Hypothyroidism Hyperthyroidism Anemia’s Rh sensitization Systemic Lupus erythematosus Anticardiolipin Antibody Syndrome Myasthenia gravis Renal Disease Epilepsy Asthma DIABETES MELLITUS is an endocrine order in which major effect is on carbohydrate metabolism and is the results from an inadequate product of insulin or insulin resistance Classification of DM: Pregestational: Gestational: Type I Type II Type III (GDM) White’s Classifications of diabetes in pregnancy Pregestational It is best if the client have her diabetes mellitus under control before getting pregnant. Blood sugars in normal ranges Preconceptual care and guidance Type I: Diabetes: Insulin therapy will vary Complications: Ketoacidosis Fetal problems-IUGR Type II: Possible oral agent will be change or change to Insulin Fetal problems Gestational Diabetes Mellitus is the result of the pancreas is unable to meet the increase demands for insulin production during pregnancy and/or insulin resistance from various hormones during pregnancy: Increase cortisol level Placenta hormones-Human Placenta lactogen (hPL), insulinase GDM starting in the last half of the pregnancy around 28-32 weeks) Client may show Clinical Manifestations of DM and problems with immune system-Freq. UTI’s and can It is diagnosis by : Elevated blood glucose levels GTT-1 hour or 3hour Review Diabetes mellitus Hypoglycemia Hyperglycemia Diabetes Ketoacidosis (DKA) Normal Adult Blood Glucose Levels Risk clinical manifestations of: factors for GDM(Class A) : Pregnancy Obesity Previous large infants, previous unexplained stillborn Complications: Varies with the degree of extent of disease process of DM Preeclampsia Polyhydraminos Abortion Fetal Anomalies‘- Cardiac and Neurolical defects Stillbirth Neonatal Problems: Macrosomia Hypoglycemia Hyperbilirubinemia Delayed lung maturity? RDS NURSING Facilitate maintaining blood glucose levels within normal levels: Teach or review: CARE: ADA diet Assessing Blood glucose Exercise Medications: NO Oral Hypoglycemic Agents ( except for those that do not cross the placenta) Insulin Monitor fetal well being- FMC and other Calories- 30-35 kcal/IBW(Kg) in first trimester and 35-36 Kcal/IBW(Kg) per day. 3-4 small meals and 3-4 snack per day Bedtime snack important with at least 25grams of carbohydrates At least 250 Grams of carbohydrates per day. Carbohydrates- 50-60% of calories Protein-12-20% of calories Fats-limited to under 30grams according to ADA & AHA Nursing Care: Monitor client for development of complications Prepare for possible preterm delivery or cesarean section. Intrapartum care will depend on the extent of the disease process and blood glucose levels- IV Insulin therapy maybe used. Maintain postpartum blood glucose levels ( blood glucose levels will drop in this period because of hormonal influences of pregnancy decrease and stop-about 34days after delivery.) Careful observation of the neonate whose mother has DM. CARDIAC DISEASE and pregnancy : Because of the hemodynamic changes that occur in pregnancy the client who has a cardiac disorder will have problems and complications. Outcomes will depend on the degree of cardiac compromise. See NYHA Classifications of heart disease. Clients who have a history of Rheumatic fever may have undiagnosed cardiac effects, and may need further evaluation. Client will never to be seen by Cardiologist and Perinatalogist NSG. DX- Decrease cardiac output, Fluid volume excess, Activity intolerance, Risk for infection, Anxiety. I II III IV Classification Asymptomatic will normal levels of activity-No physical limitations Slightly compromised Symptomatic with greater than ordinary physical activity Marked compromised Symptomatic with ordinary activity Capacity Functional Severely compromised Complications: Decreased cardiac output and altered blood flow Decreased maternal and fetal perfusion Congestive heart failure Preterm delivery Death NURSING CARE: Teach client to maintain healthy life style: Adequate nutrition for pregnancy Take Prenatal vitamins and iron to prevent anemia Avoid excessive weight gain Stress management Exercise such as walking No over exertion and frequent rest periods Monitor for signs of infection Go to all appointments with her physicians Monitor fetal well being with FMC Report signs of cardiac decompensation ( heart failure)to health care providers Assess and monitor for signs of cardiac decompensation. Medication therapy: Prenatal vitamins and iron Stool softeners Prophylactic Antibiotics with any invasive procedures and before delivery Cardiac glycosides (digitalis) Antidysrhythmia agents Furosemide (Lasix) – only with CHF Heparin if anticoagulant therapy is needed No warfarin (Coumadin) Nursing Care: Head of bed elevated Labor: Avoid excessive stress Epidural anesthesia is preferred No prolonged pushing in labor- forceps or vacuum extraction may be used Postpartum: Continue prenatal vitamins and iron Frequent rest periods No staining with BM’s Monitor closely during this period for cardiac decompensation Iron Deficiency Anemia ( Microcyctic) Folic Acid Deficiency Anemia (Macrocyctic) Sickle Cell Anemia ETC. Any problem with low RBC’s will effect oxygenation to maternal and fetal tissues Iron Deficiency Anemia is a result of a decrease intake of iron. It can range from mild to severe. The decrease of RBC’s can effect the transportation of oxygen to the maternal organs and to the fetus. All pregnant women need to increase their intake of iron during pregnancy through diet or supplements Foods high in Iron. SICKLE CELL DISORDER is a heterozygous form of hemoglobin S (HbAS) that is common in people from the Mediterrian area and Africa. It is an Autosomal Recessive Disorder. Sickle Cell Anemia(SCA) is the most common inherited anemia complicating pregnancy. SCA Crisis because of the stress of the pregnancy. Clinical manifestations of SCA Crisis: Hemolytic anemia Pain in joints , back, abdomen, extremities Blood clots Infections Infarction to organs Precipitated factors for SCA Crisis : Hypoxia Acidosis Dehydration Stress Cold Infection Complications of SCA CRISIS: Vaso-occlusion Crisis Pain Pulmonary emboli Folic anemia Fetal problems: IUGR Stillborn Hypoxia NURSING CARE: Asses and monitor client for clinical manifestations of SCA Crisis and complications Provide the client a warm environment, and hydration ,possible blood transfusions Be prepared to start IV, give O2, analgesia. Medications: Folic Acid Heparin- not warfarin Analgesia-NO ASA and Demerol