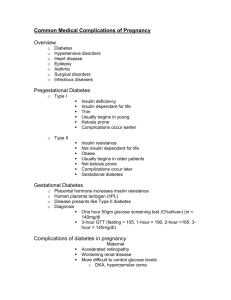
Management of maternal cardiac arrest
advertisement
Dr A Hards, Dr S Davies, Dr A Salman, Dr M Balki Mount Sinai Hospital 2010 Aim To enable you to competently manage a case of maternal cardiac arrest Objectives To review relevant maternal physiology To review standard ACLS guidelines To review ACLS modifications for pregnancy Physiology of pregnancy Respiratory System 1. 60% increase in oxygen consumption & decreased FRC Implications – rapid desaturation & hypoxemia 2. increased minute ventilation and hypoxic ventilatory response Implications - chronic respiratory alkalosis, difficult determining benign vs. sinister causes of dyspnea 3. increased capillary engorgement & mucosal edema Implications – airway bleeding, nasal congestion, difficult airway, failed intubation Physiology of pregnancy Cardiovascular System 1. cardiac output increases by 50% (due to increased HR & SV). Increased contractility and LVEF. 2. SVR and PVR fall by up to 35%. SBP, DBP, MAP decrease during mid preganancy, return to baseline near term 3. Aorto-caval compression occurs from 13-16 weeks Implications - supine hypotension - higher femoral/IVC pressures Physiology of Pregnancy Gastrointestinal System 1. Anatomical changes 2. Reduced lower esophageal sphincter pressure 3. Increased intra-gastric pressure 4. Delayed gastric emptying in labour but probably normal at other times Implications - High incidence of gastro-oesophageal reflux - Increased risk of aspiration from ~ 16-20 weeks gestation Physiology of Pregnancy Hematological System 1. 50% increase in plasma volume 2. 30% increase in red cell volume 3. Increased platelet turnover, clotting and fibrinolysis Implications - delayed presentation of hypovolaemia - physiological anemia of pregnancy - pro-coagulopathic state ACLS in pregnancy Essentially follows same guidelines as for non- pregnant patients AHA recommend some modifications based on physiology ACLS Cardiac Arrest Algorithm 2010 AHA Modifications for pregnancy Ventilate with cricoid pressure (remove if impeding ventilation, oxygenation or intubation) Early intubation with a smaller diameter ETT (such as 6.5 cm) Left Uterine Displacement Position hands 1-2cm higher on sternum for chest compressions Remove fetal monitoring for defibrillation Do not use femoral or leg veins for IV access Consider emergency cesarean section Emergency cesarean section Rationale for early CS - Provides effective maternal resuscitation (improves venous return & cardiac output) - If fetus > 24-25 weeks may save the life of the baby Management Do not move patient to OR prior to CS Continue maternal resuscitation during CS Aim for skin incision by 4 minutes Aim for delivery by 5 minutes Cause of arrest Always consider the “Hs and Ts” Hypovolemia Hypoxia Hydrogen ions Hypo/erkalemia Hypothermia Tension PTX Tamponade Toxins Thrombosis, cardiac Thrombosis, coronary Pregnancy-specific causes mnemonic “BEAU- CHOPS” Maternal cardiac arrest algorithm Copyright © American Heart Association Vanden Hoek T L et al. Circulation 2010;122:S829-S861 Any questions? Summary Reviewed relevant maternal physiology Reviewed standard ACLS guidelines Reviewed modifications for pregnancy