eprint_2_25950_825
advertisement

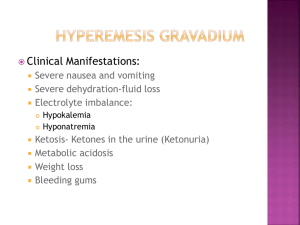
Diabetic disease in pregnancy& it’s complication Definition: is defined as carbohydrate disturbance characterized by hyperglycemia & either peripheral insulin resistance or insulin deficiency. There are 2 types of D.M : 1.IDDM(type 1) 2.NIDDM( type 2) Where there my be a serological evidence of autoimmune destruction of pancreatic islets & genetic marker in type 1 DM, type 2 may be hyperglycemia for long period without clinical symptoms( familial). The symptoms of D.M is closely related to the degree of hyperglycemia& these include polyurea, polydepsia, weight loss, recurrent vulvar boils& bleured vision. Incidence: It complicate 1-2% of pregnancy with high PNM& mortality reach about 65% but after introduction of insulin ,this percentage fall as in non diabetic mother in a well controlled D.M. Pathophysiology: During pregnancy ,there is significant change in carbohydrate metabolism& glucose homeostasis secondary to complex hormonal changes like estrogen ,progesterone ,human placental lactogen& cortisol. HPL lead to increase lipolysis in the adipose tissue, this result in the production of glycerol & fatty acid which are used as a source of energy by the mother & this lead that glucose up take in the cell is inhibited ,so a lot of glucose is available to the fetus. The placenta not only produce diabetogenic hormones but also break down insulin. Reduced threshold for glucose & increase GFR result in glucoseuria in about 5-50% of women. Classification of D.M: White classification include A. asymptomatic but abnormal GTT, equal to impaired GTT. B. Onset age equal or more than 20 years,duration less than 10 years,no vascular complication. C. Onset age 10-19 years,duration 10-19 years, no vascular complication. D. Onset age less than 10 years, duration equal or more than 20 years,vascular disease ,benign retinopathy, leg artery calcification. E. Nephropathy F. Proliferate retinopathy. Diagnosis of D.M in pregnancy: The onset of IDDM is commonly between the age of 11-14 years& therefore in most patient the diagnosis is made before pregnancy. So serial blood glucose estimation & glycosylated Hb will be useful in making the diagnosis. So the diagnostic criteria for D.M are: 1. symptoms of D.M plus RBS equal or more than 11.1 mmol\L 2. FBS equal or more 7.0 mmol\L 3. 2-hour plasma glucose equal or more11.1 mmol\L during OGGT. Complication of pre-existing D.M : 1. Maternal effect: a. exacerbation of pre-exiting disease like retinopathy ,so ophthalmic assessment is recommended during pregnancy. b. Diabetic nephropathy affect 5-10% of people. c. Cardiac disease :circulatory& CVS changes during pregnancy are responsible for the deterioration of cardiac function & mortality rate may reach 50% in patient with previous MI. Late complication like PIH&PET. Intrapartum complication: related to operative morbidity consequent to fetal macrosomia, obstructed labor& operative delivery. 2. Fetal effect: a. early complication: 1. congenital malformation: these depend on the degree & timing of glycemic control, where there is optimum control prepregnancy ,at conception& in the first trimester, the rate approximate to that of un complicated pregnancy, while it is 5-10 times higher in uncontrolled D.M. these anomalies includeASD,VSD,TGA,NTD,caudal regression syndrome( sacral agenesis which is pathognomonic) ,polycystic kidney, double ureter, tracheo-esophgeal fistula, bowel atresia &imperforated anus. 2. increase incidence of miscarriage& missed abortion. b.late complication : 1. polyhydramnia occur in 22-26% of uncontrolled D.M 2. macrosomia: body weight > 4 kg or varies from 4-4.5 kg. It is ten times higher in D.M . as there is a greater adiposity & muscle mass in macrosomic baby ,the head is spared 3.Iatrogenic preterm delivery : is three fold higher in D.M. 4. stillbirth: due to poorly controlled D.M,fetal macrosomia, co-exiting vasculopathy, PET. Stillbirth is commonly occur after 36 weeks due to :1. chronic hypoxia 2. Reduction in uterine blood flow in vasculopathy 3.frequant fluctuation in RBS level 4. ketoacidosis & infection. c. intrapartum complication: this related to macrosomia like shoulder dystocia, increase rate of C\S, long bone fracture, Erb’s pulsy & Klumpk’s pulsy. d. neonatal complication: jaundice ,polycythemia ,tetany, hypoglycemia, hypocalcemia& hypomagnecemia. Management of D.M during pregnancy: Usually achieved by team consist of physician, obstetrician, GP & diabetic midwife. Pre-pregnancy management is necessary as when control is optimum, the PNM & mortality is similar to non diabetic one. So 1.mother education about tight control. 2.screening & treating the complication like retinopathy, nephropathy & cardiac dysfunction. 3. pre-pregnancy & first trimester folic acid supplement. 4.modified diet. 5. stop smoking& adequate exercise. 6.glycosylated Hb(HbA1c) should be <6.5%. Management during pregnancy: Maternal manag. Most patient are usually on insulin before pregnancy & this should be maintained during pregnancy while patient on oral hypoglycemic drugs should be change to insulin of the risk of hypoglycemia & teratogenic effect. Other modality is insulin analog like Lispro but some study show that it is teratogenic. During first trim, Sometime need to decrease the dose of insulin because of N&Vomiting, however insulin requirement need to increase in the second & third trim. Insulin given in a different regimen either short acting giving pre-meal & long acting at bed time so blood sugar need to be monitored by doing FBS, &2hour post prandial so at least 4 reading of blood sugar is taken in addition to measurement of HbA1c which give idea about control in the previous 3 months. The patient should be educated about sign & symptom of hypoglycemia which should be treated by either oral dextrose or injectable glucagons (I.M or S.C) . Also the woman should be alert about s&s. of ketoacidosis which has high PNM reach to 30%. So the aim is to keep 1. FBS< or equal to5.5 mmol\L. 2. 2hour post prandial < or equal to 7.0 mmol\L. 3. HbA1c<6.5%. Fetal management: 1. dating U\S should be done 2. anomaly scan at 20-22 weeks & fetal echo. 3. regular U\S for fetal growth& AFI to identify macrosomia & polyhydramnia respectively. 4. close fetal surveillance during third trimester because of high incidence of still birth. Also fellow up by cick count ,NST, umbilical artery Doppler are recommended. Management of labor & delivery: If diabetic control is optimum & there is no fetal or maternal complication ,induction of labor at 38-39 weeks is done . the mode of delivery is by NVD& C\S is done for obstetric indication however the rate may reach to 50% because of fetal macrosomia & failure of induction so when fetal weight is > 4.5 kg, elective C\S is done. Insulin requirement fluctuate considerably during labor & fall quickly after delivery so continuous I.V infusion of glucose & insulin is recommended, prolonged labor is avoided. So at day of induction advice for 1. normal diet 2.no over night fasting & normal dose of insulin. 3. at day of induction give half morning dose of insulin& commence I.V infusion of5% or 10% dextrose. Insulin infusion given through infusion pump. 4. measure capillary blood glucose every 30-60 minutes to maintain blood sugar between 4.0-7.0 mmol\L 5. continuous CTG. 6. using PG pessary for cervical ripening, then do ARM & oxytocin augmentation when indicated. During C\S: 1.woman fasting from 12 midnight 2.omit morning dose of insulin 3. give 5% dextrose & insulin infusion during C\S. 4. monitoring blood sugar just like NVD. Post partum management: 1. continue with insulin infusion until the patient start eating. 2. re commence the patient to pre-pregnancy insulin dose or 1/3 the initial dose. 3. patient with NIDDM. Can recommence to their oral hypoglycemic drugs when start oral intake. 4. monitor blood sugar hourly post operative & then after each meal for the next 48 hours. 5. advice the mother about contraceptive like low dose oral contraceptive pills , progesterone only pills , condom & other barrier methods , if she complete her family sometime do sterilization. سها وتوت. LEC:2 Gestational Diabetes G.D.M.: is defined as a carbohydrate intolerance that begins or first diagnosed during pregnancy& in most cases resolves after pregnancy.(therefore woman with previously unrecognized NIDDM or newly diagnosed IDDM is considered also as G.D.M . In most cases diagnosis is made in the late second & early third trimester after screening for various indication. Incidence: It affect about 2-5% of pregnant woman & about 50% of them will develop overt type 2 D.M in the future. Screening for G.D.M: Because G.D.M is associated with adverse effect on pregnancy & significant no. of patient will develop overt D.M so it is important to screen for G.D.M. There are 2 approach for screening: universal screening & selective one. Selective screening adopted for high risk pregnancy but it will miss 50% of woman with G.D.M. HIGH RISK GROUP ARE: 1. glucose urea on one occasion in the first trim. & 2 occasion in the second trim. 2. polyhydramnia in current pregnancy 3. macrosomia (abdominal circumference >95th centile) in current pregnancy. 4. history of big baby > 4.0 kg. 5. previous unexplained still birth 6. positive family history of D.M( first degree relative) 7. obesity BMI > 25 8. old age >35 years 9. Asian race 10.previous history of G.D.M 11. history of recurrent abortion. 12.patient with PCOS. Timing of oral glucose tolerance test(OGTT) is between 26-28 weeks of gestation because insulin resistance at it’s maximum value& there is variable absorption of glucose from GIT after this gestation. Other method for screening is FBS, RBS, but those are not sensitive tests. So if blood sugar level within 2 hour is >7mmol\ L or FBS is >4.8 mmol\L then do full GTT. Other screening test is miniGTT & blood sugar >7.8 mmo\l so do full GTT. OGTT miniGTT We use 75 mg of oral glucose 50 gm is used Over night fasting no fasting Asso. With N & vomiting less N& V Measure blood sugar at 1\2 measure blood sugar at Hour, 1 hour, 2 hour 1 hour Venous blood sample is better than capillary blood for fallow up the patient blood sugar because capillary blood sugar is higher after meal than venous blood. Diagnosis of G.D.M: The diagnosis is usually depend on OGTT ( using 75 gm glucose ) However many units in USA still used 100 gm loading test. The WHO recommended criteria for diagnosis are: 1.FBS equal or >5.5 mmol\L 2. 2 hour post prandial equal or >8.0 mmol\L. Or WHO criteria as following: FBS 2 hour p.p Normal woman <7.0 mmol\l <7.8 mmol\l Impaired GTT <7.0mmol\l >7.8 mmol\l Overt G.D.M >7.0 mmol\l >11.1 mmol\l Glycosylated HbA1c has no role in the diagnosis of G.D.M but useful in the screening. Complication of G.D.M: In poorly controlled diabetes ,the PNM is 4 times higher than controlled one. 1. maternal complication: 1. PET& PIH. 2. recurrent vulvovaginitis &candidacies 3. obstructed labor 4. increase incidence of operative deliveries( forcipes, ventose &C\S) 5. D.M in the future. 2. fetal complication: ? macrosomia ? polyhydramnia ? RDS ? Preterm labor ? Unexplained IUD ? Traumatic delivery ? Neonatal complication like jaundice ,polycythemia , tetany, hypoglycemia , hypocalcaemia ,hypomagnesaemia. Management: 1. monitoring of glycemic control & this done by measuring pre & post prandial blood sugar at least 4-7 times \day. 2. fetal monitoring :it is generally accepted that antenatal fetal monitoring to minimize the risk of adverse outcome is essential in the following groups: ? poorly controlled D.M ? D.M on insulin ? Woman with history of previous still birth ? Woman with history of chronic hypertension& PIH Monitoring of fetal wellbeing is done by different approach: 1. regular U\S 2.biophysical profile 3.NST 4. Doppler velocimetry 3. glucose control: The aim is to maintain normoglycemia &this achieved by : 1. dietary control 2. insulin therapy 1. dietary control: This is best achieved by counseling of dietitian & patient is generally advice to consume 50% or more of their energy from carbohydrates, 30% of protein & less than 20% from fat. As the dietary restriction is advised to be 30-35%Kcal\kg\day or equal to2000-2400 kcal\day. During pregnancy ,there is accelerated starvation , therefore at least three meals & 4 snacks are given with the last snack at bed time to avoid the risk of overnight hypoglycemia. 2.insulin therapy: Is indicated in a. FBS>5.8 mmol\l b. 2 hour post prandial >7.8 mmol\l c. Fetal macrosomia at third trim. Diagnosed by presence of abdominal circumference of > 95centile at 29-33 weeks of gestation. d. Failed dietary treatment : failure of control blood glucose after 2 weeks of diet ,indicate switch to insulin. 3.oral hypoglycemic drugs: It is not recommended during pregnancy because: 1. are teratogenic 2. cause fetal hypoglycemia 3. it is difficult to achieve tight control with these agents. 4. delivery: There is co traversal about the time of delivery in patient with G.D.M but when there is good glycemic control& uncomplicated maternal & fetal condition, delivery is done at 38-39 weeks& because of the risk of RDS ,the use of steroid is considered in all deliveries before 36-37weeks. Usually NVD is the mode of delivery & but fetal macrosomia & risk of shoulder dystocia lead to the increase rate of C\S to 50%. So C\S is indicated in 1. fetal weight > 4.5kg 2. fetal weight between 4-4.5 kg but there is other risk factor like past obstetric history, failure of progress of labor. Note: Management of labor , delivery & when doing C\S should be the same as patient with pre-existing D.M . Puerperium: Insulin requirement after delivery usually return to pre-pregnancy level after the placenta has been delivered so after delivery ,the woman : 1. on diet :stop diet restriction 2. on insulin: must reduce their insulin requirement & insulin stopped once patient start oral intake. 3. contraceptive can be used :a. low dose o.cc.p for woman non lactating. ( b.progesterone only pills c.barriar d. rarely IUCD) for lactating one. Long term follow up: Because about 50% of them will develop type 2 D.M later in life ,so screening with full OGTT after 6 weeks (after Puerperium ) is required.