lec_2
advertisement

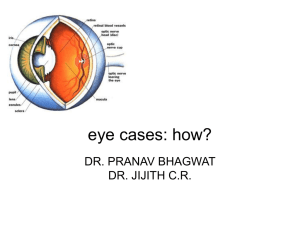
Grodno State Medical University DESEASES OF LIDS, LACRIMAL ORGANS, CONJUNCTIVA AND CORNEA Pavel Ch. Zavadski Assistant lecturer Of the Department of Ophthalmology DESEASES OF LIDS The eyelids are important both in providing physical protection to the eyes and in ensuring a normal tear film and tear drainage. Diseases of the eyelids can be divided into those associated with: •abnormal lid position •inflammation of the lid •lid lumps •abnormalities of the lashes ABNORMALITIES OF LID POSITION This is an abnormally low position of the upper eyelid. PATHOGENESIS It may be caused by: 1) Mechanical factors (Large lid lesions pulling down the lid, Lid oedema, Tethering of the lid by conjunctival scarring, Structural abnormalities including a disinsertion of the aponeurosis of the levator muscle, usually in elderly patients) 2) Neurological factors (Third nerve palsy, Horner’s syndrome, due to a sympathetic nerve lesion) 3) Myogenic factors (Myasthenia gravis, Some forms of muscular dystrophy, Chronic external ophthalmoplegia) SYMPTOMS AND SIGNS Patients present because: they object to the cosmetic effect; vision may be impaired. There is a reduction in size of the interpalpebral aperture. The upper lid margin, which usually overlaps the upper limbus by 1–2 mm, may be partially covering the pupil. The function of the levator muscle can be tested by measuring the maximum travel of the upper lid from upgaze to downgaze (normally 15–18 mm). MANAGEMENT It is important to exclude an underlying cause whose treatment could resolve the problem (e.g. myasthenia gravis). Ptosis otherwise requires surgical correction. In very young children this is usually deferred but may be expedited if pupil cover threatens to induce amblyopia. ENTROPION This is an inturning, usually of the lower lid. It may occur if the patient looks downwards or be induced by forced lid closure. It is seen most commonly in elderly patients where the orbicularis muscle becomes weakened. It may also be caused by conjunctival scarring distorting the lid (cicatricial entropion). The inturned lashes cause irritation of the eye and may also abrade the cornea. The eye may be red. Short-term treatment includes the application of lubricants to the eye or taping of the lid to overcome the inturning. Permanent treatment requires surgery. ECTROPION The malposition of the lids everts the puncta and prevents drainage of the tears, leading to epiphora. It also exposes the conjunctiva. This again results in an irritable eye. Treatment is surgical. BLEPHARITIS This is a very common condition of chronic eyelid inflammation. The condition causes squamous debris, inflammation of the lid margin, skin and eyelash follicles (anterior blepharitis). The meibomian glands may be affected independently (meibomian gland disease or posterior blepharitis). SYMPTOMS 1) tired, sore eyes, worse in the morning; 2) crusting of the lid margin. SIGNS 1) scaling of the lid margins; 2) debris in the form of a rosette around the eyelash, the base of which may also be ulcerated, a sign of staphylococcal infection;3) a reduction in the number of eyelashes;4) obstruction and plugging of the meibomian ducts;5) cloudy meibomian secretions;6) injection of the lid margin;7) tear film abnormalities. TREATMENT This is often difficult and must be long term. For anterior blepharitis, lid toilet with a cotton bud wetted with bicarbonate solution or diluted baby shampoo helps to remove squamous debris from the eye. Similarly, abnormal meibomian gland secretions can be expressed by lid massage after hot bathing. Staphylococcal lid disease may also require therapy with topical antibiotics (fusidic acid gel) and, occasionally, with systemic antibiotics. Meibomian gland function can be improved by oral tetracycline. Topical steroids may improve an anterior blepharitis but frequent use is best avoided. Posterior blepharitis can be associated with a dry eye which requires treatment with artificial tears. CHALAZION This is a common painless condition in which an obstructed meibomian gland causes a granuloma within the tarsal plate. Symptoms are of an unsightly lid swelling which usually resolves within 6 months. If the lesion persists it can be incised and curetted from the conjunctival surface. An abscess (internal hordeolum) may also form within the meibomian gland, which unlike a chalazion is painful. It may respond to topical antibiotics but incision may be necessary. A stye (external hordeolum) is a painful abscess of an eyelash follicle. Treatment requires the removal of the associated eyelash and applicationof hot compresses. Most cases are self-limiting. Occasionally systemic antibiotics are required. CYSTS Various cysts may form on the eyelids. Sebaceous cysts are opaque. They rarely cause symptoms. They can be excised for cosmetic reasons. A cyst of Moll is a small translucent cyst on the lid margin caused by obstruction of a sweat gland. A cyst of Zeis is an opaque cyst on the eyelid margin caused by blockage of an accessory sebaceous gland. These can be excised for cosmetic reasons. SQUAMOUS CELL PAPILLOMA This is a common frond-like lid lesion with a fibrovascular core and thickened squamous epithelium. It is usually asymptomatic but can be excised for cosmetic reasons with cautery to the base. XANTHELASMAS These are lipid-containing bilateral lesions which may be associated with Hypercholesterolaemia. They are excised for cosmetic reasons. NAEVUS (MOLE) These lesions are derived from naevus cells (altered melanocytes) and can be pigmented or non-pigmented. No treatment is necessary. BASAL CELL CARCINOMA This is the most common form of malignant tumour. Ten per cent of cases occur in the eyelids and account for 90% of eyelid malignancy. The tumour is: slow growing; locally invasive; non-metastasizing. Patients present with a painless lesion on the eyelid which may be nodular, sclerosing or ulcerative (the so-called rodent ulcer). It may have a typical, pale, pearly margin. A high index of suspicion is required. Treatment is by: 1) Excision biopsy with a margin of normal tissue surrounding the lesion. Excision may also be controlled with frozen sections when serial histological assessment is used to determine the need for additional tissue removal. This minimizes destruction of normal tissue. 2) Cryotherapy. 3) Radiotherapy. The prognosis is usually very good but deep invasion of the tumour can be difficult to treat. SQUAMOUS CELL CARCINOMA This is a less common but more malignant tumour which can metastasize to the lymph nodes. It can arise de novo or from pre-malignant lesions. It may present as a hard nodule or a scaly patch. Treatment is by excisional biopsy with a margin of healthy tissue. UV exposure is an important risk factor for both basal cell and squamous cell carcinoma. TRICHIASIS This is a common condition in which aberrant eyelashes are directed backwards towards the globe. It is distinct from entropion. The lashes rub against the cornea and cause irritation and abrasion. It may result from any cicatricial process. In developing countries trachoma is an important cause and trichiasis is an important basis for the associated blindness. Treatment is by epilation of the offending lashes. Recurrence can be treated with cryotherapy or electrolysis. Any underlying abnormality of lid position needs surgical correction. DESEASES OF LACRIMAL ORGANS Disorders of the lacrimal system are common and may produce chronic symptoms with a significant morbidity. The lacrimal glands normally produce about 1.2iµl of tears per minute. Some are lost via evaporation. The remainder are drained via the naso-lacrimal system. The tear film is reformed with every blink. Abnormalities are found in: 1) tear composition; 2) the drainage of tears. AQUEOUS INSUFFICIENCY—DRY EYE A deficiency of lacrimal secretion occurs with age and results in keratoconjunctivitis sicca (KCS) or dry eyes. When this deficiency is associated with a dry mouth and dryness of other mucous membranes the condition is called primary Sjögren’s syndrome. When KCS is associated with an auto-immune connective tissue disorder the condition is called secondary Sjögren’s syndrome. Rheumatoid arthritis is the commonest of these associated disorders. SYMPTOMS Patients have non-specific symptoms of grittiness, burning, photophobia, heaviness of the lids and ocular fatigue. These symptoms are worse in the evening because the eyes dry during the day. In more severe cases visual acuity may be reduced by corneal damage. SIGNS In mild cases there are few obvious signs. Staining of the eye with fluorescein will show small dots of fluorescence (punctate staining) over the exposed corneal and conjunctival surface. In severe cases tags of abnormal mucus may attach to the corneal surface (filamentary keratitis) causing pain due to tugging on these filaments during blinking. TREATMENT Supplementation of the tears with tear substitutes helps to reduce symptoms and a humid environment around the eyes can be created with shielded spectacles. In severe cases it may be necessary to occlude the punta with plugs, or more permanently with surgery, to conserve the tears. OBSTRUCTION OF TEAR DRAINAGE (INFANT) The naso-lacrimal system develops as a solid cord which subsequently canalizes and is patent just before term. Congenital obstruction of the duct is common. The distal end of the nasolacrimal duct may remain imperforate, causing a watering eye. If the canaliculi also become partly obstructed the non-draining pool of tears in the sac may become infected and accumulate as a mucocoele or cause dacrocystitis. Diagnostically the discharge may be expressed from the puncta by pressure over the lacrimal sac. The conjunctiva, however, is not inflamed. Most obstructions resolve spontaneously in the first year of life. If epiphora persists beyond this time, patency can be achieved by passing a probe via the punctum through the naso-lacrimal duct to perforate the occluding membrane (probing). A general anaesthetic is required. OBSTRUCTION OF TEAR DRAINAGE (ADULT) The tear drainage system may become blocked at any point, although the most common site is the naso-lacrimal duct. Causes include infection or direct trauma to the naso-lacrimal system. HISTORY The patient complains of a watering eye sometimes associated with stickiness. The eye is white. Symptoms may be worse in the wind or in cold weather.There may be a history of previous trauma or infection. SIGNS A stenosed punctum may be apparent on slit lamp examination. Epiphora is unusual if one punctum continues to drain. Acquired obstruction beyond the punctum is diagnosed by syringing the naso-lacrimal system with saline using a fine cannula inserted into a canaliculus. A patent system is indicated when the patient tastes the saline as it reaches the pharynx. If there is an obstruction of the naso-lacrimal duct then fluid will regurgitate from the non-canulated punctum. The exact location of the obstruction can be confirmed by injecting a radio-opaque dye into the naso-lacrimal system (dacrocystogram); X-rays are then used to follow the passage of the dye through the system. TREATMENT It is important to exclude other ocular disease that may contribute to watering such as blepharitis. Repair of the occluded naso-lacrimal duct requires surgery to connect the mucosal surface of the lacrimal sac to the nasal mucosa by removing the intervening bone (dacryocystorrhinostomy). The operation can be performed through an incision on the side of the nose but it may also be performed endoscopically through the nasal passages thus avoiding a scar on the face. INFECTIONS OF THE NASO-LACRIMAL SYSTEM Closed obstruction of the drainage system predisposes to infection of the sac (dacryocystitis). The organism involved is usually Staphylococcus. Patients present with a painful swelling on the medial side of the orbit, which is the enlarged, infected sac.Treatment is with systemic antibiotics. A mucocoele results from a collection of mucus in an obstructed sac, it is not infected. In either case a DCR may be necessary to prevent recurrence. DESEASES OF CONJUNCTIVA The ocular surface is regularly exposed to the external environment and subject to trauma, infection and allergic reactions which account for the majority of diseases in these tissues. SYMPTOMS 1) Pain and irritation. Conjunctivitis is seldom associated with anything more than mild discomfort. Pain signifies something more serious such as corneal injury or infection. This symptom helps differentiate conjunctivitis from corneal disease. 2) Redness. In conjunctivitis the entire conjunctival surface including that covering the tarsal plates is involved 3) Discharge. Purulent discharge suggests a bacterial conjunctivitis. Viral conjunctivitis is associated mainly with a watery discharge. SIGNS 1) Papillae. These are raised lesions on the upper tarsal conjunctiva, about 1imm in diameter with a central vascular core. They are nonspecific signs of chronic inflammation. They result from fibrous septa between the conjunctiva and subconjunctiva which allow only the intervening tissue to swell with inflammatory infiltrate. 2) Follicles. These are raised, gelatinous, oval lesions about 1imm in diameter found usually in the lower tarsal conjunctiva and upper tarsal border, and occasionally at the limbus. Each follicle represents a lymphoid collection with its own germinal centre. Unlike papillae, the causes of follicles are more specific (e.g. viral and chlamydial infections). 3) Dilation of the conjunctival vasculature (termed ‘injection’). 4) Subconjunctival haemorrhage, often bright red in colour because it is fully oxygenated by the ambient air, through the conjunctiva. BACTERIAL CONJUNCTIVITIS Patients present with: redness of the eye; discharge; ocular irritation. The commonest causative organisms are Staphylococcus, Streptococcus, Pneumococcus and Haemophilus. The condition is usually self-limiting although a broad spectrum antibiotic eye drop will hasten resolution. Conjunctival swabs for culture are indicated if the condition fails to resolve. The commonest organisms are: 1) Bacterial conjunctivitis (usually Gram positive). 2) Neisseria gonorrhoea. In severe cases this can cause corneal perforation. Penicillin given topically and systemically is used to treat the local and systemic disease respectively. 3) Herpes simplex, which can cause corneal scarring.Topical antivirals are used to treat the condition. 4) Chlamydia. This may be responsible for a chronic conjunctivitis and cause sightthreatening corneal scarring.Topical tetracycline ointment and systemic erythromycin is used is used to treat the local and systemic disease respectively. VIRAL CONJUNCTIVITIS This is distinguished from bacterial conjunctivitis by: 1) a watery and limited purulent discharge; 2) the presence of conjunctival follicles and enlarged pre-auricular lymph nodes; 3) there may also be lid oedema and excessive lacrimation. The conjunctivitis is self-limiting but highly contagious. The commonest causative agent is adenovirus and to a lesser extent Coxsackie and picornavirus. Adenoviruses can also cause a conjunctivitis associated with the formation of a pseudomembrane across the conjunctiva. Certain adenovirus serotypes also cause a troublesome punctate keratitis. Treatment for the conjunctivitis is unnecessary unless there is a secondary bacterial infection. Patients must be given hygiene instruction to minimize the spread of infection (e.g. using separate towels).Treatment of keratitis is controversial. The use of topical steroids damps down symptoms and causes corneal opacities to resolve but rebound inflammation is common when the steroid is stopped. CHLAMYDIAL INFECTIONS Different serotypes of the obligate intracellular organism Chlamydia trachomatis are responsible for two forms of ocular infections. Inclusion keratoconjunctivitis is a sexually transmitted disease and may take a chronic course (up to 18 months) unless adequately treated. Patients present with a mucopurulent follicular conjunctivitis and develop a micropannus (superficial peripheral corneal vascularization and scarring) associated with subepithelial scarring. Urethritis or cervicitis is common. Diagnosis is confirmed by detection of chlamydial antigens, using immunofluorescence,or by identification of typical inclusion bodies by Giemsa staining in conjunctival swab or scrape specimens. Inclusion conjunctivitis is treated with topical and systemic tetracycline. The patient should be referred to a sexually transmitted diseases clinic. Trachoma is the commonest infective cause of blindness in the world although it is uncommon in developed countries. The housefly acts as a vector and the disease is encouraged by poor hygiene and overcrowding in a dry, hot climate. The hallmark of the disease is subconjunctival fibrosis caused by frequent reinfections associated with the unhygienic conditions. Blindness may occur due to corneal scarring from recurrent keratitis and trichiasis. Trachoma is treated with oral or topical tetracycline or erythromycin. Azithromycin, an alternative, requires only one application. Entropion and trichiasis require surgical correction. ALLERGIC CONJUNCTIVITIS This may be divided into acute and chronic forms: 1) Acute (hayfever conjunctivitis). This is an acute IgE-mediated reaction to airborne allergens (usually pollens). Symptoms and signs include: itchiness; conjunctival injection and swelling (chemosis); lacrimation. 2) Vernal conjunctivitis (spring catarrh) is also mediated by IgE. It often affects male children with a history of atopy. It may be present all year long. Symptoms and signs include: itchiness; photophobia; lacrimation; papillary conjunctivitis on the upper tarsal plate (papillae may coalesce to form giant cobblestones; limbal follicles and white spots; punctate lesions on the corneal epithelium; an opaque, oval plaque which in severe disease replaces an upper zone of the corneal epithelium. Initial therapy is with antihistamines and mast cell stabilizers (e.g. sodium cromoglycate; nedocromil; lodoxamide). Topical steroids are required in severe cases but long-term use is avoided if possible because of the possibility of steroid induced glaucoma or cataract. Contact lens wearers may develop an allergic reaction to their lenses or to lens cleaning materials leading to a giant papillary conjunctivitis (GPC) with a mucoid discharge. Whilst this may respond to topical treatment with mast cell stabilizers it is often necessary to stop lens wear for a period or even permanently. Some patients are unable to continue contact lens wear due to recurrence of the symptoms. CONJUNCTIVAL DEGENERATIONS Cysts are common in the conjunctiva. They rarely cause symptoms but if necessary can be removed. Pingueculae and pterygia are found on the interpalpebral bulbar conjunctiva. They are thought to result from excessive exposure to the reflected or direct ultraviolet component of sunlight. Histologically the collagen structure is altered. Pingueculae are yellowish lesions that never impinge on the cornea. Pterygia are wing shaped and located nasally, with the apex towards the cornea onto which they progressively extend. They may cause irritation and, if extensive, may encroach onto the visual axis. They can be excised but may recur. CONJUNCTIVAL TUMOURS These are rare. They include: 1) Squamous cell carcinoma. An irregular raised area of conjunctiva which may invade the deeper tissues. 2) Malignant melanoma. The differential diagnosis from benign pigmented lesions (for example a naevus) may be difficult. Review is necessary to assess whether the lesion is increasing in size. Biopsy, to achieve a definitive diagnosis, may be required. DESEASES OF CORNEA The features of corneal disease are different and include the following: 1) Epithelial and stromal oedema may develop causing clouding of the cornea. 2) Cellular infiltrate in the stroma causing focal granular white spots. 3) Deposits of cells on the corneal endothelium (termed keratic precipitates or KPs, usually lymphocytes or macrophages). 4) Chronic keratitis may stimulate new blood vessels superficially, under the epithelium (pannus) or deeper in the stroma. Stromal oedema, which causes swelling and separates the collagen lamellae, facilitates vessel invasion. 5) Epithelial erosions are punctate or more extensive patches of epithelial loss which are best detected using fluorescein dye and viewed with a blue light. HERPES SIMPLEX KERATITIS Type 1 herpes simplex (HSV) is a common and important cause of ocular disease. Type 2 which causes genital disease may occasionally cause keratitis and infantile chorioretinitis. Primary infection by HSV1 is usually acquired early in life by close contact such as kissing. It is accompanied by: fever; vesicular lid lesions; follicular conjunctivitis; pre-auricular lymphadenopathy; most are asymptomatic. The cornea may not be involved although punctate epithelial damage may be seen. Recurrent infection results from activation of the virus lying latent in the trigeminal ganglion of the fifth cranial nerve.There may be no past clinical history. The virus travels in the nerve to the eye. It is characterized by the appearance of dendritic ulcers on the cornea. These usually heal without a scar. If the stroma is also involved oedema develops causing a loss of corneal transparency. Involvement of the stroma may lead to permanent scarring. If corneal scarring is severe a corneal graft may be required to restore vision. Uveitis and glaucoma may accompany the disease. Disciform keratitis is an immunogenic reaction to herpes antigen in the stroma and presents as stromal clouding without ulceration, often associated with iritis. Dendritic lesions are treated with topical antivirals which typically heal within 2 weeks. Topical steroids must not be given to patients with a dendritic ulcer since they may cause extensive corneal ulceration. HERPES ZOSTER OPHTHALMICUS This is caused by the varicella-zoster virus which is responsible for chickenpox. The ophthalmic division of the trigeminal nerve is affected. Unlike herpes simplex infection there is usually a prodromal period with the patient systemically unwell. Ocular manifestations are usually preceded by the appearance of vesicles in the distribution of the ophthalmic division of the trigeminal nerve. Ocular problems are more likely if the naso-ciliary branch of the nerve is involved (vesicles at the root of the nose). Signs include: lid swelling (which may be bilateral); keratitis; iritis; secondary glaucoma. Reactivation of the disease is often linked to unrelated systemic illness. Oral antiviral treatment (e.g. aciclovir and famciclovir) is effective in reducing post-infective neuralgia (a severe chronic pain in the area of the rash) if given within 3 days of the skin vesicles erupting. Ocular disease may require treatment with topical antivirals and steroids. The prognosis of herpetic eye disease has improved since antiviral treatment became available. Both simplex and zoster cause anaesthesia of the cornea. Non-healing indolent ulcers may be seen following simplex infection and are difficult to treat. BACTERIAL KERATITIS PATHOGENESIS A host of bacteria may infect the cornea. Some are found on the lid margin as part of the normal flora. The conjunctiva and cornea are protected against infection by: blinking; washing away of debris by the flow of tears; entrapment of foreign particles by mucus; the antibacterial properties of the tears; the barrier function of the corneal epithelium (Neisseria gonnorrhoea is the only organism that can penetrate the intact epithelium). Predisposing causes of bacterial keratitis include: keratoconjunctivitis sicca (dry eye); a breach in the corneal epithelium (e.g. following trauma); contact lens wear; prolonged use of topical steroids. SYMPTOMS AND SIGNS: pain, usually severe unless the cornea is anaesthetic; purulent discharge; ciliary injection; visual impairment (severe if the visual axis is involved); hypopyon sometimes (a mass of white cells collected in the anterior chamber; a white corneal opacity which can often be seen with the naked eye. TREATMENT Scrapes are taken from the base of the ulcer for Gram staining and culture. The patient is then treated with intensive topical antibiotics often with dual therapy cefuroxime against Gram + bacteria and gentamicin for Gram - bacteria) to cover most organisms.The drops are given hourly day and night for the first couple of days and reduced in frequency as clinical improvement occurs. EPISCLERITIS This inflammation of the superficial layer of the sclera causes mild discomfort. It is rarely associated with systemic disease. It is usually self-limiting but as symptoms are tiresome, topical anti-inflammatory treatment can be given. In rare, severe disease, systemic non-steroidal anti-inflammatory treatment may be helpful. SCLERITIS This is a more severe condition than episcleritis and may be associated with the collagen-vascular diseases, most commonly rheumatoid arthritis. It is a cause of intense ocular pain. Both inflammatory areas and ischaemic areas of the sclera may occur. Characteristically the affected sclera is swollen.The following may complicate the condition: scleral thinning (scleromalacia), sometimes with perforation; keratitis; uveitis; cataract formation; glaucoma. Treatment may require high doses of systemic steroids or in severe cases cytotoxic therapy and investigation to find any associated systemic disease. Scleritis affecting the posterior part of the globe may cause choroidal effusions or simulate a tumour. Thank You For Your Attention