plasmacytoma
advertisement
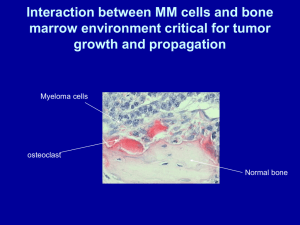
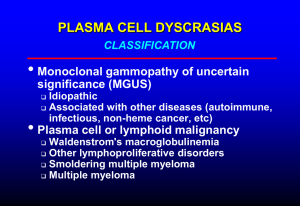
Show and Tell FIRM B - RED Our team • • • • Dr. Clarke & Dr. Vargas Shinoj & Arvind Jacob & Muneeza Chloe, Lauren & Njiye History 57 yo women presented with 3 day h/o - left sided chest pain. diffuse, pressure like, pleuritic, radiating to the back, 4/10 on pain scale and non exertional. - no shortness of breath PMH: unremarkable Labs • • • • BMP – unremarkable CBC – unremarkable EKG – normal Troponin - < 0.012 Imaging • Chest X ray: “ Mass noted in the left lateral upper lobe of the lung eroding into the fifth rib ”. • CT angiogram: “ Pleural-based mass in the posterior segment of the left upper lobe with bony erosions through the posterior fifth rib ” . D/D • Arising from the pleura - localized malignant mesothelioma, solitary fibrous pleural tumour. • Arising from lung parenchyma - adenocarcinoma • Arising from the bone - Fibrous dysplasia, Paget’s disease - Chondrosarcoma, Osteosarcoma - Multiple myeloma, Plasmacytoma Work up • Plan was to get a tissue diagnosis, possibly a bronchoscopy. • Pulmonary service were consulted • Pulmonary recs - most likely adenocarcinoma. - recommended IR guided biopsy as the mass is not accessible to bronch due to its location. Pathology report • IR guided biopsy was performed. • The biopsy result came back as “ PLASMACYTOMA ” Plasmacytoma • Plasmacytoma is a discrete, solitary mass of neoplastic monoclonal plasma cells. • Types Solitary bone plasmacytoma (SBP) Soft tissue or non-osseous extramedullary plasmacytoma (EMP) Pathophysiology • SBP : Arise from plasma cells of bone marrow EMP: From plasma cells of mucosal surfaces • SBP ~ 5% of plasma cell disorders EMP ~ 3% of plasma cell disorders • The median age of patients with SBP or EMP is 55 years. This median age is 10 years younger than patients with multiple myeloma. Presentation • The most common symptom - pain at the site of the skeletal lesion due to bone destruction by the infiltrating plasma cell tumor. • Vertebral involvement may also have evidence of nerve root or spinal cord compression. Labs • Serum electrophoresis reveals a monoclonal protein in the serum or urine in 24-72% of patients, although levels are lower than in multiple myeloma. • Uninvolved immunoglobulin levels are usually within the reference range. • Peripheral blood cell count, renal function, and calcium are within the reference range. Imaging and histology • Chest X ray: A lytic appearance with clear margins and a narrow zone of transition to healthy surrounding bone • MRI: abnormal signal intensity (low on T1weighted imaging and high on T2-weighted) • Histology: reveals infiltration of the bone by monoclonal plasma cells. SBP- Diagnostic criteria 1. Single area of bone destruction by clonal plasma cells 2. Bone marrow plasma cell infiltration not exceeding 5% of all nucleated cells. 3. Absence of osteolytic bone lesions or other tissue involvement (no e/o myeloma). 4. Absence of anaemia, hypercalcemia, or renal impairment attributable to myeloma. 5. Low, if present, concentrations of serum or urine monoclonal protein. 6. Preserved levels of uninvolved immunoglobulins Treatment • • • • • Local radiotherapy is the treatment of choice. Local control achieved in 88-100% of patients. All patients have major symptom relief. Local tumor recurrence rate of apprx 10%. Monoclonal protein is markedly reduced after radiotherapy in the majority of patients, but protein disappearance is observed in only 2050% of patients. Role of surgery & chemotherapy • Surgery is contraindicated in the absence of structural instability or neurologic compromise • Chemotherapy may be considered for patients not responding to radiation therapy. Regimens useful in multiple myeloma can be considered. • No role exists for adjuvant chemotherapy in solitary bone plasmacytoma. Prognosis Solitary bone plasmacytoma (SBP) progresses to multiple myeloma at a rate of 65-84% at 10 years and 65-100% at 15 years. The median onset of conversion to multiple myeloma is 2-5 years with a 10-year disease-free survival rate of 15-46%. The overall median survival time is 10 years. Treatment failure • 3 patterns of treatment failure described : 1> development of multiple myeloma (54%) 2> local recurrence (11%), and 3> development of new bone lesions in the absence of multiple myeloma (2%). Prognostic factors for conversion • Lesion size of at least 5 cm • High M protein levels • Persistence of M protein after treatment • Elevated B2 microglobulin • Spine lesions • In a study by Wilder et al, 10-year myelomafree survival was 91% versus 29% in patients whose M-protein did or did not resolve at 1 year following radiation therapy. Role of b2 microglobulin Southwest oncology group study • Beta 2 microglobulin is used as a prognostic marker in multiple myeloma. • 322 patients with pretreatment serum b2m values of less than 6 mcg/mL, median survival was 36 months. • 225 patients with a b2m level of greater than or equal to 6 mcg/mL, median survival of 23 months (P less than .0001). Back to my patient • Skeletal survey: no lytic lesions. • Serum immunofixation: normal • Urine immunofixation: small monoclonal spike of IgG kappa light chains • Normal renal function. • No anaemia, hypercalcemia. • Scheduled for bone marrow biopsy next week. If bone marrow shows less than 5% plasma cells – Plasmacytoma. • Radiation therapy is the next step. • Finally, close follow up to look for progression to multiple myeloma…………at my GMC !!! Thank u !