Intermittent Claudication
advertisement

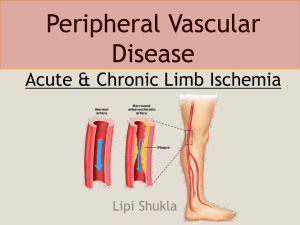
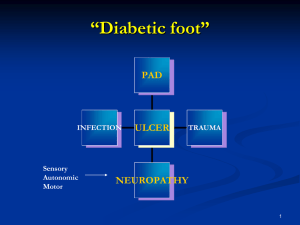
Peripheral Vascular Disease Review For The General Surgeon Elizabeth Pensler, DO Vascular Surgery Kansas City Review April 3-5th 2014 Peripheral Vascular Disease • A disorder that compromise blood flow to the limbs • The prevalence of PVD increases with age – 3% in persons younger than 60 years – More than 20% in person 75 years or older • Long term survival is reduced in pts with PVD – Risk of death 2 – 4 fold (due to MI, CVA) – Pts with claudication have a 10 year survival of 50% – Pts with critical limb ischemic have 10 years survival of 25% Risk Factors • The risk factors are similar to those that cause CAD • These include : – Cigarette smoking – Diabetes – Dyslipidemia – HTN – Hyperhomocytinemia – Family History Risk Factors Cigarette Smoking: – Developing intermittent claudication 2 – 5 fold higher in smokers than non-smokers – Continued smoking : increases the risk of progression from stable claudication to severe limb ischemia and amputation. – (2 – 4% of pts with claudication develop critical ischemia vs. 4 – 6 % in smokers) Risk Factors Diabetes – Diabetes is associated with 3 – 4 fold increase developing PVD – Infrapopliteal – Prognosis is poor for diabetics who with claudication; 30 – 40 % will develop critical limb ischemia in 6 years (vs 10 –20 years of non-diabetics) Risk Factors Dyslipidemia – Hypercholesterolemia in 40% of pts with PVD – Hypertriglyceridemia – HTN: increases risk of claudication 2 folds in man and 4 folds in women. – Hyperhomocystinemia: increases risk of PVD by 2 fold. Claudication • Latin claudicare “to limp” • Ischemic pain lower legs when walking • Inadequate blood flow leg muscles from atherosclerotic narrowing of the arteries • Annual incidence is 20 per 1,000 in persons older than 65 years. Claudication - Evaluation History • Acuteness of symptom onset • Ambulating distance before onset of pain • Whether pain is relieved by standing Physical Exam • quality of femoral, popliteal, dorslis pedis pulses • signs of arterial insufficiency - coolness, scaling, paleness (especially with leg elevation), or ulcer • ankle-brachial index (ABI) Clevland Clinic J of Med, 1997; 64:429-436 Clinical Presentation • Intermittent Claudication: • Discomfort, pain, fatigue or heaviness that is felt in the affected extremity during walking and resolved at resting. • The location of the symptoms depend on the site of stenosis – Thigh, hip or buttock claudication (and impotence) develops with proximal occlusions – aorta or iliac arteries – Calf claudication develops with femoral and popliteal arteries occlusions. – Pedal Claudication – tibial and peroneal stenoses • Rest Pain : – Pain typically in the toes and foot – initially worse at night with persistent severe ischemia – Skin breakdown occurs, leading to ulcerations, necrosis and gangrene Ischemia in Right Foot Intermittent Claudication Clinical Features • Symptoms always exertional • Muscular discomfort: Fatigue, aching, cramping • Reproducible distance • Relief by standing still (minutes) • Location of discomfort aids in localizing disease • Diagnosis – pre / post – exercise ABI Intermittent Claudication Differential Diagnosis Onset Claudication Walking Pseudoclaudication Standing & Walking Character Cramp, Pain “Parasthetic” Bilateral +/- + Walking Distance Minor Variable Cause Fairly Constant PVO Relief Standing still Sit down, lean forward Spinal stenosis PVD-Tests • ABI • Segmental B.P. measurement to assess the presence and severity of PVD • Pulse volume recording (Plethysmography) • Duplex ultrasonography • MRI • Angiography Ankle: Brachial Index (ABI) Supine systolic BP: Ankle / Brachial – Normal ABI 1.0 – Medial calcinosis (incompressability) falsely elevate ankle pressure – Low ABI (<0.9) associated increased risk for • Stroke • Cardiovascular death • All cause mortality Ankle: Brachial Index (ABI) Disease Severity ABI (rest) None > 1.0 Minimal 0.9 – 1.0 Mild (claudication) < 0.9 Moderate (claudication) 0.5 – 0.8 Severe (ischemia at rest) < 0.5 Intermittent Claudication 5 Years Outcome • Mortality 29% • Claudication improves or stable 55% • Amputation 4% Anm Vasc. Surg evt 3: 273, 1989. Claudication - Natural History • Symptoms remain stable or improve with time 65% 70% due to development of collateral vessels. • < 25% ever need surgery or angioplasty. • Low risk of losing a limb - only 1.4% per year progress to critical life-threatening ischemia • Diabetes increased overall amputation risk of 20% Intermittent Claudication Increased Risk of Limb Loss • • • • • Tobacco use Diabetes mellitus Ischemic rest pain Ischemic ulceration Gangrene Intermittent Claudication Initial Management • Aggressive modification of risk factors – Tobacco, diabetes, HTN, lipids • Diagnosis and treatment of associated – CAD (prevalence > 50%) – Carotid artery disease • Foot care and protection • Weight reduction (if obese) • Walking program TASC II Recommendations for Lipid Control in Patients with Peripheral Arterial Disease Patient Characteristics Recommendation Symptomatic PAD PAD and CAD Asymptomatic PAD and no other clinical evidence of cardiovascular diseaseLower All symptomatic PAD LDL <100 mg/dL LDL<70 mg/dL <100 mg/dL PAD and abnormal lipid fractions Consider fibrates, niacin, or both to raise HDL levels and lower triglyceride levels Dietary modification Statins—primary agents to lower Hypertension • Associated with a 2-3X risk of PAD • RF for stroke, CAD, CHF and CRF • < 140/90 mm Hg in high-risk groups (PAD) • < 130/80 mm Hg diabetes or renainsufficiency • Normotensive state • Multiple agents for control Effect of Diabetes Mellitus • Amputation value (cumulative risk 25 years) – IDDM 11.2% – NIDDM 11.0% • 12 – fold increase risk: BKA • 400 – fold increase risk: transphalangeal amputation • Account for 60% of amputations in a community Intermittent Claudication Outcome After 5 Years (Quitting Smoking) Continued (%) Stopped (%) Mortality 27 12 Major Amputation 11 0 Claudication Stable 40 56 Ann Vasc Surgery 3:273, 1989 Intermittent Claudication Pharmacologic Therapy • Antiplatelet therapy – Aspirin • Reduces risk of amputation • Reduces ischemic events • Reduces risk for revascularizaton – Clopidogrel • 8.71% relative risk reduction compared to aspirin. Pharmacotherapy for Claudication FDA Approved Drugs: • Pentoxifylline • Cilostazol There is inadequate evidence of clinical efficacy or a therapeutic role for: L-arginine, propionyl-L-carnitine, gingko biloba, oral prostaglandins, vitamin E, or chelation therapy. Effect of Cilostazol on Walking Distance in Patients With Claudication * 260 * 240 * 220 * Meters (mean) 200 * * 180 160 * * * * 140 * 120 * 100 * 80 * * * * * * * Maximal Walking Distance Cilostazol 100 mg bid (n=140) Cilostazol 50 mg bid (n=139) Placebo (n=140) Pain-Free Walking Distance * P < 0.05 vs. placebo 60 0 4 8 12 16 20 Weeks of Treatment 24 Beebe, et al. Arch Internal Medicine. 1999;159:2041-50. Cilostazol vs. Pentoxifylline: Relative Efficacy to Improve Walking Distance in Claudication Cilostazol 100 mg 2 times/day (n=227) Pentoxifylline 400 mg 3 times/day (n=232) Placebo (n=239) Percentage Change From Baseline MWD (mean) 50 40 * 30 20 10 0 0 4 8 12 16 Treatment (weeks) 20 24 MWD=maximal walking distance. *P<0.001 vs pentoxifylline. Reprinted from Dawson DL, et al. Am J Med. 2000;109:523-530 with permission from Elsevier. Pharmacotherapy of Claudication I IIa IIb III Cilostazol (100 mg orally two times per day) is indicated as an effective therapy to improve symptoms and increase walking distance in patients with lower extremity PAD and intermittent claudication (in the absence of heart failure). Intermittent Claudication: Exercise Therapy (Supervised) • Frequency: 3–5 supervised sessions/week • Duration: 35–50 minutes of exercise/session • Type of exercise: treadmill or track walking to near-maximal claudication pain • Length: 6 months • Results: 100%–150% improvement in maximal walking distance and associated improvement in quality-of-life Stewart KJ et al. N Eng J Med. 2002;347:1941-1951. SURGICAL AND INTERVENTIONAL TREATMENT OPTIONS Arterial reconstructions Endarterectomy Patch angioplasty Bypass (autologous vein graft, prosthetic graft) Endovascular techniques Thrombectomy Atherectomy Balloon angioplasty Stent placement Endograft (covered stent) Indications for Revascularization • Elective – Disabling (life style limiting) symptoms • Indication to the physician – Diabetes with significant disease – Ischemic foot pain – Ischemic ulceration – Gangrene Percutaneous Transluminal Angioplasty • Peripheral arteries – – – – Mortality 0.5% Mobility 1 – 3 days initial good results > 80% (iliac) 2 – 3 years good results > 70% • Best results in – Short, partial occlusions – Proximal disease – Good distal run – off Clinical Variables Favoring Vascular Surgery • • • • • Long, diffusely stenotic, eccentric lesions Long occlusions Stenoses adjacent to aneurysms Tibial occlusive lesions Lesions causing atheromatous embolism • Vein is best