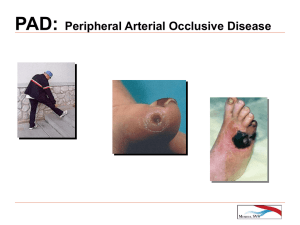
Peripheral Vascular Disease
advertisement

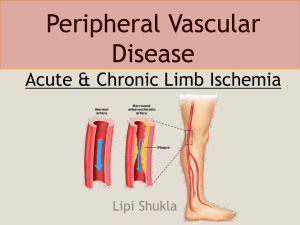
Peripheral Vascular Disease Principles and Practice Risk Factors • • • • • • • • • • Hypercholesterolemia Cigarette Smoking Hypertension Diabetes Advanced Age Male gender Hypertriglyceridemia Hyperhomocysteinemia Sedentary Lifestyle Family History Risk Factor Modification • • • • • Lipid Management Weight Management Smoking Cessation Blood Pressure Control Physical Activity Pathology of Atherogenesis • “Response to Injury” Theory Alteration in endothelial cell layer which may be toxic, mechanical, hypoxic, or infectious • Early plaque formation can be seen in second and third decades of life as lipid streaking • Arterial enlargement • Anatomic distribution Constant at areas of bifurcation Classification of Limb Ischemia • Functional • Normal blood flow at rest, but cannot be increased in response to exercise – Claudication • Three main clinical features Pain is always experienced in functional muscle unit It is reproducibly precipitated by a consistent amount of exercise Symptoms are promptly relieved by stopping the exercise Classification of Limb Ischemia • Chronic critical limb ischemia Recurring ischemic pain at rest that persists for more than 2 weeks and requires regular analgesics with an ankle systolic pressure of 50 mm Hg or less Ulceration or gangrene of the foot or toes Classification of Limb Ischemia • It is IMPORTANT to differentiate these types of patients because • Patients with claudication can be treated initially without surgery – Exercise program, Risk reduction • Patients with rest pain, gangrene, or ulceration are candidates for revascularization Chronic Occlusive Lower Extremity Disease • Patients with claudication • Have low risk of limb loss – Annual risk of mortality and limb loss – 5% and 1% • More than half of patients will improve or symptoms remain stable • 20 – 30% undergo surgery for progression of symptoms Chronic Occlusive Lower Extremity Disease • Patients with critical ischemia – rest pain, gangrene, or tissue breakdown are at high risk for limb loss • Patients should undergo angiographic evaluation for potential revascularization Aortoiliac Occlusive Disease • Often present with complaints of buttock, hip, or thigh claudication • In men, impotence may be present in 30-50% of patients • Only a small percent (10%) of patients have disease confined to just the distal aorta and common iliac segments • 90 % of patients will have more diffuse disease involving external iliac and/or femoral vessels Aortoiliac Occlusive Disease • Noninvasive Vascular Studies • Help to improve diagnostic accuracy • Physiologic quantification of severity of disease • May serve as baseline for follow-up • Angiography for patients with limb threatening ischemia Aotoiliac Occlusive Disease Surgical Treatment • Aortobifemoral Bypass • Cross Femoral Bypass – Fem-Fem bypass • Axillofemoral Bypass • Percutaneous Angioplasty Femoral-Popliteal-Tibial Occlusive Disease Surgical Treatment • Femoral – Popliteal Bypass Above Knee or Below Knee Bypass • Femoral – Tibial Bypass Anterior, Posterior tibial or Peroneal • Femoral – Dorsalis Pedis Bypass • Bypass Conduits and Technique Nonautogenous vs. Vein grafts Carotid Artery Occlusive Disease • Symptoms TIA CVA Amaurosis Fugax Resolving Neurologic Deficits • NOT Symptoms Dizziness Vertigo Memory Loss Light Headedness Carotid Artery Occlusive Disease • Imaging Studies Carotid Duplex Ultrasound Angiography CT Scan MRI/MRA Carotid Artery Occlusive Disease Surgical Indications • Symptomatic Carotid Stenosis > 50% in patients with ipsilateral TIA, Amaurosis, or RND Patients with lesser degrees of stenosis can be considered for operation if they have failed medical therapy, large ulcerations or contralateral occlusion • Asymptomatic Indications less clear but generally reserved for patients with 60-99% Stenosis Abdominal Aortic Aneurysm • Natural History Enlarge and rupture Embolization A-V Fistula GI Fistula Abdominal Aortic Aneurysm • Following rupture of AAA Only 50% of patients arrive at the hospital alive 24% die before operation 42% die in the post operative period Overall mortality of 70-95% Abdominal Aortic Aneurysm • Most important risk factor for rupture is maximal transverse diameter AAA < 5 cm – 1-3% per year AAA 5-7 cm – 6-11% per year AAA > 7 cm – 20 % per year • Symptomatic AAA are at increased risk of rupture as well Abdominal Aortic Aneurysm • Diagnosis Ultrasound CT Scan MRI Arteriography Abdominal Aortic Aneurysm • Selection of patients for repair Maximal diameter 5 cms. • Types of repair Open repair vs. Endovascular