Ocular Trauma
advertisement

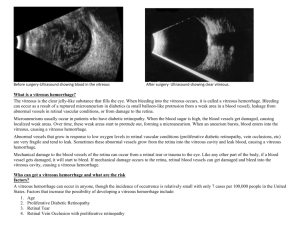
Ocular Trauma Sarah Welch Vitreoretinal Surgeon Eye Dept GLCC; Auckland Eye March 2011 Treatment of Penetrating Injury Exclude life threatening injuries CT to find any IOFB Repair lids Repair globe Restore normal anatomy Remove any tissue protruding from the wound +/- lens removal +/- vitrectomy Fundus Trauma Mechanisms of injury Direct via sclera Via vitreous Shearing via globe deformation Contrecoup Injury occurs at interface with greatest density difference - at lens and photoreceptor I/faces Commotio retinae - damage to photoreceptors May be permanent vision loss RPE may be hyperpigmented or atrophic No intra- or extracellular oedema or FFA leakage 5 types of retinal breaks Dialysis Horseshoe Operculated hole Macular hole Necrosis of retina QuickTime™ and a decompressor are needed to see this picture. Retinal dialysis Superonasal or inferotemporal Smooth, thin and transparent Commonly have cysts, 1/2 have demarcation lines May be associated with avulsion of vitreous base PVR is rare Should have cryo or laser, good reponse to buckling Detachments can present later 10% immediately, 30% 1 month, 50% 8 months, 80% 2 years Vitreous tamponades until starts to liquify Other holes Treat if detached Treat macular holes Retinal necrosis usually associated with choroid injury so tends to scar Choroidal rupture Bruch’s membrane often tears At point of contact or at posterior pole Clinically looks like subretinal hx May dissect into vitreous Becomes white crescent-shaped area with RPE atrophy Should follow pt for risk of CNV Scleral injury Scleroptia Scleral rupture claw-like fibroglial scar assoc with indirect concussive injury Suspect if APD, poor motility, marked chemosis, vitreous hx Also, deep ac, low IOP (though can be normal) Common sites Limbus, beneath recti, surgical scars Is the globe open? Poor VA Haemorrhagic chemosis IOP<5mmHg Abnormally shallow or deep ac Pupil peaking Choroidal detacjment Vitreous hx Ruptured globe 1st exam may be only opportunity Poor VA, APD, wound>10mm, wound extending behind recti, vitreous hx Goals of management 1. 2. 3. Identify extent - 360˚ peritomy Rule out FB - consider CT Close wound with limited reconstruction • 4. 5. Reposit uvea, cut vitreous Infection prophylaxis - IV Protect the other eye • Injury and sympathetic Preoperative management Protect globe Prevent infection Shield Drops + systemic Tetanus May consider leaving small (<2mm) self-sealing wounds in cooperative adults Seal - patch, CL, tissue adhesives Infection - abx Prep for surgery can wait until next day unless: IOFB If <24h, remove ASAP VR consult if post IOFBs Endophthalmitis Ret det Inexperienced surgeon Anaesthesia 10% risk of endophthalmitis Inert mat’ls may be tolerated, esp if present 7al days GA Succinylcholine causes prolonged spasm of EOM Consent for enucleation? Foreign bodies Detection Indirect is best method CT next best, including plastic and glass MRI better for organic US supplements CT and gives info on retina Plain films if no CT Foreign bodies Immediate removal if endophthalmitis or toxic material Toxicity related to redox potential Cu (chalcosis) and Fe (siderosis) have low potential and dissolve Pure>alloy Other metals, nonmetallic substances tend to be inert Wound repair Principles Prep normally with no pressure on globe Evaluate extent Try and restore normal anatomy Watertight closure If beyond limbus - peritomy Bury knots Then remove IOFB treat endophthalmitis manage lens and post segment trauma Further management Vision/scar Retina Contact lenses Remove selected sutures at 1 month Amblyopia in children PK - await at least 6 months 7-14d later Sympathetic ophthalmia 0.19% 5d to decades later, mostly 2/52 to 1 yr Warn patient about symptoms If severe and NPL, consider removal within 2/52 Post-operative management Control infection, inflammation, IOP Minimise scarring Admit Shield Abx Oral ciprofloxacin Topical Steroid - topical or systemic if severe inflammation Cycloplegics Siderosis bulbi Tends to deposit in epithelial tissues Iris - heterochromia, mid-dilated, poorlyreactive pupil Lens - brown dots and cortical yellowing Retina -pigmentary degeneration + bv sclerosis ERG - flat within 100 days Used to monitor QuickTime™ and a decompressor are needed to see this picture. Chalcosis <85% pure - chalcosis, >85% - sterile endophthalmitis Copper deposits in basement membranes DM - Kayser-Fleischer ring Iris - sluggish, greenish hue ac capsule - sunflower cataract Vireous opacification ERG like siderosis Improves if Cu removed QuickTime™ and a decompressor are needed to see this picture. Post traumatic endophthalmitis 7% of cases Skin flora most likely cause Consider Bacillus cereus if any soil S aureus 8-25% Prophylactic antibiotics Consider intravitreal if heavily contaminated IV for 3-5d post-op Traumatic infection not covered by EVS Topical also Sympathetic ophthalmia <0.5% of penetrating injury Bilateral granulomatous uveitis ac inflammation, multiple yellow spots in peripheral fundus Complications Cataract, glaucoma, optic atrophy, exudative detachments, subretinal fibrosis 80% within 3 months, 90% within 1 year Systemic immunosuppression Mostly good prognosis >6/18 However, enucleate only if no visual potential Other trauma Purtscher’s retinopathy Abuse - shaken baby syndrome 40% of abused children have ocular findings Ophthalmologist 1st to find in 6% Commotio Optic Neuropathy QuickTime™ and a decompressor are needed to see this picture. QuickTime™ and a decompressor are needed to see this picture. Chemical Injury Assessment History Type of chemical Alkali/acid Examination Four grades I - IV Based on corneal clarity Clear - cloudy = good - poor prognosis Grade I QuickTime™ and a decompressor are needed to see this picture. • • Clear cornea Limbal ischaemia - nil Grade II • Cornea hazy but visible iris details • Limbal ischaemia < 1/3 Grade III • No iris details • Limbal ischaemia - 1/3 to 1/2 Grade IV • Opaque cornea • Limbal ischaemia > 1/2 Medical Treatment of Severe Injuries 1. Copious irrigation ( 15-30 min ) • to restore normal pH 2. Topical steroids ( first 7-10 days ) • to reduce inflammation 3. Topical and systemic ascorbic acid • to enhance collagen production 4. Topical citric acid • to inhibit neutrophil activity 5. Topical and systemic tetracycline • to inhibit collagenase and neutrophil activity • Nexagon Complications Symblepharon lid deformities Keratoprosthesis Thank you for listening!