Clostridium Difficile
advertisement
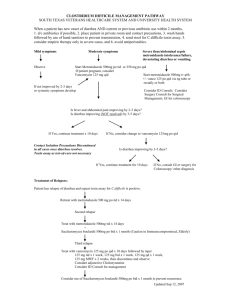
Antibiotic Associated Diarrhea The new and improved C diff: an emerging ‘superbug’?? Neil Stollman MD, FACP, FACG Associate Clinical Professor of Medicine University of California San Francisco East Bay Center for Digestive Health Oakland California Antibiotic-Associated Diarrhea (AAD) • Estimated that 10-20% of all hospitalized patients treated with antibiotics will develop diarrhea • Most frequently implicated antibiotics include penicillin, clindamycin, and cephalosporins • Only 15-20% of AAD is due to C. difficile • Prolonged use of antibiotics alters colonic flora, especially fecal anaerobes which normally metabolize malabsorbed carbohydrates and break down primary bile acids; this can result in osmotic (carbohydrate) or secretory (bile acid) diarrhea Antibiotic Associated- Diarrhea • Diarrhea predominantly mild, 3-4 four loose stools per day • Usually relieved with fasting • Fever, pain, elev WBC usually mild or absent • Fecal leukocytes and C. difficile assays usually negative • Diarrhea usually subsides with discontinuation of antibiotics Can we prevent AAD? • 89 hosp pts receiving Abx randomized to: – Lactobacilli-enriched yogurt vs placebo – AAD= >2 liquid stools/24h • AAD • LOS • C diff Yogurt 17.1% 8 days “fewer cases” Beausoleil M et al. AJG 2004;99:S234 (abstract) Placebo 37.2% 10 days (stat sig) Prevention of AAD: Probiotics • Meta-analysis of 31 RCT 1977-2005 • RR=0.43 (0.31-0.58) for AAD • Two types effective for prevention: – Saccharomyces boulardii – Lactobacullus GG • Only S boulardii prevented confirmed C diff infections McFarland LV. Am J Gastro 2006;101:812-822 Clostridium Difficile • Anaerobic, gram-positive, spore-forming bacillus, termed “difficult clostridium” because of resistance to growth in conventional medium • 1935: found in fecal flora of 50% of healthy infants • 1978: identified as a cause of antibiotic associated diarrhea and pseudomembranous colitis • 1980’s: leading cause of nosocomial diarrhea in US C Difficile: Pathophysiology • Infection requires the alteration of the normal bacterial flora, usually by antibiotics • All antibiotic have been associated with C. diff. infection, but clindamycin, PCNs most commonly in past, now flouroquinolones • 75% of strains of CD produce two protein cytotoxins, A and B, which bind to colonic brush border, causing mucosal PMN infiltration, colonic secretion and shedding and necrosis, resulting in colitis and diarrhea C Difficile: Transmission • Transmission of C diff is fecal-oral • Spores can survive for days outside of the body and are resistant to common hospital disinfectants • 50% of rooms of C diff (+) pts have culture-positive fomites (bedpans, toilets, scales, furniture) • Hospital personnel account for the great majority of person-to-person hospital transmission • Careful hand-washing and use of vinyl gloves demonstrated to reduce spread of infection; alcohol based foams inadequate. C Difficile: Epidemiology • Found in normal colonic flora of 2-5% of healthy adults and up to 70% of neonates • Approximately 20-40% of patients hospitalized for more than 2 days become colonized with C diff – Only 1/3 develop symptoms • >3 million new cases of C diff diarrhea or colitis in US hospitals each year • <20,000 infections / year acquired outside of hospital C Difficile: Risk Factors • Canadian cohort study 2002-2003 • 1187 hospital pts prescribed Abx for >3d • C diff diarrhea: – Medical wards: 10.9% (OR 4.1) – Surgical wards: 2.9% – > 3 Abx: 12.1% (OR 2.1) – 1-2 Abx: 5.1% Dial S. CMAJ 2004;171:33 Acid Suppression: New Risk Factor? • UK case:control studies (2) 1994-2004 • 1672 cases c diff matched to 10 controls • Incidence: 1/100,000 (1994) →22/100,000 (2004) • Adjusted Rate Ratios: – Current PPI use: – Current H2RA use: – Current NSAID use: Dial S et al. JAMA 2005;294:2989 2.9 (2.4-3.4) 2.0 (1.6-2.7) 1.3 (1.2-1.5) C diff: New epidemiology? • • • • • • CDC investigation in 4 states 2005 23 community-acquired c diff cases 10 peripartum cases 4 involved transmission to close contacts No Abx exposure in 24% “Certain features….close-contact transmission, young age, lack of Abx exposure….reflect changing epidemiology” MMWR 2005;54:1201-1205 Peripartum Cases? • • • • • • • • • Survey by CDC of ID clinics of CDAD in pregnancy 10 ‘severe’ cases identified 9/10 had Abx use 6/10 pre-delivery, 3/10 w/in 1 wk delivery, 1/10 w/in 4 wks WBC 11-72K 6/10 in ICU, 6/10 toxic megacolon, 5/10 required colectomy 3/10 stillborn infants 3/10 patient died CDC: “Severe CDAD may be increasing in peripartum women” Rouphael NG et al. AJOG 2008; 198:635-637 C diff: Epidemics? • Epidemic of C diff with increased morbidity and mortality in Quebec recently • Epidemic strain: toxinotype III (BI/NAP1) carrying binary toxin gene cdtB (negative regulator toxins A/B) – 67% of those with health-care-associated disease – 37% of those with community-acquired disease – Median toxin A and toxin B concentrations were 16 and 23 times higher, than isolates representing 12 different non-epidemic types Warny, M. Lancet 2005;366:1079 More data from Canada… • 1703 patients in Quebec (2004) • Incidence: 22/1000 admissions • 84% + for binary toxin and tcdC deletion – Attributable mortality: 6.9% – Urgent colectomy: 1.9% – Mortality >90 years: 14% – Quinolone use: 52% Loo VG. NEJM 2005;353:2442. And not to be left out…. • 8 US facilities (2000-2004) • 187 new isolates c/w 6000 control strains New Cases • Binary Toxin (III) 51% • Quinolone Resistance 100% McDonald LC. NEJM 2005;353:2433 Controls 17% 42% C difficile: Diagnosis • Cytotoxin Assay – Requires >48h, and tissue culture facility – Specificity >99%, Sensitivity only 85% – Detects only toxin B • Immunoassay for toxin A or A&B – Simple, cheap, available in 4 hours – Specificity >95%, Sensitivity 75% • Culture / toxin typing – Requires 96 hours and tissue culture facility – Specificity > 98%, Sensitivity > 90% – Required for outbreak typing / analysis C Difficile: Endoscopy • Sigmoidoscopy/colonoscopy are not necessary for patients with classic symptoms and a positive assay • Indicated when a rapid diagnosis needed, and no stool available due to ileus, or to rule out other confounding diseases (i.e. ischemic colitis) • Pseudomembranes virtually diagnostic of CD colitis • Colonoscopy superior to sigmoidoscopy in detecting pseudomembranes (10% right sided only) • Invasive, increased risk perforation in toxic megacolon Pseudomembranous Colitis C Difficile: Clinical Manifestations • Asymptomatic carriage (60-65%) • Antibiotic-associate diarrhea (without colitis) • Antibiotic-associated colitis (without pseudomembranes) • Pseudomembranous colitis • Fulminant colitis / Toxic megacolon (2-3%) • Relapsing infection (15-20%) C Difficile: Asymptomatic Carriers • 2/3 of infected hospital patients remain asymptomatic • Can shed toxigenic organisms and act as reservoir for continued contamination • High levels of serum IgG Abs to Toxin A appear to be protective against development of diarrhea • Treatment of asymptomatic carriers is not recommended except during epidemic hospital outbreaks Diarrhea/Colitis/Pseudomembranes • More serious with systemic manifestations – – – – Profuse, watery diarrhea 5-15/day Abdominal pain / nausea / malaise Fever and leukocytosis common Treatment clearly indicated • Fulminant: acidosis, dehydration, WBC 30K+ – ICU, CT scan, hydration, surgery consult, ? Abx – Monitor for perforation, megacolon – Ultimate treatment: subtotal colectomy C Difficile: Treatment • Supportive measures – Correct electrolytes – Hydration • Antiperistaltic agents (narcotics, Imodium) are acceptable for mild diarrhea, but are to be avoided in patients with evidence of active colitis (bloody diarrhea, fecal leukocytes, systemic toxicity) due to risk of toxic megacolon. • If patient responding to Rx, no need to retest stool C Difficile Colitis: Treatment • Stopping Abx alone is effective in 15-25% (mild dz) • Vancomycin and metronidazole are primary Abx • Prior prospective (non-blinded) trials have shown no difference in efficacy b/w them (93-97%) • Oral metronidazole 250-500 mg QID or 500-750 TID for 7-10 days is preferred initial treatment ($) • IV metronidazole 500-750 mg TID OK if NPO • Vancomycin (125 mg QID) ($$$) for those who fail metronidazole, or severe, life-threatening disease • Intravenous vancomycin does not achieve bactericidal levels in the gut and should not be used Vanco >> Flagyl? • DBRCT in 150 hospitalized patients • Flagyl 250 QID vs Vanco 125 QID x 10d Cure rates Mild dz: Severe dz: Recurrent dz: Vanco 98% 97% 7% Zar FA et al. Clin Infect Dis 2007;45:302 Flagyl 90% 76% 14% sig? ns 0.02 ns Relapsing C Difficile Diarrhea o • Approximately 15-20% of 1 infections relapse • Diarrhea usually recurs within 5 days; similar presentation, usually not progressive • After 2nd relapse, >50% recur • ? Reinfection or reactivation • ? Impaired host Ig immune response • Antibiotic resistance against vancomycin and metronidazole has not been described Relapsing C Difficile : Treatment • First Recurrence – Confirm diagnosis – Repeat 10-14 day course with metronidazole or vanco • Second Recurrence: Vancomycin Pulse / Taper – – – – – – 125 qid for 7 days 125 bid for 7 days 125 qd for 7 days 125 qod for 7 days 125 tiw for 7 days Consider adjunctive S Boulardii and/or cholestyramine McFarland LV et al. Am J Gastro 2002;97:1769 Relapsing C difficile: Bile Binders • Cholestyramine and colestipol have the potential to bind C diff toxins • Lancet 1978: reduced toxin titers & exposure time in C diff pts treated with bile binders • Most often used to treat recurrent CD • No new studies published in the last 25 years • Vancomycin is bound by cholestyramine so doses must be given three hours apart Relapsing C Difficile: Probiotics • Saccharomyces boulardii – Live, non-pathogenic yeast (Florastor®, 250mg) – Produces serine protease which digests toxins A and B and inhibits binding of toxin A to the colonic brush border (in animal models) • Prospective RCT: 60 patients with recurrent C diff – Saccharomyces 1 gm/d or placebo (plus Abx) X 4 wks – Recurrences: 35% vs 65% • Avoid in hospitalized, immunosuppressed; reports of fungemia McFarland LV et al. JAMA 1994;271:1913 Relapsing C Difficile: Probiotics • The ‘ultimate’ probiotic would be reconstitution of all fecal flora (since we don’t know which of the >400 are critical) • Stool transplantation from “healthy donors” • Can administer via NG tube, enemas or instill at colonoscopy • Reasonable uncontrolled data supports • Anecdote alert: Stollman/Surawicz 19-for-20 Relapsing C Difficile: Rifaxamin • Rifaxamin – rifampin derivative, approved for traveler’s diarrhea prevention. Not systemically absorbed. • 400 mg BID day x 2 weeks immediately after 2 week vanco course in multiple recurrence population. • “Chaser” Rx successful in 7/8 (1/8 with resistance) Johnson S et al. Clin Infect Dis 2007;44:846 Relapsing C Difficile: IVIg • Failure to mount an immunoglobulin response to CD is associated with risk of recurrent disease • 50% of population has detectable serum anti-toxin, which neutralizes toxin • 9 case reports in the literature (4 adults, 5 children) successfully cured of multiple bouts of recurrent CD by immunoglobulin infusions • Dose: 400 mg/kg repeated in 21 days with a vancomycin taper • Two case reports of success with Ig infusion for severe, acute, refractory CD colitis in adults Gut 1997;41:366-70 Relapsing C Difficile: MAbs? “Treatment with Monoclonal Antibodies against Clostridium difficile Toxins” • RDBPCT in 200 patients with symptomatic Clostridium difficile infection • Treatment with single infusion of two monoclonal antibodies against C. difficile toxins A and B or placebo, in addition to metronidazole or vancomycin • Outcome: lab documented recurrence within 3 months of infusion Lowy, I et al. N Engl J Med 2010; 362:197-205 Time to Recurrence of C difficile Infection Recurrence rates 7% vs 25% No diff in LOS or AEs Lowy I et al. N Engl J Med 2010;362:197-205 C Difficile: On the horizon… • Immune Support – Hyperimmune globulin (plasmapheresis of vaccinated donors) – HuMAbs, ? Utility for severe disease, ? prophylactically – Vaccines (in Phase II trials) • Therapeutics – – – – Tinidazole (Tindamax, available for amba, giardia, trichomoniasis) Nitazoxanide (Alinia, available for giardia, cryptosporidium) Rifalazil (under investigation) Tolevamer (binding resin, under investigation) C Difficile: Summary • The bug is changing: – risk in non-traditional (community, peripartum) pts – Increased morbidity, mortality, and chronicity – Epidemic strains w/ toxin production emerging – Flouroquinolone use likely important • We need to change: Increased monitoring, better infection control (gloves, isolation, handwashing) and more antibiotic restraint