Bez tytułu slajdu
advertisement

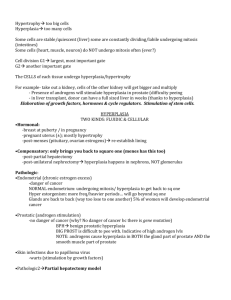
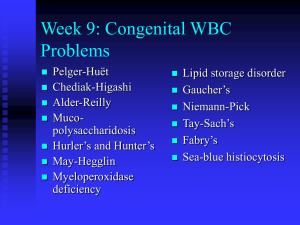
NON-NEOPLASTIC DISEASES OF HEMATOPOETIC ORGANS Pathology Jan Żeromski 20010/2011 PATHOLOGY OF THYMUS Developmental defects – aplasia (Di George anomaly), Nezelof syndrome Follicular hyperplasia with germinal center formation (myasthenia – in 70% of cases,SLE, Graves disease) Thymic tumors: 1. Thymomas - tumors of thymic epithelial cells - Benign-mostly of medullary epithelial cells - Malignant a) Type I - cytologically benign but biologically aggressive (mainly of cortical epthelial cells) b) Type II - „thymic carcinoma”- 5% of thymomas 2. Lymphomas ( of T cell) Hodgkin’ disease 3. Others ( carcinoids, teratomas etc.) PATHOLOGY OF LYMPH NODES (LN) Lack or hypoplasia of LN cortex - in immunodefic. Atrophy - in old age, after irradiation, chemotherapy Inflammations - acute, chronic, non-specific, specific Enlargement due to storage of various compounds Tumors: Primary - lymphomas Secondary - carcinomas (metastases) CHRONIC NON SPECIFIC LYMPHADENITIS Follicular hyperplasia: caused by infection with microbes activating B cells. Paracotical lymphoid hyperplasia: due to infection with microbes activating T cells. Sinus histiocytosis: accumulation of histiocytes in lymphatic sinusoids. Occurs in LNs draining cancers (of breast and/or stomach). Hyperplasia follicularis Hyperplasia follicularis CHRONIC „SPECIFIC’ LYMPHADENITIDES Toxoplasmosis: Small epithelioid cell granulomas, both T and B cell are involved. Cat scratch disease: (e.: small Gram neg. bacteria). Enlargement and suppuration of LN after skin inc ident such as cat scratch. Lymphogranuloma venereum: (e.: Chlamydia) Enlargement of LN, granuloma formation suppuration, liquefaction. Mesenteric lymphonodulitis: (e.: Yersinia pseudotuberculosa) - Granulomas with tendency to necrosis of mesenteric LNs. CHRONIC „SPECIFIC” LYMPHADENITIS 2 Tuberculosis: (e.: tubercle bacilli) Necrotic granulomas Tularemia: (e.: Francisella tularensis) Focal necrotic lesions in LN and other organs surrounded by monocytes, fibroblasts, lymphocytes as in tbc. Sarcoidosis: Granulomas formed by mononuclear phagocytes surrounded by a rim of T-helper cells and sometimes B lymphocytes. They are due to cytokine release by Th. Infectious mononucleosis: (e.EBV infection) Activation of T area, immunoblast infiltrates, dispersed light reticulum cells, sinuses widened with immunoblasts and plasma cells. Millary tuberculosis of the spleen Typical epithelioid cell tubercles with Langhans` giant cells. HE, 100x Tularemic lymphadenitis; margin of necrotic area No caseation, though there are scattered areas of necrosis. Note epithelioid cell zone with several Langhans` giant cells. Lymphadenitis due to tularemia (Pasteurella tularensis) Center: necrotic area surrounded by wide zone of epithelioid cells with a few Langhans` giant cells. At the upper boundary of the central wedgeshaped area of necrosis there is some nuclear debris. Diagnosis serologically confirmed. HE, 65x Sarcoidosis of hilar lymph nodes Epithelioid cell nodules without caseation; much fibrosis and abundant giant cells. Center: an “asteroid body”. HE, 100x OTHER LYMPHADENOPATHIES Post vaccinal and viral lymphadenitis LN draining the site of vaccination ( polio, tetanus, pertussis, diphteria) and viral infections, (CMV, influenza), Hist. - diffuse hyperplasia and an increase of immunoblasts. Anticonvulsant drug lymphadenopathy (dilantin L.) may happen after 1 week to many months after therapy Sympt. - skin rash, fever, hepatosplenomegaly, painful joints. OTHER LYMHADENOPATHIES 2 Dermatopathic L. (lipomelanotic reticulosis) associated with chronic dermatosis esp. exfoliative type Hist. - widened pale-stained T-zone areas with foaming vacuolated macrophages with fat and/or melanin droplets. Lymphadenitis following lymphangiography due to accumulation of fat globules in LN sinuses Whipple disease (e.Tropheryma whippelli Gram+ bact.) accumulation of pale-staining, PAS+ macrophages loaded with bacteria in small intestinal mucosa and sinuses of draining LN clin.: malabsorption syndrome, polyarthritis, lymphadenopathy,hyperpigmentation, psychiatric disorders OTHER LYMPHADENOPATIES - 3 HIV-related lymphadenopathy (very large lymphoid follicles with giant germinal centers, later fragmentation and atrophy) Lymphadenopathy in rheumatoid arthritis (enlargement of lymphoid follicles, low proliferative activity of germinal centers, accumulation of plasma cells between follicles, infiltration of neutrophils in sinuses Lymphadenopathy in infectious mononucleosis (in paracortical area proliferation of immunoblasts – mostly B cells, with high mitotic activity VIRUS-ASSOCIATED HEMOPHAGOCYTIC SYNDROME (VAHS) Etiology: rare complication of viral infections (EBV, CMV,adenoviruses, B19 parvovirus and other) Incidence: most often in renal transplant and/or immunosuppressed patients Clin.: fever, pulmonary infiltrates, hepatospleno-megaly, lymphadenopathy, cytopenia Hist.: LN enlarged, small lymphoid follicles without germinal centers, with abundant nuclear debris, free or in cytoplasm of proliferating histiocytes. Prognosis: uncertain, potentially reversible CASTLEMAN DISEASE Two major gross types : single localized – large tumor in mediastinum, non-specific symptoms: fever, anemia, hypo-proteinemia, polyclonal hipergammapathy;good prognosis Multifocal – general lymphadenopathy,high fever, weight loss, skin changes, hemolysis, poli- or mono-hypergammapathy, possible progress to lymphoma; poor prognosis Probable etiology: infection with herpes virus HHV-8 Histology – two types: vascular hyaline - atrophy of germinal centers in lymphoid follicles, numerous venules surrounded by hyaline masses (angiofollicular lymph node hyperplasia) (predominant in single localised type) plasma cellular – interfollicular spaces filled with plasma cells (predominant in multifocal type) SPLEEN – MAJOR FUNCTIONS Filtration of unwanted elements from blood – aged and damaged cells, but also bacteria, cell debris,abnormal metabolic molecules - phagocytic functions Major secondary organ in the immune system- antibody production, especially of IgM class A source of lymphoreticular and hematopoetic cells A reserve pool and storage site of blood cells CAUSES OF SPLENOMEGALY 1. 2. 3. 4. 5. 6. 7. Infections Congestive states Lymphohematologic disorders Parasitic infestations Connective tissue diseases Storage diseases Varia (amyloidosis, cysts, neoplasms etc.) Splenomegaly associated with acute infection (“septic spleen”) Septicemia arising from liver abscesses due to echinococcosis. Spleen weight 610g. Splenomegaly associated with acute infection Hyperplasia of reticulum cells in red pulp. Note presence of large pulp cells separated from their normal connection. Leucocyte infiltration, erythrophagocytosis. HE, 520x Chronic splenomegaly in response to infection Note active proliferation of reticulum cells, deployment of littoral cells, erythrophagocytosis. HE, 520x Hypersplenism – clinical features Splenomegaly –dragging sensations in the abdomen (left upper quadrant) Discomfort after eating Anemia, leukopenia Thrombocytopenia Hyperplasia of bone marrow precursors Banti Syndrome – Non-cirrhotic or Idiopathic Portal Hypertension Etiology After subclinical occlusion of the portal vein Symptoms Splenomegaly, hypersplenism, anemia Hist. Splenic red pulp replaced by fibrosis deposition of collagen in basement membranes of sinusoids impairs blood flow leading to excessive destruction of blood cells. Focal hemorrhages become organised with deposits of hemosiderin and calcium (Gamna-Gandi bodies). Treatment surgical shunting procedures LEUKOCYTOSIS Granulocytosis (inflammations, tissue necroses) Eosinophilia (allergy, parasitic infect., some skin diseases) Lymphocytosis (viral infections, severe chronic infections) Monocytosis (severe chronic bacterial/ fungal inf.) Mastocytosis (increased numbers of mast cells in skin and sometimes in other organs) Leukemoid reaction (huge numbers of immature cells in blood LEUKOPENIA-USUALLY GRANULOCYTOPENIA (BELOW 1000/c.mm) Reduced production Suppression of myeloid stem cells Neoplastic occupation of bone marrow Suppression of granulocyte precursors Vit. B12 or folate deficiency Accelerated removal Hypersplenism Inreased utilization-in infections Felty’s syndrome Exposure to drugs Proliferation of CD8+ LGL in bone marrow Features Of Mononuclear Phagocyte System – MPS (Reticulo - Endothelial Sys.) Compounds: Monocytes, macrophages, reticulum cells, histiocytes, endothelia, dendritic cells. Function: a. b. c. d. e. endocytosis (phagocytosis, pinocytosis) storage and clearance secretory activity role in immune reactions role in inflammation and infection PROLIFERATIVE DISORDERS OF MPS Localized (reactive or neoplastic) Multicentric reactive (Tbc, sarcoidosis) neoplastic (?) Systemic reactive (storage diseases, VAHS) neoplastic (malignant histiocytosis) LANGERHANS’ CELL HISTIOCYTOSIS (HISTIOCYTOSIS X) (1) Unifocal: eosinophilic granuloma Expanding erosive accumulation of Langerhans’ cells (dendritic cells) admixed with eosinophils, plasma cells, lymphocytes within medullary cavities of bones. Any bone may be involved, but commonly ribs, calvarium, femur but also teeth. LANGERHANS’ CELL (LC) HISTIOCYTOSIS (HISTIOCYTOSIS X) (2) Multifocal: Hand – Schuller - Christian dis. Proliferation of mature Langerhans’ cells with abundant intracytoplasmic lipids (cholesterol, its esters, neutral fats) Aberrant expression of chemokine receptors – CCR6 and CCR7 on LC – migration to tissues Clin.: triad-bone lesions, exophtalmos, diabetes insipidus (due tp involvement posterior stalk of the hypothalamus) also - fever, skin eruptions, hepatospleno-megaly Young children are affected,Prognosis fairly good LANGERHANS’CELL HISTIOCYTOSIS (HISTIOCYTOSIS X) (3) Systemic: acute disseminated (Letterer - Siwe disease progressive proliferation of L. Cells leading to destruction of hematopoesis, recurrent infections and often to death, Clin. - cutanous lesions, later involvement of internal organs – hepatosplenomegaly, lymphadenopathy, Children before two years of age are affected. Prognosis – poor GAUCHER DISEASE Pathogenesis: Proliferation of histiocytes filled up with glucocerebroside - lack of glucocerebrosidase, an enzyme needed to hydrolize glycolipids from senescent blood cells Gen.: Mutation on chromosome 1 (q21-q31) Symptoms: Splenohepatomegaly (giant spleen up to 10 kg), erosion of bones, anemia, leucopenia, various neuropathies Hist.: Infiltration of organs with Gaucher cells rich in glucocerebrosides stored in lysosomes Three types - adults (99%), infantile, juvenile. NIEMANN-PICK DISEASE Pathogenesis: Accumulation of sphingomyelin in histiocytes (derived from cell membranes, subcellular organelles, myelin sheaths) Lack of sphingomyelinase in two forms of N-P disease Hist.: Foam cells in spleen, bone marrow, liver, lymph nodes Clin.: Hepatosplenomegaly, cachexia, mental retardation Two types: A - in infants (80%) and B - without involvement of CNS That’s all. You can relax!