PAT LEC 4 HEM - neutralposture
advertisement

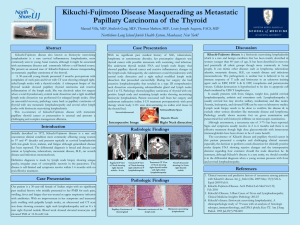
LYMPHADENOPATHY Dr. Manjit Singh Saren Pathologist, MAHSA University College. HISTOLOGY HISTOLOGY LYMPHADENOPATHY DEFINITION: Disease of lymph nodes Associated with underlying pathology. i) Involvement in variety of systemic diseases. ii) Primary lymphoid malignancies iii) Metastatic lymphoid lesions iv) Localized infections v) Localized injuries LYMPHADENOPATHY Types: 1. REACTIVE LYMPHADENITIS Inflammation of lymph nodes 2. REACTIVE LYMPHADENOPATHY Primary immune reactions REACTIVE LYMPHADENITIS NON- SPECIFIC RESPONSE 1.Acute lymphadenitis 2.Chronic lymphadenitis 1) Acute lymphadenitis: draining inflamed area. >Bacterial infections >Foreign bodies in wounds Nodes: Enlarged and tender Untreated : Chronic adenitis, necrosis and abscess 2) Chronic Lymphadenitis: A). With follicular B cell hyperplasia i. Non- specific lymphadenitis: Commonest lesion ii. Specific lymphadenitis: Rheumatoid arthritis Toxoplasmosis Syphilis AIDS B) With para-follicular T cell hyperplasia - Microbiological agents - Drugs (Dilantin) - Virus (Inf. Mononucleosis) -Post vaccinial C) With sinus hyperplasia with histiocytosis: Cancer draining sites. Micro: Phagocytes within dilated sinuses. LYMPHADENOPATHY 1. Primary: Lymphoid malignancies. Amyloidosis 2. Secondary: i. Infections: TB Sarcoidosis Syphilis Castleman’s Disease Dermatolymadenopathy Filariasis ii. Metastatic diseases CAUSES OF LYMPADENOPATHY: 1.HIV related 2.Opportunistc infections: TB, CMV, Toxoplasmosis, Norcardia. 3.Fungal: Histoplasmosis, cryptococcusis. 4.Reactive: Pyogenic infections/bacteria. 5.Venereal: (STD)- Syphilis, Chancroid, Lympho- Granuloma Venereum 6.Malignancies: i. Primary: Lymphomas ii. Secondary: Metastasis CYTO MEGALIC VIRUS CYTO MEGALIC VIRUS Toxoplasma gondii TUBERCULOUS LYMPHADENOPATHY Poor socio-economic background. Over-crowding Presentation: Night sweats Cough with hemoptysis Loss of weight Family history Diagnosis History ESR Sputum examination for AFB TB Culture Chest X-rays CT Scan MRI BIOPSY SARCOIDOSIS Etiology: Unknown. Cell mediated immune reaction Affects: Lung and lymph nodes Micro: 1. Langhans cells, Foreign body giant cells 2. Asteroid bodies, Schaumann bodies. 3. Non-caseating granuloma 4. Epitheloid cells and fibrosis Diagnosis: Kviem’s Test: Intra-dermal test FILARIAL LYMPHADENOPATHY Etiology: Wuchereia Bancrofti Brugia malayi Adult worm in: lymphatics, Lymph nodes, testis and epididymis Acute: Fever, lymphangitis, epididymo-orchitis and microfilaria. Chronic: Lymphadenopathy, hydrocele and elephantiasis. Complications: Chylous ascitis & chyluria AL AMYLOIDOSIS Associated with plasma cell dyscrasias. Secrete Immunoglobulin light chains. Can be associated with lymphadenoparthy Diagnosis: Congo red: 1.Light microscopy Eosinophilic amorphous 2.Polarised light: Apple green birefringence PART I LYMPHADENOPATHY CASTLEMAN’S DISEASE Definition: Single solid growth within lymphatic tissue Sites: Chest, stomach or neck . Abnormal enlargement of lymph nodes. CASTLEMAN’S DISEASE Etiology: Unknown Rare disorder Types: 1. Hyaline type 90% 2. Plasma type: prevalent in young DERMOTOPATHIC LYMPHADENOPATHY Definition: Reactive lymph node hyperplasia. Etiology: Secondary to eczema and dermatitis Micro: Intra-dermal macrophages containing fat and melanin CAT SCRATCH DISEASE Children 80% Self limiting Gm-ve bacterial infection Localized lymphadenopathy Sarcoid-like granulomas Stellate abscess LYMPHANGIITIS Inflammation of lymphatic vessels i. Acute Lymphangiitis: Bacterial infections: B-Strep % & Staph. Micro: inflammatory exudate and clotted lymph ii. Chronic Lymphangitis: TB, Actinomyces, syphilis, radiation,& parasites Micro: Fibrosis and chronic lymphedema KIKUCHI’S DISEASE Presentation: Fever and Tender Adenitis Micro: Necrosis and stellate abscesses Neutrophils and nuclear dust Histiocytes but rarely any eosinophils KIMURA’S DISEASE Introduction: Chronic inflammatory disorder Clinical Features: Age: 20-40 yrs and males Painless swelling of parotid Cervical lymphadenopathy KIMURA’S DISEASE Micro: Lymph node biopsy: Eosinoplilia Proliferation of vascular endothelium. Focal eosinophilic abscess Hyperplasia of lymphoid follicles: Well vascularised Warthin-Finkeldey polykaryocytes KIKUCHI’S DISEASE Common in children Cervical lymphadenopathy Also : Necrotizing histiocytic lymphadenitis Etiology: CMV EBV Herpes virus KIMURA’S DISEASE PATHOPHYSIOLOGY Allergic reaction: -Parasites, viral, arthropod bites and candidiasis. Auto-immune reaction : IgE –mediated Type I hypersensitive reaction. Cytokines: Interleukin 4 and 5 produces:- > Eosinophiltrophic cytokines & IgE 20% with nephrotic syndrome KAWASAKI’S DISEASE Age: <5yrs Cause: Unknown Lymphadenopathy Clinically: Fever (>39C) red eyes Red and cracked lips Rash on chest and genitals Swollen tongue and enlarged lymph nodes Complications: Affects heart: Arrhythmias C)Multicentric or Generalized Type CASTLEMAN’S DISEASE Multiple sites Symptoms: Same as plasma type Hepato-splenomegaly ‘POEMS Syndrome Complications : POEMS SYNDROME Kaposi’s Sarcoma Non Hodgkin’s Lymphoma LANGERHANS CELL HISTIOCYTOSIS Histiocytosis : Proliferative disorder of histiocytes or macrophages. Auto-immune disease & genetically related Types: 1. Benign: Histiocytic proliferation in lymph nodes. 2. Malignant: Histiocytic lymphoma 3. Intermediate: Langerhans cell Histiocytosis LANGHERAN CELLS: ORIGIN Derived from dendritic cells of skin. Proliferating Langerhans cells are LEUKOCYTE ANTIGEN DR (HLA-DR) positive and express CD1 antigen. Cells contain Berkeck’s granules. EM Micro: Vacuolated cytoplasm resembling tissue histiocytes and hence called Langerhans Cell Histiocytosis HISTIOCYTOSIS X 1. LITTERER SEWE DISEASE Age: 2 yrs and less Presentation:Cutaneous lesions Hepato-splenomegaly Pulmonary lesions (stiffening) Destructive osteolytic bone lesions&fractures Infiltrates bone marrow causing: anaemia and thrombocytopenia Predisposing: to infections. Rapidly fatal Chemo:50% 5 year survival 2: EOSINOPHILIC GRANULOMA Langerhans cells in bone medullary cavities Micro: Histiocytes and eosinophils along with plasma cells and lymphocytes. Lesions: Unifocal: Pain and pathological # Treatment: Local excision and radiation. May heal spontaneously 2. MULTIFOCAL LESIONS Affects children Clinical Presentation: Fever and diffuse eruptions on scalp Otitis media URTI Generalized Lymphadenopathy Hepato-splenomegaly Diabetes Insipidus (post pituitary stalk involved) 3. HAND SCHULLER CHRISTIAN DISEASE Presentation: Involvement of calvarial bone Diabetes Insipidus Exophthalmos Treatment: Spontaneous regression Chemotherapy HAND SCHULLER CHRISTIAN DISEASE Presentation: Involvement of calvarial bone Diabetes Insipidus Exophthalmos Treatment: Spontaneous regression Chemotherapy