David Counsell - National Confidential Enquiry into Patient

An Age Old Problem:
Insights from Anaesthesia
Dr David Counsell
MB ChB FRCA FFPMRCA PhD
Chair Acute Pain Special Interest
Group – British Pain Society
Chief of Staff, Anaesthetics, Critical
Care, Pain & Resuscitation CPG.
BCUHB, North Wales
Give me a
Challenge and I’ll show you an
Opportunity.
D.J Counsell 2010???
Changing Hospital Practice
Implications of:-
•
Day case target rates of 85%.
•
Eyes 100% but rarely GAs, minimal analgesia.
•
Appropriate in elderly?
•
Enhanced recovery (hip, knee, colorectal etc.)
•
100% Elective admission on day of surgery.
•
Less opportunity to go daft?
•
Increase risk to elderly patients?
•
Reduced bed numbers but ‘sicker’ patients.
Why Give Pain Relief?
Humanitarian
Pain on Movement
Impaired Mobilisation
Pain
Poor Cough/Expectoration
Deep Breathing
Slow Return Of
Lung Function / FRC
Risk of DVT
Increased BP/ Heart Rate
Increased O2 requirements
Global ? Myocardial
Pneumonia
Hypoxia Organ Failure
Organ Ischaemia
MI Gut/Sepsis
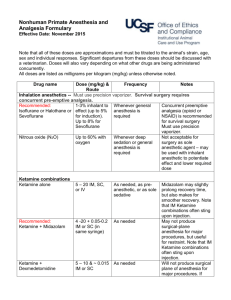
Pillars Of Analgesia
Pain Assessment
Often Difficult
Multi modal Analgesia
•
Opioids, NSAIDS, Paracetamol, Local, Other.
Patient Controlled Analgesia
•
Humanitarian but doesn’t reduce morbidity.
•
Relies on Dexterity and Understanding
- Careful Assessment
- May Precipitate Confusion
Post operative Analgesia
Dilemma
•
Opioids
• confusion,
• no reduction in morbidity
•
Regional techniques
•
Hypotension (spinal/epidural),
•
Immobility (nerve blocks)
•
But do lower morbidity/mortality
Opium Poppies – Andalucia, Spain Circa 4500 BC
•
Hypotension easily managed on HDU
• resource issues.
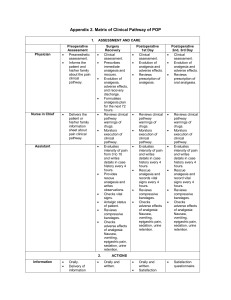
4 Clinical Groups
Report conclusions very ‘generalised’.
Unscheduled Admissions
•
Orthopaedic Trauma – mainly #NOF.
•
Other Surgery – mainly abdominal.
Scheduled Admissions
•
Orthopaedic – mainly arthroplasty
•
Other Surgery
Very different groups.
Very different challenges.
Analgesia – Trauma #NOF
Difficult challenge –opioid aversion, NSAID risk
Opioids – confusion, sleepy, impair self caring with dehydration and poor nutrition.
Non opioid methods including regional blocks done on admission have significant advantages (by
Nurses) pre and post op.
Logistics and Issues over who can safely perform/top up blocks limit their use. (ESRA).
Surgical Analgesia
Surgical Emergencies
•
Assessment/resuscitation
‘delays’ surgery often NBM
•
Direct Pain Team input mainly daytime, post op.
•
Opioids less of an issue.
•
Surgeons will give opioids to acute abdomen patients.
•
Could use PCA, not just remit of pain team/anaesthetist.
Opium poppies; tomb of Psamtek, Saqqara circa 550BC
Analgesia - Arthroplasty
Big reliance on femoral/sciatic blocks.
Limit attempts at early mobilisation.
Adverse effects in Enhanced Recovery
Solutions - Knees
•
Stop using blocks
•
Multi-modal, local infiltration.
•
No drains, Tranexamic acid
•
No (minimal) opioids
•
Mobilise on day 0, Home day 2-3
Analgesia Elective Abdominal
High risk patient group.
Epidural Analgesia improves outcome.
•
Hypotension common - 30%
•
Failure is common - 30%
Require careful supervision – pain team
Commonly need vasoconstrictors
HDU care if possible 1 st 24 Hours
Analgesia – Pain Teams
25% of hospitals have no pain service.
Does private sector offer same care?
Concerned some are NHS Hospitals (NIPPS)
Those that do are limited hours (not 24/7).
Fully support pain as ‘5 th Vital Sign’ but not just a surgical issue in the elderly.
Report underlines need for pain teams.
Under threat due to funding cuts.
Critical Care
Ageism - not rife or not admitted?
Beds at a premium.
Denied epidurals due to lack of HDU bed?
UK ‘poor neighbour’ of Western World in terms of Critical Care beds per capita.
Activity thus far – ‘Damage limitation’
Medicine for Care of Older People.
Agree we need more input.
Many examples of good practice
•
Orthogeriatricians
•
1 only in many trusts (?annual leave)
•
Often trauma (# NOF) focussed.
•
Involved in analgesia/pre op blocks.
•
What about other surgery?
•
How do we get early involvement?
Do we follow paediatrics model???
Anaesthesia – POAC
Pre Assessment for Scheduled Surgery.
Nurse/Pharmacist led (2 consultant sessions/wk)
Massive opportunity for liaison with
MCOP clinicians.
•
Automatic referral protocol based upon:-
•
Polypharmacy (4+ medicines)
•
Frailty (could introduce score)
•
Asses nutrition, analgesia etc
•
Identify those ‘at risk’ pre admission to MOCP
•
Better optimisation.
•
Focussed care during admission.
Elective Surgery v Palliation
Not ageist to ask if surgery was appropriate.
Die in post-op period or live months/years.
CPET (CPEX) Valuable investigation
•
Measures anaerobic threshold.
•
Allows improved risk assessment.
•
Informed joint decision by patients and clinicians.
Relatively inexpensive.
•
Cheap kit
– labour intensive interpretation.
•
Technicians currently at a premium
•
‘Owned’ by Cardio/Resp medicine.
•
Limited access for pre op assessment.
Anaesthesia – Delays #NOF
Often our fault.
•
Does ‘Not Fit’ mean ‘I’m too junior’
•
Better consultant Trauma input.
Surgical convenience.
•
More interesting cases go first.
•
Left late on list – multiple cancellations.
Systematic
•
Trauma list provision variable (every day)
Anaesthesia - Intraoperative
Anaesthesia comes out well.
Generally agree with conclusions.
•
Monitoring – non invasive CVS easily available needs more investment/use.
•
Hypothermia easily avoidable.
•
National anaesthetic chart ??? Not deliverable by CDs but something the RCoA might tackle.
•
Hypotension
•
Simple strategies exist – bread & butter.
•
Broader appreciation of risks in Elderly.
•
Is spinal anaesthesia as safe as we think (NAP 3).
Summary
Deaths = Tip of Pyramid.
Other poor outcomes.
Challenging on many fronts.
Underlines importance of pain teams.
•
Implement 5 th Vital Sign.
•
Introduce appropriate scoring systems.
•
Support use of high tech analgesia.
•
Ammunition to defend teams from budget cuts.
Do we need to reconsider the UK provision of Level 2 Critical Care Beds?