Department of Anaesthesia and Intensive Care
advertisement
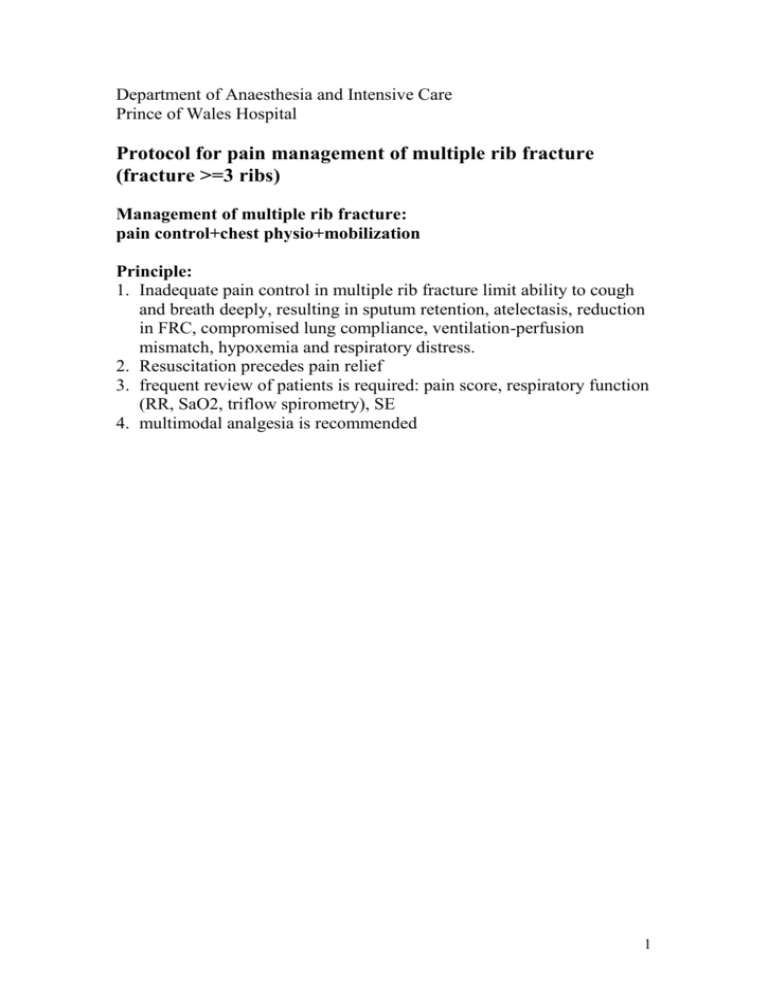
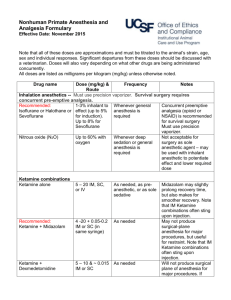
Department of Anaesthesia and Intensive Care Prince of Wales Hospital Protocol for pain management of multiple rib fracture (fracture >=3 ribs) Management of multiple rib fracture: pain control+chest physio+mobilization Principle: 1. Inadequate pain control in multiple rib fracture limit ability to cough and breath deeply, resulting in sputum retention, atelectasis, reduction in FRC, compromised lung compliance, ventilation-perfusion mismatch, hypoxemia and respiratory distress. 2. Resuscitation precedes pain relief 3. frequent review of patients is required: pain score, respiratory function (RR, SaO2, triflow spirometry), SE 4. multimodal analgesia is recommended 1 Flowchart for selection of analgesia in multiple rib fracture: High risk group: 1. Age>65? 2. >=4 rib fracture? 3. Cardiopulmonary disease? 4. DM? Yes Regional analgesia No Contraindications for regional analgesia? No Expertise available? ** Yes Yes No Contraindication for iv PCA morphine? 1. Confused? 2. CVS stable? 3. Airway obstruction? Head injury, intraabdominal injury, CVS instability? Yes No No Yes For iv PCA morphine+ oral/iv/PR medication Oral/iv/PR medication Thoracic paravertebral block Epidural analgesia 2 Options: A. Regional analgesia: **For epidural analgesia and thoracic paravertebral analgesia, please check availability of pain procedure section on coming Wednesday (preferably within 2 days of injury) and inform Dr Alice Man/ MC Chu/ Dr Simon Chan 1. Epidural analgesia a. The optimal modality of pain relief for blunt chest wall injury, the preferred technique after severe blunt thoracic trauma b. Patients with >=4 rib fractures who are >=65 years of age should be provided with epidural analgesia unless contraindicated c. Younger patients w/ >=4 rib fracture or patients aged >=65 with lesser injuries should be considered for epidural analgesia d. Advantages: superior analgesia with increase in FRC, dynamic lung compliance, VC and PaO2 reduction in airway resistance change shallow breathing to near normal and reduce paradoxical chest wall movement modify immune response e. Disadvantages: technically demanding, esp. distressed in pain may mask intraabdominal injury cause hypotension CVS instability side effect (nausea, vomiting, urinary retention, respiratory depression, pruritis) complication (dural puncture, epidural haematoma, spinal cord trauma) 2. Thoracic paravertebral block (continuous) a. effective analgesia, resulting in improved respiratory parameters and ABG b. Advantages: 3 avoid need for sedation and ventilation and allows continuous neurologic assessment (especially in patents with head injury) unilateral segmental blockade spare lumbar and sacral nerve root for monitoring (especially in patients w/ concomitant lumbar spinal injury) does not require palpation of rib, feasible for fractures of upper ribs technically simple lower incidence of complication like urinary retention and hypotension c. Complications: hypotension, vascular puncture, pleural puncture, pneumothorax, inadvertent epidural anaesthesia 3. Intercostal nerve block a. Improve peak expiratory flow rate and volume b. Disadvantages: Require multiple injection-painful Time consuming Predispose to local anaesthetic toxicity Technically difficult for upper ribs Complication: pneumothroax 4. Intrapleural a. Advantages: less complication like hypotension, bladder and lower extremity paresthesia and weakness b. Disadvantages: Significant amount of anaesthetic may be lost in presence of chest drain (may require temporary clamping which may cause tension pneumothorax) Theoretically impair diffusion of anaesthetic in presence of haemothorax Posture-dependent Complication: pneumothorax 4 B. Medication (oral/iv/PR) 1. NSAID: a. effective b. CI: GI upset, renal dysfunction, CVS instability, bleeding tendency, head injury, allergy c. Oral: voltaren SR 100mg daily d. Iv: ketorolac 15mg BD for 2/7 2. Weak opioid: Dologesic a. Oral: dologesic tab 2 qid b. CI: hepatic derangement, allergy Tramadol a. Oral/ iv/ PR tramadol 50-100mg tds b. SE: nausea, vomiting, dizziness c. CI: concomitant MAOI 3. Paracetamol: a. Oral/ PR: panadol 1g qid b. CI: hepatic derangement 4. Opioid: a. Improve pain score and vital capacity b. Advantages: Ease of administration and monitoring by nurse Without risk of invasive procedure or need for specialized personnel c. SE: respiratory depression, sedation, cough suppression d. Morphine: iv PCA- loading dose required or iv morphine prn (only in ICU) Reference: 1. Manoj K. Karmakar and Anthony M.H. Ho: Acute pain management of patients with multiple fractured ribs. The Journal of trauma injury, infection and critical care: vol 54, no. 3, 2003 2. Eastern Association for the Surgery of Trauma: Pain Management in blunt thoracic trauma. An evidence-based outcome evaluation 2nd review-2003 5