Answering the Questions of Substance Exposure
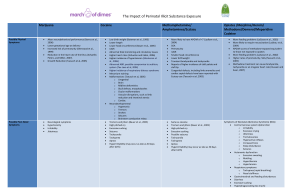
advertisement

Answering the Questions of Substance Exposure Sandra Young, DNP, RNC Healthy People 2010Substance Exposure • Abstinence from Smoking During Pregnancy 99% • Smoking Cessation During Pregnancy 30% • Abstinence from Alcohol Use During Pregnancy 94% • Goal to have 100% abstinence of illicit substance use during pregnancy How bad is it? State statistics 4.0 % of women pregnant and not pregnant (2006 MOD) (below national average 8.0 – 8.2%) 114,000 used drugs in 2007 (National Survey on Drug Use and Health) 21000 babies x 4.0 = 840 babies born substance exposed 2010 18124 The number of neonates treated for substance abuse tripled from 2003 to 2007, and was seven times greater in 2006 than 1999 816 mothers admitted to substance use from July 2007 to June 2008, 1501 mothers in 2010 103 babies required NICU level 3 care $41,815 average cost 16 day average LOS Average cost of NICU care $1000/day What is the Cost? • Baxter, Nerhood, and Chaffin (2008) – Forty-eight infants were diagnosed with NAS, with 40 (83.3%) requiring intensive care – total hospital costs $1.7 million – average cost of $36,700 – Medicaid paid 42% of cost in states 3 NICUs Who paid? Methods of Payment of Substance Using Mothers 3% 1% 10% 3% OTHER INSURANCE SELFPAY MEDICAID UNKNOWN 83% A Blueprint to Improve West Virginia Perinatal Health Policy Recommendations to Improve Perinatal Health 1. Create a Coordinated Statewide Perinatal System 2. Save State Dollars by Reducing Costly Medical Procedures 3. Reduce Exposure to Tobacco Smoke During Pregnancy 4. Reduce Drug and Alcohol Use Among Pregnant Women 5. Improve Breastfeeding Support and Promotion 6. Improve Perinatal Health and Birth Outcomes of African American Women 7. Recruit and Retain More Obstetric Providers 8. Expand Newborn Screening to 29 Conditions 9. Encourage West Virginia Businesses to Offer Perinatal Worksite Wellness 10. Improve the Oral Health of Pregnant Women Through Policy and Education Why is it a problem? – “Overwhelmed: WV Babies being turned away from intensive care” (Charleston Gazette, Nov. 2007) – Shortage of NICU Beds – Higher number of high risk infants delivered in rural hospitals – Increase in number of newborns requiring detoxification due to mother using drugs during pregnancy What do we do? Caring for drug exposed infants can be emotionally, physically, and mentally demanding upon the nurse. Education may provide an understanding of the consequences of substance abuse on the newly born (Raeside, 2003) What do we do? “Increased awareness of this growing problem is needed so that earlier interventions can be implemented” (Baxter, Nerhood, and Chaffin, 2008, p1). When can substance use be identified? • Prenatal • Postpartum Prenatal Screening • Prenatal Initiative – http://www.wvperinatal.org/downloads/committee_reports_07/Me dical_Guidelines_2008.pdf • PRISI – http://www.wvdhhr.org/rfts/forms/R300_PRSIform_2.pdf • WV Healthy Start/HAPI project • Helping Appalachian Parents and Infants When should you be more alert • Mother – – – – – – – – No prenatal care Late prenatal care Limited prenatal care Unanticipated delivery outside the birthing facility Drop in delivery (Hospital/doctor hopping) Abruptio placenta Maternal admission to drug use during pregnancy Positive Maternal drug screen When should you be more alert • Infant – – – – – Unexplainable premature delivery Unexplainable small for gestational age Unexplainable small head circumference Unexplained seizures, intracranial bleeds, or strokes Unexplained symptoms that might suggest drug withdrawal: • High pitched crying, irritability, hypertonia, lethargy, disorganized sleep, sneezing, hiccoughs, drooling, diarrhea, feeding problems, or respiratory distress. • Unexplained congenital malformations involving genitourinary tract, abdominal wall or gastrointestinal systems How is substance use identified Meconium Urine Cord Blood Hair Umbilical Cord What did the leaders say? How do you identify drugs of abuse in pregnant women? • • • • Personal Report 76.2% Blood Test 28.6% Urine Test 76.2% Other 4.8% • Prenatal Record What did OB leaders say about substance use in WV? • What do you perceive to be the most common drug exposure in your neonate population? • • • • • • Methamphetamine 15% Cocaine 30% Marijuana 85% Opiates 35% Poly substance abuse 5% Other 30% • Methadone • Cigarettes • Barbiturates in addition to those mentioned • Benzos What substances are most frequently used? • From July 2007 to June 2008 • • • • • • • • 816 or 5% reported drug or alcohol use during pregnancy. 489 (59%) reported using marijuana, 143 methadone 110 cocaine 29 methamphetamine 22 heroin Alcohol use during pregnancy was reported by 185 mothers. Poly-substance use was also identified, with 117 mothers admitting to poly-substance use (Tolliver, 2008). 2010 • • • • • • • • • 172 alcohol <1% 75 cocaine <1% 669 marijuana 3.6% 231 methadone 1.3% 30 heroin <1% 50 methamphetamine <1% 446 other opioids 2.4% 1501 drugs 8.3% Total 9.2% What are the effects of these substances? • • • • Marijuana Cocaine Methamphetamine Opiates, Methadone, Heroin Marijuana • Most commonly used substance after tobacco • CNS depressant • crosses the placenta and can cause reduction in the heart rate of the fetus • urine the first day of life and up to 3 days after delivery in meconium Marijuana and Delivery Issues • Late prenatal care (Burns, et al., 2006) • More often required NICU admission Marijuana • Alters neurobehavioral performance (Carvalho do Moraes Barros, et al., 2006) • Lower gestational age at delivery • Increased risk of prematurity (Sherwood, et al., 1999) • Reduction in the heart rate of the fetus (Schaefer, Peters, and Miller, 2007). • Growth Reduction Marijuana Possible post-natal symptoms • • • • Irritability Tremors Sleep disturbances Jitteriness Marijuana • Long term outcomes – increased risk of childhood leukemia and eye problems, as well as a link to developmental delays (D’Apolito, 1998). – increased risk of neuroblastoma in children when mothers use illicit or recreational drugs, particularly when marijuana is used in the first trimester of pregnancy. Bluhm, et al., (2006) – First trimester exposure to marijuana affected child’s depression and anxiety symptoms. Second trimester affected reading comprehension and underachievement. Goldschmidt, et al., 2004 – Speech and thought impairments Marijuana and Breastfeeding • Passes into breast milk • Half life up to 57 hours • Exposure to marijuana in breast milk has been linked to delayed motor development • Breastfeeding with marijuana use should be discouraged Cocaine • Most widely studied substance of abuse in pregnancy • CNS Stimulant • Causes vasoconstriction – Fetal, uterine and maternal – Resulting in infarcts and hemorrhages • Placenta appears to block some cocaine absorption • Cocaine can be present in neonatal urine for 1-2 days and meconium for up to 3 days following maternal ingestion Cocaine and Delivery Issues •Placental abruption (Ananth, et al., 2006) •Premature ROM (Addis, et al., 2001) •Pre term labor •Less/late prenatal care (Fajemirokin-Odudeyi, et al., 2004) •Premature Delivery/prematurity •High risk of maternal death from intracerebral hemorrhage •Stillbirth •High risk of perinatal HIV •Higher risk of syphilis Cocaine • Impact on the neonate – – – – – – – – Delayed auditory brainstem response Low birth weight (Bateman, et al., 1993) Lower length Lower head circumference (Bauer, et al., 2005) IUGR Abnormal fetal monitoring and circulatory issues Higher heart rates (Schuetze and Eiden, (2006) Higher incidence of hypertension (Shankaran, et al., 2006) Cocaine • Meconium staining • Malformations – Urogenital – Brain – Midline deformities – Skull defects, encephaloceles – Ocular malformations – Vascular disruptions, such as limb reduction and intestinal atresia – Cardiac Cocaine • Neurodevelopmental – Hypertonia – Tremors – Strokes – Seizures – Brainstem conduction relays Cocaine Possible Post-natal Effects • • • • • • • • Tremors and jitters (Bauer, et al., 2005) High pitched cry Excessive sucking Possible Seizures Tachycardia Tachypnea Apnea Hyperirritability (may occur as late as 30 days after birth) Cocaine • Long term issues – Higher infection rates – Negative behavioral outcomes at 3, 5 and 7 year follow-up (Bada, et al., 2007) – Lower IQ scores – Higher risk of SIDS Cocaine and Breastfeeding • Appears in breast milk within 15 minutes of absorption • Half life less than ½ hour • Clears from breast milk within 5 hours • A cocaine-using, breastfeeding mother should pump and discard breast milk for 24 hours after cocaine use. Ideally abstaining from cocaine would be the first choice. Habitual cocaine users should avoid breastfeeding Methamphetamine • Least studied substance of abuse • CNS Stimulant • Causes vasoconstriction – Placenta – Fetal organs – more likely to have APGAR scores of <7 (Ludlow, et al., 2004). – likely to be small for gestational age (SGA). – Administration of Narcan to a methamphetamine exposed neonate could result in the seizure activity. Methamphetamine and Delivery Issues • • • • • Higher incidence of stillbirth Poor prenatal care Sexually transmitted diseases Placental Abruption Postpartum hemorrhage Methamphetamine • Signs of exposure – hyperexcitability, – disturbances in muscle tone, • Cardiac Defects “Transposition of great vessels” • Cleft Lip • Biliary Atresia Methamphetamine Possible Post-natal Symptoms • • • • • • • • Tremors and jitters (Bauer, et al., 2005) High pitched cry Excessive sucking Possible Seizures Tachycardia Tachypnea Apnea Hyperirritability (may occur as late as 30 days after birth) Methamphetamine • Long term outcomes – – – – Mothers have lower quality of life perceptions Greater likelihood of substance use in family and social system Increased risk for ongoing legal difficulties Increased likelihood of development of a substance abuse disorder (Derauf, et al., 2007) – Potential for the following issues: • Respiratory Illnesses • Ingestion • Rashes • Burns Methamphetamine and Breastfeeding • Passes into breast milk • Half life unknown • Breastfeeding with methamphetamine should be discouraged Opiates • • • • • • Opiates Morphine Heroin Methadone Demerol/ Meperidine Codeine Opiates • More likely to require resuscitation (Ludlow, et al, 2004) • APGAR scores methadone exposed equivalent to those neonates not exposed to opiates • More feeding problems (LaGasse, et al., 2002) • Higher rates of prematurity, SGA,(Martinez, Partridge, and Taeusch, 2005) Opiates and Delivery Issues • • • • • • • • • Late prenatal care (Burns, et al., 2006) More often require NICU admission Antepartum hemorrhage Increased risk of HIV (if mother an intravenous heroin user) More likely to require resuscitation (Ludlow, et al, 2004) Higher incidence of placental abruption Higher incidence of premature delivery, preterm labor Higher incidence of chorioamnionitis Higher rates of meconium staining Opiates • Higher incidence of SIDS Opiates and Breastfeeding • All opiates pass into breast milk • Heroin using mothers should not breast feed • Methadone appears to be well tolerated in breast milk as there appears to be minimal transfer into breast milk • Breastfed babies of methadone using mothers have less symptoms of withdrawal and the need for medication treatment (AAP and Jansson, et al, 2008) Neonatal Abstinence Syndrome (NAS) • Lifshitz, et al., (2001) found that 96% of neonates exposed in-utero to narcotics exhibited NAS. • Symptoms appear on average at 72 hours • May not appear for a long as 4 weeks Symptoms of Neonatal Abstinence Syndrome • Central Nervous System Dysfunction – – – – – – – – Irritability Excessive Crying Jitteriness Tremulousness Hyperactive reflexes Increased tone Sleep disturbance Seizures Neonatal Abstinence Syndrome • Autonomic Dysfunction – – – – Excessive sweating Mottling Hyperthermia Hypertension • Respiratory Symptoms – Tachypnea (rapid breathing) – Nasal stuffiness Neonatal Abstinence Syndrome • Gastrointestinal and feeding disturbances – Diarrhea – Excessive Sucking – Hyperphagia (eating too much) How do we determine withdrawal • Do you use an abstinence/withdrawal scoring tool on your neonates? • NO • Yes – – – – 57.1% 23.7% Neonatal Abstinence Scale 14.3% Finnegan 14.3% Modified scale 9.5% Other 14.3% • CAMC • Johns Hopkins/Bayview • Use risk assessment to determine who needs tested Assessment Tools • http://www.rch.org.au/nets/handbook/media/NASS_1.pdf What do you use to treat for withdrawal in neonates – Methadone 50% – Paregoric 6.2% – Other 50% • No protocol at this time • None • Morphine • Transport out if symptoms • Transferred to tertiary center for treatment if needed • Haven’t had an infant that physicians felt needed medication Treatment Options • Where are treatment facilities? • Lack of beds where mothers and babies can go together • Impact of Methadone clinics • Infant Treatment Options – Methadone – Morphine – Phenobarbital Treatment Options • Infant – Opioids are most common treatment method • Morphine (Jackson, Ting, Mckay, Galea, and Skeoch (2004) – opioids most effective • Sarkar and Donn (2006) – Opioids - opioid and poly-substance use – Methadone – opioid use – Phenobarbital – poly-substance use What Can We Do to Help? • Rooming in • Discharge Planning • Early Intervention – At home – Community Services • • • • Birth to Three 1-866-321-4728 Right from the Start CSHCN Ski*Hi Do I have to call? • Keeping Children and Families Safe Act mandates the reporting by healthcare providers to child protective services any infant born and identified as being affected by illegal substance abuse and withdrawal symptoms • Call the county DHHR office or • Child Abuse and Neglect Hotline – (1-800-352-6513) – 7 days a week, 24 hours a day Where can I find help? • www.samhsa.gov Questions Thank you!