Fibrinolytic Therapy Use Among STEMI Patients Transferred to a
advertisement
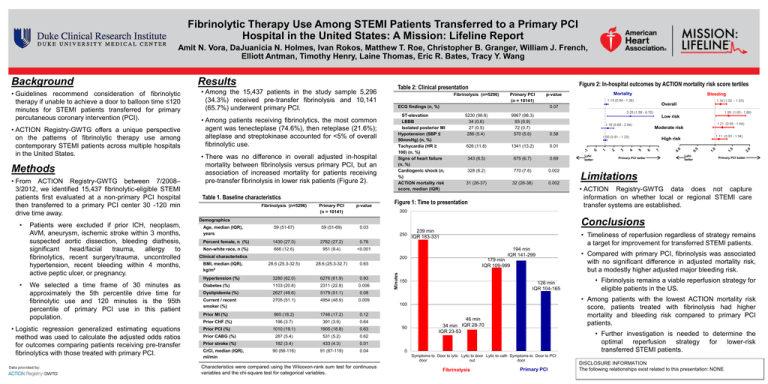
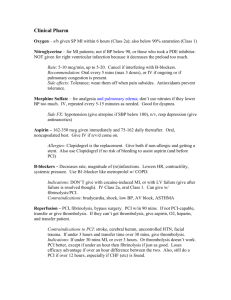
Fibrinolytic Therapy Use Among STEMI Patients Transferred to a Primary PCI Hospital in the United States: A Mission: Lifeline Report Amit N. Vora, DaJuanicia N. Holmes, Ivan Rokos, Matthew T. Roe, Christopher B. Granger, William J. French, Elliott Antman, Timothy Henry, Laine Thomas, Eric R. Bates, Tracy Y. Wang Background • Guidelines recommend consideration of fibrinolytic therapy if unable to achieve a door to balloon time ≤120 minutes for STEMI patients transferred for primary percutaneous coronary intervention (PCI). • ACTION Registry-GWTG offers a unique perspective on the patterns of fibrinolytic therapy use among contemporary STEMI patients across multiple hospitals in the United States. Methods • From ACTION Registry-GWTG between 7/2008– 3/2012, we identified 15,437 fibrinolytic-eligible STEMI patients first evaluated at a non-primary PCI hospital then transferred to a primary PCI center 30 -120 min drive time away. • Among the 15,437 patients in the study sample 5,296 (34.3%) received pre-transfer fibrinolysis and 10,141 (65.7%) underwent primary PCI. • Among patients receiving fibrinolytics, the most common agent was tenecteplase (74.6%), then reteplase (21.6%); alteplase and streptokinase accounted for <5% of overall fibrinolytic use. • There was no difference in overall adjusted in-hospital mortality between fibrinolysis versus primary PCI, but an association of increased mortality for patients receiving pre-transfer fibrinolysis in lower risk patients (Figure 2). Table 1. Baseline characteristics Fibrinolysis (n=5296) Primary PCI (n = 10141) p-value 59 (51-69) 0.03 Fibrinolysis (n=5296) Primary PCI (n = 10141) ECG findings (n, %) ST-elevation LBBB Isolated posterior MI Hypotension (SBP ≤ 90mmHg) (n, %) Tachycardia (HR ≥ 100) (n, %) Signs of heart failure (n, %) Cardiogenic shock (n, %) ACTION mortality risk score, median (IQR) 5230 (98.8) 34 (0.6) 27 (0.5) 286 (5.4) 9967 (98.3) 93 (0.9) 72 (0.7) 570 (5.6) Age, median (IQR), years 59 (51-67) Percent female, n (%) 1430 (27.0) 2762 (27.2) 0.76 Non-white race, n (%) 666 (12.6) 951 (9.4) <0.001 Low risk Moderate risk 0.58 High risk 626 (11.8) 1341 (13.2) 0.01 343 (6.5) 675 (6.7) 0.69 328 (6.2) 770 (7.6) 0.002 31 (26-37) 32 (26-38) 0.002 Figure 1: Time to presentation 250 239 min IQR 183-331 Primary PCI better Lytic better Primary PCI better Limitations • ACTION Registry-GWTG data does not capture information on whether local or regional STEMI care transfer systems are established. • Timeliness of reperfusion regardless of strategy remains a target for improvement for transferred STEMI patients. 194 min IQR 141-299 200 28.6 (25.3-32.7) 0.63 Hypertension (%) 3280 (62.0) 6276 (61.9) 0.93 We selected a time frame of 30 minutes as approximately the 5th percentile drive time for fibrinolytic use and 120 minutes is the 95th percentile of primary PCI use in this patient population. Diabetes (%) 1103 (20.8) 2311 (22.8) 0.006 Dyslipidemia (%) 2627 (49.6) 5179 (51.1) 0.08 Current / recent smoker (%) 2705 (51.1) 4954 (48.9) 0.009 Prior MI (%) 965 (18.2) 1746 (17.2) 0.12 Prior CHF (%) 196 (3.7) 391 (3.9) 0.64 • Logistic regression generalized estimating equations method was used to calculate the adjusted odds ratios for outcomes comparing patients receiving pre-transfer fibrinolytics with those treated with primary PCI. Prior PCI (%) 1010 (19.1) 1905 (18.8) 0.63 Prior CABG (%) 287 (5.4) 531 (5.2) 0.62 Prior stroke (%) 182 (3.4) 433 (4.3) 0.01 90 (68-116) 91 (67-119) 0.04 CrCl, median (IQR), ml/min Lytic better Conclusions Clinical characteristics BMI, median (IQR), kg/m2 Bleeding Overall 0.07 Demographics Patients were excluded if prior ICH, neoplasm, AVM, aneurysm, ischemic stroke within 3 months, suspected aortic dissection, bleeding diathesis, significant head/facial trauma, allergy to fibrinolytics, recent surgery/trauma, uncontrolled hypertension, recent bleeding within 4 months, active peptic ulcer, or pregnancy. Mortality p-value 300 28.6 (25.3-32.5) • Figure 2: In-hospital outcomes by ACTION mortality risk score tertiles Table 2: Clinical presentation Minutes • Results 179 min IQR 109-999 150 126 min IQR 104-165 Characteristics were compared using the Wilcoxon-rank sum test for continuous variables and the chi-square test for categorical variables. 46 min IQR 28-70 34 min IQR 23-53 • Further investigation is needed to determine the optimal reperfusion strategy for lower-risk transferred STEMI patients. 0 Symptoms to Door to lytic Lytic to door Lytic to cath Symptoms to Door to PCI door out door Fibrinolysis • Fibrinolysis remains a viable reperfusion strategy for eligible patients in the US. • Among patients with the lowest ACTION mortality risk score, patients treated with fibrinolysis had higher mortality and bleeding risk compared to primary PCI patients. 100 50 • Compared with primary PCI, fibrinolysis was associated with no significant difference in adjusted mortality risk, but a modestly higher adjusted major bleeding risk. Primary PCI DISCLOSURE INFORMATION The following relationships exist related to this presentation: NONE