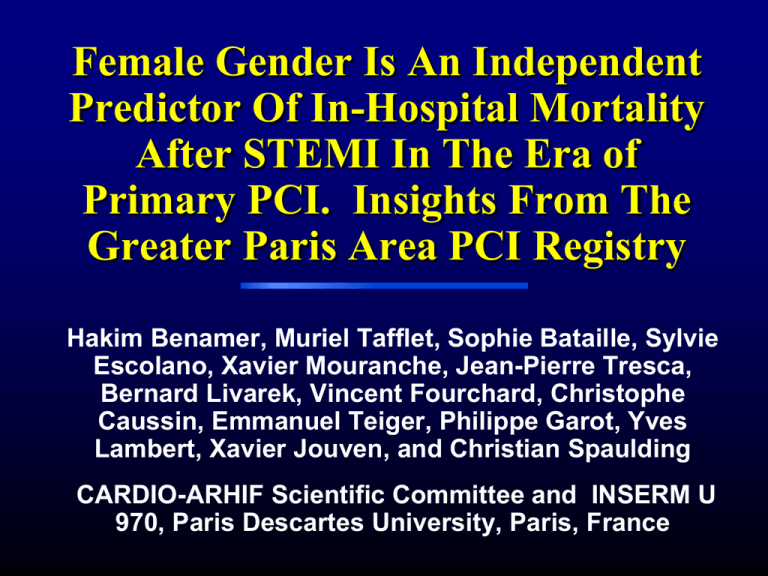
Female Gender Is An Independent
Predictor Of In-Hospital Mortality
After STEMI In The Era of
Primary PCI. Insights From The
Greater Paris Area PCI Registry
Hakim Benamer, Muriel Tafflet, Sophie Bataille, Sylvie
Escolano, Xavier Mouranche, Jean-Pierre Tresca,
Bernard Livarek, Vincent Fourchard, Christophe
Caussin, Emmanuel Teiger, Philippe Garot, Yves
Lambert, Xavier Jouven, and Christian Spaulding
CARDIO-ARHIF Scientific Committee and INSERM U
970, Paris Descartes University, Paris, France
Presenter Disclosure Information
• Christian Spaulding
• Female gender is an independent predictor of inhospital mortality after STEMI in the era of primary
PCI: Insights from the Greater Paris Area Registry
FINANCIAL DISCLOSURE: The Greater Paris Area
registry is funded by a French government hospital
agency (ARH)
UNLABELED/UNAPPROVED USES DISCLOSURE: none
Introduction
• In patients presenting with STEMI, PCI has been
shown to significantly improve survival and rescue
and adjunctive PCI are effective therapies after
thrombolytic therapy
• Studies of sex differences in mortality after STEMI
have consistently indicated that women have higher
death rates, especially for short-term follow-ups
• Although different baseline and procedural
characteristics may account for increased mortality,
they are not sufficient to explain the discrepancy in
outcome. Furthermore, most of these studies were
performed before the widespread use of PCI for
STEMI
Introduction
• Greater Paris Area Registry: mandatory registry
which gathers the clinical and angiographic data on
all coronary angiograms and PCIs performed in this
region
• Aim of the study: to determine if female gender is still
an independent predictor of mortality in patients with
STEMI treated by PCI
Methods
• Population : The Greater Paris area comprises 11
million inhabitants and accounts for 18% of the
French population. 42 centers perform PCI. In 2001,
the government hospital agency of the Greater Paris
area set up a mandatory registry of all PTCAs
performed in this region
• Variables entered: Patients demographics,
procedural information, per and post-procedural
complications and clinical status at hospital
discharge
• Quality check: Internal and external audits are
performed twice a year. Deaths are crossed-checked
in another hospital-based data-base (PMSI)
French guidelines for AMI
• The majority of STEMI patients are transported to
hospital by a pre-hospital emergency system
ambulance with a physician on board
• French guidelines recommend primary PCI as
reperfusion therapy if the transportation time to a
catheterization laboratory is less than 45 minutes
• If the expected transportation time is more than 45
minutes, pre-hospital thrombolytic therapy is
administered if no contra-indications are noted
• In all cases, patients are transported to a PCI capable
hospital
Outcomes of interest
• Aim of this study: to examine the relationship
between gender and in-hospital outcome in STEMI
treated by PCI within 24 hours of onset of chest pain
• Data entered between 2003 and 2007 in 16 726
procedures was screened for:
– STEMI of less than 12 h of duration or STEMI of
more than 12 but less than 24 h of duration if the
operator considered emergency PCI necessary
because of continuous ischemia or complications
– cardiogenic shock and/or successfully
resuscitated OHCA due to acute coronary artery
occlusion
• In-hospital all-cause mortality rate was chosen as the
primary endpoint and independent predictors were
assessed
Baseline characteristics
N
Men
Women
N=13096
N=3664
p
Clinical factors
Age, years (SD)
16726
59.3 (13.0)
69.7 (14.3)
<0.0001
Diabetes Mellitus, n (%)
16538
2016 (15.6)
687 (19.0)
<0.0001
Cardiogenic shock, n (%)
16760
522 (4.0)
246 (6.7)
<0.0001
16280
10496 (82.6)
3177 (88.9)
<0.0001
Successful thrombolysis, n (%)
1254 (9.8)
228 (6.4)
Failed thrombolysis, n (%)
956 (7.5)
169 (4.7)
Reperfusion strategy
Primary PCI, n (%)
Angiographic characteristics
N
Men
Women
N=13096
N=3664
Coronary lesions <50%
331 (2.5)
96 (2.6)
One vessel disease (%)
5627 (43.0)
1599 (43.7)
Two vessel disease (%)
4081 (31.2)
1111 (30.3)
Three vessel disease (%)
3049 (23.3)
855 (23.3)
Left main stenosis (%)
421 (3.2)
136 (3.7)
p
Coronary artery disease
extension
16749
0.8
0.1
Percutaneous coronary intervention data
N
Men
Women
N=13096
N=3664
p
No Treated lesions mean +/- SD
16328
1.28 (0.60)
1.30 (0.61)
0.4
Primary success %
16326
95.9
94.7
0.002
No of BMS/patient mean +/- SD
16375
1.15 (0.84)
1.14 (0.85)
0.9
No of DES/patient mean +/- SD
15948
0.15 (0.47)
0.14 (0.46)
0.06
PCI of SVG, n (%)
16584
132 (1.0)
28 (0.8)
0.2
In-hospital all cause mortality and
complications
N
Men
Women
N=13096
N=3664
p
In hospital mortality
16358
4.3 (551)
9.8 (350)
<0.0001
Vascular
16536
5.4 (708)
7.9 (289)
<0.001
Transfusion
16514
0.4 (45)
1.2 (42)
<0.0001
Vascular surgery
16514
0.2 (16)
0.2 (7)
0.3
complications
Independent predictors of mortality by multivariate
analysis
OR
[IC]
p
Female gender
Female vs Male
1.29
[1.06 – 1.56]
0.01
Age
Per year
1.06
[1.05 – 1.07]
<0.0001
Diabetes Mellitus
Yes vs no
1.54
[1.25 – 1.90]
<0.0001
Cardiogenic Shock
Yes vs no
19.10
[15.48 – 23.58]
<0.0001
PCI failure
per %
0.26
[0.18 – 0.35]
<0.0001
BMS
no BMS vs at least one BMS
0.76
[0.58 – 1.00]
0.05
DES
No DES vs at least one DES
0.40
[0.26 – 0.61]
<0.0001
Left main
Yes vs no
2.04
[1.50 – 2.79]
<0.0001
Lesion extension
2 and 3 vessel vs one or none
0.58
[0.33 – 1.03]
0.06
Thrombolysis
Failed thrombolysis vs successful
1.80
[1.05 – 3.08]
0.03
In-hospital mortality according to age and
gender
Figure1: In hospital Mortality
Years old
>= 75
16,1 p = .0005
12
7 p = .4
6,2
[65-75[
[55-65[
3
4,5 p = .06
2,4
1,7
< 55
0
Women (n=3573)
Men (n=12751)
p = .2
5
10
15
20
Limitations
• To obtain a high rate of patients with complete data,
the number of clinical and angiographic variables
entered in the database was limited
• Out of hospital mortality is unknown
• Analysis of subgroups in registries is limited by the
observational nature of the analysis. However, the
large number of patients included in our registry
limits this potential bias
• The analysis was limited to patients who were
catheterized within 24 hours of an acute myocardial
infarction and no data is available on patients who
were not reperfused
Conclusion
• Previous studies have demonstrated that female
gender was an independent predictor of in-hospital
mortality after STEMI
• However, PCI was not widely used in these registries
• In our large registry based analysis, in patients
treated with PCI for STEMI, female gender was still an
independent predictor of in-hospital mortality after
STEMI
• There is a clear need for further studies to explain
this difference so that gender inequities in clinical
care can be eliminated