neurorad-neuropath_12-12
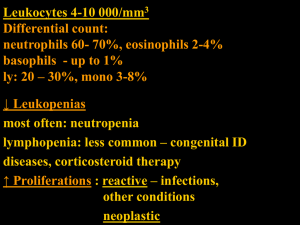
advertisement
Neuroradiology Neuropathology UNC Conference, Dec 2012 Josh Gibson, MD Fellow in Neuroradiology Case 1, History 52-year-old male with history of heart transplant July 2012 Presented in August 2012 with seizure, felt to possibly be related to tacrolimus Imaging at time of admission demonstrated a mass in the fourth ventricle Surgery initially delayed secondary to recent heart transplant Operative findings The lesion was somewhat firm and easily delineated from the surrounding tissues except at the inferior anterior portion where it appeared to be attached to the brainstem with no clear plane. This was initially easily friable at the surface, but otherwise, resected by debulking without significant blood loss. Choroid plexus papilloma • Choroid plexus tumors (CTTs) are rare, with an annual US incidence of one to three cases per 10 million people per year, but they account for up to 20% of pediatric brain tumors arising in the first year of life. • Lateral or third ventricle in children, often under 2 years of age; fourth ventricle or the cerebellopontine angle in adults • Histologically, choroid plexus may be classified as follows: • Choroid plexus papilloma, WHO grade I (60% of CTTs) • Atypical choroid plexus papilloma, WHO grade II (15%) • Choroid plexus carcinoma, WHO grade III (25%) • Chance of recurrence is greater with atypical adenoma or carcinoma • Gross total removal is best chance for cure. Malignant progression is rare. • Children with CPC appear to have a high frequency of TP53 germline mutations in association with Li–Fraumeni Syndrome (LPS). This raises the question whether all children with CPC should be tested for TP53 germline mutations in order to institute screening to enhance early detection and treatment of subsequent cancers. Burger PC and Scheithauer BW, eds. Diagnostic Pathology: Neuropathology. Amirsis Publishing Inc., 2012. Paulus W and Janisch W. Acta Neuropathol (1990) 80:635- 641. Gozali A, et al. Pediatr Blood Cancer 2012;58:905–909. Wolff JE, Finlay JL. Choroid plexus tumors. In: Carroll WL, Finlay JL, editors. Cancer in children and adolescents. Massachusetts: Jones and Bartlett Publishers; 2009. p. 299. Case 2, History 44-year-old female with right flank and low back pain with radiation to the right lower extremity for 2 days Found to have right paraspinal mass on outside CT, transferred to our hospital (CT not available) Pre Gd Post Gd Operative findings Vascular tumor with good plane around the normal anatomy. The mass expanded the foramen. The bone was thinned out and very soft. S100 IHC Melanotic schwannoma • Melanotic schwannoma is a pigmented tumor composed of Schwann cells capable of melanogenesis • Most commonly occur in spinal nerves, cranial nerves, and autonomic nerves • Median age at presentation is 38 years • May be sporadic or associated with Carney complex, which is a multiple neoplasia syndrome characterized by spotty pigmentation, cardiac myxomas, endocrine overactivity, and psammomatous melanotic schwannomas. • Melanotic schwannomas associated with Carney complex typically show psammoma bodies • Aggressive or malignant varieties of melanotic schwannoma comprise about 10–25% of cases Burger PC and Scheithauer BW, eds. Diagnostic Pathology: Neuropathology. Amirsis Publishing Inc., 2012. Arvanitis LD. Pathology – Research and Practice 206 (2010) 716–719. Case 3, History 62-year-old male with history of AML s/p bone marrow transplant in 2010 Had resection of cervical ganglioneuroma in July 2012 and then presented (Sept) with altered mental status and seizures was found to have a new right frontal lobe lesion. Myeloperoxidase IHC Myeloid sarcoma • Myeloid sarcoma is a solid tumor composed of extramedullary (outside the bone marrow) myeloid precursor cells. Previously named “chloroma” due to its greenish hue, a result of the presence of myeloperoxidase, or “granulocytic sarcoma”. • Myeloid sarcoma is often associated with acute myeloid leukemia (AML), chronic myeloid leukemia, or myeloproliferative disorders/myelodysplastic syndrome (MDS). • Myeloid sarcoma may present prior to or along with bone marrow involvement by leukemia. Most commonly occurs concomitantly with AML or as the first sign of relapse of AML. Myeloid sarcoma has been observed in 3–5% of AML. • In 88% of the patients with no evidence of a hematological abnormality at presentation, AML develops within 11 months (range 1–49 months); however, in a small group of patients with myeloid sarcoma, AML never appears. • Almost any organ can be affected, with the most common being skin, lymph nodes, testis and bone. The CNS is rarely affected, accounting for approximately 3% of all cases. • Bone involvement is most frequently seen subperiosteally and is commonly localized in the vertebrae, sternum, orbits, and cranium. • Intracranial myeloid sarcomas usually present as extra-axial masses and are believed to emerge from the bone marrow of the skull. Widhalm G, et al. J Neurosurg 105:916–919, 2006. Bain EE, et al. J Cutan Pathol 2012. Hodges G, et al. 44:573-4, 2012. Case 4, History 43-year-old male presented in October 2012 with 2-3 month history of worsening headaches and blurry vision. Denied weakness, numbness, personality change, and seizures. Operative Findings As we proceeded deeper and deeper into the neoplasm, we did not find an obvious plane that corresponded to the one seen on the imaging. We searched carefully for this, in fact, did not notice any real difference in consistency between the normal white matter and the lesion. Low-grade (grade II) glioma • Seizure is the presenting symptom in more than 80% of patients with LGG. • Median age at presentation was 37 years. • In one series of 1249 grade II gliomas, the histological types were as follows: 24% — astrocytoma 56% — oligodendroglioma 20% — oligoastrocytoma (mixed glioma) • 18% of the LGGs involved the corpus callosum and 5% crossed the midline • “Incidental” LGGs represented 3.7% of the population of adults presenting with LGGs. • Incidence of transformation of a LGG to a high-grade glioma ranges from 17% to 73%, with the timing of this transformation ranging from 2.1 to 10.1 years. • Oligoastrocytoma has an intermediate prognosis relative to astrocytoma & oligodendroglioma. Pallud J, et al. Ann Neurol 68:727–733, 2010. Sanai N, et al. J Neurosurg 115:948–965, 2011 Shaw et al. Neurosurgery 34:577–582, 1994