Cardiac Disorders Endocarditis
advertisement
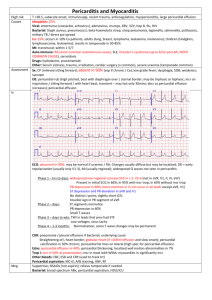
Cardiac Disorders Endocarditis Description: Endocarditis is infection of endocardium or heat valves resulting from invasion of bacteria or other organisms. It may be acute, sub- acute ,or chronic Etiology 1. Causative organisms * Bacteria (eg, Streptococcus viriclans, Staphylococcus aureu * Fungi (eg, Candida albicans, Aspergillus) * Rickettsiae Predisposing factors History of valvular heart disease Prosthetic valve replacement surgery Debilitation Indwelling, catheter placement Prolonged intravenous antibiotic therapy Intravenous drug abuse Dental surgery Path physiology: Ineffective organisms travel through the bloodstream and are deposited on heart valves or other portions of the endocardium.This triggers fibrin and platelet aggregation, which engulfs the organisms, forming friable verrucous vegetations. The vegetations typically form on valves but also may extend to, endocardium.Vegetations covering the valve surface can lead to ulceration and necrosis with subsequent deformity and dysfunction of the valve leaflets. Clinical manifestations 1.Weakness and fatigue 2.Weight loss and anorexia 3.Fever, with chills and diaphoresis 4.Cough 5 .Arthralg 6.Splenomegaly 7.Petechiae of the anterior trunk , and mucosa 8. New heart murmur or a change in an existing murmur, especially in the presence of fever 9- Splinter hemorrhage of nail pad 10.Skin changes such as Roth spots, osler nodes or Janeway lesions Janeway lesion 2. Laboratory and diagnostic study findings a. Blood analysis findings Positive blood cultures for causative organisms Elevated WBC count and erythrocyte Anemia sedimentation rate (ESR) b. Echocardiogram shows valvular damage c. ECG identifies changes indicating arrhythmias and cardiomegaly Nursing management Administer prescribed medications, which include antibiotics Provide ongoing assessment. Monitor temperature at regular intervals. Draw blood for serial cultures to evaluate the effectiveness of therapy. Observe for signs and symptoms of CHF, cerebral vascular complications, and valve stenosis or regurgitation Prepare the client for possible valve replacement/ which greatly improves the prognosis for clients with severely damaged heart valves. Provide client and family teaching : a. Discuss the need for prophylactic antibiotics before dental work , birth; genitourinary, gastrointestinal, or gynecologic procedures procedure or event that can cause transient bacteremia. B. Review signs and symptoms of complications to watch for and report. C. Discuss the need for regular temperature monitoring. Pericarditis Definition: What is pericarditis? Pericarditis is an inflammation of the lining sac surrounds the heart. It can be associated with a collection of fluid (pericardial effusion) in the space between the heart and the Pericardium. Pericarditis accounts for approximately 1 in 1,000 in hospital admission. It is found in about 5% of patients at autopsy. It occurs without symptoms severe enough to come to medical attention. What causes pericarditis? In most patients with pericarditis, no specific cause can be found, and the condition is termed idiopathic pericarditis. Specific diseases known to cause pericarditis. These disease damage the , pericardium, thereby triggering the body's immune defenses to attack pericardium tissue and cause pericarditis. These includes Infections (virus, bacteria, fungus, and tuberculosis) Heart attack that damages the whole thickness of the heart muscle wall Kidney failure, uremia Cancer (usually lung, breast, and lymphoma) Radiation therapy to the chest Trauma involving the chest Drugs, including hydralazine (Apresoline), and phenytoin (Dilantin) Diseases of connective tissue (lupus and rheumatoid arthritis) Cardiac surgery Myxedema cholesterol deposits in the pericardium What is the path physiology of pericarditis? °Acute pericarditis: may be fibrinous or effusion, producing serous or hemorrhagic exudates. Chronic constrictive pericarditis: is marked by progressive pericardial thickening 1. Chest pain is the most common symptom. Chest pain is usually felt behind the breast bone (sternum). The pain is described as sharp, often aggravated by deep breathing or coughing, and worsened by lying down. Onset of pain Varies, may be preceded by "flu-like" symptoms for several days to weeks quality of pain Pleuritic Sharp, stabbing, relived by Sitting up, Shallow breathing and NSAIDs 2. Unlike the chest pain experienced with coronary insufficiency (angina), the pain of pericarditis is constant and unrelated to exertion. 3. Patients often report shortness of breath, in part due to their shallow breathing to minimize chest pain. 4. Patients may also notice weakness, fever, and chills. Additional symptoms are often due to the underlying disease process. 5. Fast heart rhythms (tachycardia). 6. Rarely the patients develop rapid accumulation of fluid in the pericardial sac .. This fluid causes compression of the heart muscle chambers, thereby limiting the amount of blood pumped to the rest of body and causing shock. This lifethreatening condition, called pericardial tamponade,' can occur in up to 15% of patients with percarditis The doctor notes the symptoms of chest pain and examines the chest area. Further evaluation can include chest x-ray, ECG, and echocardiogram, as well as consideration of any underlying predisposing disease processes. When a stethoscope is placed on the chest, a scratchy, rubbing sound (pericardial rub) can sometimes be heard with each heart beat. This is believed to come from the friction of the inflamed pericardial sac rubbing against the beating heart. A pencardial rub can be heard in about 50 to 75% of patients with pericarditis. When a sizable fluid collection (pericardial effusion) is present, the chest x-ray shows an enlarged heart shadow, often with a more circular configuration than normal. An echocardiograrm:This test is useful in detecting and measuring the amount of fluid around the heart and assessing the effect of this fluid on the heart chambers. Since not all patients with pericarditis develop pericardial fluid, an echocardiogram cannot be used alone in making the diagnosis. Blood tests for underlying diseases, such as lupus and rheumatoid arthritis are evaluated. Skin tests can be performed to detect tuberculosis and other fungal infections. When pericardial tamponade causes low blood pressure or shock, a needle can be used to withdraw fluid from the pericardial space Removal of the fluid relieves pericardial tamponade, , reverses shock, and improves blood pressure. The aspirated fluid can be examined for infection and cancer How is pericarditis treated? When the cause of the pericarditis is known, treatment is directed toward the underlying disease. For example, if bacteria are found in the pericardial fluid,(intravenouse antibiotic given. When systemic diseases such as lupus and rheumatoid arthritis are responsible for the pericarditis, anti-inflammatory drugs and medications that suppress the immune system. Idiopathic pericarditis and pericarditis following heart surgery usually respond to no steroidal anti-inflammatory drugs such as aspirin ,ibuproden. When the pain is not controlled with these drugs, corticosteroids , Prednsone an be used and are generally effective. Corticosteroids have powerful anti-inflammatory effects. Unfortunately, long term use of corticosteroids can lead to side ' effects such as one bone thinning ,high blood pressure increase blood sugar, It usually given in large doses daily until symptoms resolve, and then rapidly tapered over 7 to 14 days. When the treatment of pericarditis is successful, the inflammation and any pericardial fluid usually resolve over 2 to 6 weeks. Patients are often initially hospitalized for 24 to 48 hours to exclude a possible heart attack or infectious condition Blood thinning medications (anticoagulants)] are generally avoided in patients with pericarditis in order to minimize the risk of bleeding into the pericardial sac, thereby causing tamponade. In rare cases, scarring of the pericardial sac around the heart causes constrictive pericarditis. In this condition, the scarred pericardial sac causes constriction of heart chambers, leading to impaired heart pumping similar to tamponade. Surgical removal of the constricting pericardial sac may be needed to improve symptoms.