Example Case Write-Pericarditis

Example Case Write-Up
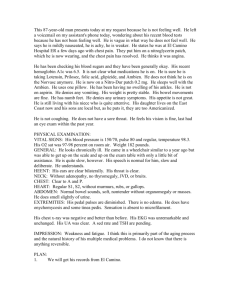
CC: “I feel like crap and my chest hurts.”
HPI: 58-year-old gentleman who arrived to the emergency department with complaints of flu-like symptoms for approximately 1 week with the onset of chest pain today. The patient states he was initially evaluated at the
Taylorsville InstaCare for his flu-like symptoms and chest pain. The patient stated that he had been experiencing nausea, vomiting, and fever as well as general malaise and muscle aches. The chest pain started abruptly this AM and he described it as intermittent, left-sided, sharp, and worse when lying flat. At the InstaCare, the patient was given 3 liters NS and had a chest x-ray and an EKG done. The patient's EKG was noted to be abnormal with some
ST-segment elevations. He was, therefore, told to come to the emergency department for further workup. Mr.
Dalton was not complaining of any chest pain in the ED, but stated that when he arrived, he had an episode of chest pain while in the parking lot and had a hard time walking from his car here to the emergency department due to feeling very "winded and exhausted." In addition he reports intermittent SOB and diaphoresis with exertion.
Meds: Daily ASA
NKDA
PMHx: No significant medical problems, no history of heart conditions, no history of DVTs or PEs
PSHx: none
Social Hx: A resident of Texas here working temporarily. Denies any H/O of tobacco, alcohol, or drug use.
Family Hx: Father with coronary artery disease
PE:
VITAL SIGNS: T36.3, P109, RR16, BP147/86, SPO2 93% on 2 L of oxygen.
GENERAL: ill-appearing adult male, slightly pale and diaphoretic
HEENT: Normocephalic. Sclerae are nonicteric. His oropharynx is moist and pink.
NECK: Supple, without JVD.
LUNGS: CTA B
HEART: Tachycardic no M/G/R appreciated, no friction rub appreciated
ABDOMEN: Soft, nondistended, and nontender.
RECTAL: Stools are brown and Hemoccult negative.
EXTREMITIES: Without cyanosis, clubbing, or edema.
SKIN: Warm and dry.
NEUROLOGIC: A&O times 3
Differential Diagnosis:
1. Acute Coronary Syndrome
2. Pulmonary embolus.
3. Influenza with atypical chest pain
4. Pericarditis.
5. Myocarditis
EMERGENCY DEPARTMENT COURSE: An EKG showed sinus tachycardia with ventricular rate of 112. There were also noted to be ST-segment elevations in leads
V2, V3 as well as V4 and V5 with PR depressions in the same leads. (attached EKG)
A Chest X-ray showed no evidence of pulmonary infiltrates or consolidation. A bedside TTE was done which showed an ejection fraction of 50% and a moderate pericardial effusion with no evidence of tamponade physiology.
LABORATORY DATA: Showed a white count of 12.3, hemoglobin of 16.9, hematocrit of
49.7. CMP was within normal limits. Creatinine was 0.9. Cardiac enzymes were noted to be abnormal. CK was normal at 187. CK-MB was high at 10.9 as was the
CK-MB index at 5.8. Troponin was also elevated at 1.38. He was negative for influenza. Urine was negative for any signs of infection.
Disposition and Diagnosis: Admitted to cardiology with presumed diagnosis of viral pericarditis. He was started on Metoprolol and Prednisone 20mg. The patient’s condition improved and he was discharged home after 3 days once his EKG had normalized. He was to follow-up within 2 days for repeat physical exam and in one week for repeat EKG and cardiac ultrasound.
Pericarditis: Pericardial inflammation due to an infectious cause is most often viral in nature. Occasionally the myocardium can become involved causing myopericarditis. Viral agents known to cause pericarditis include
Influenza, Parainfluenza, Coxsackie, Echovirus, EBV, Hep B, and HIV. The most common symptom is retrosternal chest pain described as sharp or stabbing. The chest pain may be aggravated by deep inspiration and is typically more severe when the patient supine and relieved by sitting up. Associated symptoms include low-grade fever, dyspnea, and dysphagia. A pericardial friction rub is the most common physical exam finding but may be hard to appreciate, especially in a noisy ED.
There are several ECG findings that can help point to the diagnosis of pericarditis and are divided into four stages:
Stage 1: usually seen with onset of pain, diffuse ST elev except AVR and V1 and PR depression. Stage 2: sev days later with return of ST seg to baseline and inversion of T waves. Stage3: inverted T waves. Stage 4: return to baseline. A pericardial effusion can develop during the course of pericarditis and tamponade physiology can develop if the effusion collects quickly enough.
Treatment is mostly supportive and viral pericarditis will usually respond to NSAIDs for 7 days to 3 weeks. If myopericarditis is suspected, treatment with steroids may be warranted and patients should be hospitalized in order to monitor for signs and symptoms of CHF.
Tintinalli, J. Emergency Medicine A Comprehensive Study Guide. 6 th ed. The McGraw-Hil Companies, Inc. 2004.
Journal Articles: (2 is enough but you can put more than 2 if you like)
1) Demangone, D. ECG Manifestation of Noncoronary Heart Disease. Emerg Med Clinics of North America 2006;
24(1): 113-31.
2) Butler, K. Chest Pain: A Clinical Assessment. Radiologic Clinics of North Amercia 2006; 44(2): 160-79.
3) Shih-Hung, T. et al. Use and Interpretation of Cardiac Troponins in the Emergency Department. American Journal of Emergency Medicine 2008; 26(3): 331-41.