Pharmacology of the CVS: Angina (Physiology)
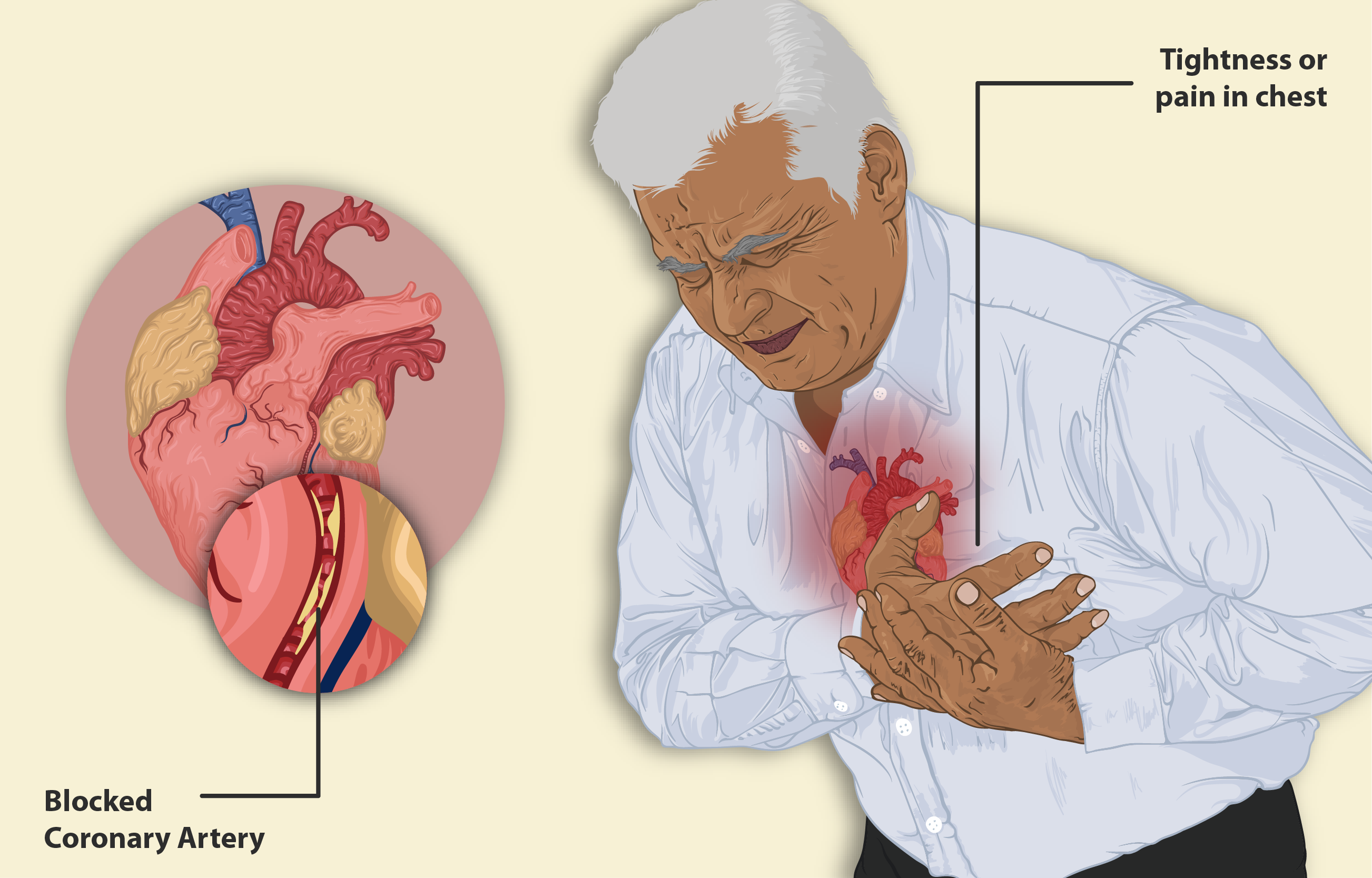
Session summary Angina pectoris means strangulation of the chest. This is because one of the symptoms of Angina is a feeling of pain and tightness in the chest. It is an important condition with over 3 million sufferers and is caused by local myocardial ischemia. The causes, symptoms and treatment will be explored as a means of revising consolidating the material presented in the cardiovascular lectures so far.
-
What is the definition of angina pectoris? (2)
★ Angina: Derived from the Latin verb "angere," meaning "to choke or throttle"
★ Pectoris: Refers to the Latin "pectus," meaning "breast" or "chest"
-
What are the symptoms of angina pectoris? (3)
★ Feeling of cramping and severe constriction in the chest
★ Referred pain to jaw, shoulders, neck, and arms
★ May be associated with shortness of breath, sweating, nausea, and increased heart rate
-
What causes the pain symptoms in angina pectoris? (2)
★ Ischaemia: Reduced blood flow to the myocardium
★ Locally affected myocardium releases various compounds, including potassium, lactate, adenosine, bradykinin, and prostaglandins
-
How does the activation of myocardial pain receptors lead to pain perception in angina pectoris? (3)
★ Activation of myocardial pain receptors by released compounds
★ Transmission of signals via sensory neurons (cardiac nerves and upper posterior nerve roots) to the brain
★ Perception of pain in the brain
-
What is the prevalence of chronic stable angina pectoris in Western countries? (2)
★ Affects around 2-4% of the population in Western countries
★ Associated with an estimated annual risk of death and non-fatal myocardial infarction (MI) of 1-2% and 3%, respectively
-
How many people in the UK are estimated to be living with angina, and what is the gender distribution? (2)
★ Estimated that 1.3 million people in the UK are living with angina
★ Approximately 775,000 men and 560,000 women are affected
-
What is angina an important sign of?
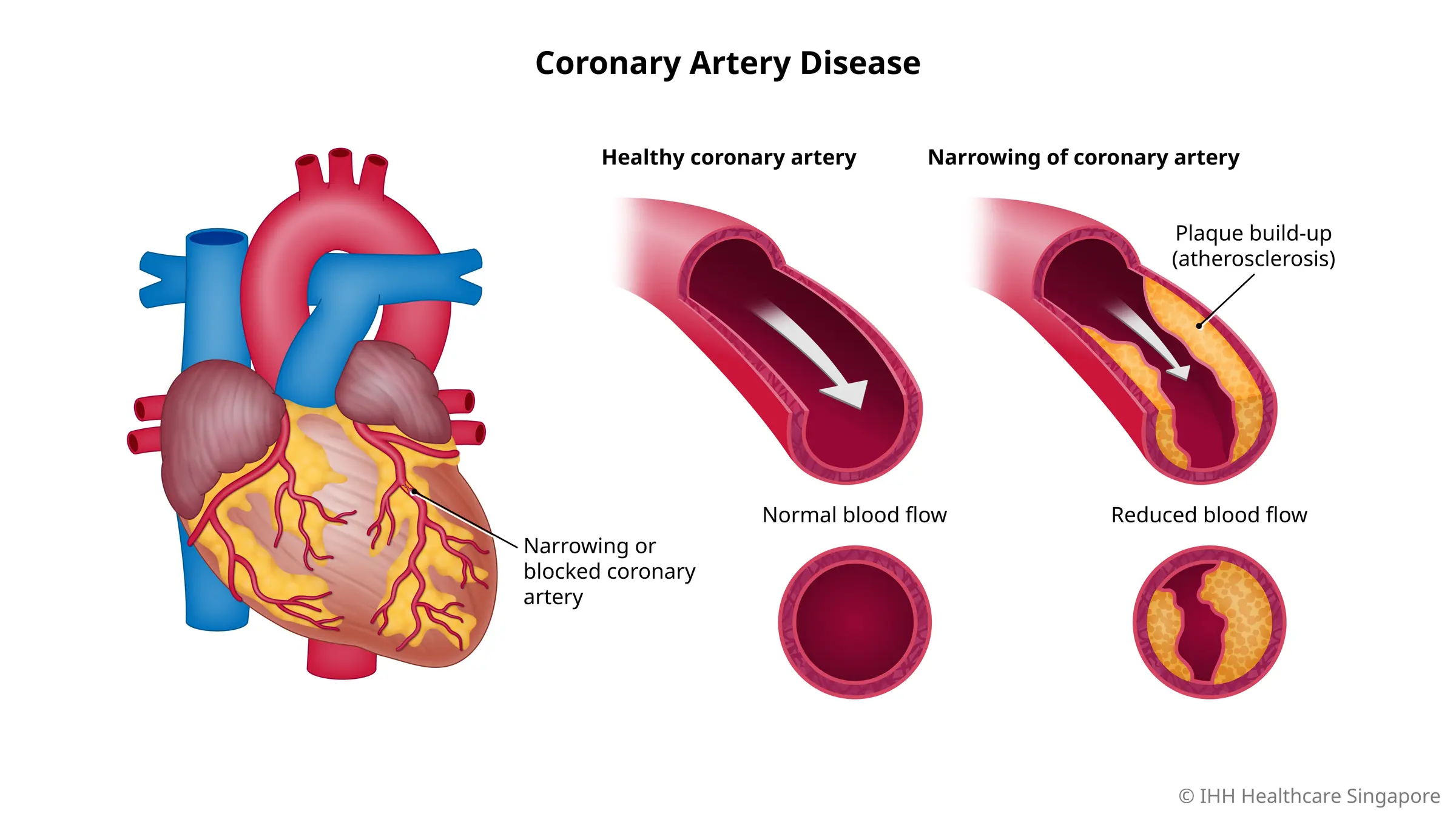
★ Angina is an important sign of Coronary Heart Disease (CHD), also known as Ischaemic Heart Disease (IHD)
-
What are the traditional classifications of angina based on the patient's chest pain symptoms? (3)
★ Typical angina: Substernal chest discomfort of characteristic quality and duration, provoked by exertion or emotional stress, relieved by rest and/or nitrates within minutes
★ Atypical angina: Presentation of two of the typical angina characteristics
★ Non-anginal: Presentation of only one or none of the chest pain characteristics
-
What are the classifications of angina based on aetiology and chest pain symptoms in the new classification? (4) REMEMBER 'SUPM'
★ Stable Angina: Attributed to myocardial ischaemia and coronary artery disease
★ Unstable Angina: Due to complications from stable angina.
★ Prinzmetal Angina (Angina Inversa): Usually due to a spasm in the coronary arteries, tends to happen in cycles, and cocaine use is a leading cause of coronary vasospasms
★ Microvascular Angina: Patients have angina symptoms but no evidence of coronary artery disease; normal or near-normal coronary angiogram
-
What is the aetiology of stable angina? (3)
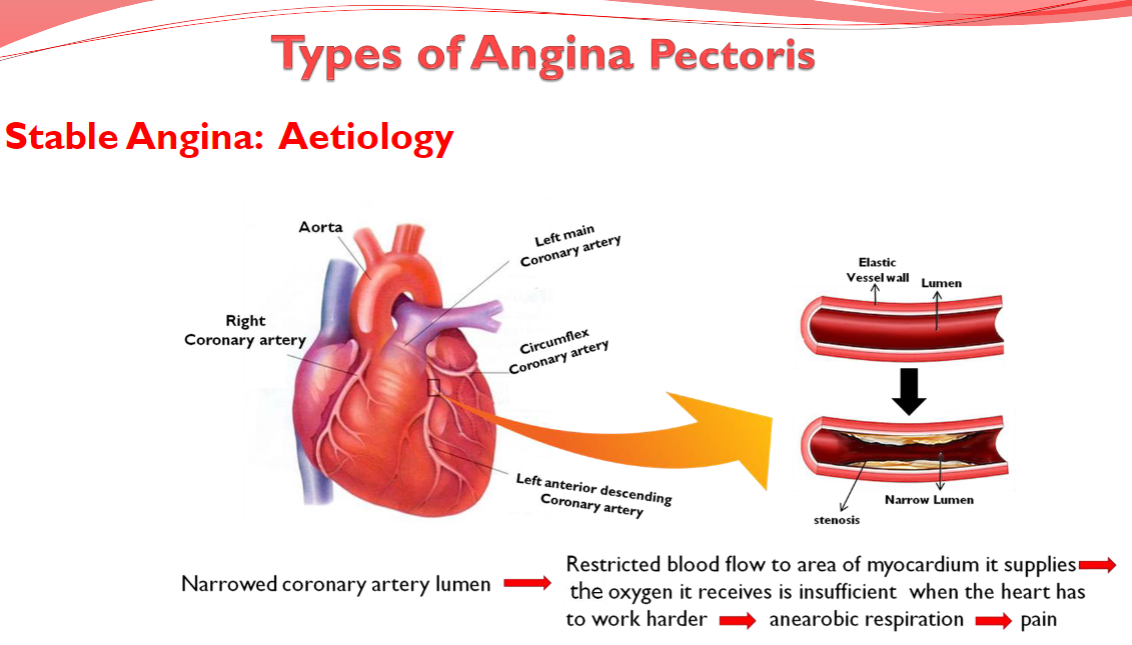
★ Narrowed coronary artery lumen leads to restricted blood flow to the area of myocardium it supplies
★ The oxygen it receives is insufficient when the heart has to work harder, leading to anaerobic respiration
★ Anaerobic respiration leads to pain
-
What are the characteristics of stable angina (classic, typical)? (5)
★ Follows a set pattern and is predictable; recurrent episodes tend to have a similar onset pattern, duration, and intensity
★ Short duration radiation of pain to the left arm, neck, jaw, or back; builds to a peak and lasts 2–5 minutes
★ Precipitated by exertion or increased cardiac oxygen demand, such as walking uphill, climbing stairs, exercise, emotional stress, or exposure to cold
★ Not life-threatening but can be a warning sign for something serious, such as a heart attack or stroke
★ Relieved by rest or taking medications. Symptoms are attributed to myocardial ischaemia
-
What is the aetiology of unstable angina? (3)
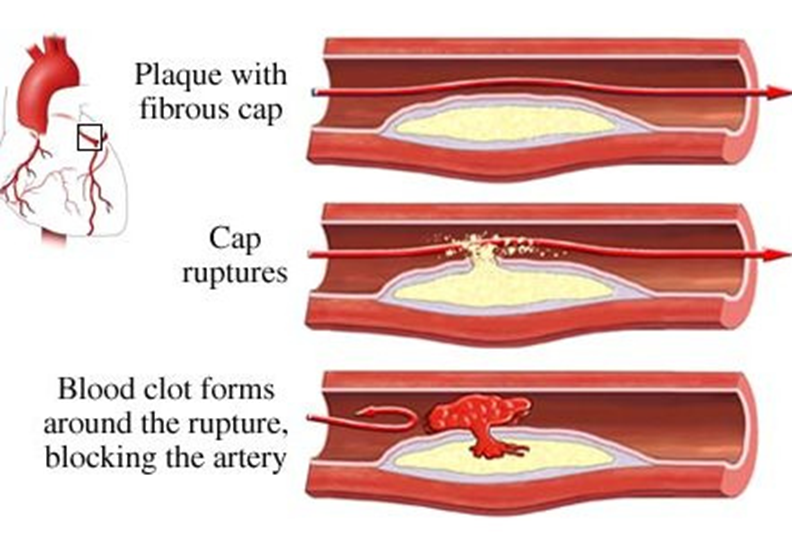
★ Clot formation occludes the artery (e.g., following plaque rupture), leading to critical reduction in blood flow.
★ Oxygen supply becomes inadequate even at rest.
★ This inadequate oxygen supply leads to pain
-
What are the characteristics of unstable angina? (6)
★ Unpredictable occurrence
★ Pain symptoms are more severe, can persist, and last longer
★ Can happen at rest with little exertion and may not have a trigger
★ Not usually relieved by rest and medications
★ Progression from stable angina is impossible to predict.
★ Regarded as a serious emergency, and patients are advised to go to the hospital
-
What is the aetiology of Prinzmetal Angina? (3)
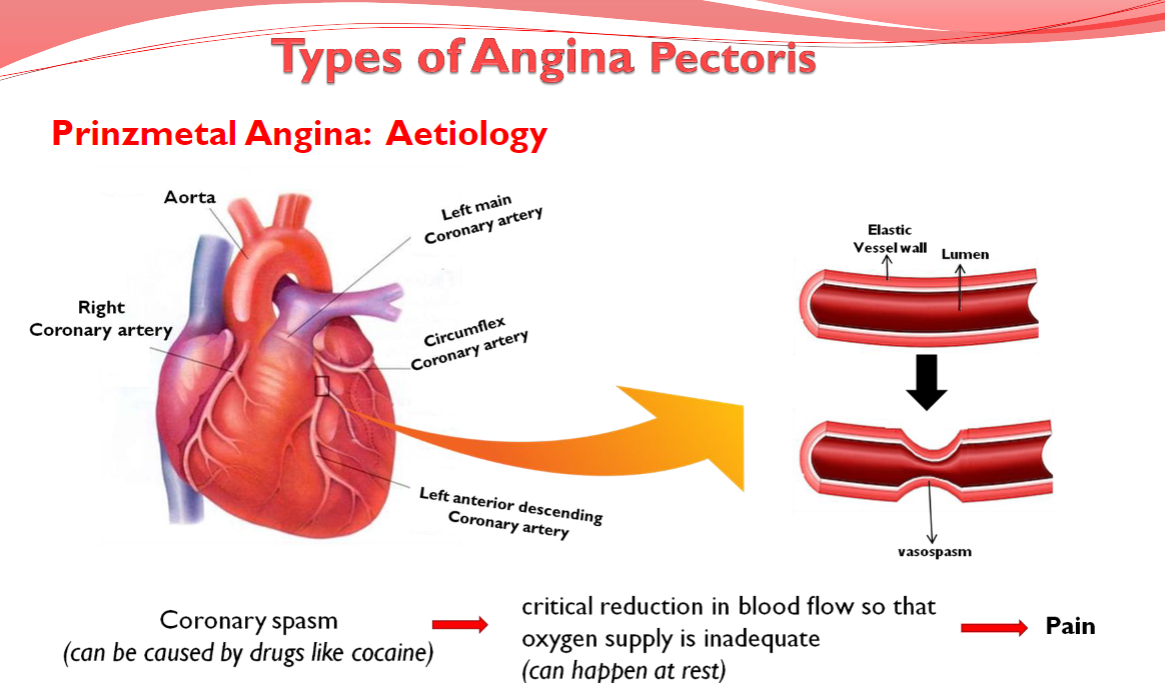
★ Coronary spasm
(can be caused by drugs like cocaine)
★ Critical reduction in blood flow so that
oxygen supply is inadequate
(can happen at rest)
★ Pain
-
What are the Types of Angina Pectoris: (3)
★ Stable Angina
★ Unstable Angina
★ Variant Angina (Prinzmetal Angina)
-
What are the Characteristics of Prinzmetal Angina (Variant Angina): (10)
★ Occurs while resting and during the night or early morning hours
★ Episodes last around 5 to 15 minutes (longer in some cases)
★ Rare (1 in 100 Angina cases)
★ Typically seen in younger patients
★ Attacks are severe and described as very painful
★ Pain may radiate from the chest to the head, shoulder, or arm
★ Associated symptoms include heartburn, nausea, sweating, dizziness, palpitations, migraines, and Raynaud's phenomenon
★ Often due to a spasm in the coronary arteries and tends to come in cycles
★ Cocaine use is a leading cause of coronary vasospasms
★ Can be relieved by taking medication
-
What is the aetiology of microvascular Angina? (3)
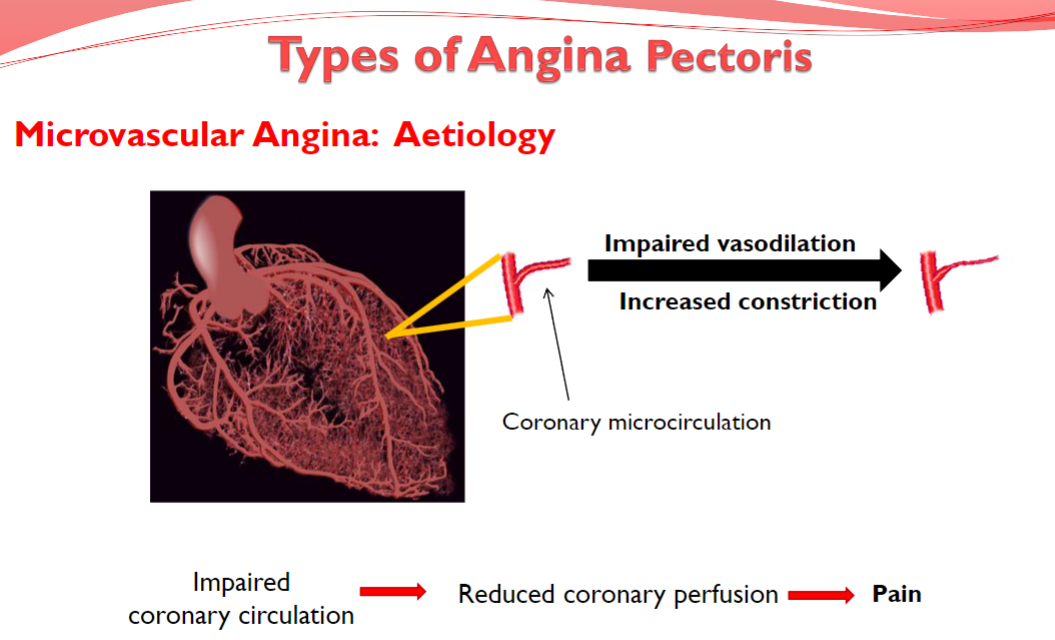
-Increased constriction
-Impaired vasodilation
-Pain
-
What are the types of angina pectoris? (4)
★ Stable Angina
★ Unstable Angina
★ Variant Angina (Prinzmetal Angina)
★ Microvascular Angina (Cardiac Syndrome X)
-
What are the characteristics of Microvascular Angina (Cardiac Syndrome X)? (6)
★ Impaired coronary circulation due to coronary microvascular dysfunction from abnormal vasodilation or increased vasoconstriction
★ Patients do not have obstructive coronary artery disease
★ Occurs with exertion and at rest but may respond less well to nitrates
★ Problem diagnosing it early as coronary microvasculature (vessels <300 um in diameter) cannot be directly imaged in vivo
★ Positron emission tomography (PET) or cardiac magnetic resonance (CMR) can be used to assess coronary microvascular blood flow
★ Treatment will vary depending on the cause of the microvascular angina
-
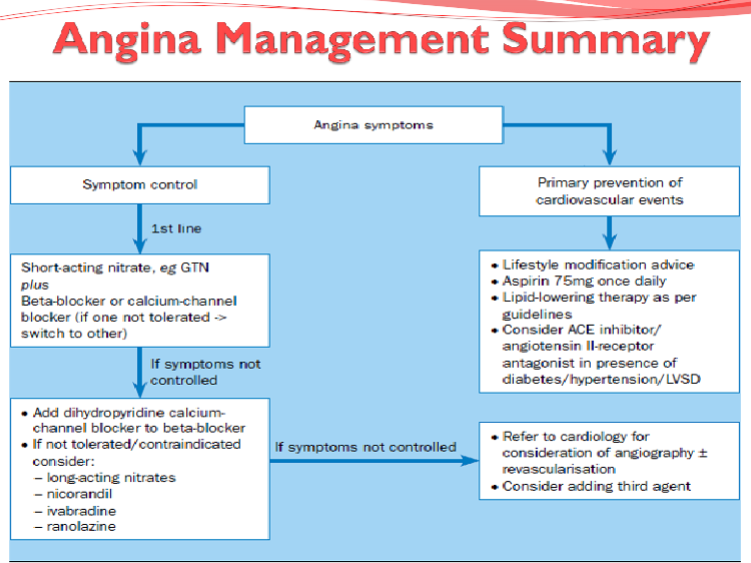
What are the treatment aims? (3)
★ To enhance quality of life through reduction of symptoms
★ To improve prognosis and prevent complications such as MI (Myocardial Infarction) and premature death
★ To be well tolerated and cause minimal side effects
-
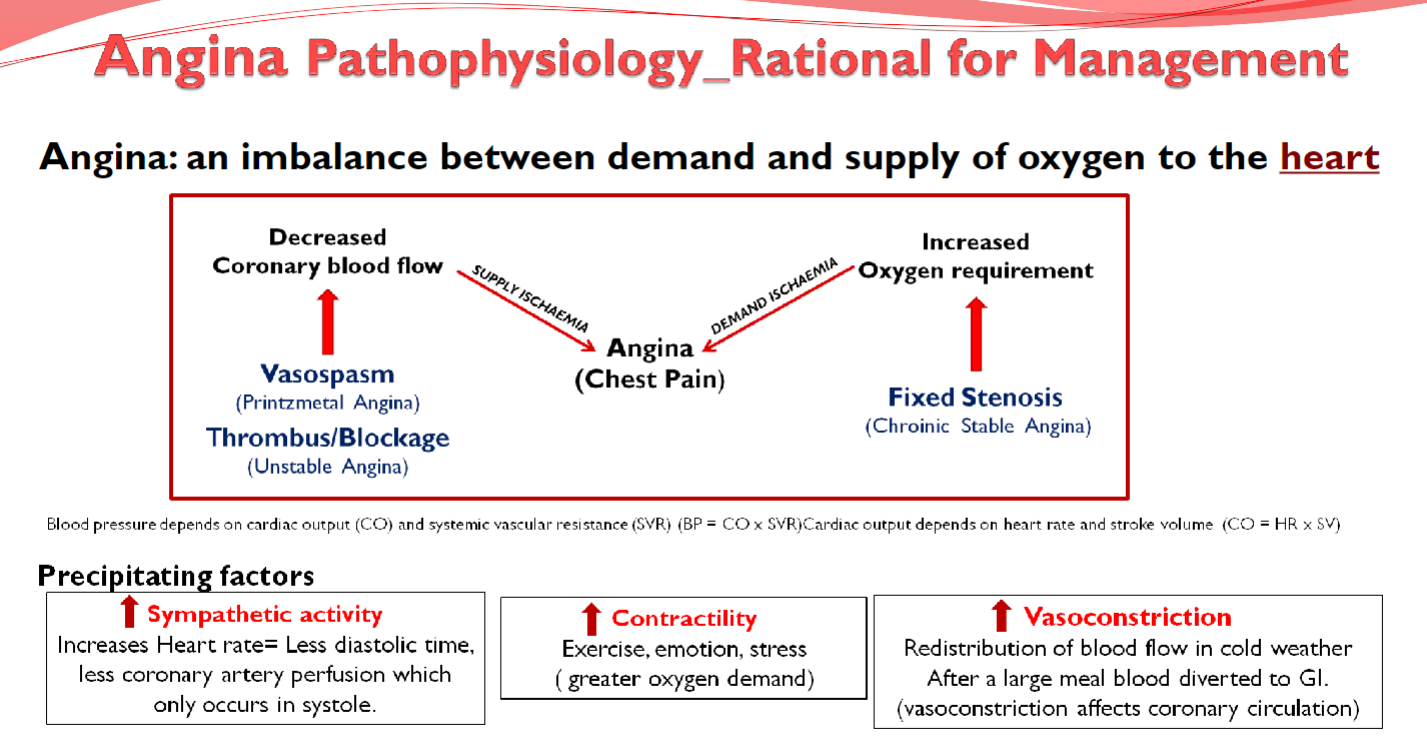
Picture demonstrating Angina Pathophysiology:
-
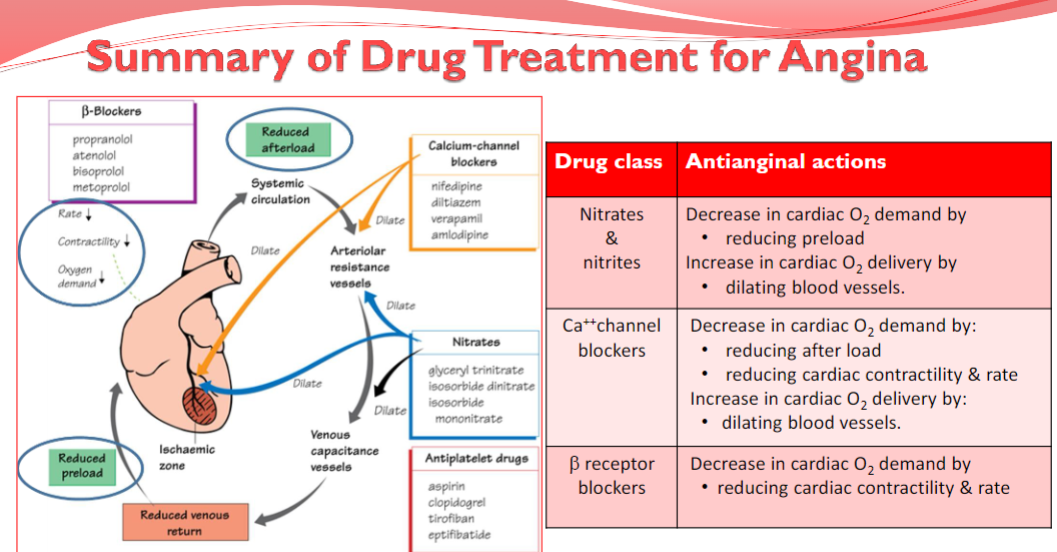
What are the treatment strategies for angina?
To improve perfusion:
Increase Oxygen Delivery by improving coronary blood flow using coronary vasodilators.
To reduce metabolic demand: (3)
-Reduce Oxygen Demand by decreasing cardiac work using:
-Vasodilators to reduce afterload and preload.
-Cardiac depressants to reduce heart rate and contractility.
Prevention: (3)
Prophylactic measures to reduce the risk of subsequent episodes, including:
Lipid Lowering Drugs
Anti-Coagulants
Fibrinolytic Anti-platelet treatments
-
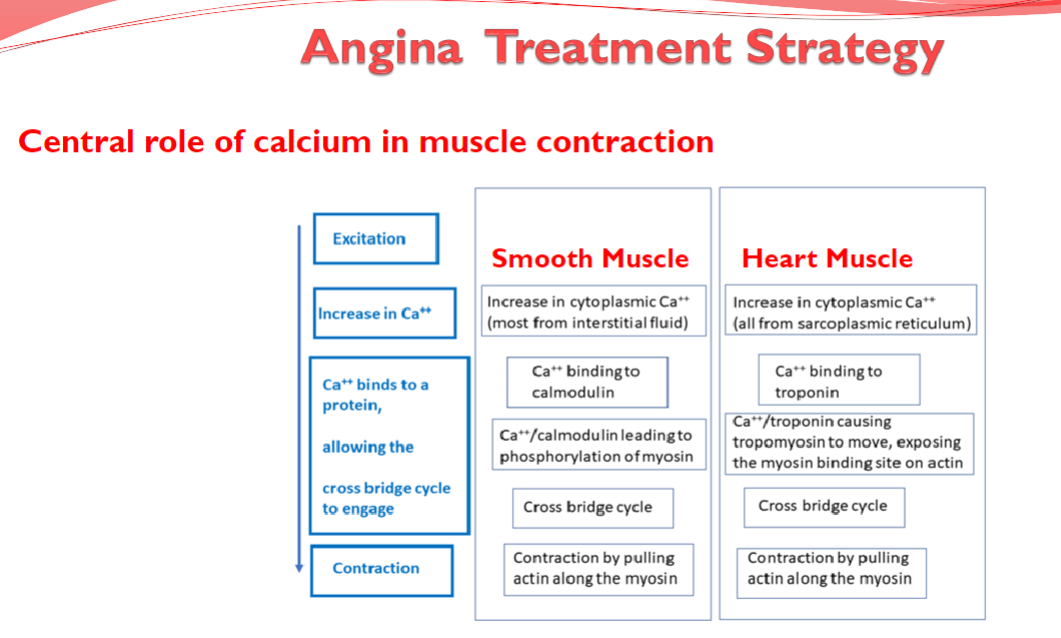
Picture demonstrating another angina treatment strategy related to Ca2+
-
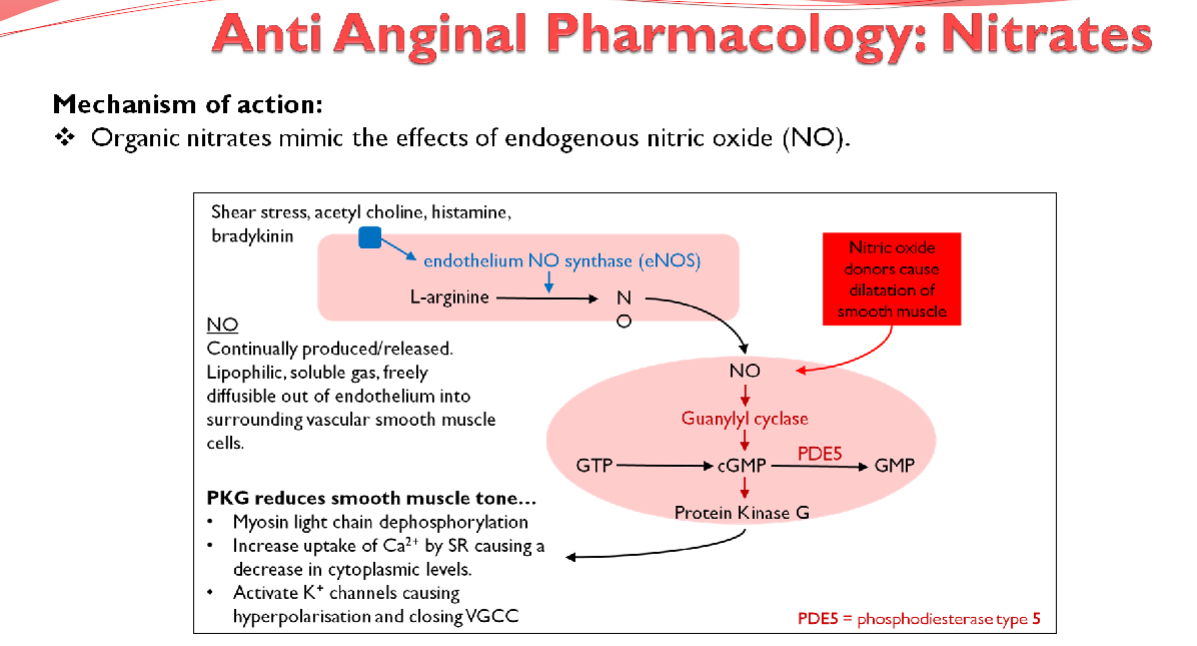
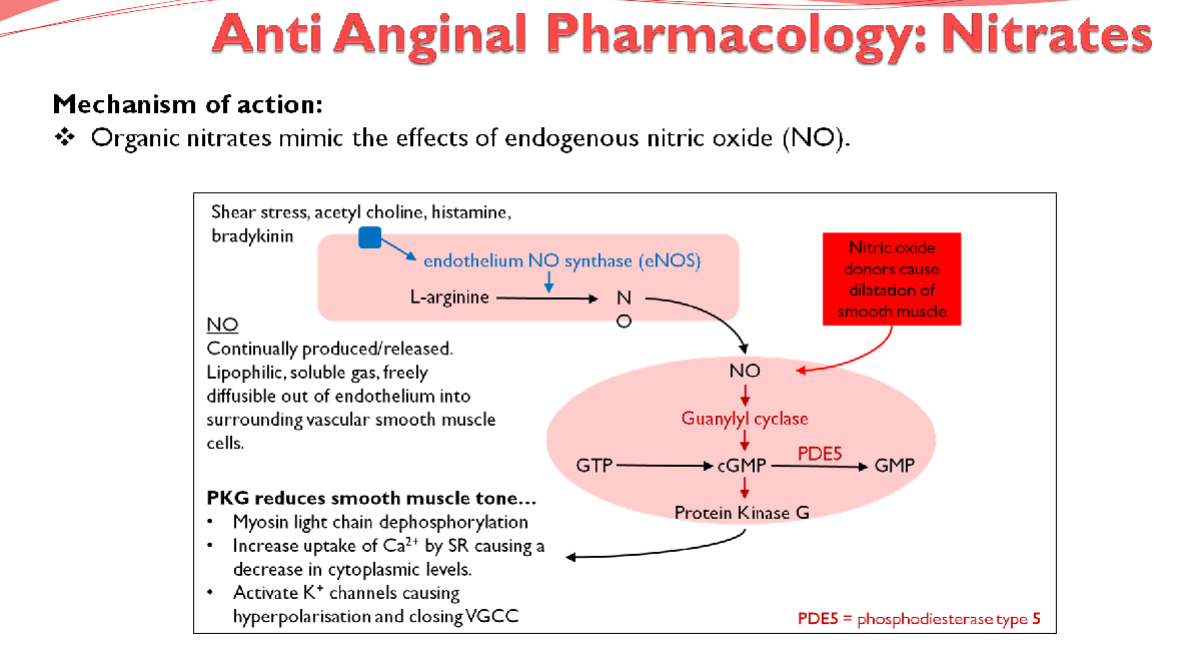
What are examples of nitrates used in anti-anginal therapy? (2)
★ Glyceryl Trinitrate (GTN)
★ Isosorbide Mononitrate
-
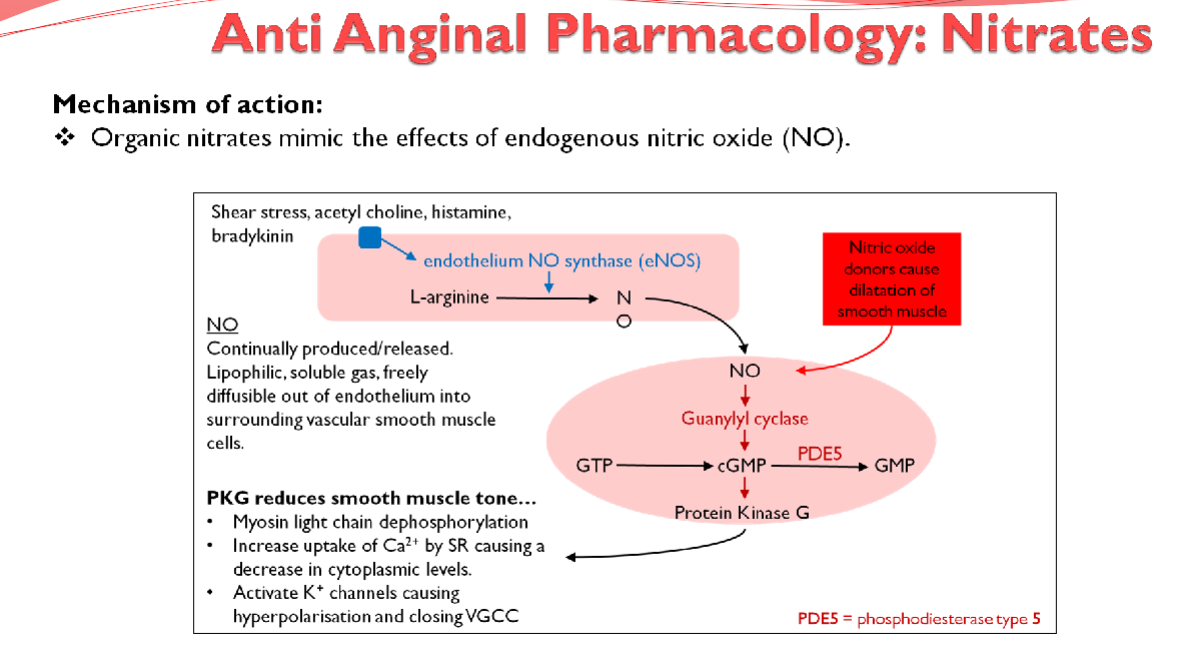
What are the effects of nitrates on the cardiovascular system? (3)
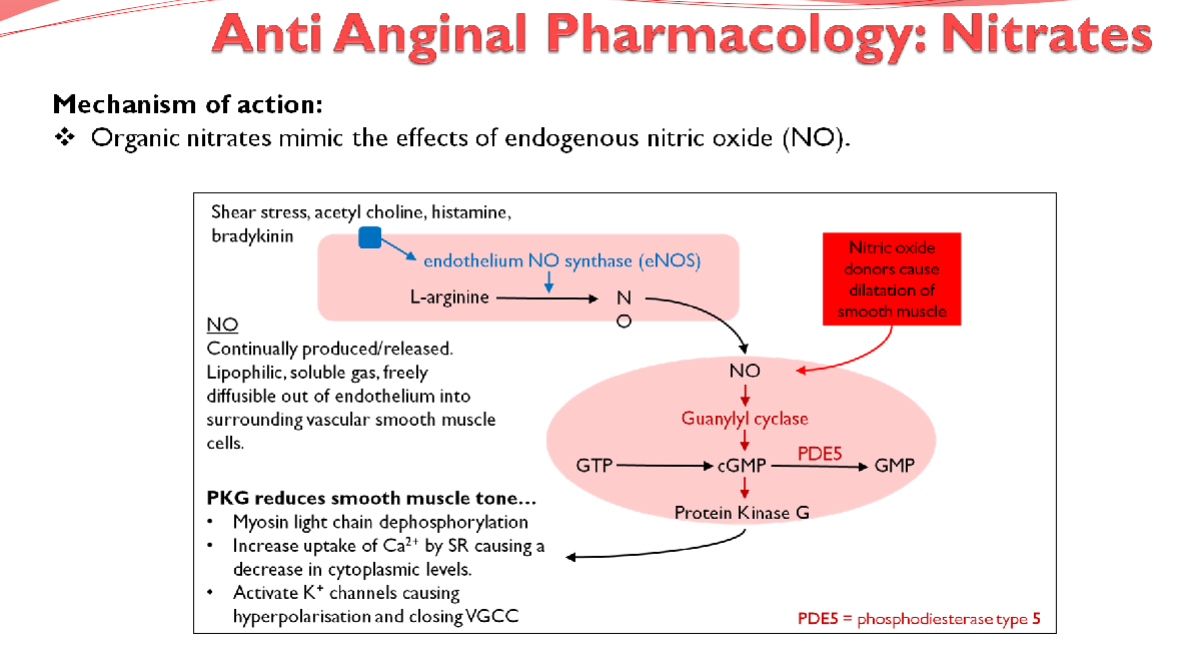
★ Peripheral Venodilation: decreases intraventricular pressure, reducing cardiac preload
★ Arterial Dilation: decreases total peripheral resistance (TPR), thereby reducing afterload
★ Both actions lower oxygen demand by decreasing the work of the heart
-
What is the effect of nitrates on coronary vessels affected by atherosclerosis? (1)
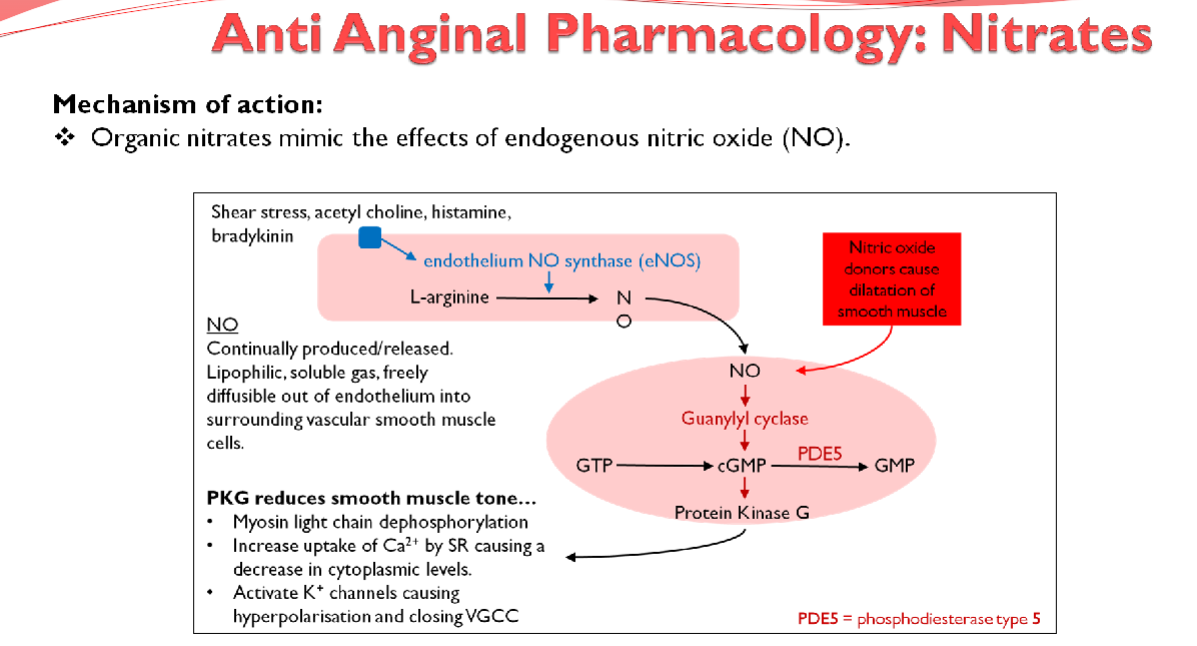
Limited effect on coronary vessels affected by atherosclerosis
-
What are the adverse effects associated with nitrates? (3)
★ Throbbing headache, flushing, and syncope (Arterial dilation)
★ Postural hypotension (Venodilation)
★ Reflex tachycardia (Sympathetic outflow)
-
Picture demonstrating the mechanism of action of anti-anginal pharmacology; Nitrates
-
What are examples of beta-blockers used in anti-anginal therapy? (2)

★ Atenolol
★ Bisoprolol
-
What are the effects of beta-blockers on the cardiovascular system? (4)
★ Inhibits If (Intrinsic Frequency) pacemaker current in the sinoatrial node (AV conduction)
★ Reduces the force of cardiac contractions, improving exercise tolerance
★ Both actions reduce cardiac output and lower blood pressure
★ Slower heart rate lengthens diastole, providing more time for coronary perfusion, effectively improving myocardial oxygen supply
-
What are the adverse effects associated with beta-blockers? (3)
★ Bronchospasm
★ Fatigue
★ Postural hypotension
-
What are the contraindications for beta-blockers? (2)
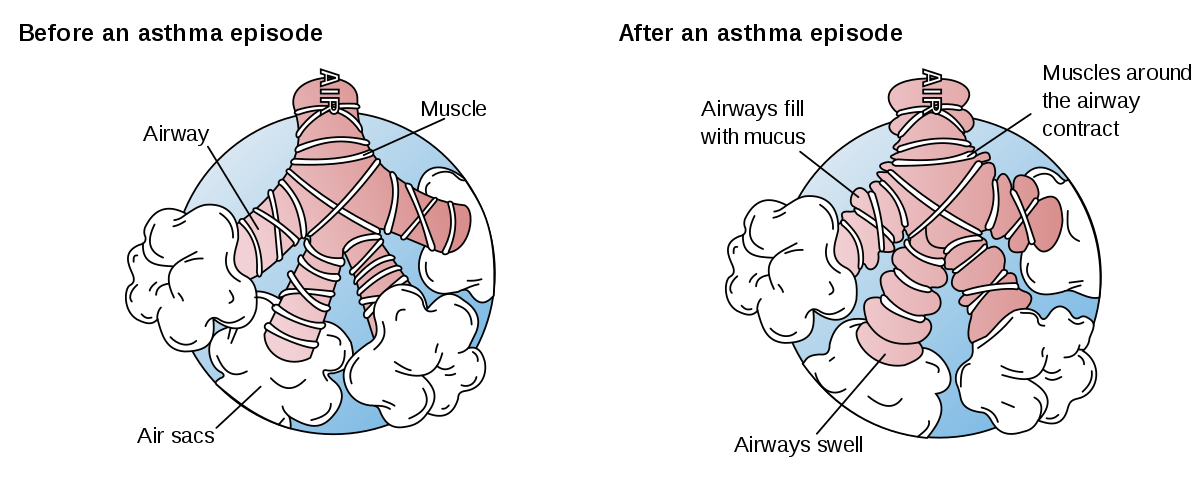
★ Asthma: Blocking B2 receptors can cause constriction and bronchospasm
★ Heart block where atrial-ventricular conduction is poor: may block AV node, further decreasing heart rate
-
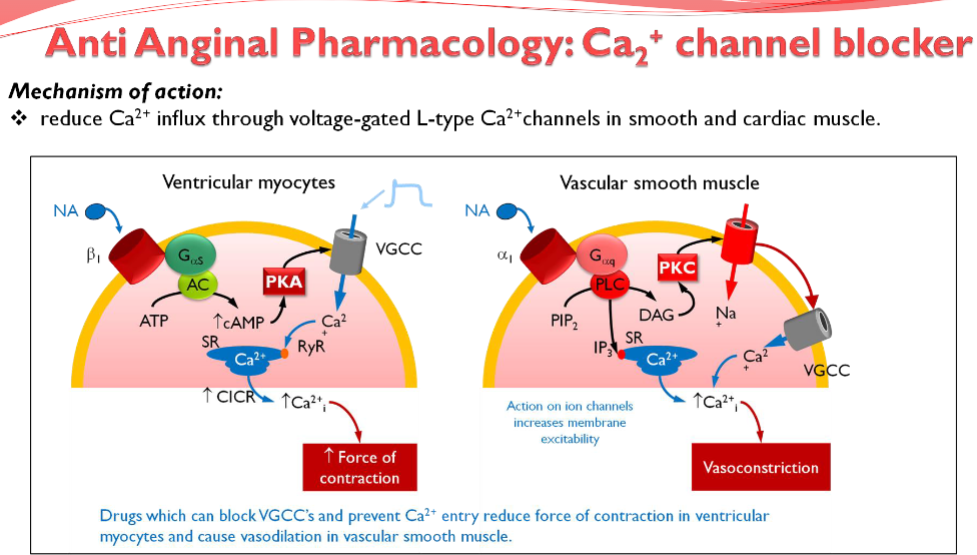
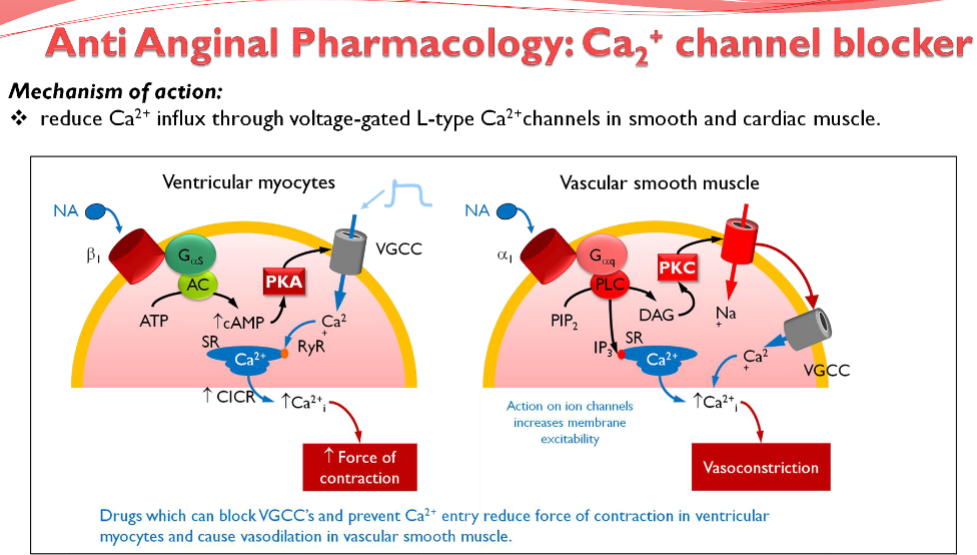
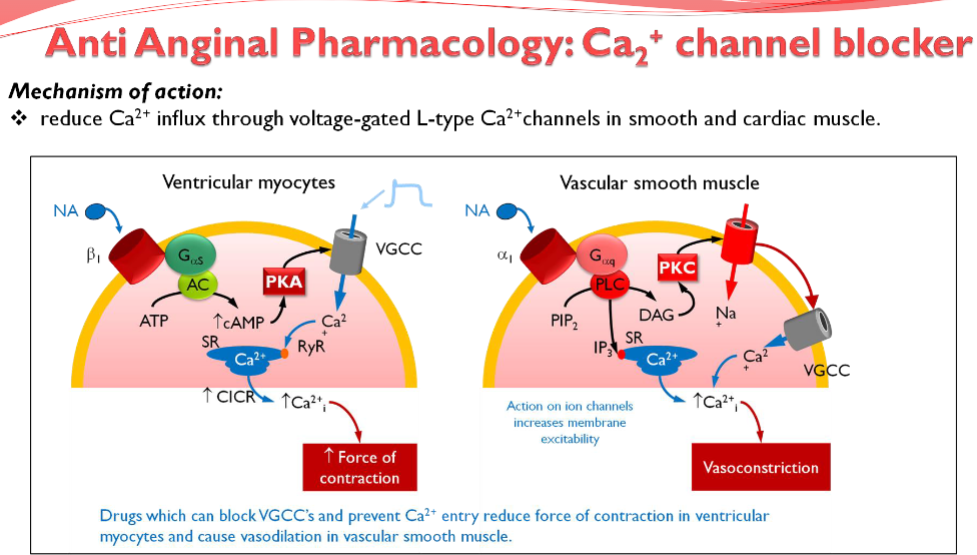
Picture demonstrating the mechanism of action of anti-anginal pharmacology; Ca2+ channel blocker
-
What is the mechanism of action of aspirin in the prophylactic treatment of angina? (2)
★ Inhibits COX enzyme (cyclooxygenase), thereby inhibiting the production of thromboxane A2
★ Inhibits platelet aggregation, including the expression of GP IIb/IIIa
-
What is the mechanism of action of clopidogrel in the prophylactic treatment of angina? (2)
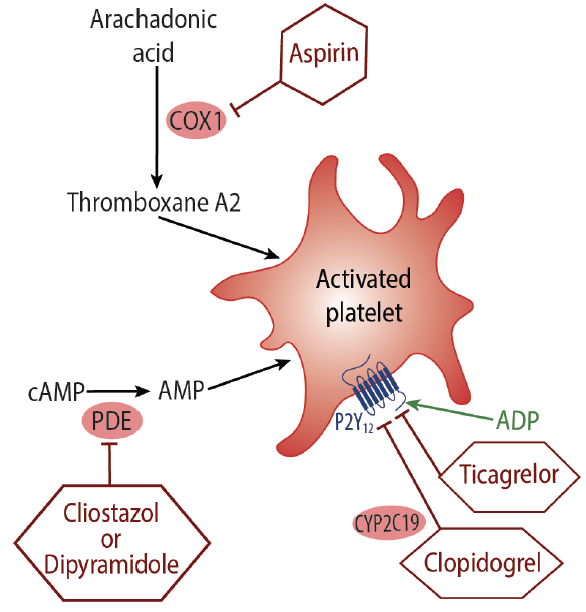
★ Inhibits ADP receptor on platelets
★ Reduces platelet aggregation
-
How do aspirin and clopidogrel act together in reducing thrombosis? (1)

Both drugs reduce thrombosis through entirely different mechanisms, allowing them to be used together effectively.
-
What is the mechanism of action of statins in the prophylactic treatment of angina? (2)
★ HMG Co-A reductase inhibitor
★ Lowers cholesterol levels
-
Picture demonstrating a summary of Drug Treatment:
-
What is the mechanism of action of Nicorandil in the treatment of angina? (3)

★ Potassium channel activator, leading to hyperpolarization
★ Blocks voltage-gated calcium channels (VGCCs) and reduces Ca2+ entry
★ Induces coronary vasodilation; it also has a nitrate moiety, contributing to its vasodilator action via the generation of nitric oxide (NO)
-
What is the mechanism of action of Ivabradine in the treatment of angina? (2)
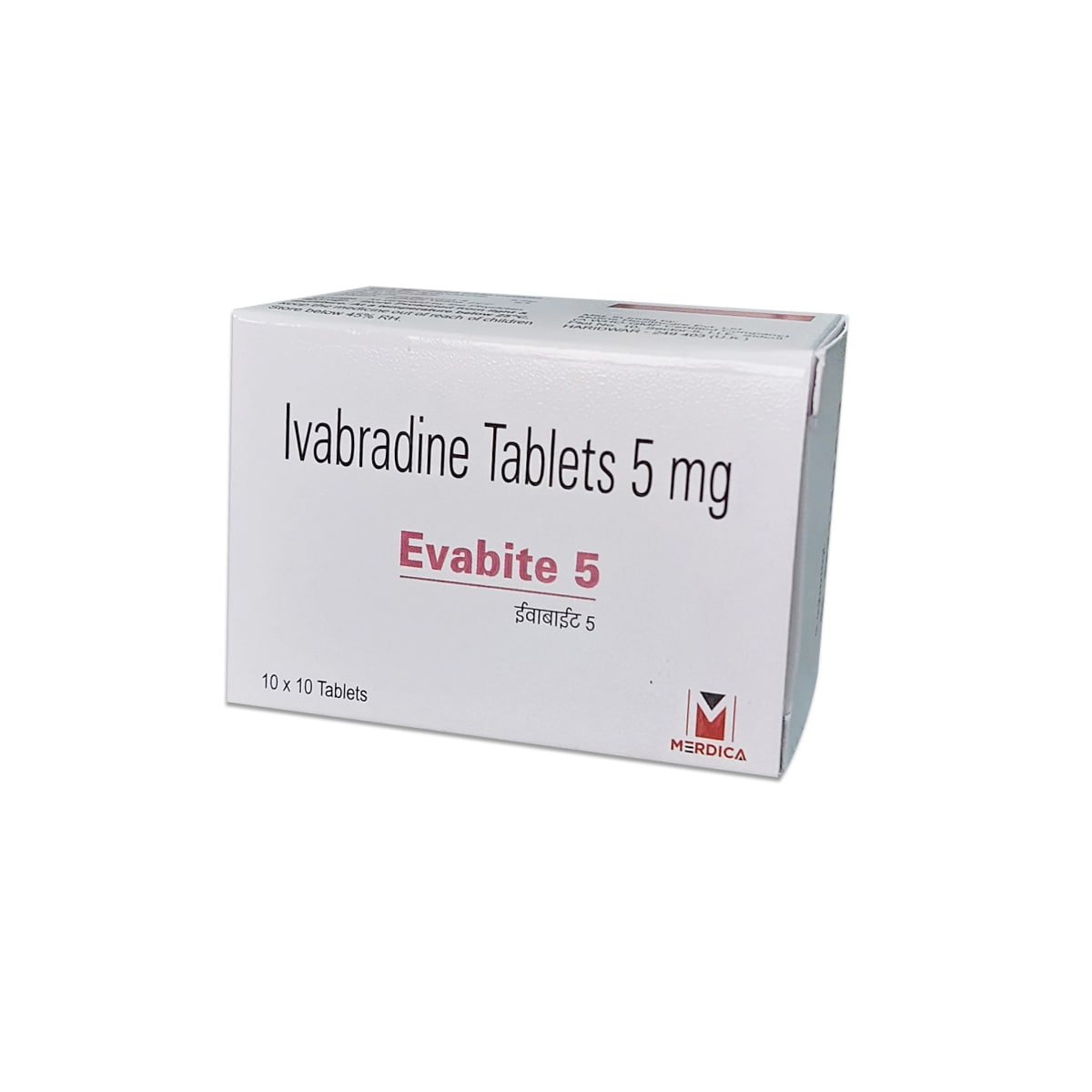
★ Specific inhibitor of the If current in the sino-atrial node, slowing sinus heart rate
★ Decreases pacemaker potential frequency, leading to a reduction in heart rate and subsequently reducing myocardial oxygen demand
-
What is the mechanism of action of Ranolazine in the treatment of angina? (3)

★ Inhibits the late sodium current, reducing intracellular Ca2+ in ischemic myocardial cells
★ Reduces oxygen demand
★ Decreases compression of small intra myocardial coronary vessels, thereby improving myocardial perfusion
-
What does NICE recommend for people on beta-blocker or calcium channel blocker monotherapy whose symptoms are not controlled, and the other option is contraindicated or not tolerated? (1)
Consider one of the following additional drugs: ivabradine, nicorandil, or ranolazine
-
Angina management summary: