What is the definition of angina pectoris? (2)
★ Angina: Derived from the Latin verb "angere," meaning "to choke or throttle"
★ Pectoris: Refers to the Latin "pectus," meaning "breast" or "chest"
What are the symptoms of angina pectoris? (3)
★ Feeling of cramping and severe constriction in the chest
★ Referred pain to jaw, shoulders, neck, and arms
★ May be associated with shortness of breath, sweating, nausea, and increased heart rate
What causes the pain symptoms in angina pectoris? (2)
★ Ischaemia: Reduced blood flow to the myocardium
★ Locally affected myocardium releases various compounds, including potassium, lactate, adenosine, bradykinin, and prostaglandins
How does the activation of myocardial pain receptors lead to pain perception in angina pectoris? (3)
★ Activation of myocardial pain receptors by released compounds
★ Transmission of signals via sensory neurons (cardiac nerves and upper posterior nerve roots) to the brain
★ Perception of pain in the brain
What is the prevalence of chronic stable angina pectoris in Western countries? (2)
★ Affects around 2-4% of the population in Western countries
★ Associated with an estimated annual risk of death and non-fatal myocardial infarction (MI) of 1-2% and 3%, respectively
How many people in the UK are estimated to be living with angina, and what is the gender distribution? (2)
★ Estimated that 1.3 million people in the UK are living with angina
★ Approximately 775,000 men and 560,000 women are affected
What is angina an important sign of?
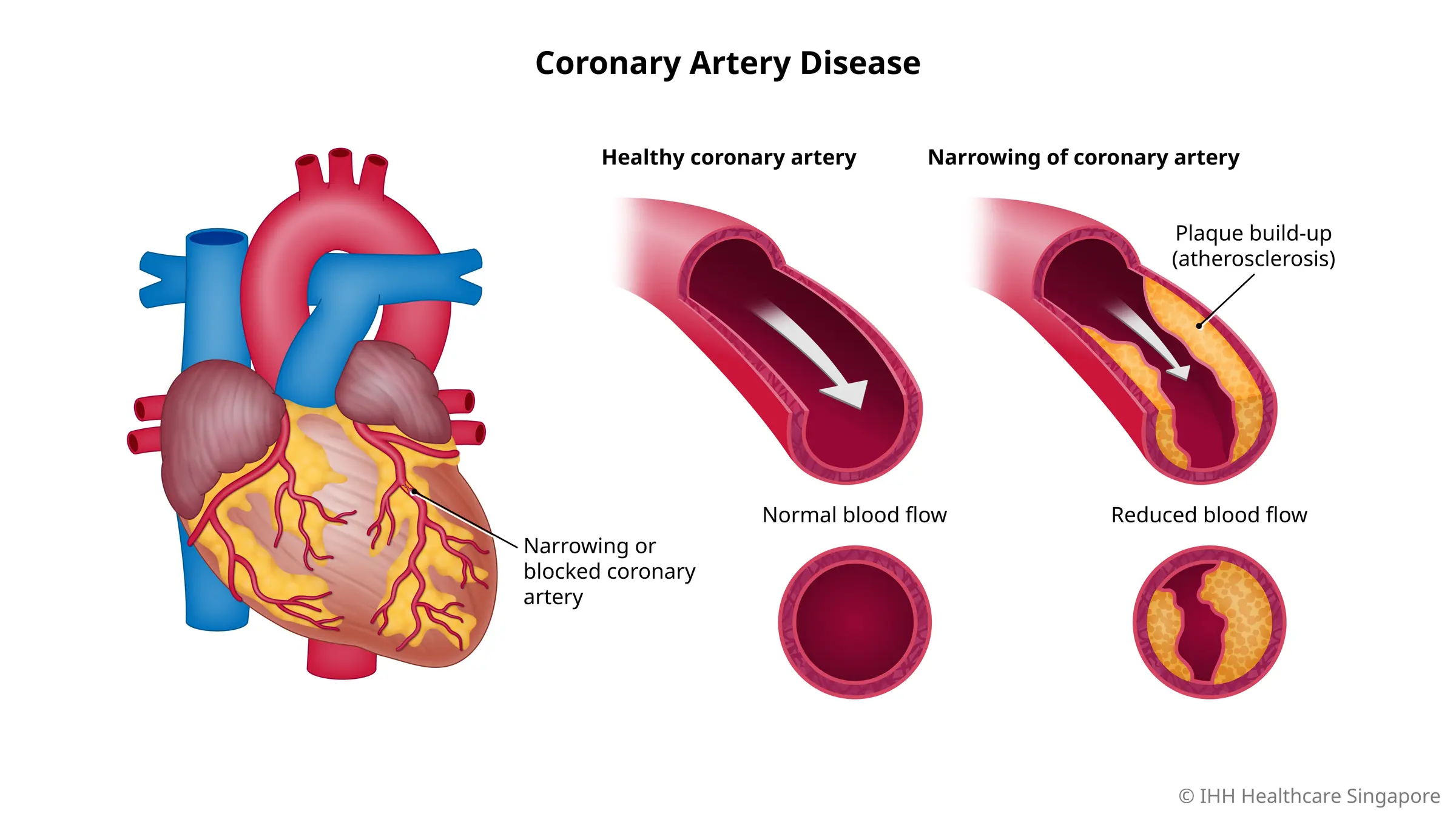
★ Angina is an important sign of Coronary Heart Disease (CHD), also known as Ischaemic Heart Disease (IHD)
What are the traditional classifications of angina based on the patient's chest pain symptoms? (3)
★ Typical angina: Substernal chest discomfort of characteristic quality and duration, provoked by exertion or emotional stress, relieved by rest and/or nitrates within minutes
★ Atypical angina: Presentation of two of the typical angina characteristics
★ Non-anginal: Presentation of only one or none of the chest pain characteristics
What are the classifications of angina based on aetiology and chest pain symptoms in the new classification? (4) REMEMBER 'SUPM'
★ Stable Angina: Attributed to myocardial ischaemia and coronary artery disease
★ Unstable Angina: Due to complications from stable angina.
★ Prinzmetal Angina (Angina Inversa): Usually due to a spasm in the coronary arteries, tends to happen in cycles, and cocaine use is a leading cause of coronary vasospasms
★ Microvascular Angina: Patients have angina symptoms but no evidence of coronary artery disease; normal or near-normal coronary angiogram
What is the aetiology of stable angina? (3)
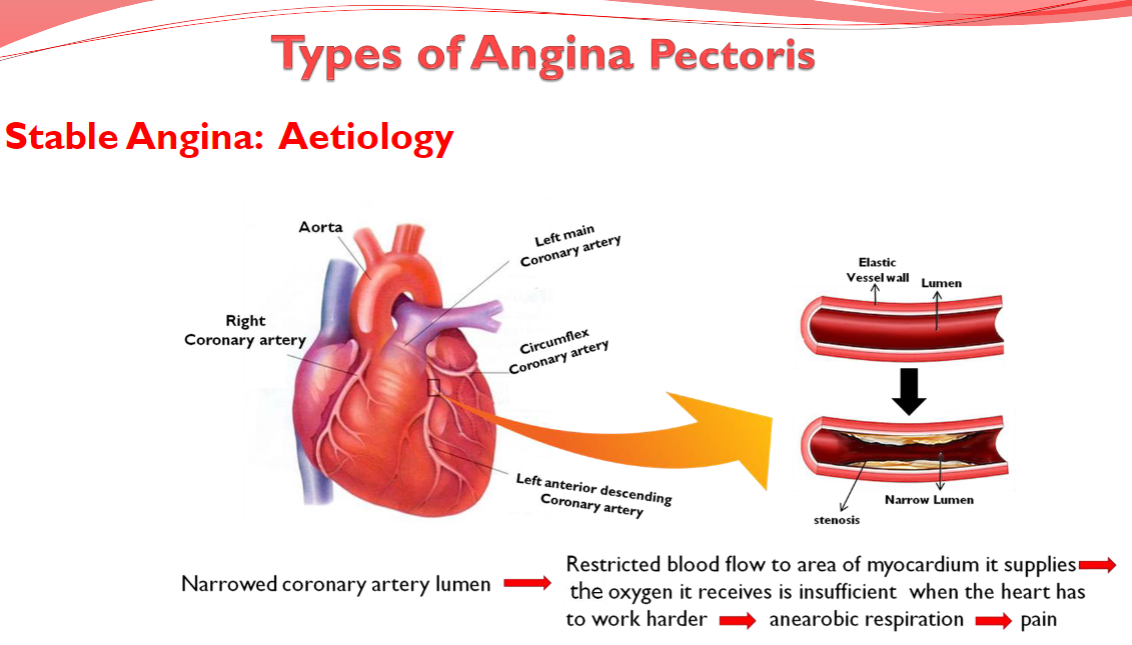
★ Narrowed coronary artery lumen leads to restricted blood flow to the area of myocardium it supplies
★ The oxygen it receives is insufficient when the heart has to work harder, leading to anaerobic respiration
★ Anaerobic respiration leads to pain
What are the characteristics of stable angina (classic, typical)? (5)
★ Follows a set pattern and is predictable; recurrent episodes tend to have a similar onset pattern, duration, and intensity
★ Short duration radiation of pain to the left arm, neck, jaw, or back; builds to a peak and lasts 2–5 minutes
★ Precipitated by exertion or increased cardiac oxygen demand, such as walking uphill, climbing stairs, exercise, emotional stress, or exposure to cold
★ Not life-threatening but can be a warning sign for something serious, such as a heart attack or stroke
★ Relieved by rest or taking medications. Symptoms are attributed to myocardial ischaemia
What is the aetiology of unstable angina? (3)
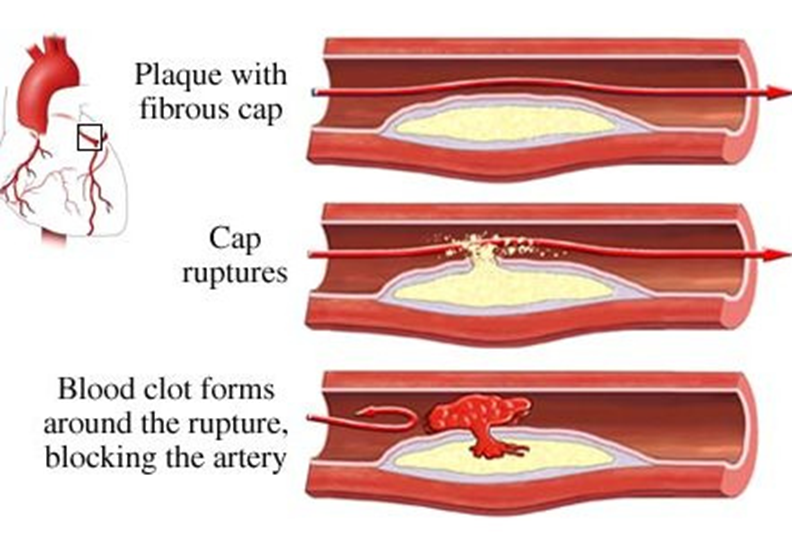
★ Clot formation occludes the artery (e.g., following plaque rupture), leading to critical reduction in blood flow.
★ Oxygen supply becomes inadequate even at rest.
★ This inadequate oxygen supply leads to pain
What are the characteristics of unstable angina? (6)
★ Unpredictable occurrence
★ Pain symptoms are more severe, can persist, and last longer
★ Can happen at rest with little exertion and may not have a trigger
★ Not usually relieved by rest and medications
★ Progression from stable angina is impossible to predict.
★ Regarded as a serious emergency, and patients are advised to go to the hospital
What is the aetiology of Prinzmetal Angina? (3)
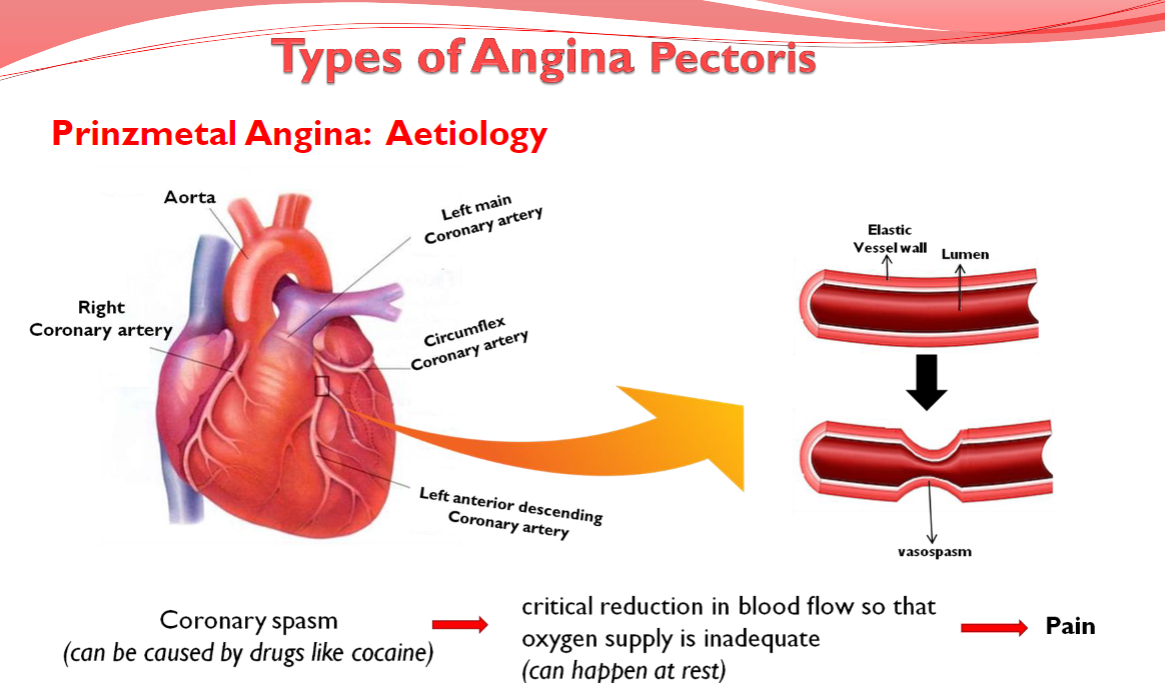
★ Coronary spasm
(can be caused by drugs like cocaine)
★ Critical reduction in blood flow so that
oxygen supply is inadequate
(can happen at rest)
★ Pain
What are the Types of Angina Pectoris: (3)
★ Stable Angina
★ Unstable Angina
★ Variant Angina (Prinzmetal Angina)
What are the Characteristics of Prinzmetal Angina (Variant Angina): (10)
★ Occurs while resting and during the night or early morning hours
★ Episodes last around 5 to 15 minutes (longer in some cases)
★ Rare (1 in 100 Angina cases)
★ Typically seen in younger patients
★ Attacks are severe and described as very painful
★ Pain may radiate from the chest to the head, shoulder, or arm
★ Associated symptoms include heartburn, nausea, sweating, dizziness, palpitations, migraines, and Raynaud's phenomenon
★ Often due to a spasm in the coronary arteries and tends to come in cycles
★ Cocaine use is a leading cause of coronary vasospasms
★ Can be relieved by taking medication
What is the aetiology of microvascular Angina? (3)
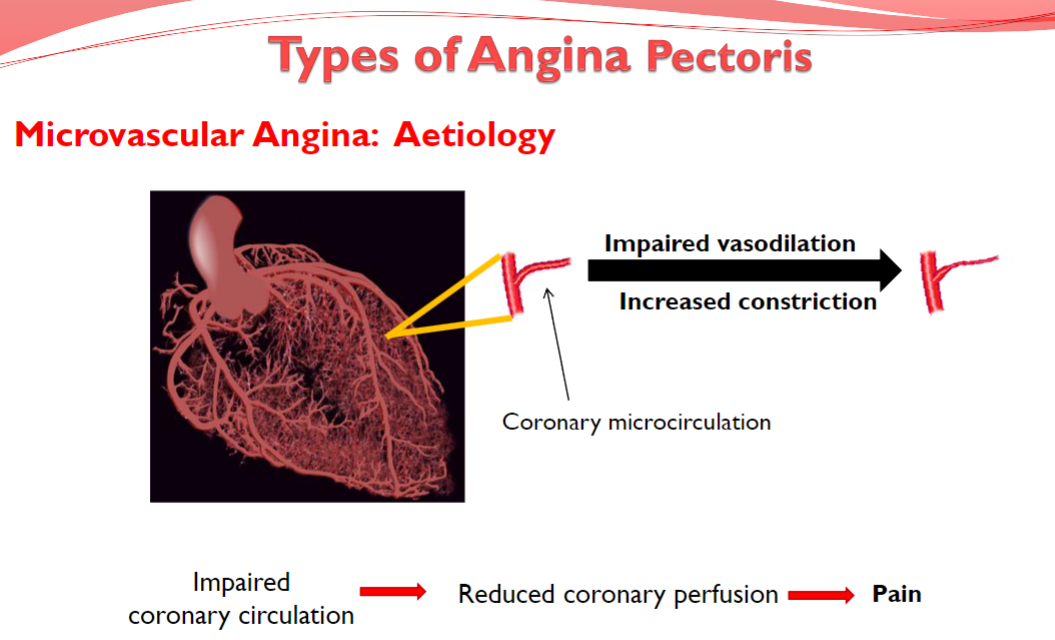
-Increased constriction
-Impaired vasodilation
-Pain
What are the types of angina pectoris? (4)
★ Stable Angina
★ Unstable Angina
★ Variant Angina (Prinzmetal Angina)
★ Microvascular Angina (Cardiac Syndrome X)
What are the characteristics of Microvascular Angina (Cardiac Syndrome X)? (6)
★ Impaired coronary circulation due to coronary microvascular dysfunction from abnormal vasodilation or increased vasoconstriction
★ Patients do not have obstructive coronary artery disease
★ Occurs with exertion and at rest but may respond less well to nitrates
★ Problem diagnosing it early as coronary microvasculature (vessels <300 um in diameter) cannot be directly imaged in vivo
★ Positron emission tomography (PET) or cardiac magnetic resonance (CMR) can be used to assess coronary microvascular blood flow
★ Treatment will vary depending on the cause of the microvascular angina
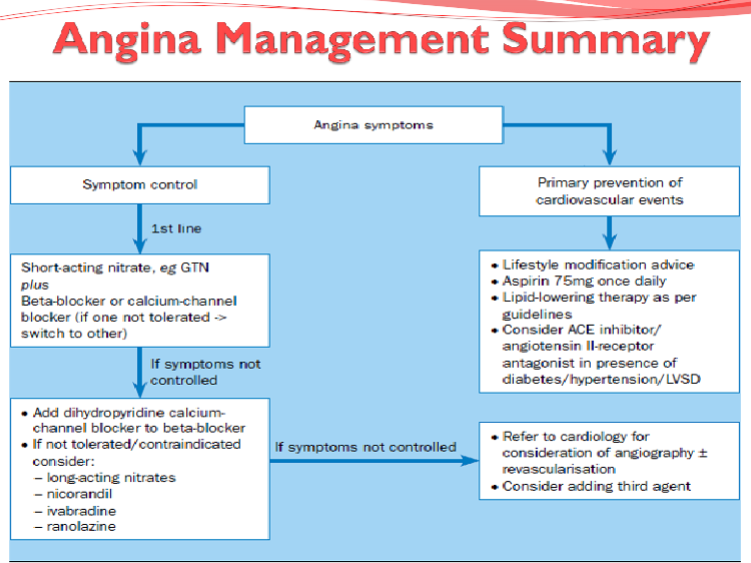
What are the treatment aims? (3)
★ To enhance quality of life through reduction of symptoms
★ To improve prognosis and prevent complications such as MI (Myocardial Infarction) and premature death
★ To be well tolerated and cause minimal side effects
Picture demonstrating Angina Pathophysiology:
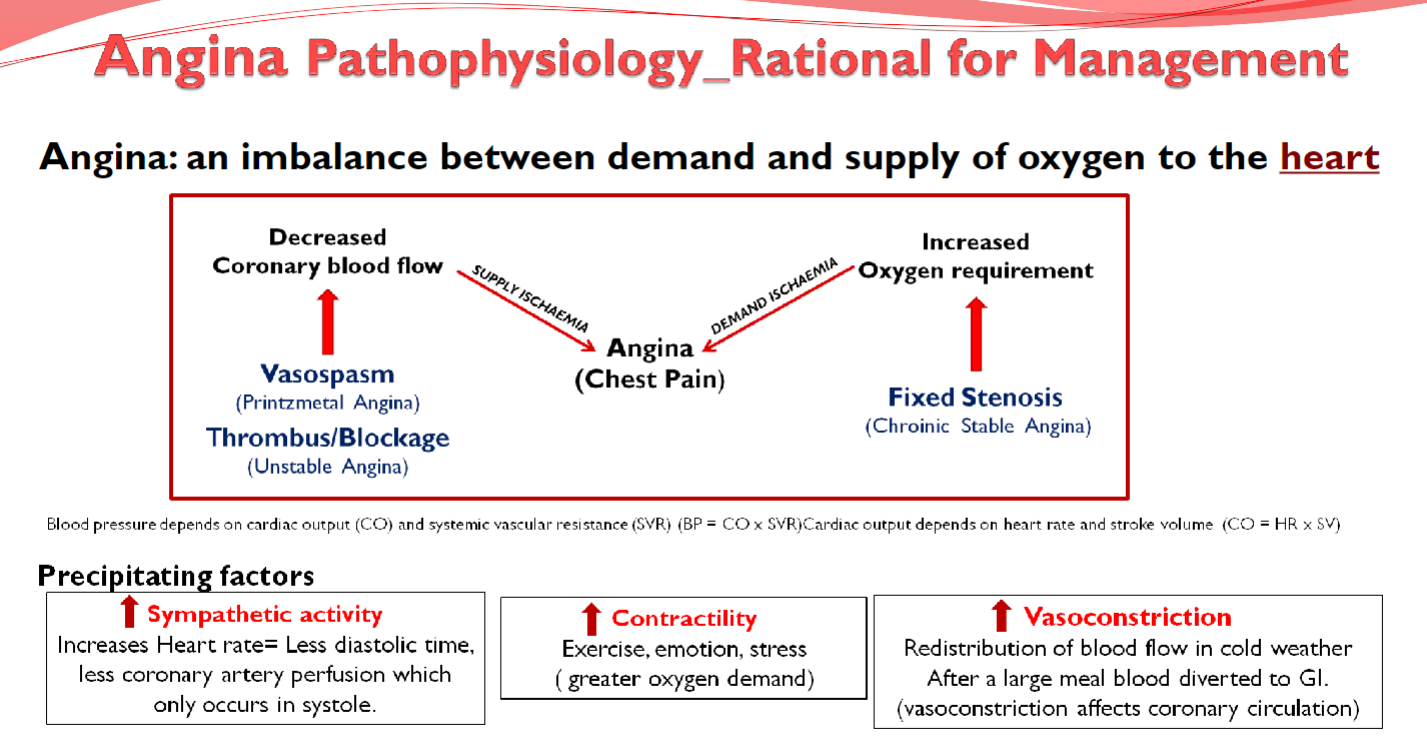
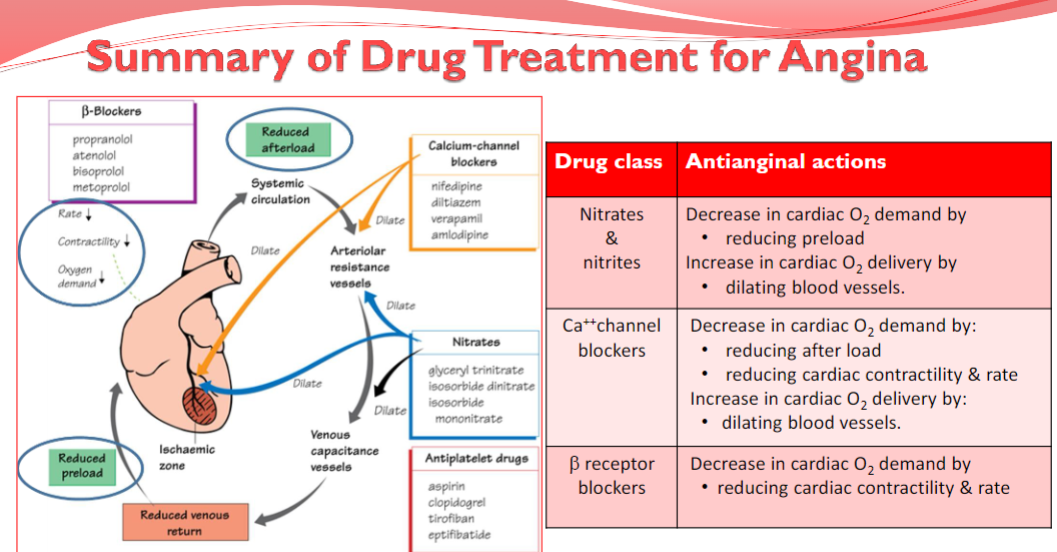
What are the treatment strategies for angina?
To improve perfusion:
Increase Oxygen Delivery by improving coronary blood flow using coronary vasodilators.
To reduce metabolic demand: (3)
-Reduce Oxygen Demand by decreasing cardiac work using:
-Vasodilators to reduce afterload and preload.
-Cardiac depressants to reduce heart rate and contractility.
Prevention: (3)
Prophylactic measures to reduce the risk of subsequent episodes, including:
Lipid Lowering Drugs
Anti-Coagulants
Fibrinolytic Anti-platelet treatments
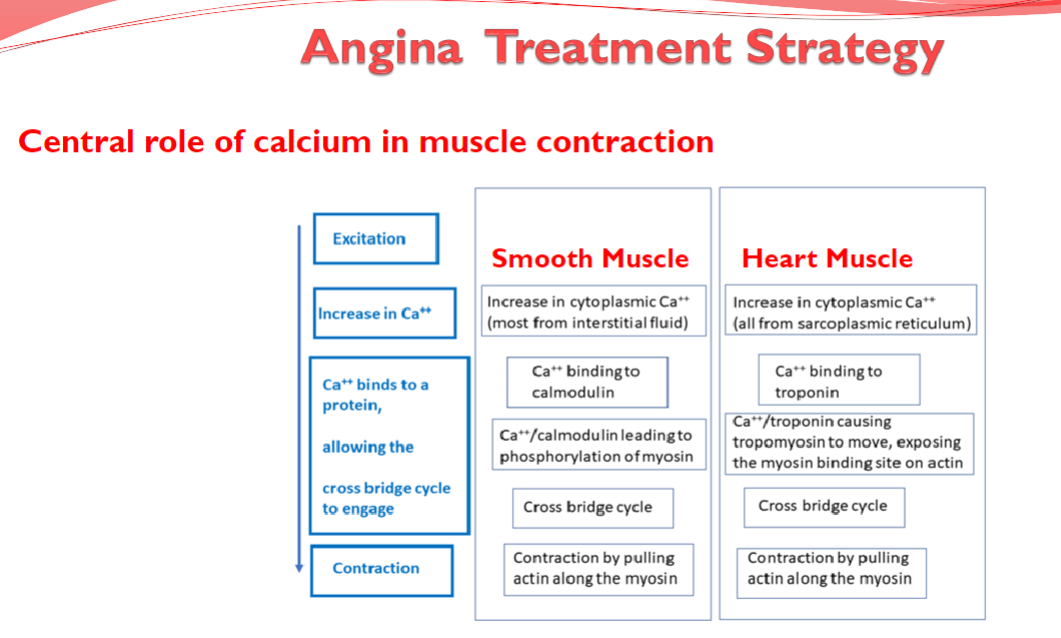
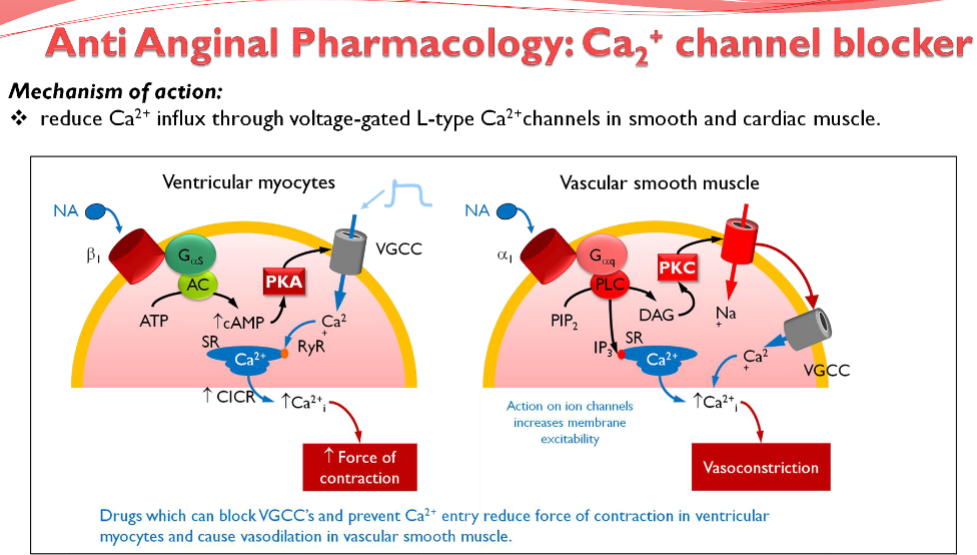
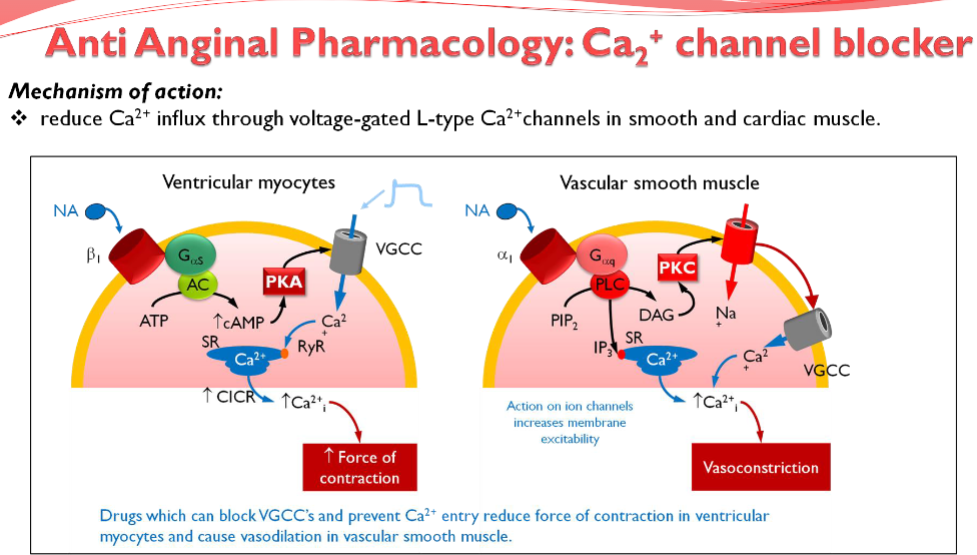
Picture demonstrating another angina treatment strategy related to Ca2+
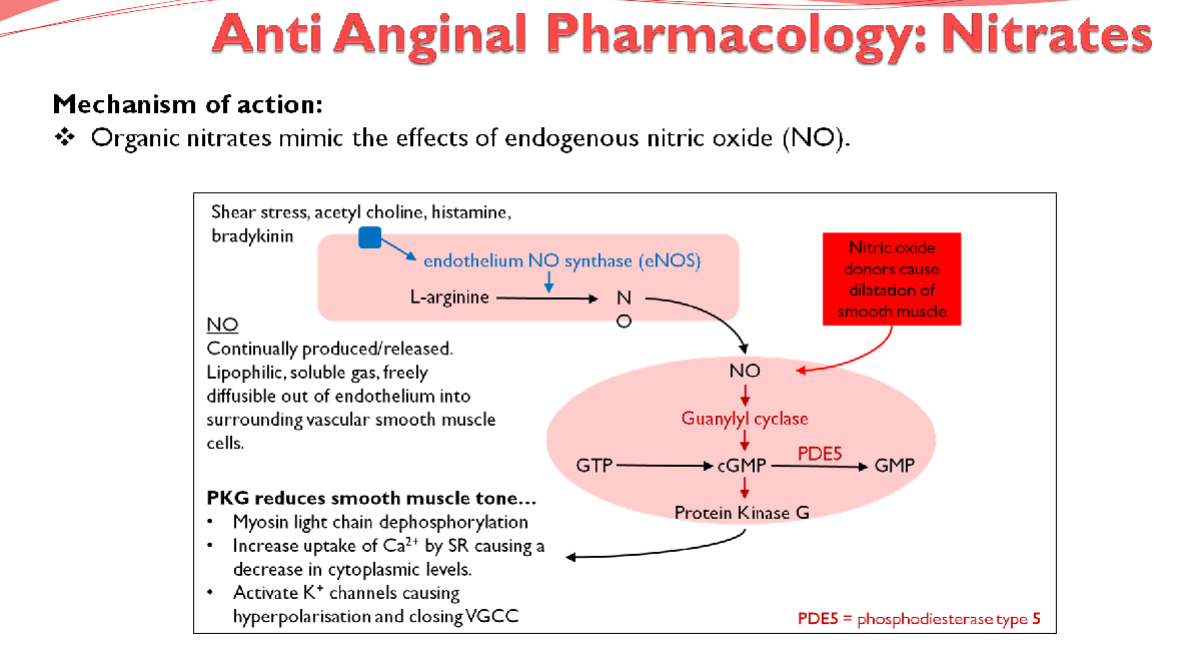
What are examples of nitrates used in anti-anginal therapy? (2)
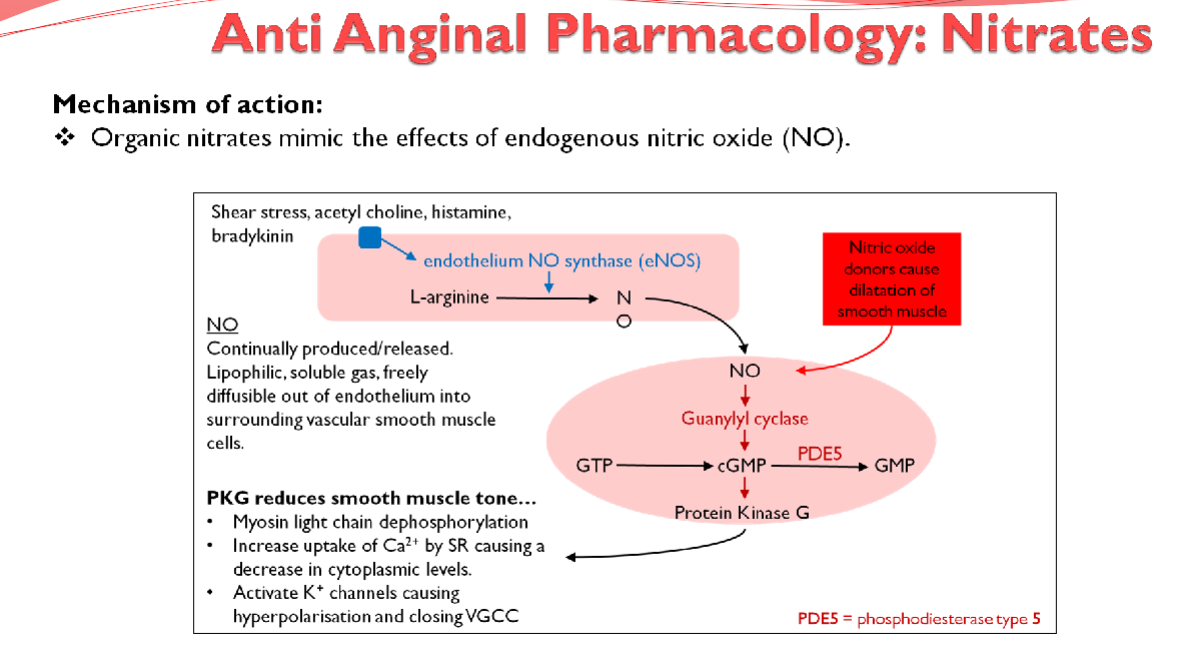
★ Glyceryl Trinitrate (GTN)
★ Isosorbide Mononitrate
What are the effects of nitrates on the cardiovascular system? (3)
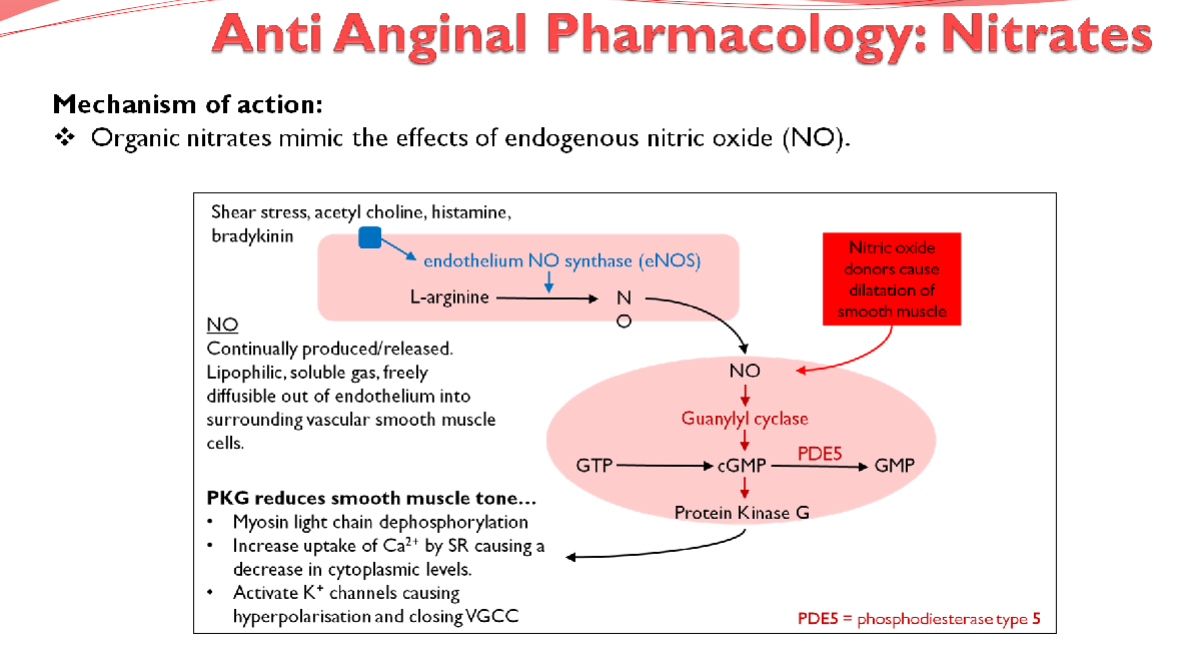
★ Peripheral Venodilation: decreases intraventricular pressure, reducing cardiac preload
★ Arterial Dilation: decreases total peripheral resistance (TPR), thereby reducing afterload
★ Both actions lower oxygen demand by decreasing the work of the heart
What is the effect of nitrates on coronary vessels affected by atherosclerosis? (1)
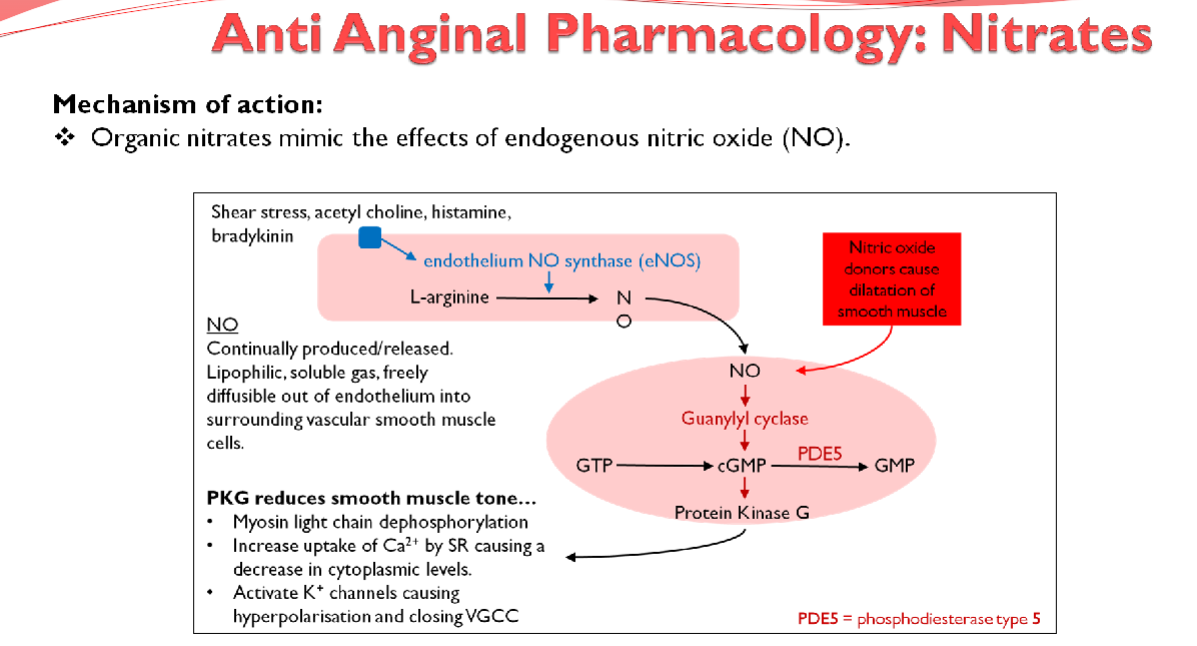
Limited effect on coronary vessels affected by atherosclerosis
What are the adverse effects associated with nitrates? (3)
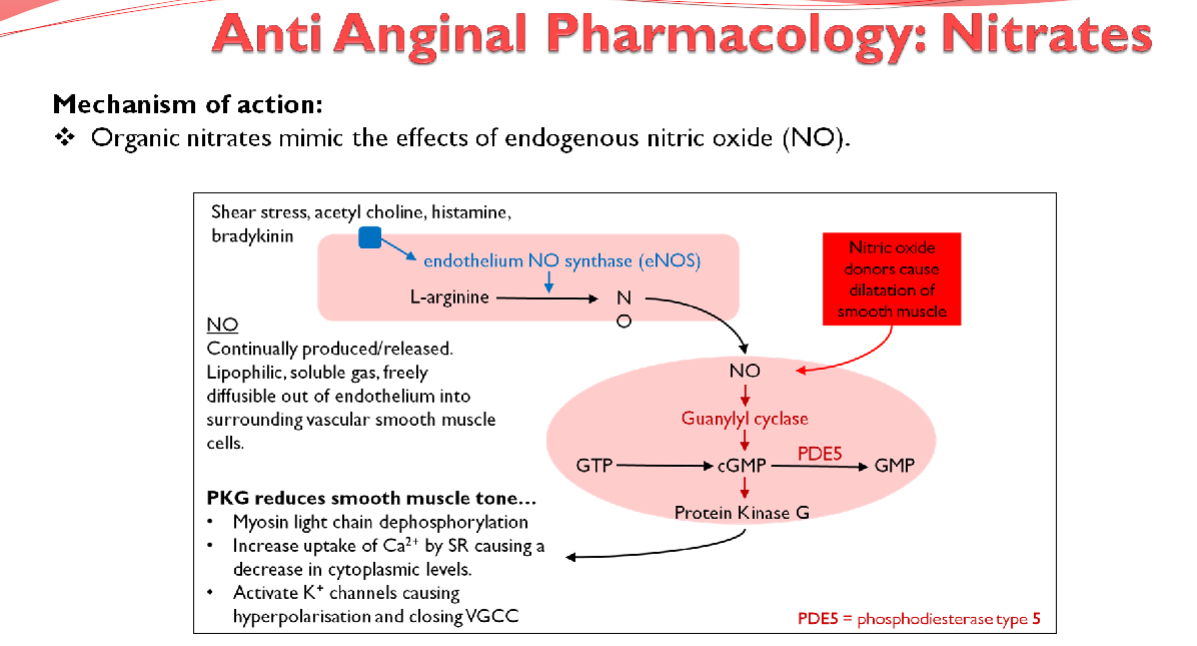
★ Throbbing headache, flushing, and syncope (Arterial dilation)
★ Postural hypotension (Venodilation)
★ Reflex tachycardia (Sympathetic outflow)
Picture demonstrating the mechanism of action of anti-anginal pharmacology; Nitrates
What are examples of beta-blockers used in anti-anginal therapy? (2)

★ Atenolol
★ Bisoprolol
What are the effects of beta-blockers on the cardiovascular system? (4)
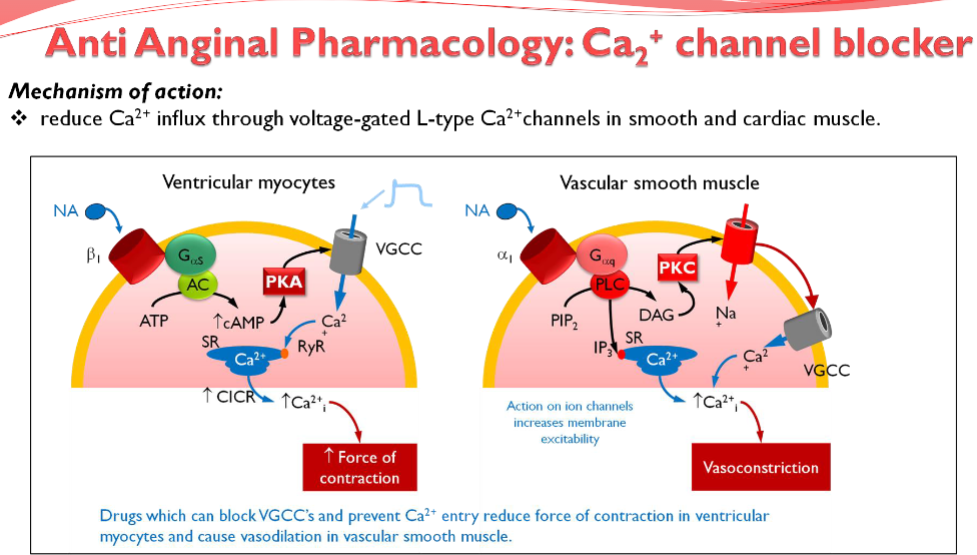
★ Inhibits If (Intrinsic Frequency) pacemaker current in the sinoatrial node (AV conduction)
★ Reduces the force of cardiac contractions, improving exercise tolerance
★ Both actions reduce cardiac output and lower blood pressure
★ Slower heart rate lengthens diastole, providing more time for coronary perfusion, effectively improving myocardial oxygen supply
What are the adverse effects associated with beta-blockers? (3)
★ Bronchospasm
★ Fatigue
★ Postural hypotension
What are the contraindications for beta-blockers? (2)
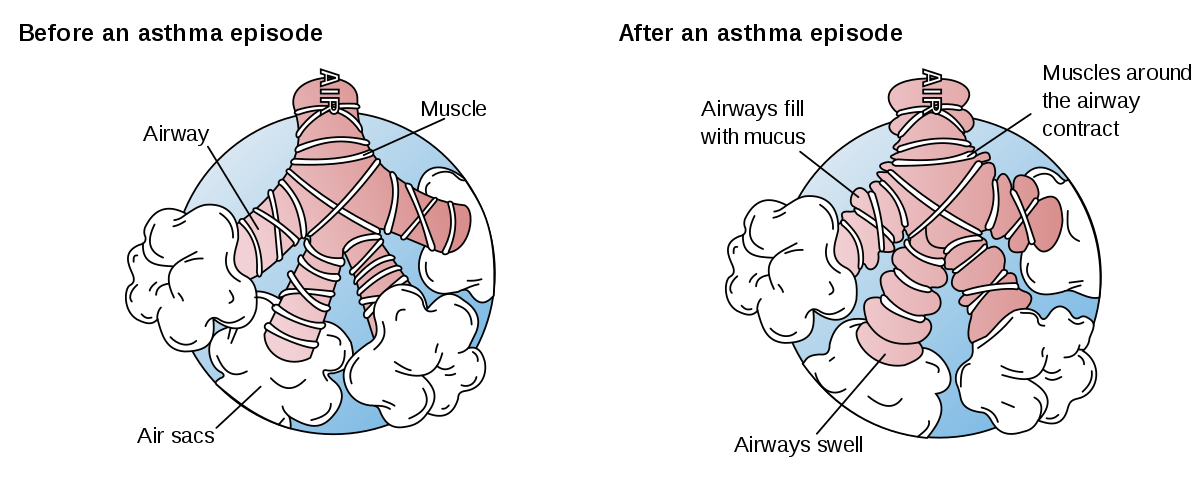
★ Asthma: Blocking B2 receptors can cause constriction and bronchospasm
★ Heart block where atrial-ventricular conduction is poor: may block AV node, further decreasing heart rate
Picture demonstrating the mechanism of action of anti-anginal pharmacology; Ca2+ channel blocker
What is the mechanism of action of aspirin in the prophylactic treatment of angina? (2)
★ Inhibits COX enzyme (cyclooxygenase), thereby inhibiting the production of thromboxane A2
★ Inhibits platelet aggregation, including the expression of GP IIb/IIIa
What is the mechanism of action of clopidogrel in the prophylactic treatment of angina? (2)
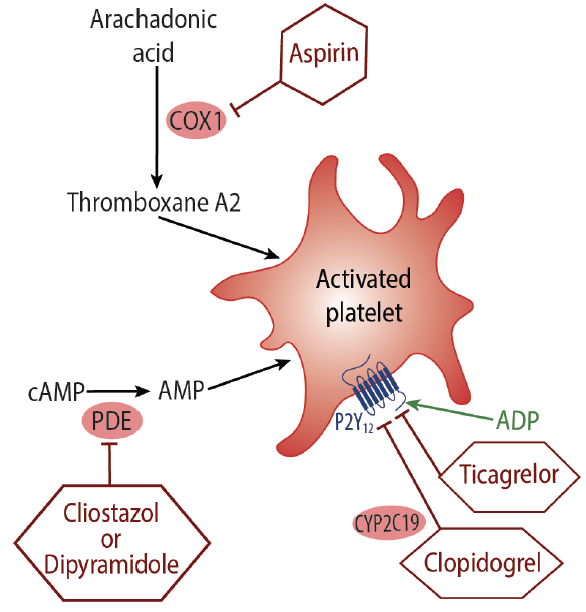
★ Inhibits ADP receptor on platelets
★ Reduces platelet aggregation
How do aspirin and clopidogrel act together in reducing thrombosis? (1)

Both drugs reduce thrombosis through entirely different mechanisms, allowing them to be used together effectively.
What is the mechanism of action of statins in the prophylactic treatment of angina? (2)
★ HMG Co-A reductase inhibitor
★ Lowers cholesterol levels
Picture demonstrating a summary of Drug Treatment:
What is the mechanism of action of Nicorandil in the treatment of angina? (3)

★ Potassium channel activator, leading to hyperpolarization
★ Blocks voltage-gated calcium channels (VGCCs) and reduces Ca2+ entry
★ Induces coronary vasodilation; it also has a nitrate moiety, contributing to its vasodilator action via the generation of nitric oxide (NO)
What is the mechanism of action of Ivabradine in the treatment of angina? (2)
★ Specific inhibitor of the If current in the sino-atrial node, slowing sinus heart rate
★ Decreases pacemaker potential frequency, leading to a reduction in heart rate and subsequently reducing myocardial oxygen demand
What is the mechanism of action of Ranolazine in the treatment of angina? (3)

★ Inhibits the late sodium current, reducing intracellular Ca2+ in ischemic myocardial cells
★ Reduces oxygen demand
★ Decreases compression of small intra myocardial coronary vessels, thereby improving myocardial perfusion
What does NICE recommend for people on beta-blocker or calcium channel blocker monotherapy whose symptoms are not controlled, and the other option is contraindicated or not tolerated? (1)
Consider one of the following additional drugs: ivabradine, nicorandil, or ranolazine
Angina management summary: