-
Macule
flat, distinct, discolored area of skin. It usually does not include a change in skin texture or thickness.
-
Papules
solid or cystic raised spot on the skin that is less than 1 centimeter (cm) wide. It is a type of skin lesion
-
Annular
ring shaped
-
pruritus
itching
-
Vesicle, pustule
fluid filled
-
scaling
loss of outer layer
-
plaques
uraised red patches covered with a whitish buildup of dead skins cells called scale
-
Types of infections of the skin
Bacterial- caused by strep A & B hemolytic streptococcus
Fungal
Viral
-
Scalded skin syndrome

-
Folliculitis

inflammation of follicule
-
Impetigo

Highly contagious
-red sores that form around nose and mouth. The sores rupture and ooze then form yellow-brown crust
Antibiotics
-
Tinea capitis (Fungal)

ring worm
-affecting scalp
-
Tinea cruris
Jock itch
-affecting groin
-
Tinea pedis
athletes foot
-affecting feet
-
tinea corporis
affecting any other parts of the body
-
Tinea versicolor
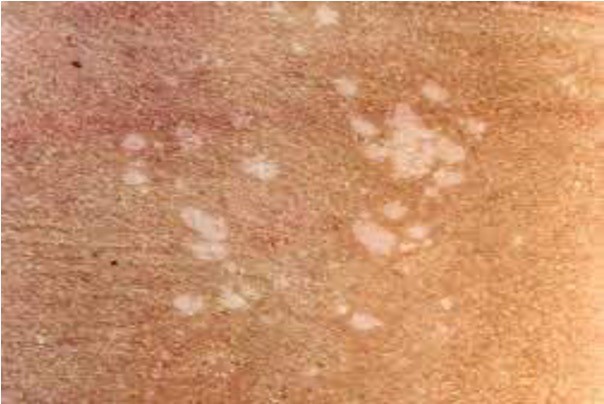
presents differently; hypopigmentation lesions on upper body
-
Acute hypersensitivity reactions (inflammatory)

-diaper dermatitis- diaper rash
-contact dermatitis- response to antigenic substance exposure
-erythema multiforme- acute, self limiting hypersensitivity reaction; usually in response to viral infection or medication
-Uriticaria- hives; antigen-antibody response of histamine release from mast cells
-
Chronic hypersensitivity disorder

atopic dermatitis - eczema; dry, itchy patches
-
Chronic inflammatory skin disorders not from hypersensitivity

-Seborrhea-chronic inflammatory dermatitis that may occur on the skin or scalp; excess oil accumulation; cradle cap.
-Psoriasis-chronic inflammatory skin disease with periods of remission and exacerbation; build up of scaley red lesions that may burn or itch
-
Prevention and management of diaper rash
-change diapers frequently
-avoid harsh soaps, baby wipes with fragrance/preservatives
-allow child to go diaper less for periods of time
-blow dry rash area (we don't want it wet)
-
Contact dermatitis
Causes
-Antigenic substance exposure
-Allergy to nickel or cobalt in clothing, hardware, or dyes
-Exposure to highly allergenic plants: poison ivy, oak, and sumac
Complications
-Secondary bacterial skin infection
-Lichenification (thick and leathery) or hyperpigmentation
-
Risk Factors for CA-MRSA
-Turf burns
-Towel sharing
-Participation in team sports
-Attendance at day care or outdoor camps
-
Causes of Urticaria(hives)
-Foods
-Drugs
-Animal stings
-Infections
-Environmental stimuli
-Stress
-
Injuries

-Pressure ulcers
-Minor injuries
-Burns
-Sunburn
-Cold injury- frost-bite; 1st-4th degree;
-Animal bites – dog bites most frequent; cat bite most infection; hand and face common site; rabies, tetanus
-Insect stings and bites-Hymenoptera class of insects sting; bacterial infection can follow, anaphylaxis
-
Nursing Interventions for Children with Extensive Burns
-Promoting oxygenation and ventilation
-Restoring and maintaining fluid volume
-Preventing hypothermia
-Cleansing the burn
-Preventing infection
-Managing pain with atraumatic care
-Treating infected burns
-Providing burn rehabilitation
-
Common Medications
-Antibiotics (topical, systemic)
-Corticosteroids (topical)
-Antifungals (topical, systemic)
-Topical immune modulators (moderate to severe atopic dermatitis)
-Antihistamines
-Isotretinoin (cystic or severe acne)
-Coal tar preparations (psoriasis, atopic dermatitis)
-Silver sulfadiazine 1% (burns)
-
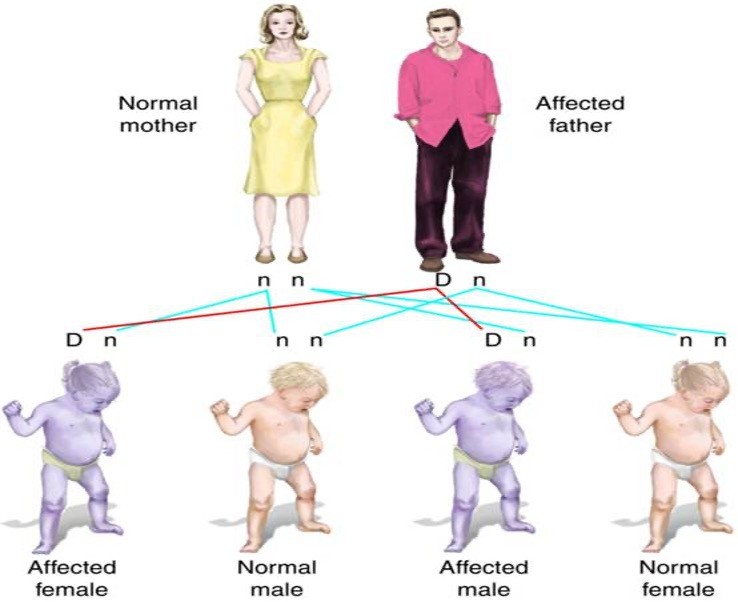
Autosomal dominant inheritance pattern
50% chance of child having affected genes
-
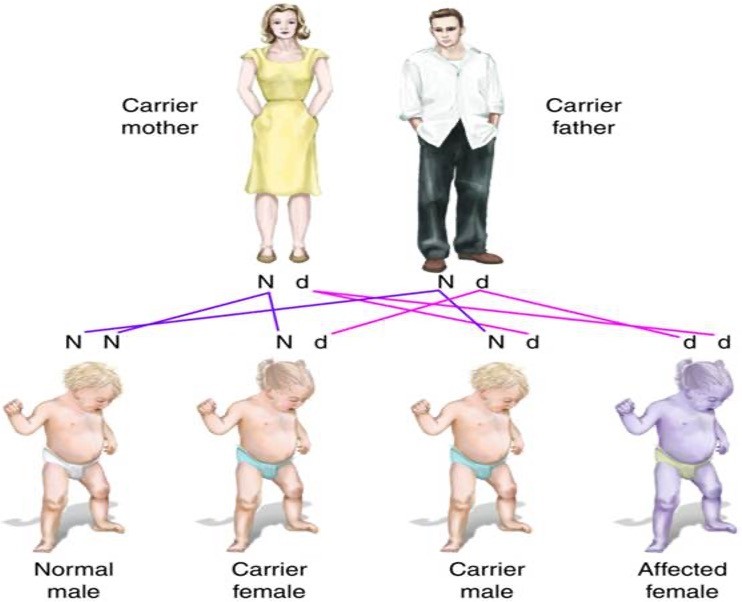
Autosomal recessive inheritance pattern
25% chance of having child affected
-
Significant Findings in Medical History of a Child with a Genetic Disorder
•Maternal age older than 35 years or paternal age older than 50
•Repeated premature births, breech delivery - Congenital hip dysplasia
•Abnormalities found on ultrasound or in prenatal blood screening tests
•Amniotic fluid abnormalities
•Multiple births
•Exposure to medications and known teratogens
•Decreased fetal movement
Recommend Genetic counseling - allows families the opportunity to prepare for special needs of an unborn child and to consider options for current and future pregnancies
-
Neurofibromatosis (autosomal dominant)
type 1 most common (von Recklinghausen disease) tumors grow on nerves; skin changes, bone deformties; progressive disease; diagnosis = two or more clinical signs including – 2 or more neurofibromas, tumor on optic nerve, more than 6 café-au-lait spots(brown spot) > 5 mm diameter à high level of suspicion; treament is supportive
-
Huntington disease (autosomal dominant)
rare; usually presents in 30-40’s; progressive breakdown of nerve cells in brain; muscle problems, abnormal eye movements, impaired gait
-
Achondroplasia (autosomal dominant)

most common type of short-limbed dwarfism; can also be a mutation; short limbs, large head, average trunk; 4 ft 1in – 4ft 4in; sleep apnea, ear infections, spinal stenosis
-
Marfan syndrome (autosomal dominant)
affects connective tissue effects the heart, eyes, blood vessels, and bones; tall and thin with long arms, legs, fingers, and toes; treatment includes medications to keep blood pressure low, eyeglasses or contact lenses, and surgery.
-
Osteogenesis imperfecta type 1 (autosomal dominant)
brittle bone
-
Complications of Neurofibromatosis
•Headaches
•Hydrocephalus
•Scoliosis
•Cardiac defects, hypertension, seizures
•Vision and hearing loss
•Neurocognitive deficits
•Higher risk for neoplasms
-
Cystic fibrosis (Autosomal Recessive)
affects the cells that produce mucus, sweat, and digestive juices. It causes these fluids to become thick and sticky. They then plug up tubes, ducts, and passageways.
-
Phenylketonuria (Autosomal Recessive)
amino acid called phenylalanine to build up in the body; untreated phenylketonuria can lead to brain damage, intellectual disabilities, behavioral symptoms, or seizures; Treatment includes a strict diet with limited protein
-
Tay–Sachs (Autosomal Recessive)
destroys nerve cells in the brain and spinal cord; typically found in people with certain ancestry, such as Eastern European Jews; A fatty substance in the brain destroys nerve cells; Symptoms of slowed development usually appear around six months of age. Symptoms progress until they lead to death, often around age four; There is no cure
-
Hemophilia
prolonged bleeding due to insufficent clotting factors; hemophilia A, associated with a low level of factor 8 (factor VIII
-
Color blindness (red/green [most common], blue/green)
reduced ability to distinguish between certain colors.
-
Duchenne muscular dystrophy
progressive muscular weakness, typically in boys; no cure, but steroids may control symptoms
(The way they get up- gawar sign)
-
Trisomy 21 (Down Syndrome)
Cause
•Presence of all or part of an extra 21st chromosome
Characteristics
•Some degree of intellectual disability
•Characteristic facial features
•Other health problems (e.g., cardiac defects, visual and hearing impairment, intestinal malformations, and an increased susceptibility to infections)
-
Health Guidelines for Children with Down Syndrome #1
•Have your child evaluated by a pediatric cardiologist, including an echocardiogram
•Take your child for routine vision and hearing tests. By 6 months have your child seen by a pediatric ophthalmologist
•Make sure your child gets regular medical care, including recommended immunizations and a thyroid test at 6 and 12 months and then yearly
•Have your child follow a regular diet and exercise routine
•Make sure the child gets a cervical radiograph between 3 and 5 years of age to screen for atlantoaxial instability (C1 and C2).
Recommend genetic counseling
oMultidisciplinary care
-
Physical Characteristics of Turner Syndrome

•Loss of all or part of an X chromosome
•Webbed neck
•Low posterior hairline
•Wide-spaced nipples
•Edema of the hands and feet
•Amenorrhea
•No development of secondary sex characteristics
•Sterility
•Perceptual and social skill difficulties
-
Physical Characteristics of Klinefelter Syndrome
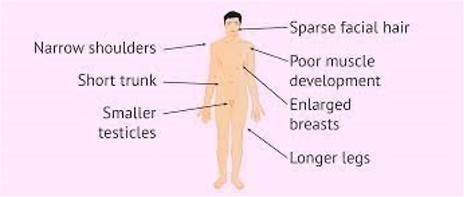
•One or more extra X chromosome; affects males
•Decreased facial hair
•Gynecomastia
•Decreased pubic hair
•Hypogonadism
•Underdeveloped testes,
•Taller than average by 5 years of age, with long legs and a short torso
•Cognitive impairments of varying degree: motor delay, speech or language difficulties, attention deficits, and learning disabilities
-
Clinical manifestations Associated with Fragile X Syndrome
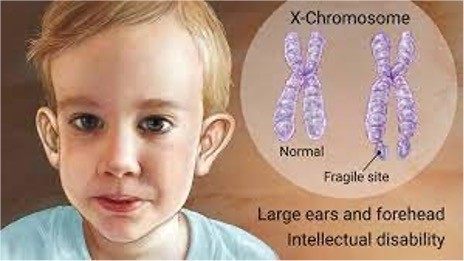
•Most common inherited cause of intellectual disability; can affect males and females but females typically have milder symptoms
•Minor dysmorphic features
•Developmental delay/Intellectual impairment
•Behavior problems:
•Attention deficits
•Hand flapping and biting
•Hyperactivity
•Shyness and social isolation
•Low self-esteem
•Gaze aversion
-
Nutritional deficiency
Iron deficiency, folic acid deficiency, pernicious anemia (deficiency in B12)
-
Toxin exposure
-lead poisoning
toxic effect on bone marrow, interferes with synthesis of heme- precursor to hgb
-
Aplastic anemia
failure of bone marrow to produce cells- acquired as an adverse reaction to medication (chemo, anticonvulsants).
-rare congenital bone marrow failure (fanconi anemia- autosomal recessive )
-
Hemolytic anemia
sickle cell anemia, thalassemia
-
Food high in iron
-red meat
-tuna & salmon
-eggs
-tofu
-leafy green veggies
-dried beans, peas and fruit
-enriched grains
-iron fortified breakfast cereals
-
Nursing assessment for aplastic anemia
History
Exposure to myelosuppressive medications or radiation therapy
Detailed family, environmental, and infectious disease history
Epistaxis, gingival oozing, or increased bleeding with menstruation
Headache, fatigue
Physical examination
Ecchymoses
Petechiae or purpura
Oral ulcerations
Tachycardia
Tachypnea
-
Complications of lead poisoning
Lower levels-Behavioral problems-Learning difficulties
Higher levels (requires chelation treatment)-Encephalopathy-Seizures-Brain damage
-
Types of Hemoglobinopathies
Thalassemia - inherited blood disorder that causes less hemoglobin; anemia; can be mild to severe
Sickle cell disease (SCD)- inherited, most common in autosomal recessive, African, Mediterranean, middle eastern, and Indian descent, hemoglobin SS disease is most common (crescent shaped blood cells)
Types of SCD:
Hemoglobin Ss (Hbss)
Hb "S" gene (abnormal form of hemoglobin) from each parent → sickle cell anemia;
More of the Hb is abnormal
more severe form of the disease
Hemoglobin SC (HbSC) - less severe form
one HbS gene and one HbC gene (another abnormal type)
Sickle cell trait-
Only have HbS from one parent
-
Symptoms of sickle cell disease
-Anemia
-Pain/sickle cell crisis
-acute chest syndrome
-stroke
-jaundice
-splenic pooling
-priapism
-
Treatment for Sickle cell disease
-pain medication
-hydration
-blood transfusions
-vaccinations
-folic acid for anemia
-eye exams to assess retinopathy
-Hydroxyurea- medication that may reduce frequency of pain crisis and ACS; makes RBC less likely to turn into sickle shape
-Bone marrow transplant- for children with severe complications
-
Thalassemia
alpha-thalassemia -severity depends on number of gene mutations you inherit; ; synthesis of the a chain of the hemoglobin protein is affected
beta-thalassemia- severity depends on part of the hemoglobin molecule is affected. the B-globulin chain in hemoglobin synthesis is reduced or entirely absent; severe hemolytic anemia and chronic hypoxia
Thalassemia minor (also called B-thalassemia trait): leads to mild microcytic anemia; often no treatment is required.
Thalassemia intermedia: child requires blood transfusions to maintain adequate quality of life.Thalassemia major: to survive the child requires ongoing medical attention, blood transfusions, and iron removal; Cooley's Anemia
Left untreated, B-thalassemia major is fatal by age 5 years, but use of blood transfusions and chelation therapy increases life expectancy of these children
-
Hemosiderosis
Excessive supply of iron; accumulation in tissues
Result of rapid hemolysis of RBCs, decrease in hemoglobin production, increased absorption of dietary iron in response to the severely anemic state.
excess iron is deposited in the body's tissues, causing bronze pigmentation of the skin, bony changes, and altered organ function, particularly in the cardiac system, splenomegaly, endocrine abnormalities, osteoporosis, liver and gallbladder disease, and leg ulcers.
-
Thalassemia management
PRBC transfusions(blood transfusion) as prescribed to maintain an adequate level of hemoglobin for oxygen delivery to the tissues
-Excess iron is removed by chelation therapy. Administer the chelating agent deferoxamine with the transfusion.
Deferoxamine binds to the iron and allows it to be removed through the stool or urine. Oral deferasirox may also be prescribed.
-
Glucose-6-Phosphate Dehydrogenase
Deficiency
G6PD -an enzyme that helps RBC's work properly is insufficient or abnormal; X-linked recessive
causes red blood cells to break down (hemolysis) in response to certain medications, infections, or other stressors.
Triggers that may result in oxidative stress and hemolysis-
• bacterial or viral illness
exposure to certain substances such as medications (e.g., sulfonamides, sulfones, malaria-fighting drugs [such as quinine], or methylene blue [for treating urinary tract infections]), naphthalene (an agent in mothballs), or fava beans.
• Tea colored urine, splenomegaly
* Administer 02; improve one trigger or illness is removed
-
clotting disorders
-Idiopathic thrombocytopenia purpura (ITP)
-Henoch-Schonlein purpura
-Disseminated intravascular coagulation (DIC)
-Factor deficiencies
-Hemophilia A (factor VIII deficiency)
-von Willebrand disease
-
Idiopathic Thrombocytopenia Purpura
Immune response following viral infection that destroy platelets
-Normal platelet count -150,000 to 450,000 platelets per microliter of blood
-Petechiae:Pinpoint hemorrhages occurring on the body that do not blanch to pressure,
-Purpura:Larger purplish areas of hemorrhage in which blood collects under the tissues; complication = bleeding into organs and intracranial pressure - although both rare
* Platelet counts below 10,000/mm3, corticosteroids may be administered for 2 to 3 weeks
• Single dose of intravenous immunoglobulin (IVIG) may be used as an adjunct
-Platelet transfusions are not indicated unless life-threatening bleeding is present.
-Refer the child for follow-up care with a pediatric hematologist.
-Usually, self-limiting
-
Henoch-Schönlein Purpura
Mostly male children
Associated with viral or bacterial illness- often respiratory
Vasculitis with immunoglobulin A (IgA) -dominant immune deposits affecting small vessels in the skin, gut, and kidney
Benign in most children and resolves with no issues
nephrotic syndrome may occur as a result of renal injury, and those children may have
hypertension.
Pulmonary, cardiac, and neurologic complications can also occur.
Treatment with corticosteroids, such as prednisone, may be helpful in children with severe joint or GI manifestations
-
Disseminated Intravascular Coagulation
Complex condition leads to activation of coagulation
Usually occurs in critically ill childrenSeptic shock, endotoxins, viruses, tissue necrosis, cancer treatments
Deficiencies of coagulation and anticoagulation pathways occur
Hemorrhage and organ tissue damage result and can be irreversible if not recognized and treated immediately.
Treat underlying issue -ex. infection → antibiotics
-
Hemophilia
group of X-linked recessive disorders that result in deficiency in one of the coagulation factors in the blood
transmitted by carrier mothers to their sons, so usually only males are affected by hemophilia
coagulation factors in the blood are essential for clot formation either spontaneously or from an injury, and when factors are absent bleeding will be difficult to stop
The most common= hemophilia A - deficiency of factor VIII
Prevent bleeding
Helmets, avoid contact sports, medical alert bracelet
-
Von Willebrand Disease
Mild bleeding disorder
• genetically transmitted bleeding disorder that may affect both genders and all races
deficiency in von Willebrand factor (vWF)
serves two functions:bind with factor VIII, protecting it from breakdownserve as the "glue" that attaches platelets to the site of injury
-
Cancer in Children
-The most common childhood cancers in order of frequency-
-Leukemia, CNS tumors, lymphoma, neuroblastoma (adrenal glands), rhabdomyosarcoma (muscles), Wilms tumor (kidney), bone tumors, and retinoblastoma
Warning signs of cancer-
-most often related to changes in blood cell production; changes in blood cell production may result in fatigue, pallor, frequent or severe infection, or easy bruising
-a result of compression, infiltration, or obstruction caused by the tumor; infiltration, obstruction, or compression by a tumor may result in bone or abdominal pain, swelling, unusual discharge
-
Function of:
1. Erythrocytes/RBC’s
2. Thrombocytes/Platelets
3. Leukocytes/WBC
1. carry oxygen throughout body
2. clotting
3. fight infection
Low erythrocyte/rbc- anemia(pica, pale, tired)
Low platelets- prolonged bleeding
-
types of immunity
Passive
-Antibodies received from an external source (mother to baby, IVIG)
Cellular
-Antibodies produced by native T-cell lymphocytes (thymus)
Humoral
-Antibodies produced by native B-cell lymphocytes (bone marrow)
-
Assessments for Wiskott-Aldrich
Syndrome
History of petechiae
• Bloody diarrhea or bleeding episode in the first 6 months of life
History of hematemesis or intracranial or conjunctival hemorrhages
Eczema
Laboratory findings of low IgM concentration, elevated IgA and IgE concentrations, and normal IgG concentrations
-
Ten Warning Signs of Primary
Immunodeficiency
Four or more new episodes of acute otitis media in 1 year
Two or more episodes of severe sinusitis
Treatment with antibiotics for 2 months or longer with little effect
Two or more episodes of pneumonia in 1 year
Failure to thrive in the infant
Recurrent deep skin or organ abscesses
Persistent oral thrush or skin candidiasis after 1 year of age
History of infections requiring IV antibiotics to clear
Two or more serious infections such as sepsis
Family history of primary immunodeficiency
-
Signs and Symptoms of HIV Infection in
Children
-Failure to thrive
-Recurrent bacterial infections
-Opportunistic infections
-Chronic or recurrent diarrhea
-Recurrent or persistent fever
-Developmental delay
-Prolonged candidiasis
-
food allergies
-dairy (cows milk)
-eggs
-penuts
-tree nuts
-fish and shellfish
-wheat
-soy
-
PRIMARY IMMUNODEFICIENCIES
Wiskott-Aldrich Syndrome/ Deficiency -X-linked genetic disorder; defective gene that results in immunodeficiency, eczema, and thrombocytopenia, autoimmune hemolytic anemia, neutropenia, skin or cerebral vasculitis, arthritis, inflammatory bowel disease, and renal disease
Severe Combined Immune Deficiency (SCID) - X-linked or autosomal recessive disorder; it can occur in girls or boys. SCID is
characterized by absent T-cell and B-cell function.
-
Nursing Assessment of Severe Combined
Immune Deficiency (SCID)
-Chronic diarrhea
-Failure to thrive
-History of severe infections early in infancy
-Persistent thrush
-Adventitious sounds related to pneumonia
-Lab findings of very low levels of immunoglobulins
-
Goals of Nursing Care of the Child with HIV
Infection or Other Chronic Immune Disorder
-Avoiding infection
-How can we avoid infection?
-Promoting compliance with the medication regimen
-Promoting nutrition
-Providing pain management and comfort measures
-Educating the child and caregivers
-Providing ongoing psychosocial support
-
Common Laboratory and Diagnostic Tests
for Systemic Lupus Erythematosus (SLE)
-SLE definition: chronic multisystem autoimmune disorder with periods of exacerbation and remissions; inflammatory response
Laboratory testing includes:
-CBC (decreased Hgb, Hct)
-Platelet count (decreased)
-WBC (decreased)
Treatment and support - treating the inflammation; NSAIDs, corticosteroids, antimalarials (can reduce autoantibodies), dialysis if in renal failure
(molar/butterfly rash (erythema on cheeks))
-
Pituitary Disorders
Growth hormone deficiency
Precocious puberty
Delayed puberty
Diabetes insipidus
Syndrome of inappropriate antidiuretic hormone secretion
-
Growth Hormone deficiency
-hypopituitarism or dwarfism, is characterized by poor growth and short stature
-result of the failure of the anterior pituitary or hypothalamic stimulation on the pituitary to produce sufficient GH.
-lack of GH impairs the body’s ability to metabolize protein, fat, and carbohydrates.
-injury to, or destruction of, the anterior pituitary gland or hypothalamus; tumor, trauma, infection
-genetic syndrome, such as Prader–Willi syndrome or Turner syndrome, or the result of a genetic mutation or deletion
Goal = 3 to 5 in in linear growth in the first year of treatment Treatment stops when the epiphyseal growth plates fuse
-
Precocious Puberty
-Development of sexual characteristics before the usual age of pubertal onset ->secondary sex characteristics develop in girls before the age of 8 years and in boys younger than 9 years
-more common in females, majority of the time the cause is unknown in females
-premature activation of the hypothalamic–pituitary–gonadal system
-Short stature if untreated ->premature closure of growth plates
-Must determine the cause; GnRH analog to halt or reverse growth and development
-
Delayed Puberty
-delayed secondary sexual development
-Girls -if the breasts have not developed by age 12
-boys when no testicular enlargement or scrotal changes have occurred by age 14
-constitutional delay- most common cause, hereditary pattern of growth and development (or a “late bloomer”)
-Therapeutic management involves administering testosterone (males) or estradiol-conjugated estrogen; usually necessary for only a short time to get puberty started
-
Central Diabetes Insipidus (dehydrated)
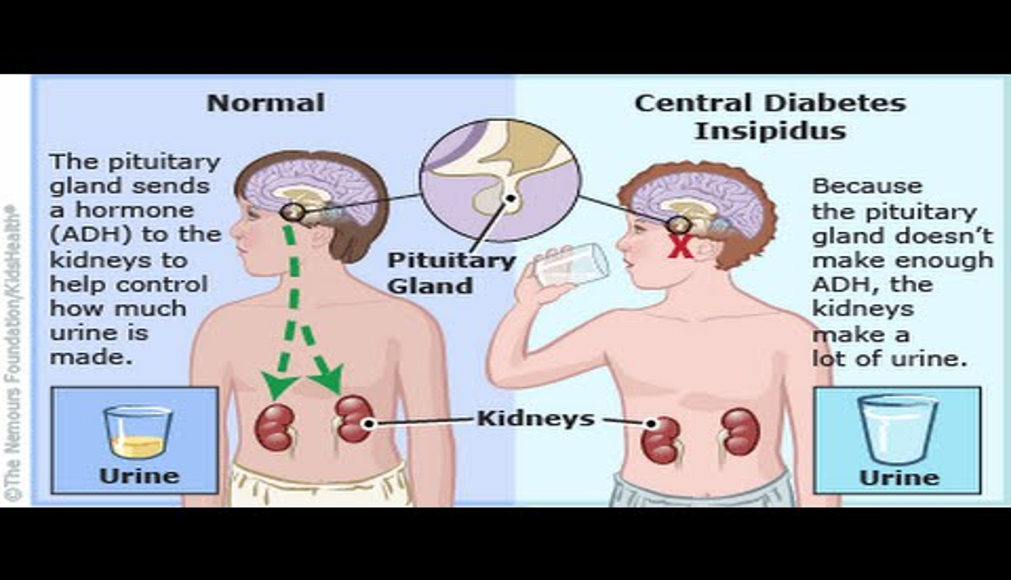
HYPERNATREMIA
•Body produces high urinary output and does not retain water in the correct amount
-low levels Antidiuretic hormone (ADH) aka Vasopressin
-ADH is made in hypothalamus and stored in the kidney
-Damage to pituitary gland, tumor, head injury, illness
•Symptoms –
-Polyuria and polydipsia
-Kidney loses massive amounts of water and retains sodium in the serum
•Treatment
-replacement of ADH/vasopressin à Desmopressin (brand name -DDAVP); can be taken oral or nasal
-low sodium and low protein
-remove tumor if present
-
Syndrome of Inappropriate Antidiuretic Hormone (SIADH)- over hydrated
Too much ADH- HYPONATREMIA
-Causes water retention(low urinary output), decreased serum sodium due to hemodilution, and extracellular fluid volume expansion.
-Caused by CNS infections such as meningitis, head trauma, brain tumors, intracranial surgery, and certain medications such as analgesics, barbiturates, or chemotherapy.
-May be caused by excessive treatment of DI
Therapeutic management -correcting the underlying disorder, fluid restriction, and intravenous sodium chloride administration to correct hyponatremia and increase serum osmolality
-
Hyperthyroidism symptoms
Rare in children
excessive T3,T4
TSH low
Treated with destruction of thyroid gland
Symptoms
-diarrhea
-bulging eyes
-tachycardia
-weight loss
-amenorrhea
-localized edema
-always hot
-
Hypothyroidism symptoms
can be congenital or acquired
-Certain populations at risk (Downs, maternal hypothyroidism)
-Decreased thyroid hormones
Decreased T3, T4
TSH usually elevated
Lifelong thyroid supplementation
Symptoms
-lethargy
-dry skin
-constipation
- always cold
-facial edema
-brittle nails/hair
-weight gain
bradycardia
-
Acquired Hypothyroidism
•Hashimoto
•antibodies develop against the thyroid gland, causing the gland to become inflamed, infiltrated, and progressively destroyed
•Management involves oral sodium L-thyroxine, Synthroid
Symptoms-
•goiter -enlargement of the thyroid gland
•Deep tendon reflexes may be sluggish and the face, eyes, and hands may be edematous
•thinning or coarse hair, muscle hypertrophy with muscle weakness, and signs of delayed or precocious puberty.
•Diagnostic evaluation involves serum thyroid function studies
-
Hyperthyroidism
•Hyperfunction of the thyroid gland, excessive levels of circulating thyroid hormones
•Uncommon in children, 5 times more in girls than boys
•increased rate of growth; weight loss despite an excellent appetite; hyperactivity
•Usually develop a goiter
•Congenital hyperthyroidism -neonatal thyrotoxicosis - occurs in infants of mothers with Graves disease- life threatening, self-limiting disorder lasting 2 to 4 months
•Therapeutic management –decrease thyroid hormone levels. Current treatment involves antithyroid medication, radioactive iodine therapy, and subtotal thyroidectomy. First-line treatment involves methimazole (MTZ, Tapazole) - blocks the production of T3 and T4
-
Signs of Thyroid Storm
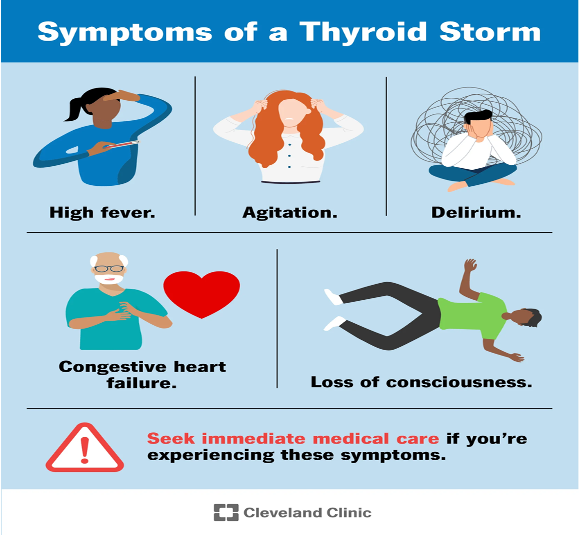
Acute, life-threatening, hypermetabolic state severely elevated Thyroid Hormone
-Graves disease, neonatal graves, thyroid nodules
Symptoms:
•Sudden onset of severe restlessness and irritability
•Fever
•Diaphoresis
•Severe tachycardia
Treatment:
•antithyroid medications, potassium iodide, beta blockers, and steroids.
-
Congenital adrenal hyperplasia
-adrenal glands don’t produce enough cortisol, adrenal gland enlarges to compensate
-Males=enlarged penis, puberty by 2-3; females = ambiguous genitalia(can't tell if boy or girl), fertility issues
-Treatment = hormone replacement, steroids
-
Cushing syndrome
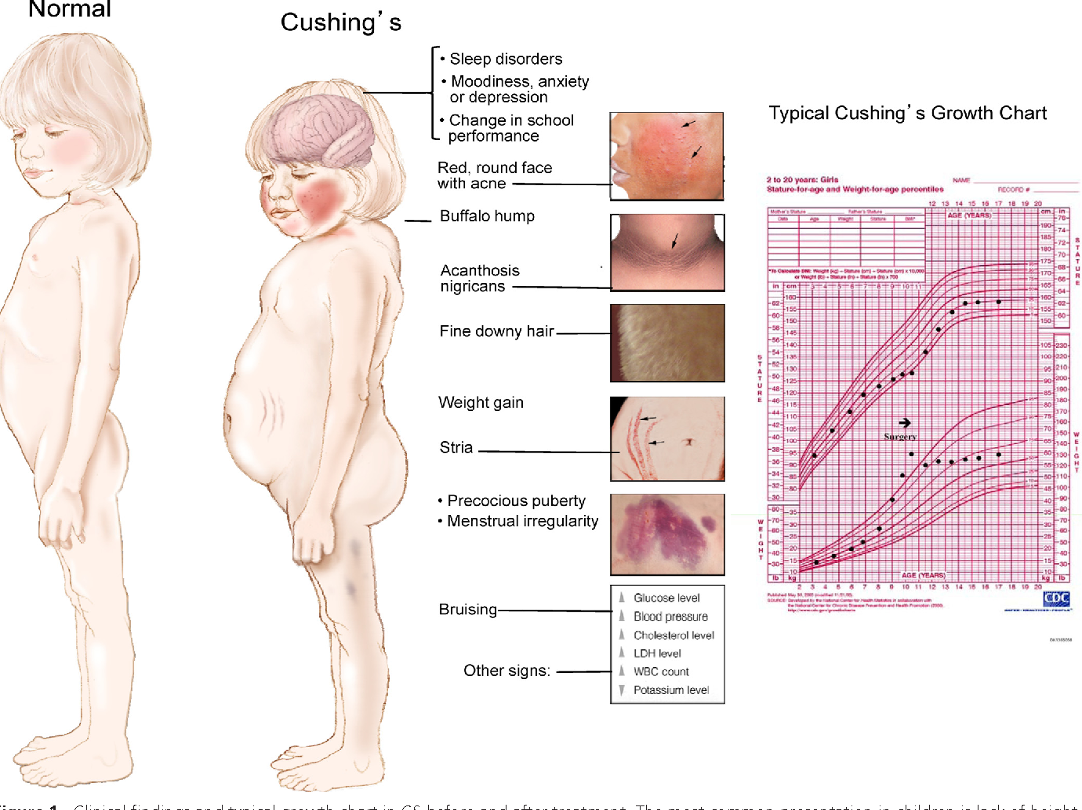
condition from high cortisol levels; caused by use of steroids or overproduction by adrenal glands
-red round face
-hunch back(buffalo hump)
-carry fat in stomach (bulging0
-
Addison disease
adrenal insufficiency – weakness, fatigue, fragile and thin skin
-
Polycystic Ovary Syndrome
testosterone production by the ovaries and adrenal cells is excessive, causing hirsutism, balding, acne, increased muscle mass, and decreased breast size.
-
Role of Insulin
-A hormone made by the islet cells of the pancreas
-Controls the amount of sugar in the blood by moving it into the cells, where it can be used by the body for energy.
-
Diabetes Type 1
autoimmune disorder
-Destruction of beta cells of pancreas ->inadequate insulin secretion ->hyperglycemia
-Kidneys try to lower blood glucose ->glycosuria and polyuria
-Protein and fat are used for energy -> buildup of ketones and acidosis
-
Diabetes Type 2
Pancreas produces insulin but:
-Body is resistant to insulin or there is inadequate insulin produced
-Overtime, insulin production decreases
-
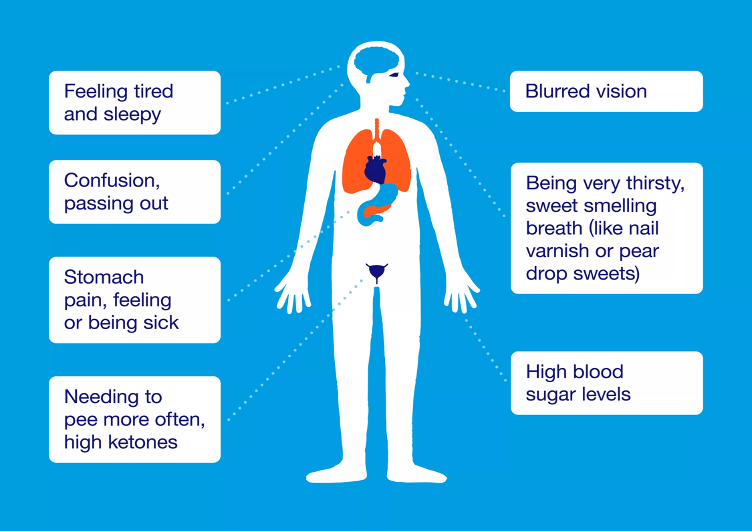
DKA
Body is using fat instead of glucose for energy)
-producing excess blood acids -ketones
-If unrecognized or not treated, DKA – fat catabolism develops
Symptoms:
-anorexia, nausea and vomiting, lethargy, stupor, altered level of consciousness, confusion, decreased skin turgor, abdominal pain, Kussmaul respirations (deep, rapid, labored) and air hunger, fruity (sweet-smelling) or acetone breath odor, presence of ketones in urine and blood, tachycardia, and, if left untreated,.
-
Diabetic Ketoacidosis - DKA management
•blood glucose monitoring
•Hemoglobin A1C – shows blood glucose control over previous 3 months
• daily injections of insulin and/or administration of oral hypoglycemic medications
• a realistic and well-balanced diet
•an exercise program
•self-management and decision-making skills.
-
Insulin Type
Rapid acting- 15 min
Short acting- 30 min-1hr
Intermediate acting- 2-4 hrs
Long acting- 2-4hrs
-
Complications of Diabetes Mellitus
Damage to nerves and vessels d/t prolonged exposure to high blood glucose levels
•Failure to grow
•Delayed sexual maturation(erection)
•Poor wound healing
•Recurrent infections (especially of the skin)
•Retinopathy
•Neuropathy
•Vascular complications
•Nephropathy
•Cerebrovascular disease
•Peripheral vascular disease
•Cardiovascular disease
-
The nurse is caring for a child diagnosed with juvenile diabetes. Which of the following medical treatments would be appropriate for this child?
a. Surgery
b. Irradiation
c. Radioactive iodine
d. Glucose monitoring
d. Glucose monitoring. Glucose monitoring is an intervention appropriate for managing diabetes.

