-
Check for Assessment
-Health hx
-physical exam (least - most invasive)
-Inspection and observation
-color- icteric(yellow/ jaundice)
-Hydration- absence of tears (dehydration
-Abdomen size and shape- protuberant- ascites, fluid, gas, tumor; depressed- high and. obstruction or dehydration (inspection, auscultation, percussion, papatation)
-Mental status- lethargy
-
Auscultation
-Auscultate all four quadrants
-Nurse can determine absence of bowel sounds after 5 minutes period (can be difficult with infants/children)
-
Hyperactive bowel sounds
Can be noted in children with diarrhea or gastroenteritis
-
Hypoactive or absent bowel sounds
Can signify an obstructive process
-Immediately report hypoactive or absent findings to physician
-
Percussion
-Can reveal normal finding of dullness or flatness along the right costal margin and 1 to 3 cm below costal margin of liver
-area above symphysis pubis may be dull in young children with full bladders (normal finding)
-Percussion of remainder abdomen should reveal tympany
-
What to know about pediatric patients?
increased risk of hemorrhage
Premature infants have greater risk of bleeds because of more capillaries
-
Head size
Size in infant/young children is larger than body
Head continues to grow until 5 years of age
-
Nervous system
complete but immature at birth
-
Health History
Prematurity, difficult birth, infection during pregnancy, genetic disorders, seizure disorders, headaches, nausea, vomiting, changes in gait, visual disturbances, recent trauma, lethargy, poor feeding, increased irritability, fever,
-
Inspection and Observation
Level of consciousness
vital signs
head, face, neck
cranial nerve function
motor function
reflexes
sensory function
Increased ICP
-
Level of consciousness
Alertness and ability to respond to stimuli and show verbal or motor response
-5 states
-Full consciousness
-confusion: disoriented, responds inappropriately to questions
-Obtunded: limited responses and falls asleep if not stimulated
-Coma: not arousable
-
Head, Face , Neck
size and shape of head, asymmetry, head circumference
-
Cranial nerve function
Dolls eyes maneuver (turn head right, eyes should look left
Nystagmus: static
Sunset eyes
-
Sensory Function
Distinguish between light touch, pain, vibration, heat and cold
-
Scoring
-Less than or equal to 12 suggests severe head injury
-Score less than 8 suggests need for intubation and ventilation
-Score less than or equal to 6 suggests need for intracranial pressure monitoring
(The higher the score, the better/ the lower the score means lower level of consciousness)
-
Pediatric Glasgow Coma Scale
Eye test
-
Cranial nerves
-olfactory
-optic
-trigeminal
-facial
-acoustic
-glossopharyngeal
-accessory
-hypoglossal
-
Changes in motor function
Abnormal posturing due to brain injury
Decorticate- extremities flexed
Decerebrate- extremities extended and pronated (on stomach)
-
Palpation and auscultation for neurologic disorder
Palpitation of newborn or infant skulls and fontanels (feeling inflammation or depression)
Bruits (whooshing sound)- vibrations resulting from turbulence in intracranial vessels (abnormal)
-
Increased ICP
sign of neurologic disorder
Possible causes
-head trauma
-birth trauma
-hydrocephalus
-infection
-brain tumors
-
Early signs of ICP
headache
projectile vomiting
visual changes
dizziness
decreasing HR and respirations
changes in pupil reactions
sunset eyes
changes in LOC
seizures
bulging fontanel and increasing head circumference
-
Late signs of ICP
Decreased LOC
Depressed motor, sensory
responses
bradycardia
irregular respirations
cheyne- stokes respirations
decerebrate/decorticate postures
fixed and dilated pupils
-
Types of neural structural defects
Neural tube defects
Microcephaly
Arnold-Chiari malformation
Hydrocephalus
Intracranial Arteriovenous malformation: AVM
Craniosynostosis
Positional Plagiocephaly
-
Neural tube defects
Occurs 1st few weeks of embryonic life
ex. spina bifida, myelomeningocele, meningocele, anencephaly
Drugs, malnutrition, chemicals, and genetics
-
Microcephaly
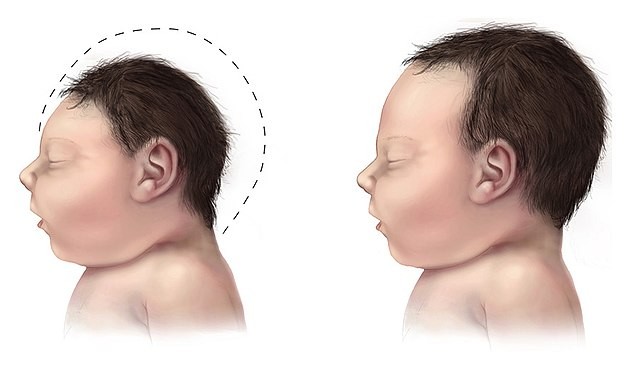
HC3 standard deviations below the mean for age and the sex of the child
Can be congenital (genetic) or acquired (malnutrition, perinatal infection, anoxia)
-
Arnold-Chiari malformation
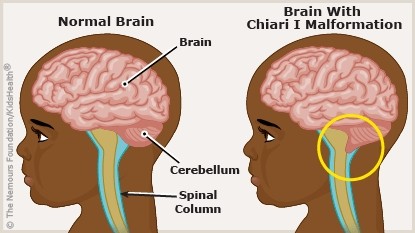
Downward displacement of cerebral structures
Cerebellum, medulla oblongata, and the 4th ventricle are displaced into the cervical canal causing obstruction to CSF flow and resulting in Hydrocephalus
-
Hydrocephalus
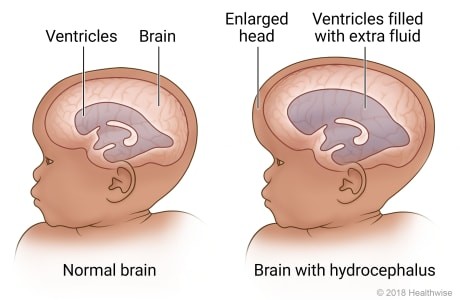
imbalance in the production and absorption of the CSF; obstruction to the flow of CSF
-increased head size
-loss of developmental milestones
-changes in personality in older children
MAY REQUIRE SURGICAL INTERVENTION TO RELIEVE PRESSURE WITH A VENTRICULAR SHUNT
-
Intracranial Arteriovenous malformation: AVM
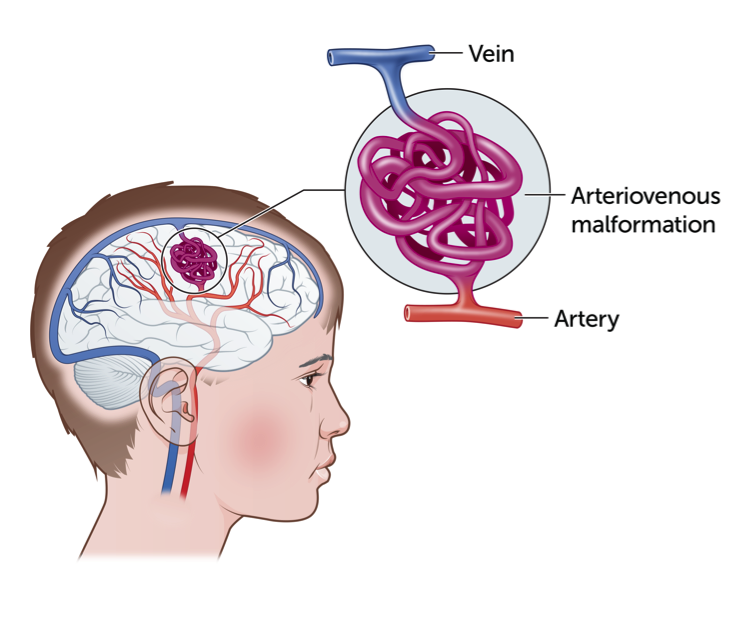
Irregular. connected and poorly formed blood vessels; can cause bleeding, seizures
-
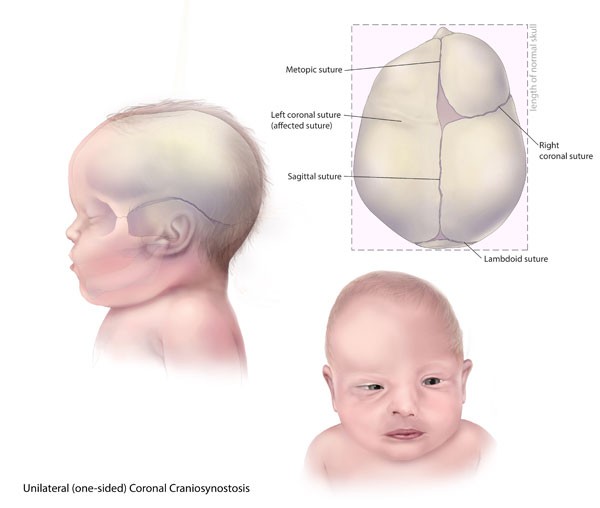
Craniosynostosis
Premature closure of the sutures
-
Positional Plagiocephaly
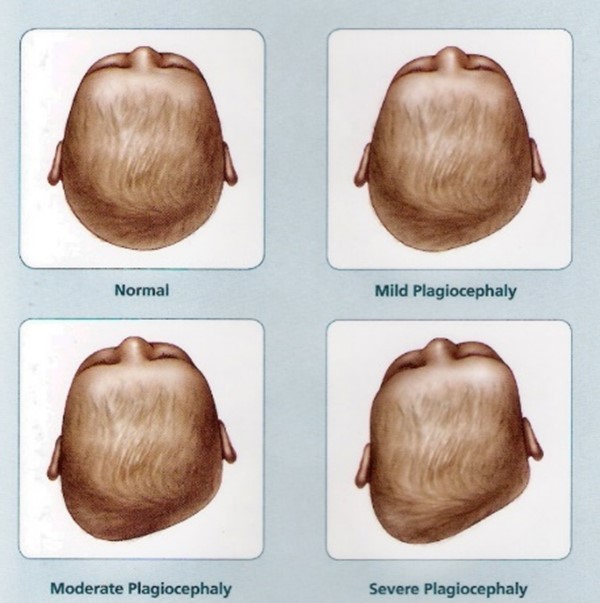
Asymmetry of head without fused sutures
-
Shunt
hollow tube surgically placed in brain to drain cerebrospinal fluid and redirect it to another location in the body where it can be reabsorbed
-
Signs and symptoms of shunt infection
-elevated vital signs
-poor feeding
-vomiting
-decreased responsiveness
-seizure activity
-signs of local inflammation along the shunt tract
-
Types of Seizure
Infantile spasms: spasm seen in infancy 3-12 m
Absence: uncommon before 5 years old, staring, twitching
Tonic: stiffening of muscles, arms legs, back
Clonic: muscle will spasm, jerk and then relax
Tonic-clonic: combination of above
Myoclonic: sudden brief muscle jerks that involve entire body or one part (may lose consciousness )
Atonic: drop seizures, sudden loss of muscle tone, may lose consciousness
Focal seizure without impairment of consciousness: tonic clonic movements, sensory autonomic, psychic symptoms
Focal seizure with impaired consciousness: automatisms and complex purposeful movements
status epileptics: neurologic emergency, lasting more than 5 min/ 2 or more within 5 min
Febrile seizure
-
Febrile Seizures
Most common type, seen in children less than 5
Associated with 102.2F temperature or higher
Benign
-
Bacterial Meningitis
Infection of meninges
Serious illness that can lead to brain damage, nerve damage, deafness, stroke and even death
-Causes inflammation, swelling, purulent exudates, tissue damage to brain. Can occur secondary to sinus or ear infection
-MEDICAL EMERGENCY
-May rest in muscles in back, neck and legs spasm and contract (neck pain, bulging fontanel)
-Positive(bad) kerning and Brudzinski signs: indicate irritation of meninges
Inspect child for rash
-
Kernig's sign

supine patient, with hips and knees flexed, extend the leg passively. The test is positive if leg extension causes pain
-
Brudzinski's sign
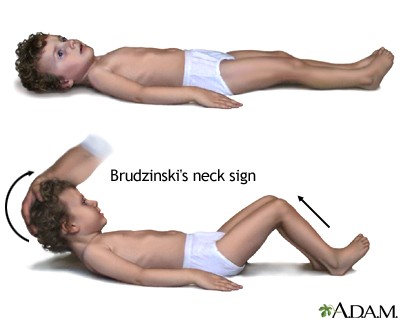
is positive when passive forward flexion of neck causes the patient to involuntarily raise his knees or hips in flexion
-
Spinal tab/ LP
-Laying on side, knees to chest
-leaning forward, legs flexed
-
Medications to treat
Antibiotics
Anticonvulsants
Bensodiazepines
Analgesics
Osmotic diuretics
Corticosteriods
-
Positional alterations
Internal tibial torsion: Lower extremities have bowed appearance
Genuine Valgum: knock knees; knees touch and ankles are significantly separated; resolves by 7-8 y/o
in-toeing: normal finding; feet remain flexible and passively move to midline
Pes planus: (flat feet) noted in infants when they begin to walk; arch develops as they grow
-
Fractures
rule out possibility of abuse
-
Casts
Immobilize bone that's injured or deseased
serves to hold the bone in reduction (preventing deformity as it heals)
keeps bones aligned
reduce pain and allow child increased mobility
-
Type of casts
Short arm cast (forearm)
Long arm cast (full arm)
Shoulder spica cast (one shoulder and down waist)
Long leg cast (full cast)
Short leg cast (calf)
Long leg hip spica cast (chest to both full legs)
One and a half hip spica cast (hip to one full leg and half of other)
Abduction boots (full legs)
-
Traction
method of immobilization
-
External fixation
-Used for complicated fractures, especially open fractures with soft tissue damage
-A series of pins or wires are inserted into bone and then attached to an external frame
-INFECTION
-
Spina Bifida Occulta (can't be seen)
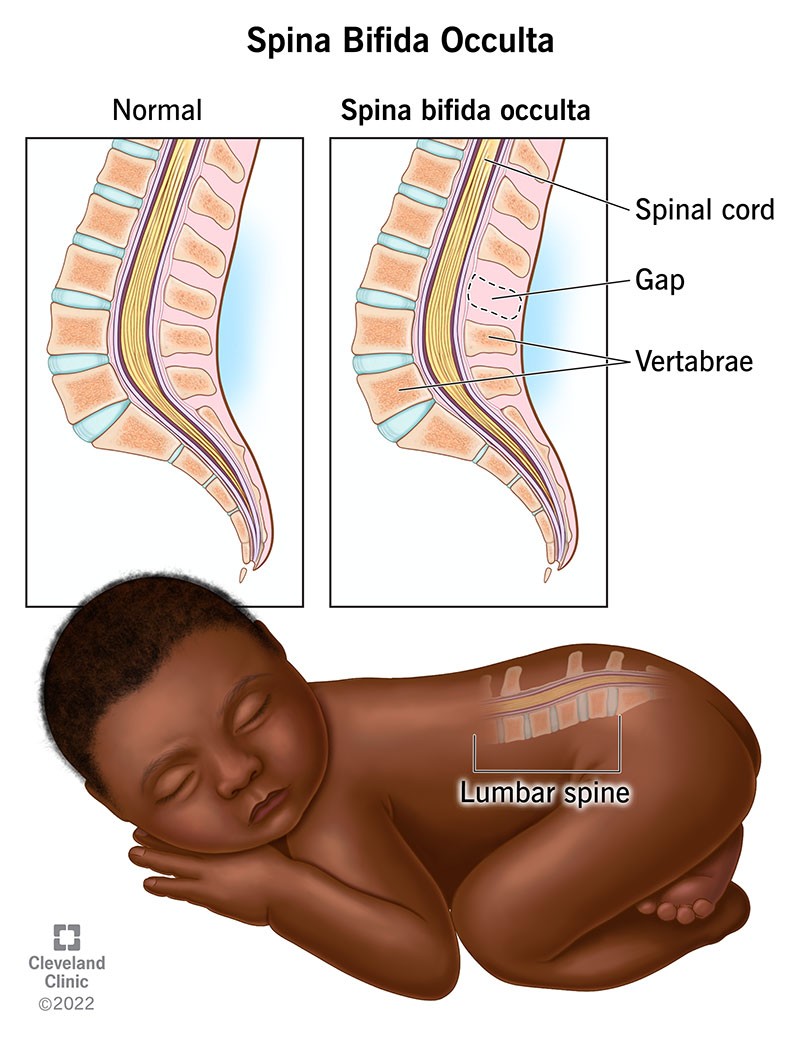
-defect of vertebral bodies without protrusion of spinal cord or meninges
-not visible externally and in most cases no adverse effects
-need no immediate medical intervention
-complications are rare, abnormalities of spinal cord
-dimpling or tats of hair in lumbosacral area- MRI
-
Neural tube defects
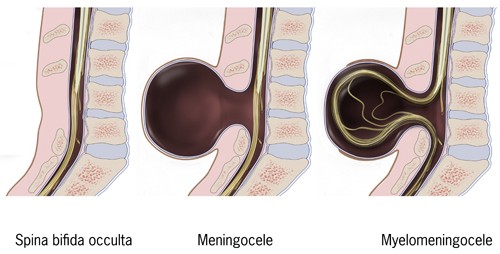
spina bifida cystica- meningocele and myelomeningocele
Meningocele- meninges herniate through a defect in the vertebrae
visible external sac protruding from spinal area: care to prevent rupture of sac
Treatment included surgical correction of lesion
Myelomeningocele- most severe
spinal cord often ends at the point of defect, resulting in absent motor and sensory function
long term complications pf paralysis, orthopedic deformities, and bladder and bowel incontinence
accompanying hydrocephalus
-
Nursing management of myelomeningocele
Preventing infection
Promoting urinary elimination
Promoting bowel elimination
Promoting adequate nutrition
Preventing latex allergic reaction
Maintain skin integrityEducating and support child and family
-
Chest Wall Deformities
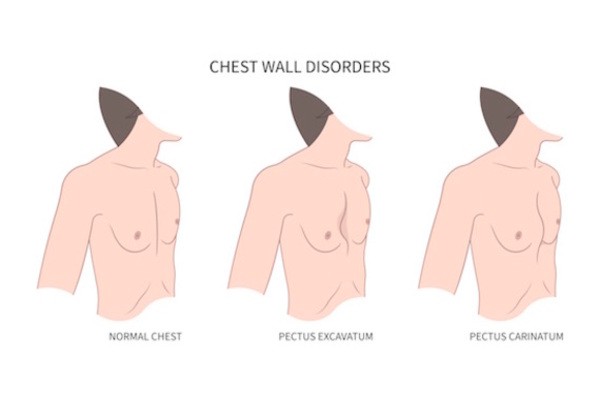
Pectus excavatum: funnel shaped chest, depression that sinks inward is apparent at diploid process, progresses with growth. When pectus more pronounced, cardiac and pulmonary compression occurs
Pectus carinatum: protuberance of the chest wall, accounts for only 5 to 15% of anterior chest wall deformities
-
Limb deficiencies
absence of limb
-
Amniotic bands
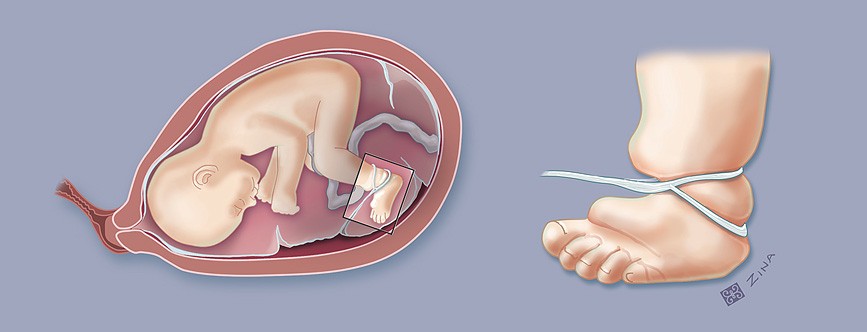
wrapping of limp and causes no blood flow
-
Polydactyly
Presence of extra digits on hand or foot
-involves digits at border of hand or foot, can occur by any central digit
-note if there is bone present
-possible surgical
-
Syndactyly

Webbing of fingers and toes
-
Metatarsus Adductus
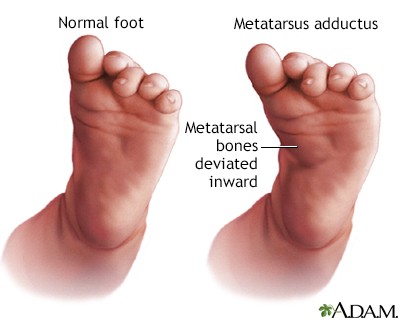
Medal deviation of forefoot
-occurs most commonly in utero
-observation
-stretching
-serial casting
surgery-rarely
-
congenital club foot
Talipes varus (inversion of heel)
talipes equinus (plantar flexion of foot; heal raised and would not strike ground in standing position)
Foot resembles the head of a golf club
-
Cerebral Palsy
Caused by damage or abnormal development in parts of brain that control movement
-Some children with CP will have cognitive issues
-Symptoms include exaggerated reflexes, floppy or rigid limbs, and involuntary motions
Complication: mental impairments, seizures, growth problems, impaired vision/hearing, abnormal sensation and hydrocephalus
Ataxia: lack of coordination of muscle movements during voluntary movements such as walking or picking up objects
-
Osteogenesis Imperfecta
sclera may have blue, purple or gray tint
results in low bone mass, increased fragility of bones, connective -tissue problems such as hyper mobility, instability of joints
-fractures
goal is to decrease fractures and maintain mobility
-
Hip Dysplasia
asymmetric gluteal, thigh, labial folds
-
Torticollis
-painless muscular condition
-may result in utero positioning or difficult birth
-preferential turning head to one side while lying supine (flatten head one side)
-results from tightness of sternocleidomastiod muscle
-plagiocephaply
-
Tibia Vara (Blount disease)
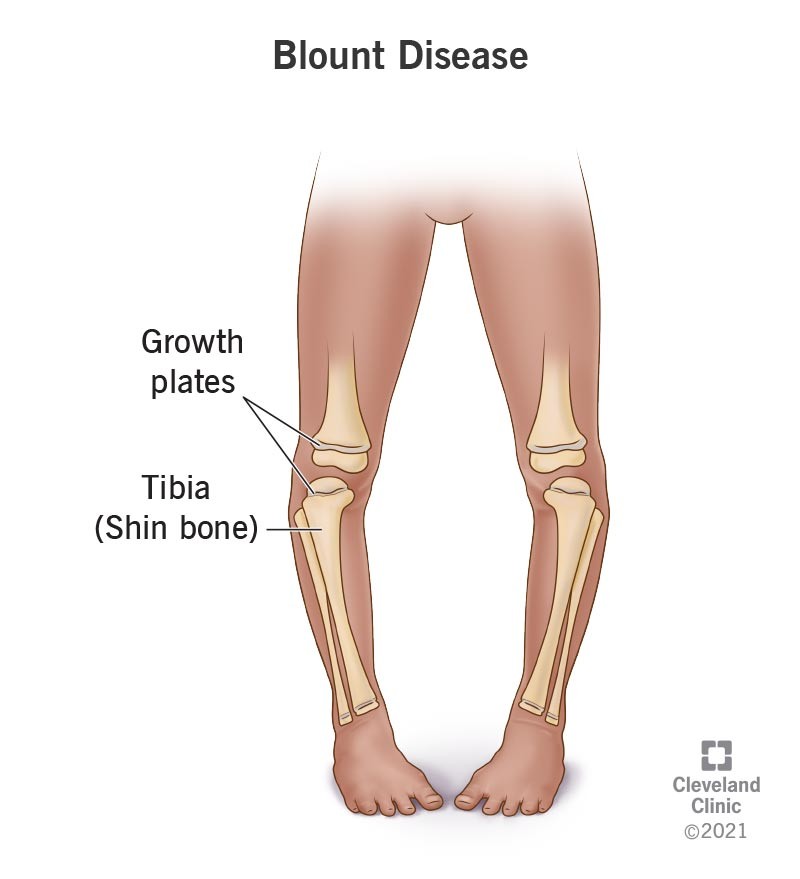
normal physiologic bowing or gene vacuum becomes more pronounced in the child with tibia vara
-occurs in early walkers, associated with obesity
-If left untreated, growth plate of upper tibia ceases bone production
-assymetric growth at knee
-
Muscular dystrophy
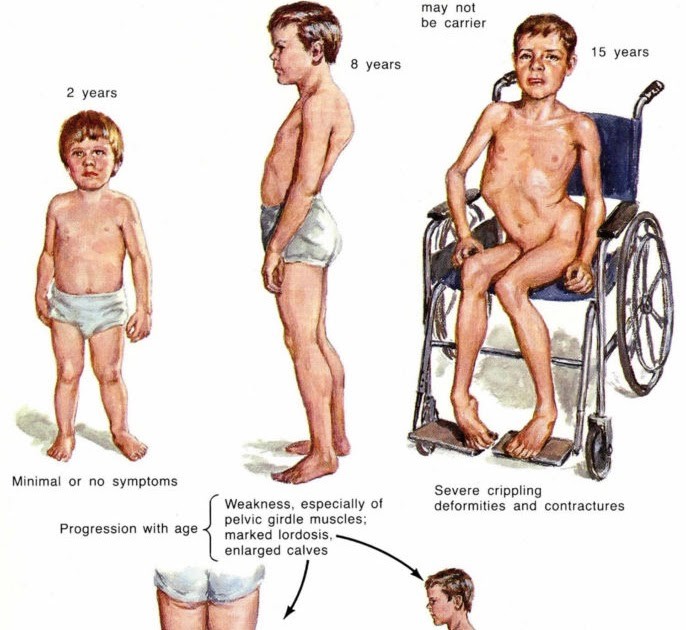
Duchaunee
inherited genetic disorder
progress muscle weakness and wasting
no cure, steroids may slow
Hall mark sign: Gowers sign- difficult to stand up from floor
-
Rickets
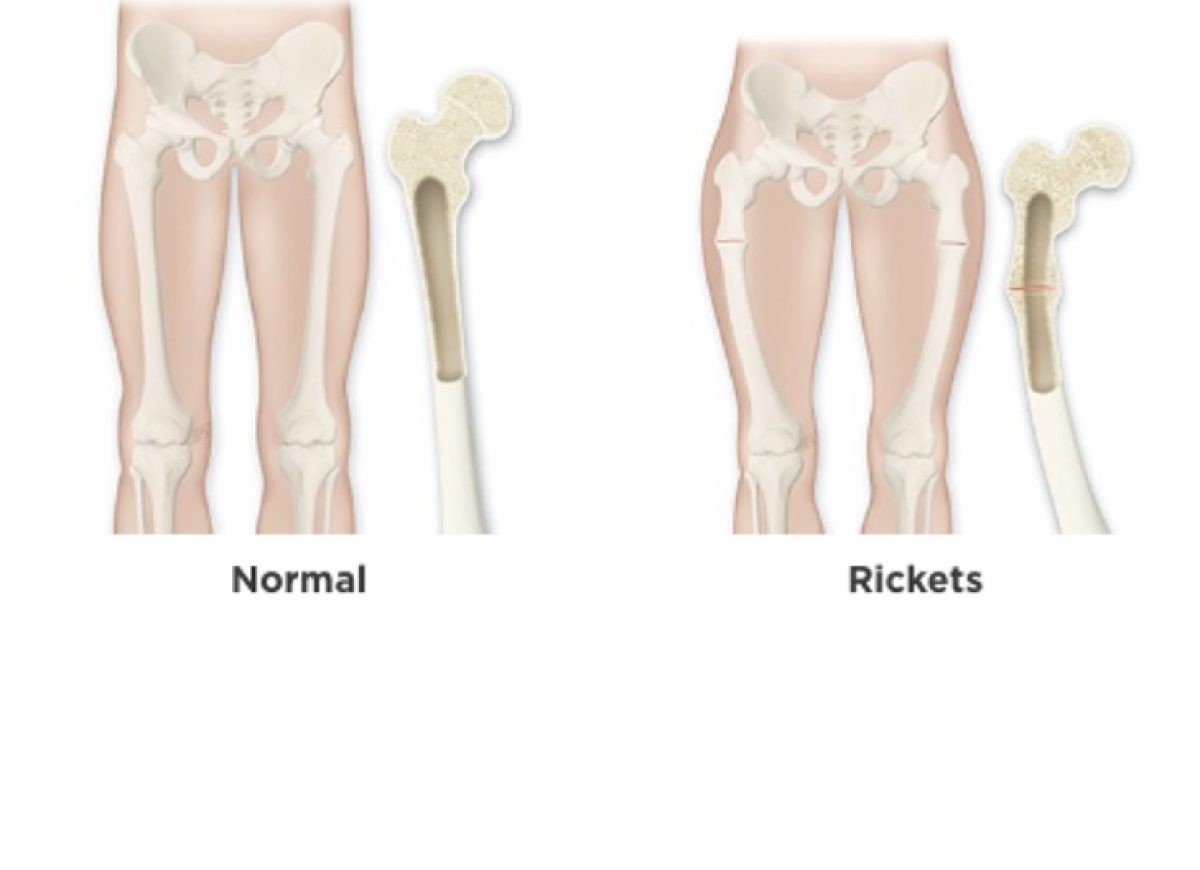
-Softening or weakening of the bones
-Childhood rickets may occur as a result of nutritional deficiencies such as inadequate consumption of calcium or vitamin D or limited exposure to sunlight (required for adequate production of vitamin D).
Rickets caused by vitamin D deficiency is a preventable condition
-
Scoliosis
Lateral curvature of the spine greater than 10 degrees
-May be congenital, associated with other disorders, or acquired
-Assess: auscultate heart and lung sounds to make sure there is no compromise
-Management
Braces (multiple types based on severity)Surgical repair for severe cases - for curve greater than 45 degreesEncourage compliance if bracedPost-op careBody image
-
Slipped capital femoral epiphysis
Femoral head dislocates from the neck and shaft of femur at the level of the epiphyseal plate
-left hip is more often affected-Chronic SCFE may lead to shortening of the affected leg and thigh atrophy
-
Transient synovitis of hip
-Also termed toxic synovitis
-The exact cause is unclear, but it is thought to be associated with recent or active infection, trauma, or allergic hypersensitivity
-It is a self-limiting disease and most cases resolve within a week, but it may last as long as 3 to 6 weeks.
-
Signs and symptoms of spinal cord injury
-Emergency
-Immobilization
-Prevention!
-Inability to move or feel extremities
-Numbness
-Tingling
-Weakness
-Loss of voluntary movement below the level of the lesion
-Inability to breathe, if injury is at a high cervical vertebra
-
Sprains
Twisting or turning motion of affected body part
tendons and ligaments stretch excessively and may tear slightly
-Want inflammation (body doing what it needs)
MEAT:
-Movement
-Exercise
-Analgesics
-Treatment
-
Nursemaid's elbow
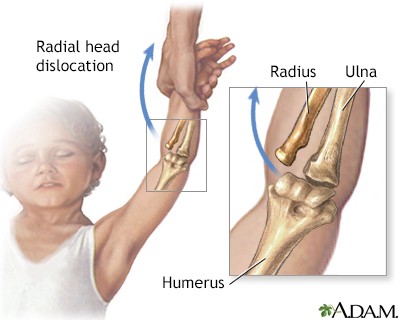
occurs when radius slips out of place from where it normally attaches to the elbow joint
-immediate pain
-refusal or inability to move arm
-
A 6-month-old infant is admitted with a diagnosis of bacterial meningitis. Which room is appropriate for this infant?
a. room with a 12-month-old infant who has a urinary tract infection
b. room with an 8-month-old infant with failure to thrive
c. private room near the nurses’ station
d. multibed room with other infants who have bacterial meningitis
c. private room near the nurses' station
-
The nurse is caring for a 6-year-old child who has a history of febrile seizures and is admitted with a temperature of 102.2°F (39°C). What is the nurse's highest priority?
a. Institute safety precautions.
b. Offer age-appropriate activities.
c. Provide family teaching related to the child's history.
d. Encourage the child to do his or her own self-care.
a. Institute safety precautions
-
. A nurse is preparing a presentation for a group of expectant parents about neural tube defects and prevention. Which would the nurse emphasize?
a. smoking cessation
b. aerobic exercise
c. increased calcium intake
d. folic acid supplementation
d. folic acid supplementation
-
What finding is consistent with increased intracranial pressure (ICP) in an infant?
a. Emotional lability
b. Increased appetite
c. Narcolepsy
d. Bulging fontanels (fontanelles)
d. Bulging fontanels (fontanelles)
-
During the physical assessment of a 2½-month-old infant, the nurse suspects the child may have hydrocephalus. Which sign or symptom was observed?
a. Dramatic increase in head circumference
b. Pupil of one eye dilated and reactive
c. Vertical nystagmus
d. Posterior fontanel (fontanelle) is closed
a. Dramatic increase in head circumference
-
The nurse is observing an infant who may have acute bacterial meningitis. Which finding might the nurse look for?
a. Flat fontanel (fontanelle)
b. Irritability, fever, and vomiting
c. Jaundice, drowsiness, and refusal to eat
d. Negative Kernig sign
b. Irritability, fever, and vomiting
-
A pregnant client asks if there is any danger to the development of her fetus in the first few weeks of her pregnancy. How should the nurse respond?
a. “As long as you were taking good care of your health before becoming pregnant, your fetus should be fine during the first few weeks of pregnancy.”
b. “Bones begin to harden in the first 5 to 6 weeks of pregnancy, so vitamin D consumption is particularly important.”
c. “During the first 3 to 4 weeks of pregnancy, brain and spinal cord development occur and are affected by nutrition, drugs, infection, or trauma.”
d. “The respiratory system matures during this time, so good prenatal care during the first weeks of pregnancy is very important.”
c. “During the first 3 to 4 weeks of pregnancy, brain and spinal cord development occur and are affected by nutrition, drugs, infection, or trauma.”
-
A 4-year-old child is brought to the emergency department after being in a motor vehicle accident. The child experienced head trauma in the accident. When assessing the child, which will be the first change noted in the presence of increasing intercranial pressure?
a. change in level of consciousness
b. reduction in heart rate
c. increase in heart rate
d. decline in respiratory rate
a. change in level of consciousness
-
What information is most correct regarding the nervous system of the child?
a. The child's nervous system is fully developed at birth.
b. As the child grows, the gross and fine motor skills increase.
c. The child has underdeveloped fine motor skills and well-developed gross motor skills.
d. The child has underdeveloped gross motor skills and well-developed fine motor skills.
b. As the child grows, the gross and fine motor skills increase.
-
A nurse is assessing a 3-year-old child for possible bacterial meningitis. Which sign would indicate irritation of the meninges?
a. Positive Kernig sign
b. Negative Brudzinski sign
c. Positive Chadwick sign
d. Negative Kernig sign
a. Positive Kernig sign
-
Preterm infants have more fragile capillaries in the periventricular area than term infants. This put these infants at risk for which problem?
a. moderate closed-head injury
b. early closure of the fontanels (fontanelles)
c. congenital hydrocephalus
d. intracranial hemorrhaging
d. intracranial hemorrhaging
-
A nurse is talking with the parents of a child who has had a febrile seizure. The nurse would integrate an understanding of what information into the discussion?
a. The child's risk for cognitive problems is greatly increased.
b. Structural damage occurs with febrile seizure.
c. The child's risk for epilepsy is now increased.
d. Febrile seizures are benign in nature.
d. Febrile seizures are benign in nature.
-
A nurse is applying a cast to a 12-year-old boy with a simple fracture of the radius in the arm. What is most important for the nurse to do when she has finished applying the cast?
a. Assess the fingers for warmth, pain, and function
b. Apply a tube of stockinette over the cast
c. Cut a window in the cast over the wrist
d. X-ray the cast to make sure the bones are aligned properly
a. Assess the fingers for warmth, pain, and function
-
A nurse has provided care to several children during their well-child visits. The nurse has assessed each child’s neurologic status. Which assessment finding indicates a problem requiring intervention?
a. a 2-month-old infant who reaches for a rattle several times before connecting with it
b. a 10-month-old infant who is able to ambulate with assistance
c. a 2-year-old toddler who can walk up the steps one at a time
d. a 4-year-old preschool-age child who consistently walks on tiptoes
d. a 4-year-old preschool-age child who consistently walks on tiptoes
-
The nurse is educating a group of caregivers about fractures seen in children. One of the caregivers states, “I have heard that if a bone breaks it can cause permanent damage and stop the growth of the bone.” This statement is accurate if the break occurs in the:
a. humerus.
b. joint.
c. xiphoid process.
d. epiphyseal plate.
d. epiphyseal plate.
-
The nurse is caring for a 14-year-old client in traction prior to surgery. The client has been in the hospital for 2 weeks and will require an additional 10 days in the hospital following surgery. The client states, "I feel isolated and I am refusing any more treatment." Which response by the nurse is most appropriate?
a. “I know it is boring here, but the best place for you to remain immobile is the hospital.”
b. "I will see if you can have friends come spend a few nights with you.”
c. “Let's come up with things for you to do and see if your friends can come visit.”
d. “If you refuse further treatment, your condition will only get worse.”
c. “Let's come up with things for you to do and see if your friends can come visit.”
-
The nurse receives a report on a child admitted with severe muscular dystrophy. The nurse suspects the child has been diagnosed with the most severe form of the disease, known as:
a. Duchenne.
b. facioscapulohumeral.
c. limb-girdle.
d. myotonia.
a. Duchenne.
-
A nurse is providing instructions for home cast care. Which response by the parent indicates a need for further teaching?
a. “We must avoid causing depressions in the cast.”
b. “Pale, cool, or blue skin coloration is to be expected.”
c. “The casted arm must be kept still.”
d. “We need be aware of odor or drainage from the cast.”
b. “Pale, cool, or blue skin coloration is to be expected.”
-
An infant has been born and diagnosed with a meningocele. Which action will the nurse incorporate into each contact with this infant?
a. inspection of the cystic sac on the child’s back for leakage
b. auscultation for bowel sounds
c. listening for a shrill cry
d. careful supine positioning
a. inspection of the cystic sac on the child’s back for leakage
-
The pediatric nurse practitioner (PNP) records "positive Gowers' sign" after finishing the assessment of a young boy. How will the student nurse reading the PNP's note interpret this?
a. The boy has a large tan skin lesion on his torso.
b. Severe lordosis is evident in the lumbar spine.
c. The head is held tilted with limited side-to-side motion.
d. The boy rises from the floor by walking his hands up his legs.
d. The boy rises from the floor by walking his hands up his legs.
-
The parents of a infant born with an abnormality on the back are told by the neonatologist that their child has a myelomeningocele. They ask the nurse what exactly that means. Which would be the nurse's best reply?
a. "It is a herniation through the skin of the back of your child with both the spinal cord and nerve roots involved."
b. "The contents of the sac you see only has fluid in it and should cause the child no problem."
c. "Your child's defect involves only the nerves to the bladder and bowel and can be easily repaired."
d. "The sac is a very small cyst and should resolve within the first year of life."
a. "It is a herniation through the skin of the back of your child with both the spinal cord and nerve roots involved."
-
What information would the nurse include in the preoperative plan of care for an infant with myelomeningocele?
a. positioning supine with a pillow under the buttocks
b. covering the sac with saline-soaked nonadhesive gauze
c. wrapping the infant snugly in a blanket
d. applying a diaper to prevent fecal soiling of the sac
b. covering the sac with saline-soaked nonadhesive gauze
-
The nurse is assessing the neuromusculoskeletal system of a newborn. What is an abnormal assessment finding?
a. sluggish deep tendon reflexes
b. full range of motion in extremities
c. absence of hypotonia
d. lack of purposeful muscular control
a. sluggish deep tendon reflexes
-
An 8-year-old girl was diagnosed with a closed fracture of the radius at approximately 2 p.m. The fracture was reduced in the emergency department and her arm placed in a cast. At 11 p.m. her mother brings her back to the emergency department due to unrelenting pain that has not been relieved by the prescribed opioids. Which action would be the priority?
a. Notifying the doctor immediately
b. Applying ice
c. Elevating the arm
d. Giving additional pain medication as ordered
a. Notifying the doctor immediately
-
When developing the plan of care for a child with cerebral palsy, which treatment would the nurse expect as least likely?
a. skeletal traction
b. physical therapy
c. orthotics
d. occupational therapy
a. skeletal traction
-
Risk Factors for Respiratory Disorders
•Prematurity
•Chronic illness (diabetes, sickle cell anemia, cystic fibrosis, congenital heart disease, chronic lung disease)
•Developmental disorders (cerebral palsy)
•Passive exposure to cigarette smoke
•Immune deficiency
•Crowded living conditions or lower socioeconomic status
•Daycare attendance
-
Nursing Assessment for Child with Respiratory Distress
•Health history – PMH, FH, Hx present illness, immunization hx, exposure to smoke
•Atopy –genetic tendency to asthma, allergic rhinitis, atopic dermatitis
•Physical exam
•Inspection and observation
•Palpation
•Percussion
•Auscultation
-
Inspection and Observation
•Anxiety and restlessness
•Color: pallor, cyanosis
•Hydration status
•Clubbing
•Breath sounds
•Rate and depth of respirations: tachypnea
•Respiratory effort
•Nose and oral cavity
•Cough and other airway noises: stridor
-
Adventitious Breath Sounds
•Wheezing
•High-pitched sound usually heard on inspiration; sometimes on expiration
•May occur with obstruction in lower trachea or bronchioles
•May occur in asthma or viral infections
•Rales
•Crackling sounds heard when alveoli become fluid filled
•May occur with pneumonia
-
Common Medical Treatments for respiratory
•Oxygen
•High humidity
•Suctioning
•Chest physiotherapy and postural drainage
•Saline gargles or lavage
•Mucolytic agents
•Chest tubes
•Bronchoscopy
-
Acute respiratory Infectious Disorders
•Common cold – viral URI or nasopharyngitis; e.g., Respiratory syncytial virus (RSV);
•Sinusitis – bacterial; acute or chronic
•Influenza – viral infection; ‘the flu’; bacterial infections may follow
•Pharyngitis, tonsillitis– often viral
•Laryngitis – inflammation of larynx
•Croup syndromes – parainfluenza main cause; inspiratory stridor; worse at night
•Pneumonia and bronchitis
•Infectious mononucleosis –caused by Epstein-Barr virus; ‘kissing disease’, often in adolescence; spleen rupture, Guillain-Barre syndrome; meningitis
-
Signs and Symptoms of Bronchiolitis (RSV)
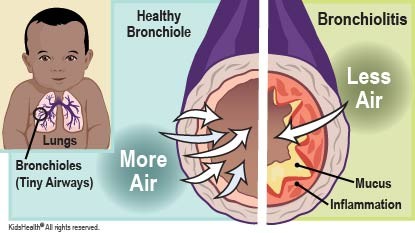
•Onset of illness with a clear runny nose(sometimes profuse)
•Pharyngitis
•Low-grade fever
•Development of cough 1 to 3 days into the illness, followed by a wheeze shortly thereafter
Poor feeding

