Micturition (Physiology)
Session Summary This session introduces you to micturition - the act of urination - which is elegantly illustrated here by Brussels' famous Manneken Pis statue. Elegance is subjective, of course. Micturition ends the series of lectures on the kidney, although the kidney features only briefly here. We begin by following the movement of urine from the kidney to the bladder, via the ureter. The majority of the lecture is on the bladder, in particular how its anatomy and innervation allow this organ to switch between filling with urine and expelling urine, and how bladder function is under both involuntary and voluntary control. Along the way, we cover various clinical problems that can occur within the urinary tract, and how these can be managed. Apologies in advance for every time I mispronounce micturition as micturation! This session was adapted from a previous lecture by Dr Suman Rice. Learning outcomes At the end of this session you will be able to understand: The transport of urine from the kidney to the bladder The anatomy of the bladder & sphincters The innervation of the bladder Motor innervation Sensory innervation The process of bladder filling & emptying (micturition) The micturition reflex Problems associated with bladder ageing Treatments for bladder conditions
-
What is the pathway of urine from the kidney to the ureter? (3)
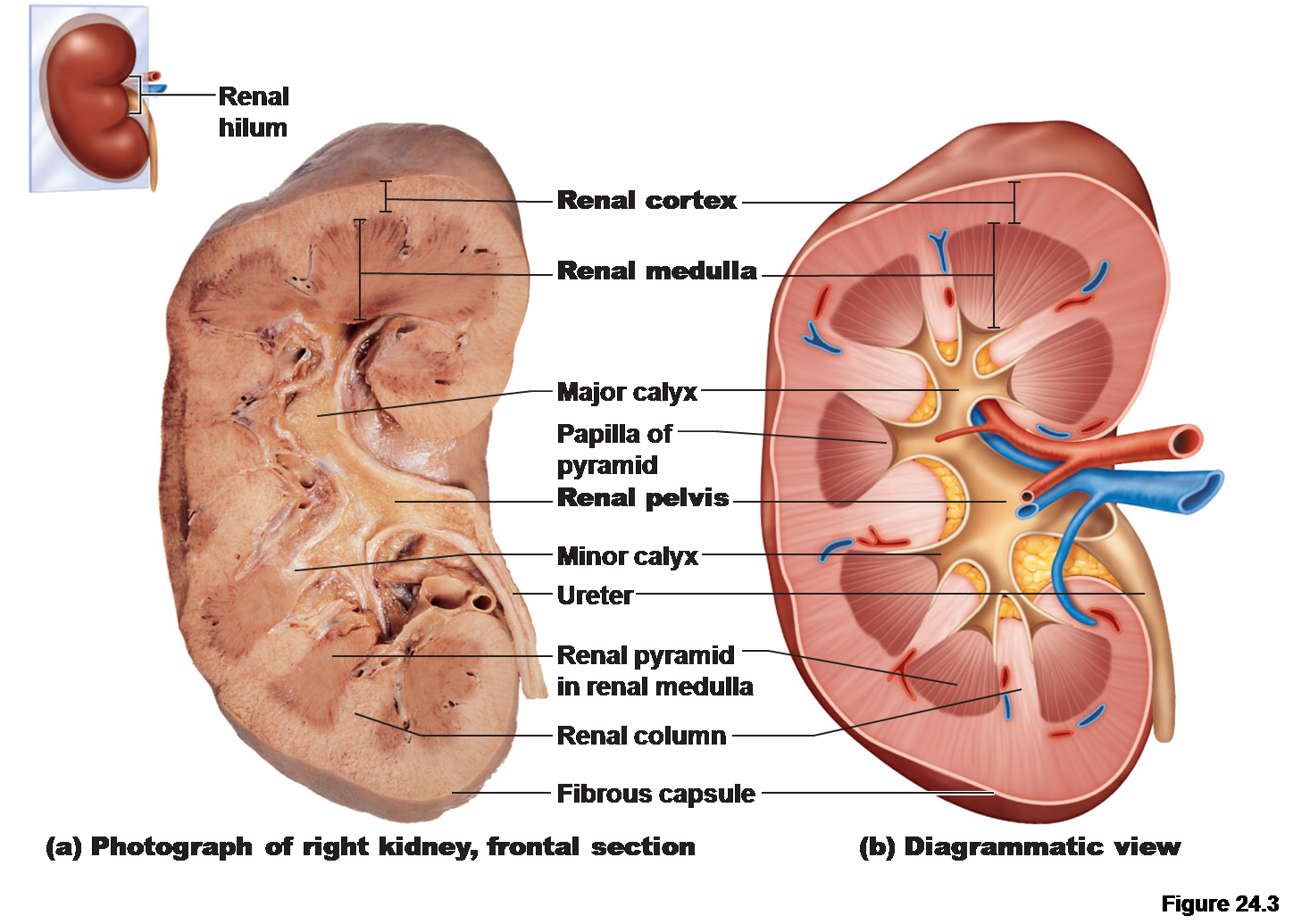
✶Urine from all collecting ducts of all nephrons
✶Empties into the renal pelvis
✶Urine enters the ureter
-
What are the mechanisms involved in urine transport through the ureter? (3)
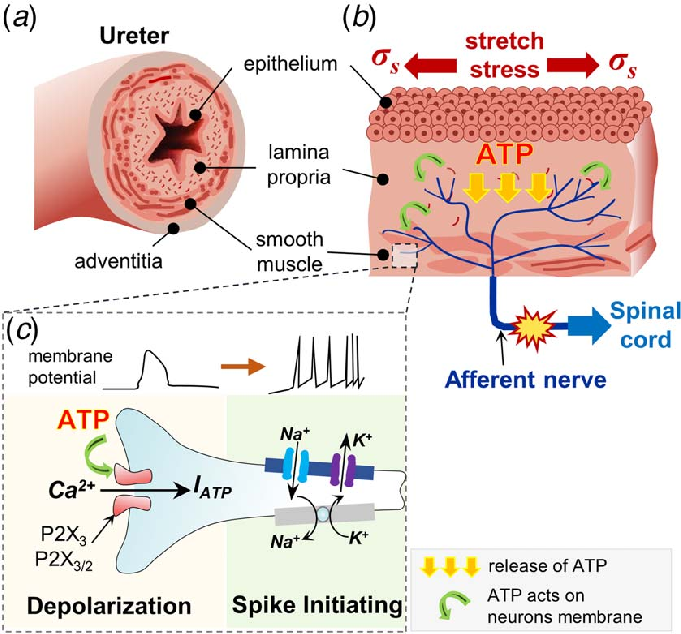
✶Peristaltic waves in ureter occur at a frequency of approximately 1-6 contractions per minute.
✶Ureters squeeze urine to a pressure of 10-20 mmHg.
✶Urine enters the ureter, distends it, and smooth muscles contract around it.
-
How do ureters connect to the bladder, and what controls ureteric peristalsis? (3)
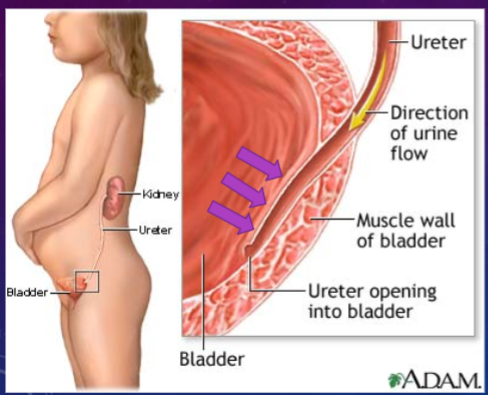
✶Ureters open obliquely (at a downwards angle) into the bladder, preventing reflux of urine back into the ureters by a passive flap-valve effect.
✶Ureteric peristalsis is myogenic in origin and NOT under CNS control.
✶Coordination is required between peristalsis and changing urine volume.
-
What is the capacity of the bladder, and how does its shape change with urine volume? (2)
✶The bladder can hold up to 400ml without much increase in pressure.
✶It takes on a spherical structure as it fills with urine.
-
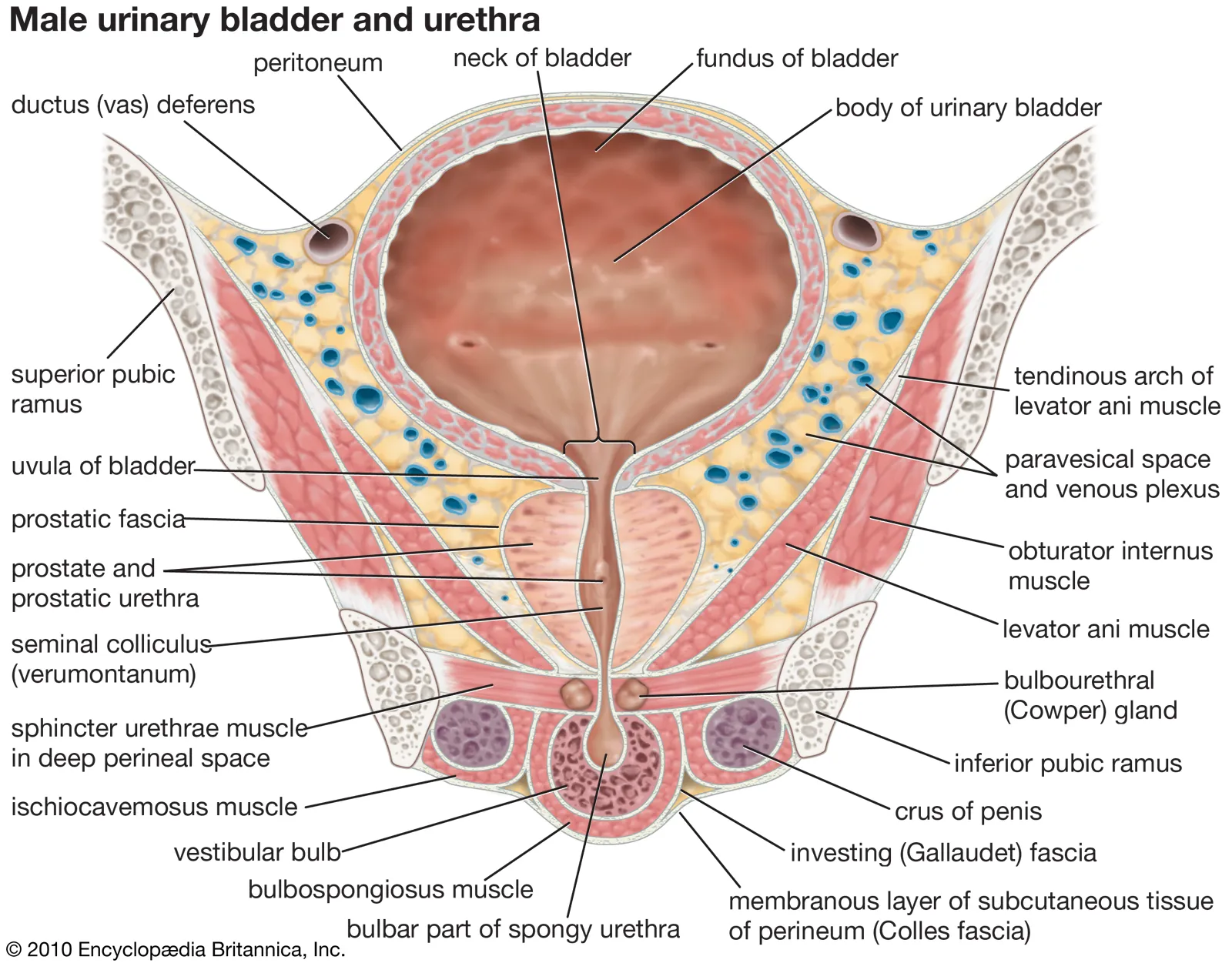
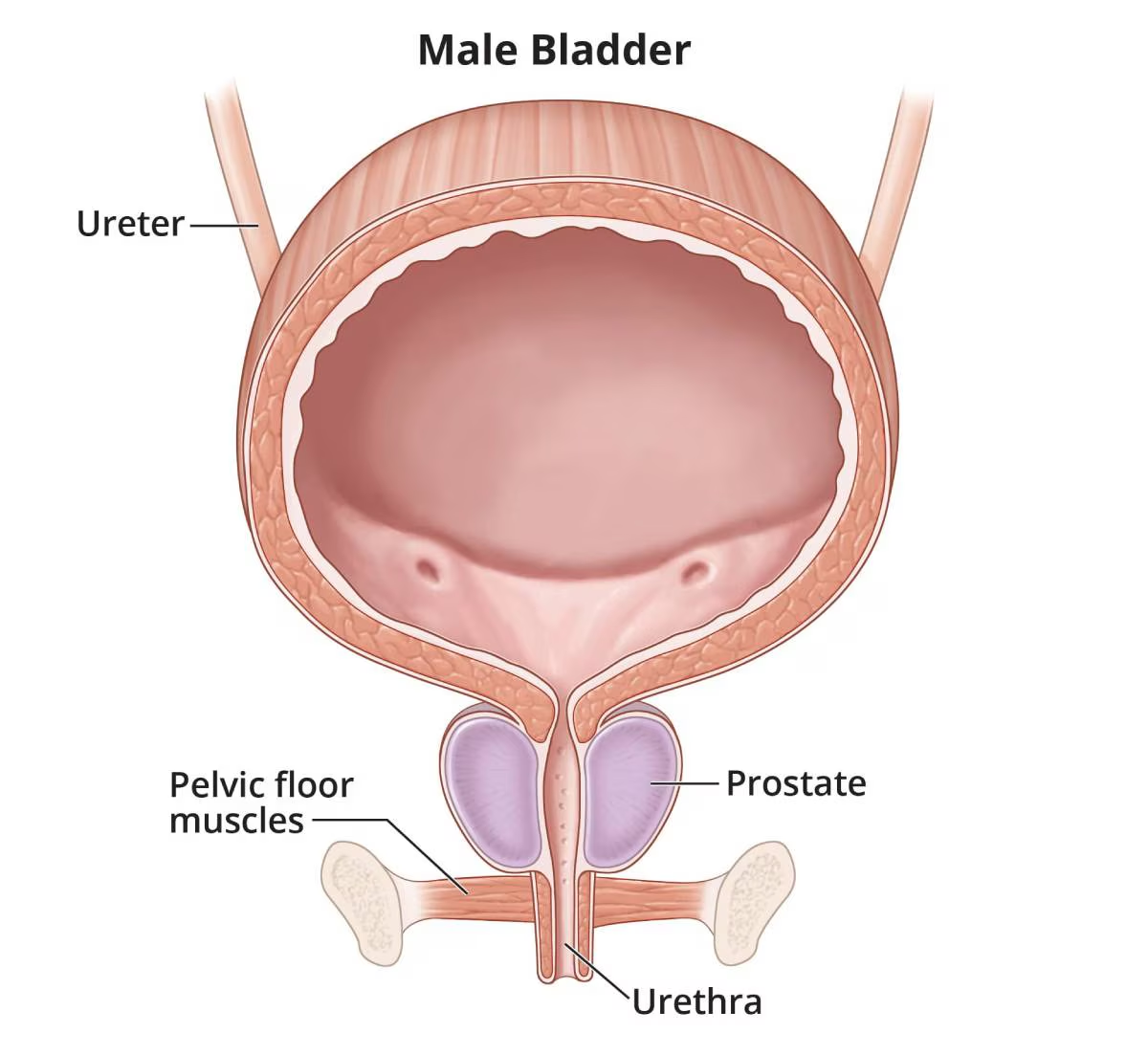
What are the two sphincters of the bladder, and are they under voluntary control? (2)
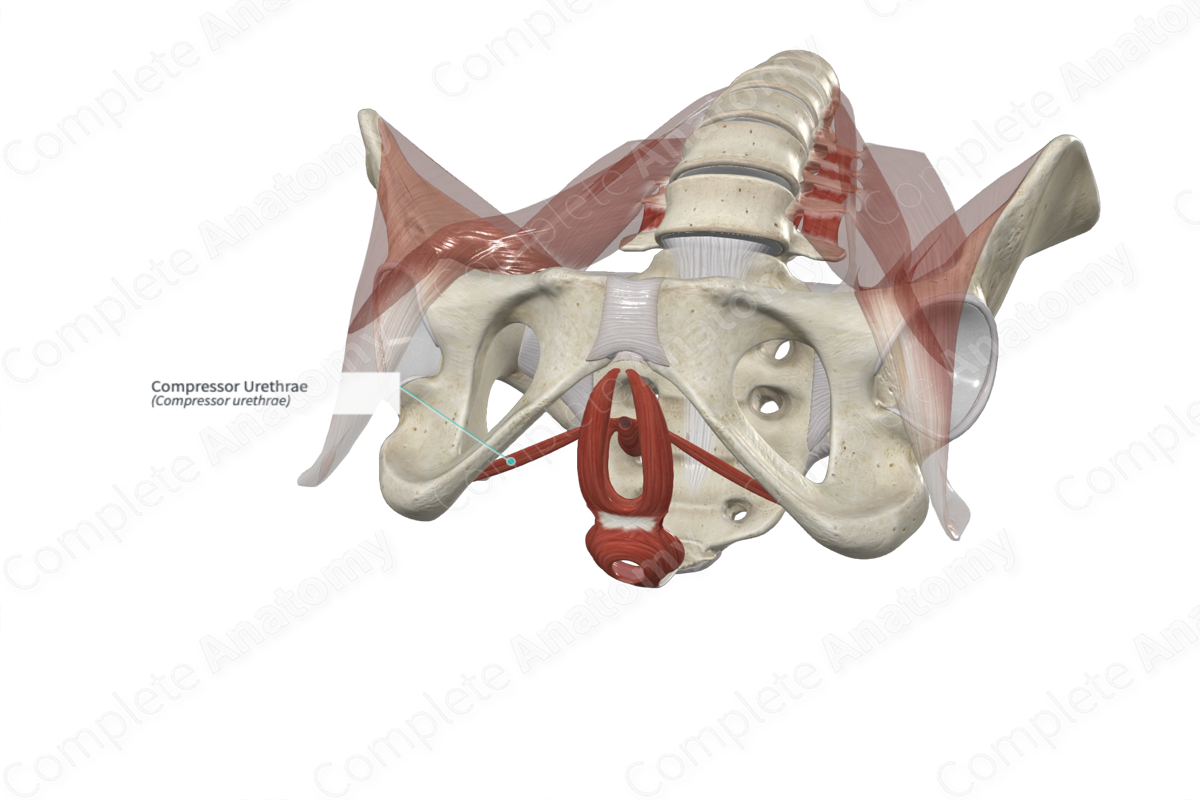
✶Internal Sphincter: An extension of the detrusor muscle, it is NOT under voluntary control.
✶External Sphincter: Composed of two striated muscles (compressor urethrae & bulbocavernosus) surrounding the urethra, these muscles are responsible for continence and ARE under conscious, voluntary control.
-
What are some characteristics of the female bladder and urethra? (3)
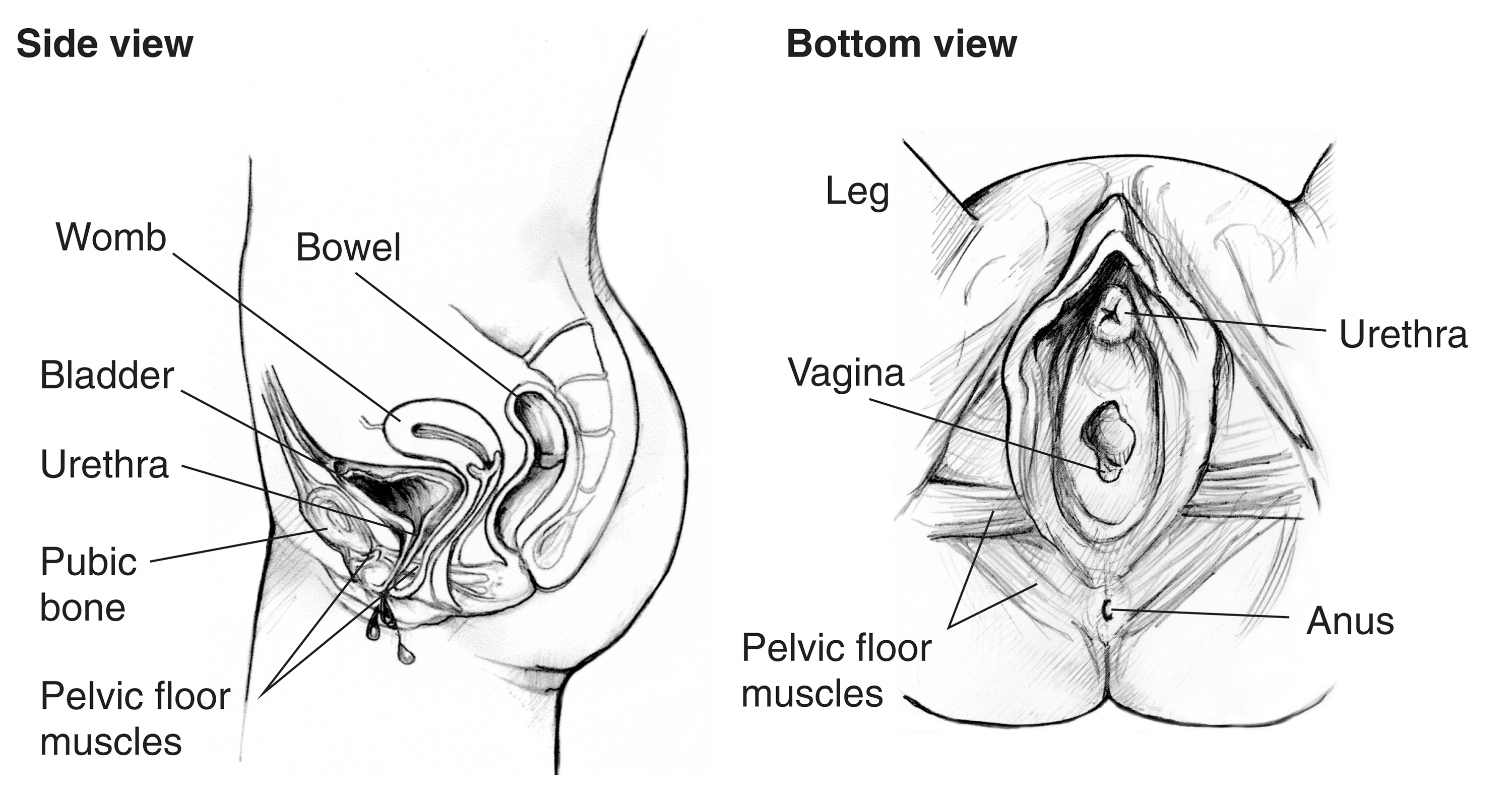
✶Short urethra: It only carries urine.
✶Poorly developed external sphincter....
✶This makes females more prone to incontinence, particularly after childbirth.
-
What are some characteristics of the male bladder and urethra? (2)
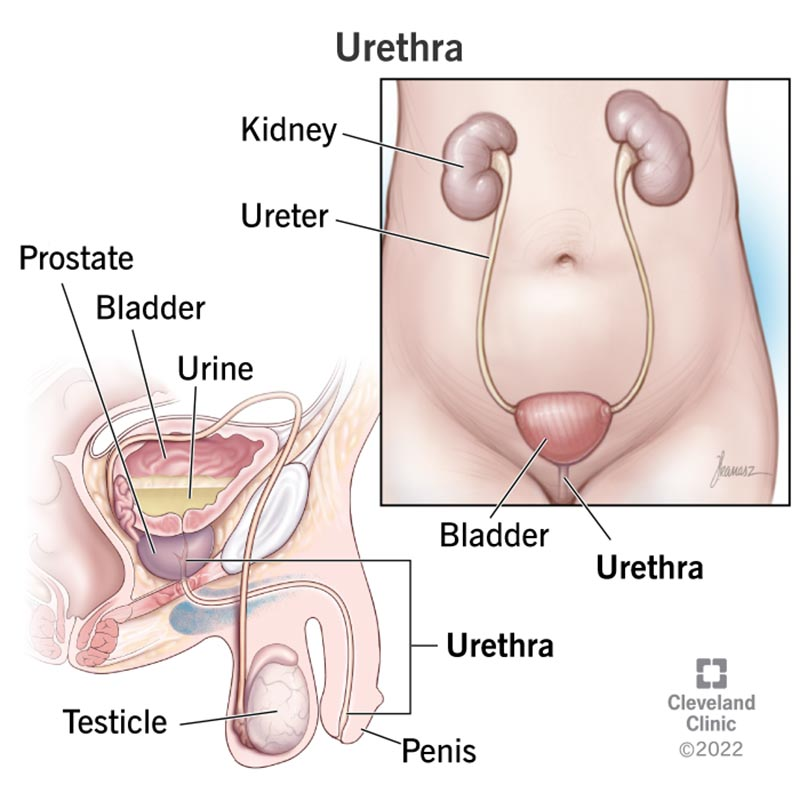
✶Carries urine and semen: Unlike the female urethra, the male urethra serves a dual function, allowing both urine and semen to pass through.
✶Urine elimination aided by contraction of bulbocavernosus muscles in penis: These muscles aid in the expulsion of urine from the male urethra.
-
What are some characteristics of the bladder and its outlet into the urethra? (5)
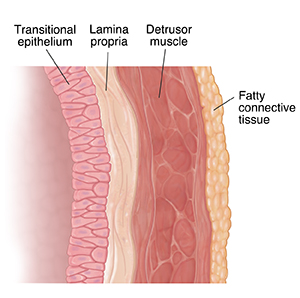
✶Bladder lining: Composed of transitional epithelium.
✶Bladder muscle: Consists of the detrusor muscle responsible for contraction during urination.
✶Impermeable to salt and water: Prevents the leakage of these substances into the bladder.
✶Permeable to lipophilic molecules: Allows certain lipid-soluble substances to pass through the bladder lining.
✶Outlet of bladder into urethra: Includes the internal sphincter, made of smooth muscle and under involuntary control, and the external sphincter, composed of striated muscle and under voluntary control.
-
What are some key points about kidney stones (renal calculi)? (5)

✶Most common disorder of the urinary tract.
✶Develop from crystals that precipitate from urine within the urinary tract.
✶Normal urine contains inhibitors like citrate to prevent their formation.
✶Calcium is present in nearly all stones, typically as calcium oxalate or, less commonly, as calcium phosphate.
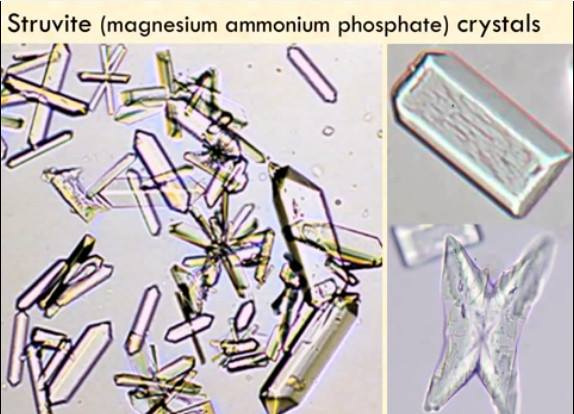
✶Other types include uric acid stones (<10%), struvite stones (<10%), and cysteine stones (<5%).
-
What are some additional points about kidney stones (renal calculi)? (6)

✶They are not the same as gallstones.
✶They are more common in men than in women, with a ratio of 2-3:1, possibly due to testosterone.
✶Causes include excess dietary intake of stone-forming substances, poor urine output or obstruction, altered urinary pH, low concentration of inhibitors, and infection.
✶Kidney stones can vary in composition, including calcium oxalate, calcium phosphate, uric acid, struvite, and cysteine.
✶Symptoms may include severe pain in the side and back, pain radiating to the lower abdomen and groin, painful urination, blood in the urine, and nausea and vomiting.
✶Treatment options include pain relief medications, drinking plenty of fluids, medication to relax the ureter muscles, and, in some cases, surgery to remove the stones.
-
What are some symptoms and implications of ureterolithiasis, also known as kidney stone disease? (4)
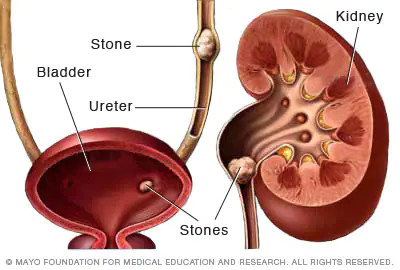
✶Kidney stones can form anywhere within the urinary tract, including the kidney, ureter, or bladder.
✶Symptoms may include dysuria (painful urination), hematuria (blood in the urine), loin pain or back pain, reduced urine flow, and urinary tract obstruction.
✶Urinary tract obstruction caused by kidney stones can lead to considerable pain, known as renal colic, with pressures reaching up to 50 mmHg.
✶As the stone approaches the tip of the urethra, intense pain can inhibit micturition, a condition known as strangury.
-

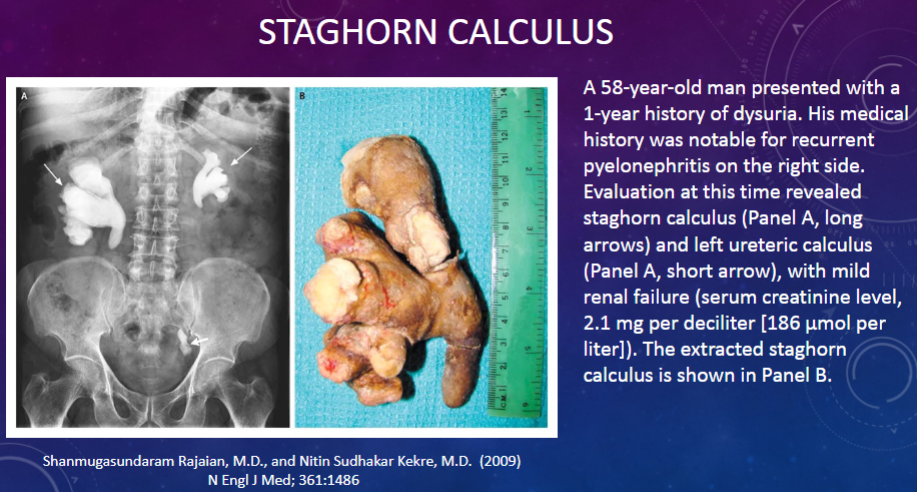
What is a staghorn calculus? (2)
✶A staghorn calculus, also known as a staghorn stone or coral calculus, is a large kidney stone that fills the renal pelvis and branches into multiple calyces of the kidney, resembling the antlers of a stag.
✶These stones are typically composed of struvite, which is a type of mineral that forms in alkaline urine and is commonly associated with urinary tract infections caused by certain bacteria, such as Proteus mirabilis.
-

Picture demonstrating a case involving a staghorn calculus:
-
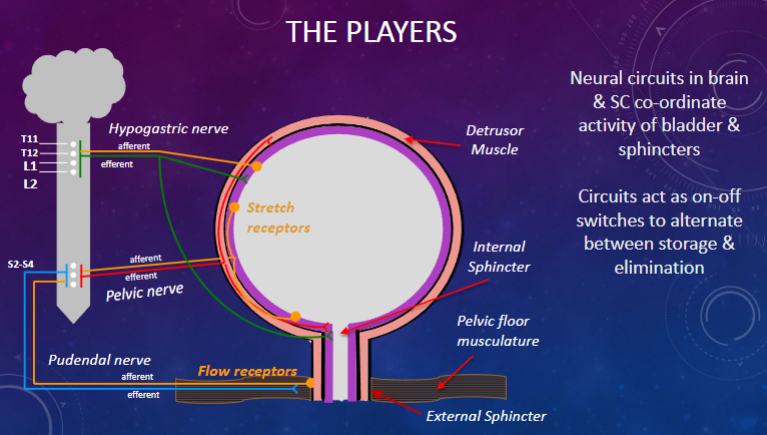
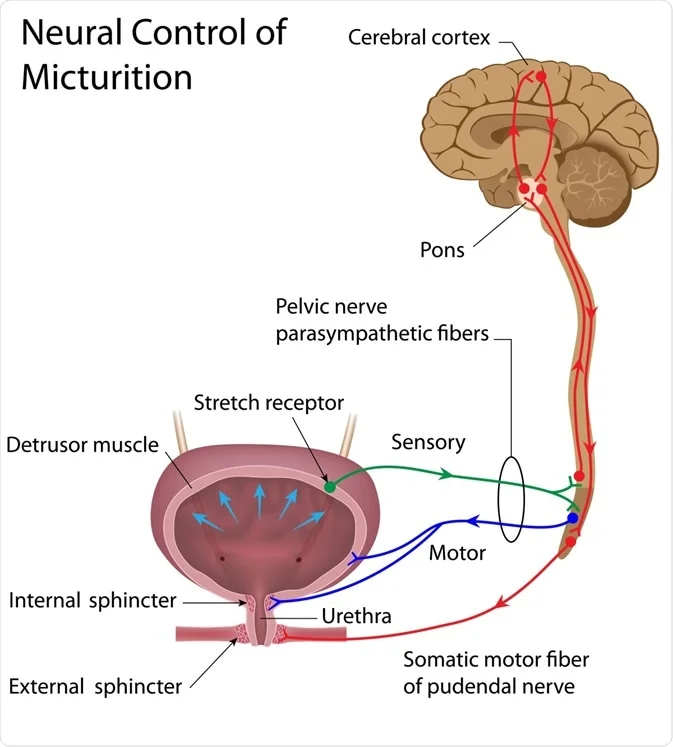
Picture demonstrating the players in micturition (bladder innervation):
-
What nerves are involved in bladder control? (3)
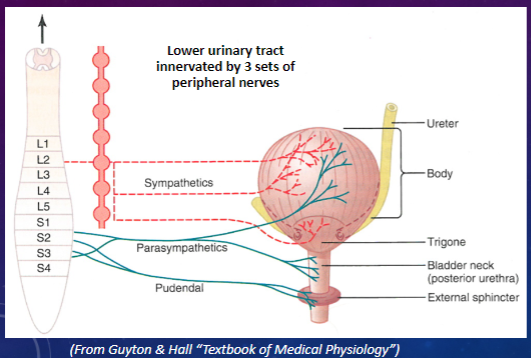
✶Sympathetic (hypogastric nerve)
✶Parasympathetic (pelvic nerve)
✶Somatic (pudendal nerve)
-
What is the difference between afferent and efferent nerves in bladder control? (2)
✶Sensory (afferent): Provides sensation (awareness) of fullness and pain from disease.
✶Motor (efferent): Causes contraction and relaxation of detrusor muscle and external sphincter to control micturition.
-
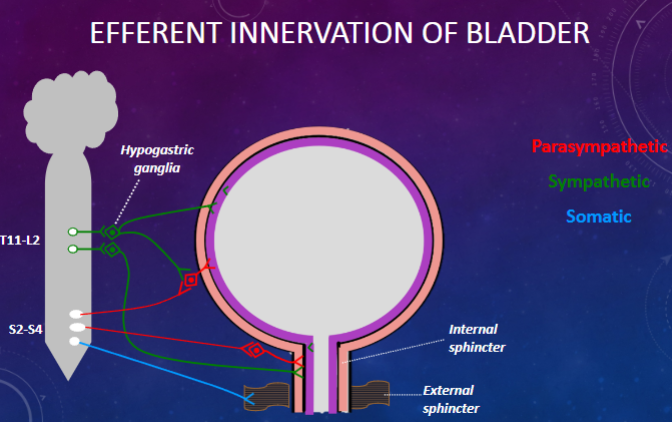
Picture demonstrating the efferent innervation of the bladder:
-
How does the efferent innervation affect the detrusor muscle? (3)
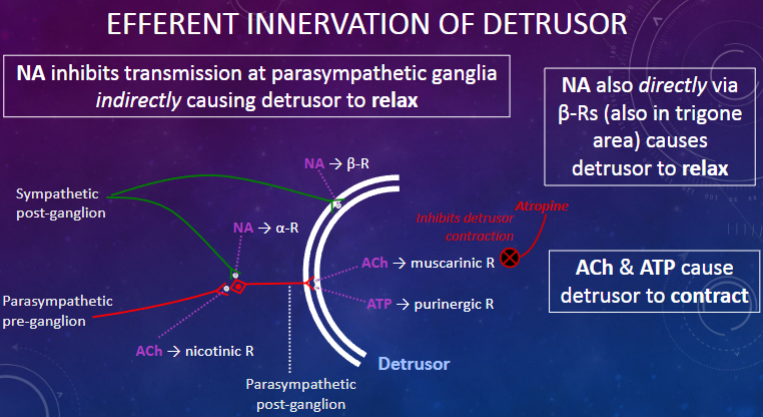
✶NA inhibits transmission at parasympathetic ganglia indirectly causing detrusor to relax.
✶NA also directly via β-Receptors (also in trigone area) causes detrusor to relax.
✶ACh & ATP cause detrusor to contract.
-
How is the innervation of the sphincters affected? (3)
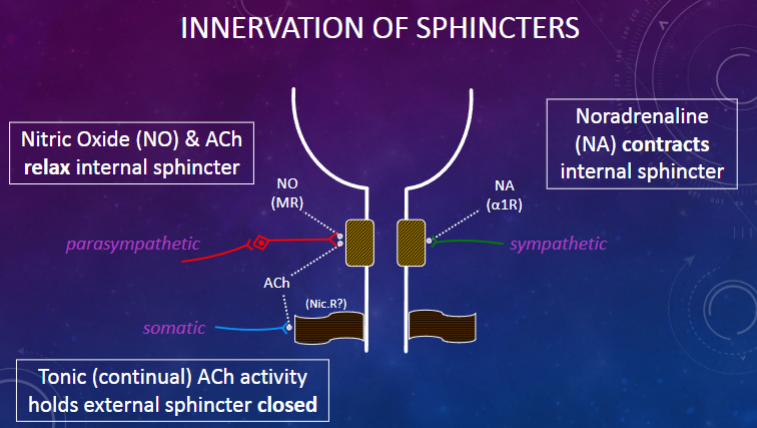
✶Nitric Oxide (NO) & ACh relax internal sphincter.
✶Noradrenaline (NA) contracts internal sphincter.
✶Tonic (continual) ACh activity holds external sphincter closed.
-
What are the effects of motor innervation on bladder function? (5)
Parasympathetic neurons:
✶Contract detrusor via ACh (muscarinic R) & ATP (purigenic R)
✶Relax internal sphincter via NO (cGMP) & ACh (nicotinic R?)
Sympathetic neurons:
✶Relax detrusor indirectly via NA (α-R) and directly via NA (β-R)
✶Contract internal sphincter via NA (α-R)
Somatic neurons:
✶Contract external sphincter via ACh (nicotinic R)
-
What are the types of afferent (sensory) nerve fibres involved in bladder function? (4)
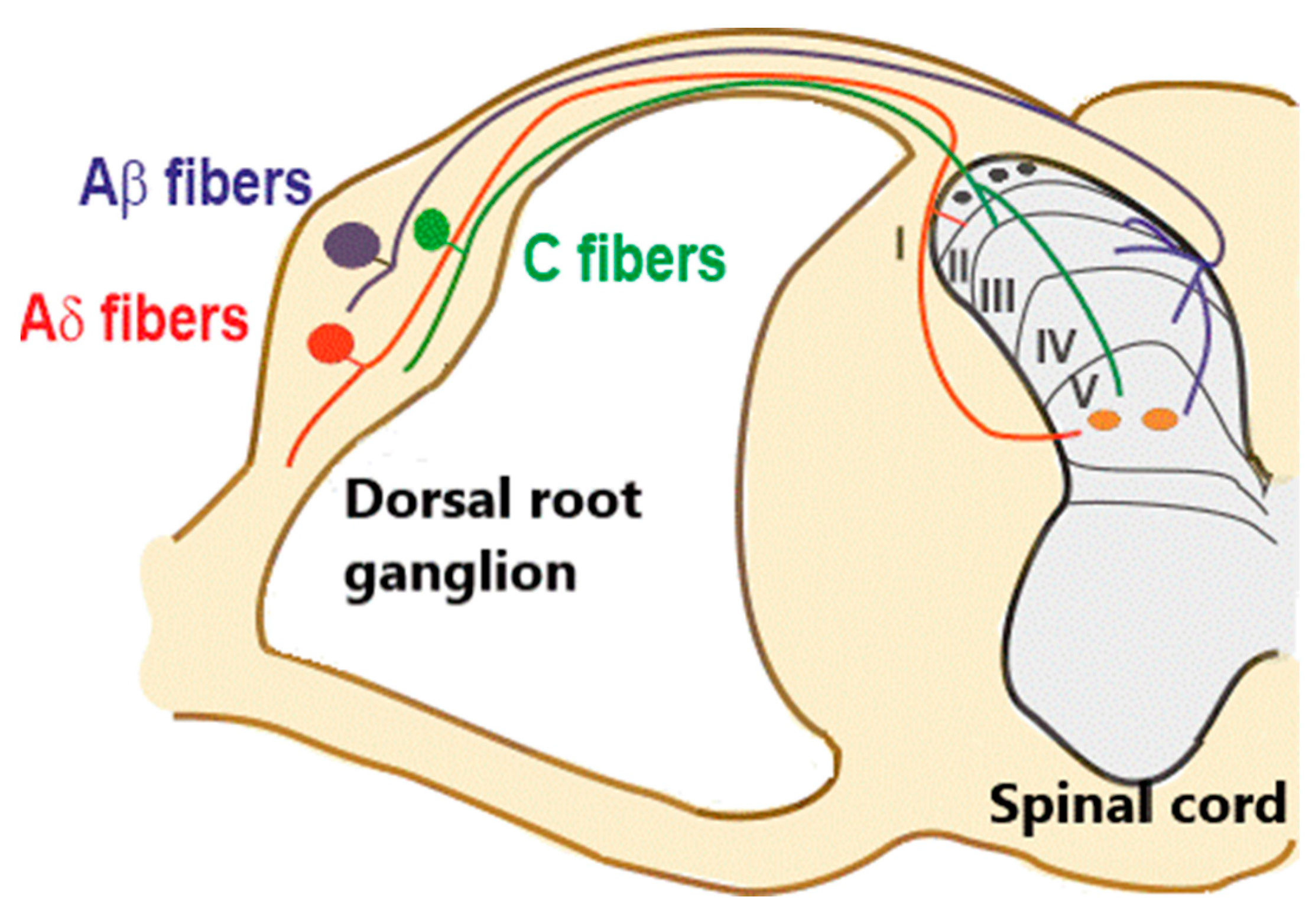
"A fibers": Sense tension in detrusor:
✶Filling of bladder
✶Detrusor contraction
✶Resulting in bladder fullness and discomfort
"C fibers":
✶Respond to damage and inflammatory mediators, resulting in pain and an urgent desire to micturate
-
What is involved in the afferent (sensory) innervation of the bladder? (8)
✶Main afferent pathway: Via pelvic nerve (parasympathetic)
✶Small myelinated Aδ-fibers: Involved in the micturition reflex
✶Stretch receptors: Signal wall tension
✶Volume receptors: Signal bladder filling
✶Unmyelinated C fibers: Endings in or near the epithelium
✶Nociceptors: Sensing pain (e.g., during cystitis or excessive distension)
✶Hypogastric (sympathetic) and pudendal (somatic) pathways
✶Flow receptors (external sphincter)
-
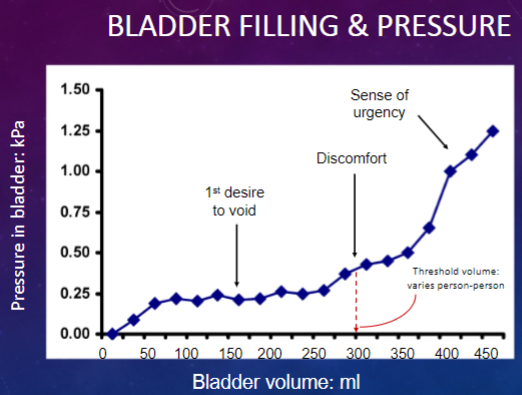
What happens during bladder filling? (7)
Initially: Bladder is empty
✶Sphincters closed
✶Tonic activity of sympathetic and somatic nerves
✶Bladder pressure is low
Arrival of urine:
✶Detrusor muscle relaxes progressively
✶Sympathetic activity inhibits parasympathetic transmission
✶Little increase in pressure
✶Sphincters still closed, leading to "receptive relaxation"
-
Picture demonstrating bladder filling and pressure:
-
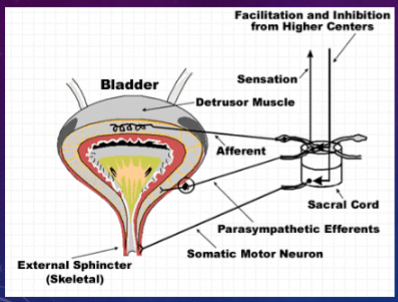
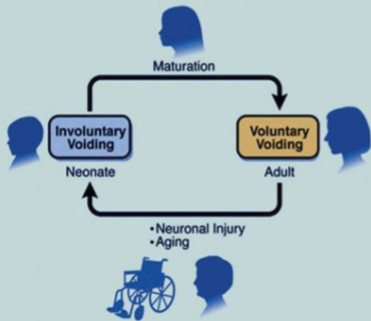
How does bladder emptying (micturition) occur? (6)
Micturition is an autonomic reflex:
✶Seen in babies (<18 months) and adults with spinal cord transected above sacral region
Reflex is modified by voluntary control:
✶Inhibited or initiated by higher centres in the brain
✶Bladder maturation complete by >6 years
✶Basic circuits act as on/off switches to alternate between two modes of operation: storage and elimination
Disease, injury, or ageing to the nervous system in adults disrupts voluntary control of micturition:
✶Leading to bladder hyperactivity and urge incontinence
✶Stress incontinence
-
Picture demonstrating micturation and age:
-
What is the micturition (emptying) reflex? (4)
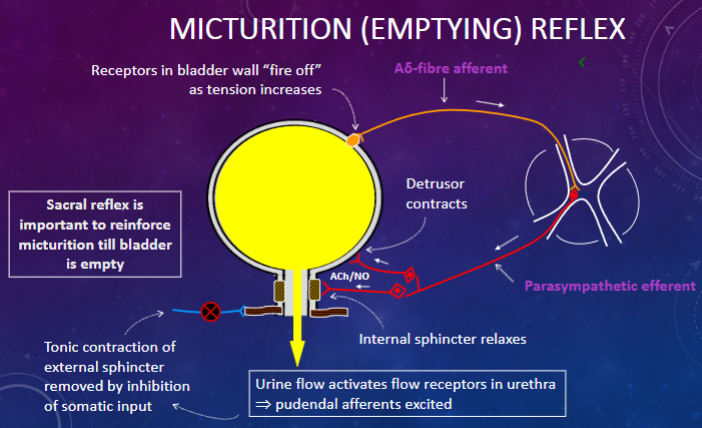
✶Receptors in bladder wall "fire off" as tension increases.
✶Sacral reflex is important to reinforce micturition until bladder is empty.
✶Urine flow activates flow receptors in urethra, leading to pudendal afferents being excited.
✶Tonic contraction of external sphincter is removed by inhibition of somatic input.
-
How is the micturition reflex modified by higher centres? (2)
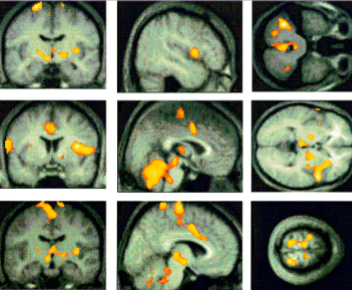
✶The activation pattern during micturition is superimposed on averaged MRI scans.
✶A widespread involvement of cortical and subcortical areas including the specific pontine micturition centre (PMC) is observed.
-
How can the micturition reflex be voluntarily modified? (2)
✶Higher centres can modify the micturition reflex for a while by consciously contracting the external sphincter and levator muscle.
✶This modification also involves increasing sympathetic firing to the bladder and internal sphincter, which interferes with positive feedback to bladder emptying by inhibiting parasympathetic transmission and tightening the internal sphincter.
-
Other methods of voluntary modification include what? (3)
✶Halted urine stream by "strangury" (urethral pain) due to urethritis from STI or renal calculi.
✶Inhibition of micturition by pinching the glans penis.
✶At night, the pontine micturition center (PMC) and arousal center wake you up if the bladder fills to capacity to prevent involuntary emptying.
-
What are the components involved in the normal control of micturition? (10)
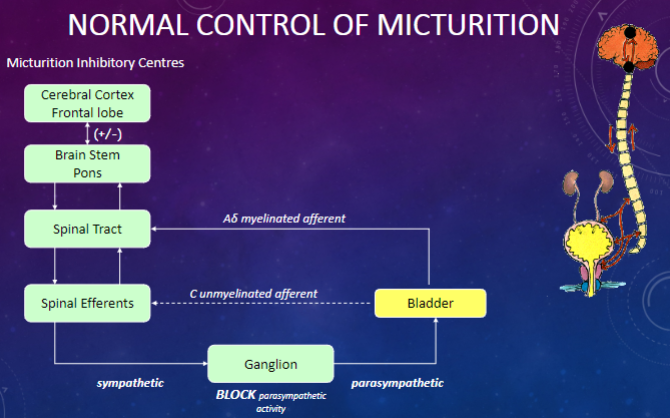
✶Cerebral Cortex (Frontal lobe)
✶Brain Stem (Pons)
✶Spinal Tract
✶Spinal Efferents
✶Ganglion
✶Bladder
✶Aδ myelinated afferent
✶C unmyelinated afferent
✶(+/-) sympathetic and parasympathetic pathways
✶Micturition Inhibitory Centres
-
How does voluntary control of micturition work? (3)
✶The bladder is contained in the floor of the abdominal cavity.
✶By contracting abdominal muscles, the increased intra-abdominal pressure is transmitted to the bladder and urethra.
✶Reflex contraction of peri-urethral striated muscles also helps compress the urethra, aiding the micturition reflex.
-
Why is bladder emptying important? (4)
✶Urine is normally sterile but occasional bacterial entry can occur.
✶Complete emptying of the bladder restores sterility by removing bacteria.
✶Bacteria in retained urine can seed fresh urine, leading to clinical infection such as urinary tract infection (UTI).
✶Repeated infections can destroy renal function if they ascend to the kidney.
-
What are the different types of urinary tract infections (UTIs) based on the area of infection? (4)
✶Bladder: Infection in the bladder is called cystitis or a bladder infection.
✶Kidneys: Infection of one or both kidneys is called pyelonephritis.
✶Ureters: Rarely the site of infection.
✶Urethra: Infection of the urethra is called urethritis.
-
What are some risk factors for urinary tract infections (UTIs)? (10)
✶More common in women due to a shorter urethra.
✶Common in men over 40 due to prostatic disease, causing bladder outflow obstruction.
✶Diabetes mellitus.
✶Long-term catheterization.
✶Pregnancy.
✶Enlarged prostate.
✶Prolonged immobility.
✶Kidney stones.
✶Bowel incontinence.
✶Advanced age.
-
What are some problems associated with the aging bladder? (2)
✶Slow urine stream: Often caused by prostate enlargement, known as benign prostatic hyperplasia (BPH), which is the most common cause of lower urinary tract symptoms in men over 40 years old (25% of men in this age group).
✶Slow urine stream can lead to incomplete emptying of the bladder, which increases the risk of urinary tract infections.
-
What are some causes of incontinence? (2)
Causes:
✶Weakening of sphincters, such as in stress incontinence, which is common in women after childbirth due to weakened pelvic floor muscles.
✶Failure of nervous control, leading to conditions like overactive bladder (OAB), where the detrusor muscle contracts spastically, resulting in sustained high bladder pressure and urge incontinence.
-
What are some consequences of incontinence? (3)
Consequences:
✶Social embarrassment: Incontinence can be socially embarrassing, leading to discomfort in public situations.
✶Diminished self-esteem: Constant worry about incontinence can impact self-esteem and confidence.
✶Reduced quality of life: Incontinence can significantly diminish the quality of life, affecting daily activities and overall well-being.
-
What are two treatment options for incontinence? (2)
✶Anti-muscarinics: These medications relax smooth muscle and decrease detrusor contraction. An example is oxybutynin, a non-specific muscarinic receptor antagonist, although it can have wide-ranging side effects.
✶Bladder retraining: This approach is used for stress and urge incontinence and involves creating a timetable for voiding and performing Kegel exercises to strengthen pelvic floor muscles.
-
What is the Kegel exercise? (4)
KEGEL exercises:
• Clench the muscles you would use to stop the flow of urine.
• Hold the squeeze for 10 seconds, then relax.
• Do three or four sets every day.
• As these muscles grow stronger, so will your bladder control.
-
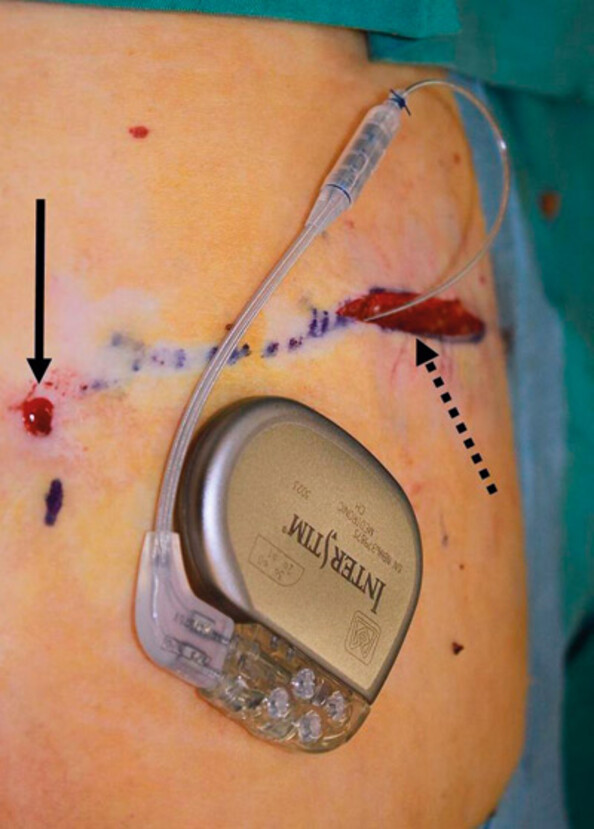
What are two additional treatments for incontinence? (2)
✶Surgery:
Bladder neck suspension
Botulinum toxin or collagen injections into muscles around the urethra to relax the bladder (used for overactive bladder)
✶Sacral Nerve Stimulation (SNS):
Involves an implanted neurostimulation system that delivers electrical impulses to the sacral nerve.
-
What are two emerging treatments for incontinence? (2)

✶Stem cell therapy:
Frauscher et al (2004) cultured stem cells into the bladder wall, resulting in 90% experiencing no leakage. However, this is limited by the supply of stem cells, mainly from bone marrow.
✶Tissue-engineered bladder:
Involves the use of synthetic and natural scaffolds to form a three-dimensional structure using human tissue. Currently, this method is in phase II trials.
-
State a list of the possible treatments of incontinence (6)
-Anti-muscarinics
-Bladder retraining/Kegel exercises
-Surgery
-Sacral nerve stimulation
-Stem cell therapy (emerging)
-Tissue-engineered bladder (emerging)
-
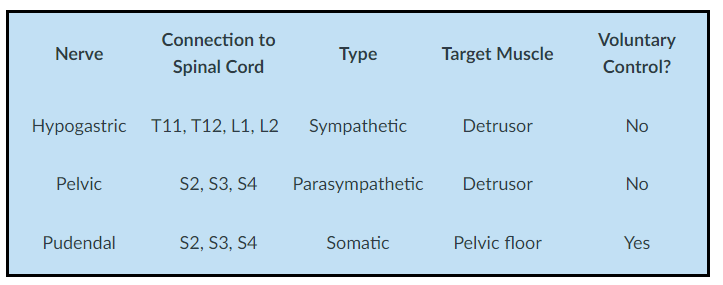
There are three types of bladder innervation, state the nerves, their connection to Spinal Cord, Type, Target Muscle and whether it's under Voluntary Control?