-
Kidneys, Electrolytes and Fluid Balance
1. Kidneys take out from blood what is not needed and put back what is in needed.
2. Loop of Henly reinfuses electrolytes.
3. Osmolality, how concentrated urine is particles per water.
4. Kidney controls BP through excretion.
-
Urine Assessments
1. Changes in voiding habits
2. Urinary retention
3. Cloudy/discolored urine
4. Foul-smelling urine
5. Blood tinged
6. Lower back pain
7. Pain with urination
8. Fluid and electrolyte balances.
-
Urinary Function Tests and Labs
1. Renal function tests - US, MRI, cystography, angiography, endoscopy
2. Urinalysis / Culture and sensitivity
3. Creatine - Muscle metabolism, for men 0.74 to 1.35
4. GFR - filtration function 60 or up
5. Blood urea nitrogen (BUN) - Kidney function: 6-24 mg/dL (problem if too low)
6. Specific Gravity- Urine dilution: 1.005 - 1.030
7. Albumen - Kidney damage: below 30 g/dL
8. WBC: 2-5
9. RBC: 2-4
-
Reading Urine Color
1. Clear: overhydration, diuretics, or diabetes insipidus
2. Straw yellow: normal color result of urobilin
3. Orange: dehydration or infection
4. Brown: increased bilirubin, blood break down or liver disease
5. Red: blood from infection, stone or tumor, menstruation. Dyed by drugs such as Rifampicin or Rhubarb.
6. Blue/green: contrast medium after scan
7. Cola: rhabdo, muscle break down, major trauma or muscle injury
-
UTI Risk factors
1. Catherization
2. Female
3. Hygiene issues
4. Sex
5. Immunosuppression
6. Post menopausal,
7. E. Coli
-
UTI Clinical Manifestations and Prevention
1. confusion
2. fever
3. pain w/ urination
4. urgency/frequency issues
Protection by: hydration and safe sex.
5. Dx by: dipstick for leukocyte esterase and nitrates, UA and C+S
-
Cystitis (Lower UTI)
1. Lower tract infection
2. Bacterial is common
3. Reflux to kidneys
4. Issues with urinary urgency, frequency, pain with urination
5. NC: output, pain management, cognitive assessment, fall risk, teach cleanliness
-
Pyelonephritis (Upper UTI)
1. Bacterial is common, use antibiotics (levoflaxcin, sulfonamides).
2. s/s: fevers, chills, low flank pain, pain on urination
3. NC: output, pain management, cognitive assessment, fall risk
-
Renal Calculi
1. Risk factors: hydration, diet high in salt or calcium or vit D.
2. Clinical p: pain, blood in urine
3. Prevention: hydration
Renal calculi can be formed in kidneys or bladder. ureters are usually the issue. most organs don't have pain receptors for injury but do for stretching.
-
Urolithiasis (kidney stones)
1. Stones mostly made of Ca
2. Risk factors: previous stones, urinary status, gout, male, lifestyle, diet, excess body weight.
3. Clinical p: pain, lower flank pain, waves of pain, burning with urination, frequency issues, discolored urine, fevers, chills.
4. Stag horn kidney stones require surgical intervention.
-
Extracorporeal Shock Wave Lithotripsy (ESWL)
ESWL is a noninvasive procedure that breaks down stones in parts of the urinary system, in the pancreas and in the bile ducts. It uses shock waves that are aimed at stones, with the help of X-rays or ultrasound. Stones in the kidneys and ureter often pass on their own after EWSL.
-
Renal Calculi Nursing Considerations
1. Pain
2. Monitor urine amount and character
3. Increase fluids
4. Strain all urine
Tx: ultrasound shockwave or surgery
-
Acute Kidney Injury (AKI)
1. RF: utis, trauma
2. CM: increased creatine ≥0.3 mg/dL within 48 hrs, or increased serum creatine x1.5 times the baseline in past 7 days, or a urine volume of less than 0.5mL/kg/hr for 6 hours
-
Causes of AKI
1. Decreased blood flow
2. Direct damage to kidneys
3. Blockage of urinary tract
-
AKI treatments
1. Prerenal: correct hemodynamic derangements, fluids or diuretics
2. Intrarenal: treat the underlying disease
3. Postrenal: relieve obstruction, through foley, nephrostomy tube, antibiotics
-
Four Phases of AKI
1. Onset (hours to days): renal blood flow 25% of normal, urine output < 0.5mL/kg/hour
2. Oliguric/anuric (8-14 days): output < 400mL in a day, increase in BUN and creatine. Electrolyte disturbances, fluid overload since kidneys can't excrete water
3. Diuretic phase (7 to 14 days): Occurs when AKI cause is corrected, increased GFR, daily urine output > 400 mL, Possible electrolyte depletion from excretion of more water and osmotic effects of high BUN.
4. Recovery phase (months to 1 year): decreased edema, normal fluid/electrolyte balance, return of GFR to 70-80% of normal
-
AKI Nursing Considerations
1. Prevent further injury
2. Treat underlying cause
3. Correct fluid/electrolyte imbalance (diuretics, treat hyperkalemia)
4. Avoid nephrotxic drugs, NSAIDs, contrast dyes
5. Good assessment (resp, cardiac, skin)
6. Nutrition (sodium and calorie restriction)
7. Monitor I/O and VS
-
Prerenal, Intrarenal, and Postrenal concerns practice
Prerenal: decreased cardiac output, hypovolemia,
Intrarenal: calculi, nephrotoxic drugs, acute glomerulonephritis
Postrenal: , calculi, prostate cancer
-
Chronic Renal Failure
1. RF: HTN, DM, NSAIDs, genetics, previous kidney injuries, age
2. CM: electrolyte/fluid imbalance, anemia, acidosis
3. Prevention: life choices, prevent utis
4. Stages: 1=normal 2= mild 3= moderate 4= severe 5= failure
-
Dialysis
1. Preserve kidney function for as long as possible with medications.
2. Peritoneal dialysis: abdominal catheter, slow movement of waste (homeostasis), peritoneal membrane is semipermeable, 3-5 times a day.
3. Hemodialysis: implanted shunt, outpatient procedure, 3 times a week for 3-4 hours.
-
Renal Failure Nursing Considerations
1. Daily weights
2. Monitor electrolytes and renal labs
3. Dietary restrictions: Reduced sodium, potassium, and phosphorus (SPPP), reduced protein, fruits and veggies.
4. nutritional support
5. Monitor for infection
6. Encourage activity
7. Psychosocial support
-
Breast disorders
1. Mastitis: infection/inflammation of breast tissue
2. Cysts: fluid formed can be drained, 5-10mL
3. Pain
4. Cancer: very common in breasts
-
Breast Cancer Risk Factors
1. Advanced age
2. Alcohol
3. Female
4. Nulliparity (no pregnancies)
5. Ashkenazi Jewish heritage
6. Late menopause
7. Recent HRT
8. Genetics
(not malnutrition)
-
Breast Assessment
1. Lumps
2. Skin dimpling
3. Change in skin color or texture
4. Change in how nipple looks, like pulling of nipple
5. Clear or bloody fluid leaks from nipple
-
Breast Diagnostics Tools
1. Mammography
2. Biopsy
3. Ultrasound
something show up on US but not on mammo. Biopsy takes core sample of tissue, huge risk for hematoma afterwards, pressure for first 24 hrs is helpful.
-
Modified Radical Mastecotomy
1. Once cancer is in lymph nodes it can spread anywhere. Prostate cancer matasizies to the bone.
2. Staging of cancer helps determine level of treatment.
3. Large incision with lots of drainage to remove breast tissue. JP drains to remove fluid
4. Teach JP drains, when to empty (starts to loose suction), concerning colors (green/yellow), clip to shirt, showering, outline infections and date it
5. Elevate arm after mastectomy
-
Post Mastectomy Care
1. Elevate affected side w/ distal joint higher than proximal joint.
2. No BP, injections on affected side.
3. Psychological concerns
4. Maintain pressure dressings
5. Watch for edema and infection
6. Arm exercise within 24 hrs after surgery.
-
Mastectomy Discharge Teaching
1. Pt goes home within 24 hrs usually
2. Silicon implants have risks
3. Lymphedema, lymph doesn't have pump, needs movement to move blood.
4. Arm exercises
5. Pain management.
-
Menstural Disorders
1. Purpose of mensuration: slough off lining of uterus when not pregnant.
2. Premenstrual syndrome: body reacts to ebb and flow of different hormones being released. mood swings/discomfort
3. Dysmenorrhea: lower abd pain, just before or during menstruation.
4. Amenorrhea: absence of menstruation
-
Contraception / Abortion
1. Types of contraception: hormonal, barrier, rhytm/withdrawl
2. Abortion: spontaneous (before 20th week), emergency, induced
-
Infertility Pregnancy complications
1. Female Factors: egg levels
2. Male Factors: lack of mature sperm
3. Pregnancy complications: ectopic pregnancies, fertilized egg but implants in fallopian tube, is an emergency, gets bigger until it ruptures.
-
Infectious disorders / Structural Disorders women reproductive
1. Bacterial vaginosis: can be fungal as well
2. STI
3. fistula is a connecting hole
4. Loose ligaments
5. uterine prolapse, not threating but surgery can be done to correct.
-
Malignant disorders of menopause
1. Older women rf
2. Cessation of mensturation
cancer can affect any internal strucutres
-
Benign Prostatic Hyperplasia (BPH)
1. RF: over 50 yrs old
2. S/s: frequency, nocturia, hesitation, difficulty starting stream
3. Dx tests: Rectal digital test, transdermal ultrasound, checking PSA levels (PSA will be high with BPH)
4. Complications: flank pain, decreased urine output.
-
BPH Meds
1. Alpha adrenergic agonists: relax the smooth muscle, ex: tamsulosin (flomax), terazosin (hyrtrin), doxazosin (cardura).
2. Alpha reductase inhibitors: inhibit enzyme responsible for formation of androgen, ex: finasteride (proscar), dutasteride (avodart)
-
Transurethral Resection of the Prostate (TURP)
x. Go in through the penis urethra, not surgical
1. CBI
2. Close observation of drainage system, maintain catheter patency
3. Bladder spasms
4. Pain control w/ analgesics limit activity first 24 hours
5. Avoid straining with BMs, high fiber and laxatives
6. Complications: hemorrhage go to light pink urine in 24 hrs, urinary incontinence, infections, DVTs
7. do not elevate pelvis
8. There should be NO PSA after removal of prostate, if there is that means cancer.
-
Continuous Bladder Irrigation (CBI)
1. Threeway catheter: Irrigation, Balloon, Drainage
2. Use sterile irrigation solution
3. Blood clots are expected
4. Ideal color is light pink, no clots
5. remove 2-4 days post op
6. Do not elevate pelvis
-
Other Male Reproductive disorders
1. Erectile dysfunction: physical or hormonal dysfunction.
2. Cancer: can affect any of the structures, penile, testicular, prostate, fast growing easy to detect easy cure.
3. Infection: prostatitis, infection of prostate, ependymitis=infection of testicles.
-
Chlamydia and Gonorrhea
1. Chlamydia - most common STI, gonorrhea 2nd most common
2. Both are bacterial infections
3. Antibiotics to cure
4. S/s: vaginal/penile discharge, bleeding, pain, fever chills n/v, pelvic inflammatory disease (PID). can cause sterility in women, can prevent sperm getting through in men.
5. RF: poor hygiene, multiple sex partners, unprotected sex, history of STIs. Discontinue IUD.
-
Herpes
1. Oral or genital
2. Viral infection treated with antivirals. Not a cure.
3. S/s: dormant vs outbreaks, itching, pain, ulcerations contagious.
4. Stages: prodroma, vesicular (blister) ulceration (lesion rupture)
5. Medical management: cannot be cured, anti virals to control symptoms and discomfort, keep lesions clean.
6. Prevention: avoid contact
7. Pregnancy risk: can be passed on birth, antibiotic eye drops soon as born.
-
Syphilis
1. Was considered fatal, unethical study with tuskgee airmen
2. Bacterial, can be treated with antibiotics at chance for cure if caught early.
3. Stages:
primary = chancre,
secondary = rash,
latent = asysptomatic
tertiary = multisystem, brain heart bones
4. Antibiotics and curable for most
5. Prevention: avoid skin contact, sexual contact, keep clean.
-
Human Papillomavirus
1. Most common virus in US = HPV
2. basically warts not curable because viral, causes CANCER
3. s/s: genital warts, painful, emotional distress
4. mm: treat warts if present with ablation with cyrotherapy, can go away on its own
5. Prevention: avoid skin contact, sexual contact, vaccine series available
-
HIV (human immune deficiency virus)
1. Virus attacks CD4 immune cells
2. Stages:
stage1 = flu symptoms then asymptomatic
stage2 = opportunistic infections
stage3 = AIDs
3. mm: not curable, antiviral therapy life long multiple drugs, pill fatigue
4. prevention: avoid sexual contact until virally suppressed, not contagious with viral suppression.
-
Adrenal Function
1. Adrenal glands regulate many hormones.
2. Cortisol regulates: stress response, metabolism, fluid balance
-
Addison's Disease (Adrenocortical Insufficiency)
1. Not enough cortisol
2. Often caused by autoimmune or feedback loop issues
3. Increased excretion of sodium, chloride, and water
4. Dx: physical assessment (often start nonspecific), labs for cortisol levels, CT can give insight
5. S/s: weight loss, darken skin, BP lower, fainting, salt cravings, muscle cramping, joint pain, hypoglycemia, n/v
-
Corticosteroid Therapy
1. Used to: suppress inflammation, allergic reactions, reduce swelling control autoimmune disorders, Addison's Disease
2. Common drugs: Hydrocortisone, Prednisone
3. Allows for better stress responses
4. Needs to be tapered off
-
Cushing Syndrome
1. Too much cortisol
2. Causes: long term use of corticosteroids, adrenal tumors (comes with prolonged use)
3. S/s: high glucose, poor wound healing, weight gain, easy bruising, cardiac hypertrophy, osteoporosis, weakness
4. NI: skin assessment for bruise/tears, wound healing. Monitor pulse, orthostatic BP, BGL, energy levels, weight
-
Addison's / Cushing syndrome teaching
1. Mood changes mental health
2. impact of long term corticosteroid use
3. treatment is life long
4. health maintenance; diet and exercise
5. Watch fluid balance, daily weights, sodium and water balance.
-
Diabetes Risk Factors
1. Obesity
2. Family history
3. Age
4. Ethnicity
5. Gestational diabetes
-
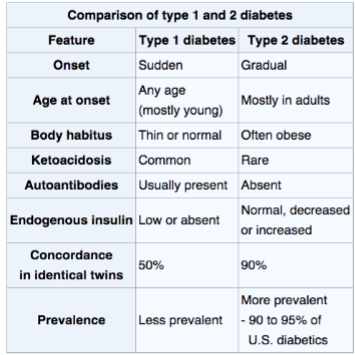
Type 1 vs. Type 2 Diabets
-
Diabetes Diagnostics
1. Fasting blood glucose levels, >126 is diabetes
2. Symptoms of hyperglycemia (thirst, hunger, peeing alot, tired)
3. Oral Glucose Tolerance test (OGTT) - screens for type 2, measures sugar tolerance
4. HgbA1C - couple month average of sugars
-
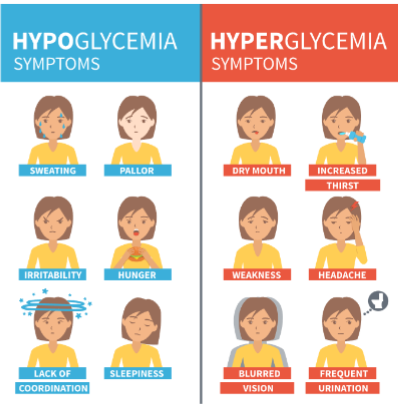
Hypoglycemia vs. Hyperglycemia
-
Hypoglycemia Treatment
1. Give apple or orange juice, 15 carbs with no fat or protein if able to swallow.
2. If not able to swallow, IV D50 or glucagon (IM).
3. Recheck sugars in 15 minutes
4. Repeat until at normal levels
5. At normal BGL, give long acting carb and protein.
-
Type II Diabetes
1. Insulin resistance
2. Usually older than 30
3. Reduced Insulin production
4. Slow progression
5. Vascular damage
6. Can be preventable
7. manage: exercise, monitoring, education, diet, pharmacologic therapy.
-
Diabetes Labs to Watch
1. Blood Labs: Potassium, Ketones, Glucose, Renal function, Lipids
2. Urine: albumin, ketones, glucose
-
Common Diabetes Medications
1. Glyburide: take at breakfast, watch for hypoglycemia, GI upset
2. Metformin: take twice a day with meals, watch for hypoglycemia, GI upset, avoid imaging contrast dyes
3. Glucagon: for seriously low BG levels.
-
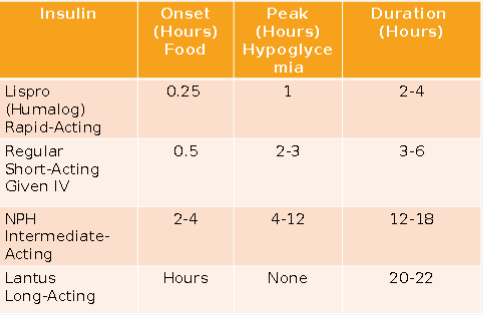
Insulins
-
Mixing insulin
1. Draw up Clear (regular) before Cloudy (Long acting/ NPH)
-
Insulin delivery
1. Rotate sites
2. Give before meals if possible
3. Teach how to give injections
4. Carb counting orders: 1 unit of insulin per 15-grams of carbohydrate.
-
Sick days in Type 1+2 Diabetes
1. Emotional and physical stress can result in hyperglycemia.
2. Maintain diet/fluid intake
3. Do NOT withhold medications
4. Supplement intake with carbohydrate containing fluids.
5. Check BGL every 4 hours
6. Check urine for ketones if BGL > 240 mg/dL
-
Diabetes and Exercise
1. Improves insulin sensitivity
2. Best to do after meals but not when insulin peaks
3. Individualized
4. Monitor BGL before, during, and after exercise
5. Carry fast-acting source of carbohydrate.
6. Don't exercise if ketones are present in urine.
7. If BGL < 100 mg/dL, eat a 15-gram snack
-
Diabetes Complications
1. Ulcers/Wounds
2. Stroke
3. MI
4. Peripheral Edema
5. Neuropathy / PAD
6. Testing for sensation in those with diabetes especially in feet, talk about appropriate footwear.
7. Semmes-Weinstein monofilament is used to assess feet of diabetics it weighs 10 grams
8. Periodontal disease
9. Retinopathy, glaucoma, cataracts
10. Kidney disease
-
Type I Diabetes
1. Destruction of the pancreatic islet cells
2. Causes: gentics, environment
3. Onset: often younger people
4. Produce little to no insulin
5. Not preventable
-
Diagnosing Type II Diabets
1. Usually diagnosed with a1c test.
2. <5.7% is normal, 5.7 to 6.4% is prediabetic, and >6.5 indicates diabetes.
3. Fasting bgl test >126 diabetes
4. Random BGL. >200 diabetes
5. Oral glucose tolerance test: >200 diabetes
-
Management of Type I diabetes
1. Insulin dependent, use insulin pumps
2. Continuous glucose monitoring
3. diet and exercise
4. avoid alcohol
5. watch for DKA
-
Diabetic Ketoacidosis (DKA)
1. Medical emergency
2. Ketones in blood or urine
3. S/s: fatigue, confusion, stomach pain, pee more, blurred vision, thirsty, SWEET BREATH, high BGL
4. Tx: IV fluids, insulin, electrolyte replacement
-
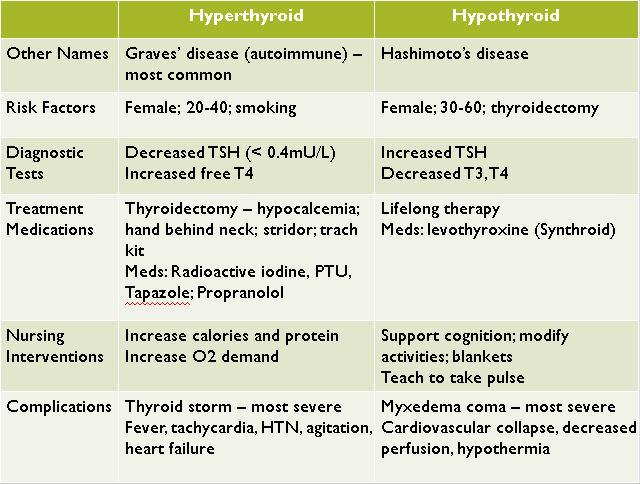
Thyroid disorders
1. T3 and T4 needed to increased the rate of metabolism.
2. Oxygen consumption, tissue function in every major organ system, Ca level balance (inc w/ parathyroid syndrome with hypothyroidism)
3. Hypothyroidism = suboptimal levels of thyroid hormone (myxedema coma)
4. Hyperthyroidism = excessive levels of thyroid hormone (thyroid storm)
-
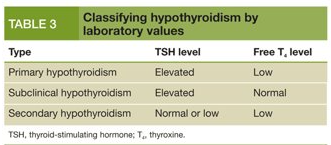
Hypothyroidism
1. Classified as : adult-risk for myxedema with severe standing, Juvenile (1-2 yr), Congenital: occurring at, or around birth
2. Causes: thyroidectomy, autoimmune thyroiditis (Hashimoto's disease)
3. Most common in women 30-60 years old.
4. S/s: slowed metabolism, hair loss, fatigue, sensitivity to COLD, dry skin, constipation, sore muscles
5. Dx: TSH and T4 levels, blood test, TSH avg 0.5-5 mL
-
Hypothyroidism Treatment
1. Replace missing thyroid hormones
2. Levothyroxine: synthetic form of t4, take on EMPTY stomach at same time each day. Do not change brands, life long treatment, follow up thyroid labs, may take 4-6 weeks for effect, watch for hyperthyroid
-
Hypothyroid complications
1. Of hypo: myxedema coma, low energy, cardiac dysfunction, slow metabolism, hypotension
2. Of treatment: hyperthyroidism, thyroid storm, HTN and tachycardia.
3. Teaching: monitor O2 levels, routine for taking meds, s/s of both hyper/hypothyroid, lifelong treatment, follow-up appointments for t4 levels
-
Hyperthyroidism
1. Overexcretion of thyroid hormone
2. Causes: Graves disease, toxic multinodular goiter, toxic adenoma, thyroid tumors
3. Much more common in women.
4. s/s: overactive metabolism, heat insentivity, tremors, BM more frequent, goiter (swelling at neck), irritability
5. Dx: enlarged thyroid (goiter), elevated thyroid hormone levels, increase uptake of radioactive iodine (thyroid uses iodine to make t4).
-
Hyperthyroidism Management
1. Antithyroid meds
2. Cardiac meds for arrythmias (propanolol)
3. Radioactive iodine to kill off thyroid
4. Surgery - to remove most of thyroid
5. Treat HTN
-
Thyroidectomy Post OP Care
1. Head of bed semi-fowler's, neck aligned
2. Possible Ca supplement if parathyroid was accidently taken.
3. Possible levothyroxine treatment for life.
4. Pain management
5. JP drains, monitor incision for infection
6. Should not exercise strenuously for 3 weeks, do not overextend neck backwards, can shower after drain has come out
-
Hyperthyroidism Complications
1. Of hyperthyroid: thyroid storm, blurred vision, heart failure, osteoporosis
2. Of treatment: hypothyroidism, Iodine toxicity (if using using radioactive iodine)
-
Hypothyroid vs. Hyperthyroid
-
Overview of Eye
1. Eye assessment: CN 3,4,6 , PERRLA, Ptosis(drooping), Nystagmus(involuntary movement), Redness/discharge, visual acuity.
-
Common Eye Medications
1. Anesthetic agents (numbness) (-caine): Proparacaine, tetracaine.
2. Mydriatic (dilators/diagnostic testing): epi, tropicamide
3. Antiallergy: -olopatadine
4. Anti-inflammatory: Corticosteroids, NSAIDs
5. Anti-infectives: Antibiotics=penicillin, Antifungals=amphotericin B
-
Glaucoma
1. Group of conditions related to increase in intraocular pressure (IOP). Cause damage to ocular nerve. Slow onset cannot be cured.
2. Classifications: open, acute, congenital
3. S/s: blurred vision, headaches, sudden or serve pain, n/v (acute), loss of peripheral vision, halos around lights.
4. In acute see more severe HA, blurred vision, n/v, redness in eye.
-
Glaucoma Treatments / NI
1. Meds: betablockers (timolol) reduce aqueous humor production, cholinergic (pilocarpine) promote fluid outflow.
2. Surgery to promote outflow of fluids
3. Goal: lower IOP, stable optic nerve
4. NI: pain, safety, teach proper med admin, diet LOW salt
-
Cataracts
1. Lens become cloudy, gradual loss of vision
2. Causes: aging, trauma, UV rays, smoking
3. S/s: painless, blurred vision, loss on contrast, double vision
4. Half all muricans >80 have cataracts
-
Cataract Treatment
1. Surgery: removal of lens, lens replacement options implants or glasses/contacts
2. Goal: restoration of visual function
3. NI: post op eye drops: anti-inflammatory and antibiotics; teach cleanliness signs of infection; avoid lying on affected side; avoid IOP (don't strain with BM, don't bend over)
-
Retinal Detachment
1. When part of the retina pull away from neurosensory layer, can lead to retinal tear
2. Ocular emergency
3. Causes: trauma, diabetic retinopathy, eye surgeries
4. Symptoms: visual disturbances
5. Tx: surgery, reattach retina through contact with neurosensory layer
6. NI: post op eye drops, anti-inflammatory, antibiotics, teach s/s of IOP, avoid lying on affected side.
-
Macular Degeneration
1. Related to aging
2. Irreversible visual impairment
3. Can lead to total blindness, people lose vision in center of eye as macula thins.
4. Wet: abnormal blood vessel growth and leakage
5. Dry (more common): thinning of macula with aging.
6. Tx: Wet inject VEGF inhibitors, Dry there is no treatment, can slow progression through healthy lifestyle.
7. NI: safety, ability for selfcare, avoid lying on operative side, avoid IOP (straining, bending over)
-
Emergency Eye Treatment
1. Apply eye patch
2. HOB elevated
3. Removal of foreign bodies
4. Low light
5. Pain management
6. Antibiotics, aseptic techinques.
-
Anatomy of Immune system
1. bone marrow (wbc) produced
2. Spleen releases leukocytes
3. Barrier organs, skin/mucous membranes
-
Function of immune system
1. Defends body, antigens trigger a response, injury triggers a response (antibodies)
2. Immune responses: increased respiratory secretions and/or inflammation
3. Immune system learns to make antibodies for diseases.
-
Types of Immunity
1. Natural/Active = acquired immunity your body learns how to defend, vaccine or actually getting disease
2. Passive immunity = breast milk or IV antibodies
3. Herd immunity = majority of people immune through vaccine or having disease, wont spread
-
Disfunction of Immune System
1. Neoplastic disorders: cancer we form cancer cells all the time but immune system gets rid of them.
2. Autoimmune disorders: immune system attacks healthy cells and tissues. More than 80 diseases, genetic component to some, women, symptoms depend on tissue attacked.
-
Lupus
1. Immune system identifies part of cell nucleus as foreign
2. Has immunological, genetic, hormonal, environmental
3. Affects many systems
4. Characterized by exacerbations
5. Inflammatory response - joint swelling and pain
6. Tx: corticosteroids, monoclonal antibodies.
7. S/s: butterfly rash, deep ulcerative, Raynaud's phenomena, red skin
-
Rheumatoid Arthritis
1. Autoimmune disorder, joints in body are attacked and actual degeneration of the joint occurs.
2. Most obvious in hands and fingers. ULNAR drift
3. Can be systemic as well: fever, weight loss, fatigue, anemia
4. more common in women
-
Allergies
1. Normal immune response: antibodies react to antigens
2. Abnormal response: harmful response to harmless substance
3. Allergies: symptoms of a reaction
4. Hypersensitivity: immunological process in body
-
Treating Mild Allergies
1. Remove allergen
2. Monitor airway
3. Antihistamines - diphenhydramine (help later but will take hours to filter out histamines)
4. Steroids- Flonase, hydrocortisone cream
5. Allergy history
6. Teach to avoid allergens
7. Desensitization therapy
-
Anaphylactic Shock
1. Severe allergic reactions
2. Potent vasoactive substance released: histamine, bradykinin.
3. Widespread vasodilation and capillary permeability
4. Huge drop in BP, arrythmias
5. Dyspnea - laryngeal edema
6. S/s: LOC, hives, swelling
-
Treating Anaphylactic shock
1. Remove allergen
2. Airway support, check mouth
3. Epi
4. Benadryl/antihistamine
5. Albuterol inhaler or nebulizer
6. BP support, fluid management
7. Monitor cardiac function.
-
HIV (Human Immune deficiency)
1. Virus that replicates inside CD4 cells
2. Non curable (viral)
3. HIV - acquired immune deficiency
4. AIDS - acquired immune deficiency syndrome
-
HIV Diagnosing and progression
1. Stages: Initial infection, Equilibrium to symptomatic, AIDS
2. Dx: antibody/antigen testing, viral load, cd4 cell count, s/s of opportunistic infections
3. Transmission: person to person, unprotected sex, pregnancy, needles, blood
4. 90-90-90: aware, on treatment, virally suppressed
5. Meds: anti viral (ART), multidrug treatment, life long
-
Osteoporosis
1. Osteopenia starts, Osteoporosis
2. Loss of bone density
3. more common in women
4. Osteoclasts = break down bone
5. Osteoblasts = build up bone
6. RF: age >50, low Ca, sedentary lifestyle, smoking, family history, short stature, Vit. D levels, corticosteroid use, Low estrogen
7. CM: fractures, postural changes
8. Dx: DEXA scan, quantitative CT
9. Management: weight exercises, eliminate smoking/alcohol, good nutrition.
10. Meds: biphosphonates (fosamax), pth stimulants, estrogen, vit d, Ca supplments
-
Osteoarthritis
1. Degeneration of the joint
2. Damage not caused by inflammation.
3. By age 40, 90% of population has some degeneration
4. Degen from: mechanical factors, genetic factors, biochemical factors
5. RF: female, obese, repetitive motion, genetics
6. CM: loss of cartilage w/ osteophyte formation, weight bearing joints, Bouchard's and Heberden's nodes, increased pain with activity, swelling, crepitus, decreased ROM, instability.
-
Progression of Degeneration in Osteoarthritis
1. Bones changes in weight bearing joints.
2. Cartilage damage
3. Synovitis
4. Osteophyte formation
-
Management of Osteoarthritis
1. Prevention
2. Pharmalogical: NSAIDs/ acetaminophen, duloxetine (cymbalta), cortisone or lubrication injection into joints, vit D and Ca supplement
3. Joint replacement
4. PT/OT
5. Transcutaneous electrical nerve stimulation (TENS)
6. Weight bearing exercise
7. Weight loss

