Kidneys, Electrolytes and Fluid Balance
1. Kidneys take out from blood what is not needed and put back what is in needed.
2. Loop of Henly reinfuses electrolytes.
3. Osmolality, how concentrated urine is particles per water.
4. Kidney controls BP through excretion.
Urine Assessments
1. Changes in voiding habits
2. Urinary retention
3. Cloudy/discolored urine
4. Foul-smelling urine
5. Blood tinged
6. Lower back pain
7. Pain with urination
8. Fluid and electrolyte balances.
Urinary Function Tests and Labs
1. Renal function tests - US, MRI, cystography, angiography, endoscopy
2. Urinalysis / Culture and sensitivity
3. Creatine - Muscle metabolism, for men 0.74 to 1.35
4. GFR - filtration function 60 or up
5. Blood urea nitrogen (BUN) - Kidney function: 6-24 mg/dL (problem if too low)
6. Specific Gravity- Urine dilution: 1.005 - 1.030
7. Albumen - Kidney damage: below 30 g/dL
8. WBC: 2-5
9. RBC: 2-4
Reading Urine Color
1. Clear: overhydration, diuretics, or diabetes insipidus
2. Straw yellow: normal color result of urobilin
3. Orange: dehydration or infection
4. Brown: increased bilirubin, blood break down or liver disease
5. Red: blood from infection, stone or tumor, menstruation. Dyed by drugs such as Rifampicin or Rhubarb.
6. Blue/green: contrast medium after scan
7. Cola: rhabdo, muscle break down, major trauma or muscle injury
UTI Risk factors
1. Catherization
2. Female
3. Hygiene issues
4. Sex
5. Immunosuppression
6. Post menopausal,
7. E. Coli
UTI Clinical Manifestations and Prevention
1. confusion
2. fever
3. pain w/ urination
4. urgency/frequency issues
Protection by: hydration and safe sex.
5. Dx by: dipstick for leukocyte esterase and nitrates, UA and C+S
Cystitis (Lower UTI)
1. Lower tract infection
2. Bacterial is common
3. Reflux to kidneys
4. Issues with urinary urgency, frequency, pain with urination
5. NC: output, pain management, cognitive assessment, fall risk, teach cleanliness
Pyelonephritis (Upper UTI)
1. Bacterial is common, use antibiotics (levoflaxcin, sulfonamides).
2. s/s: fevers, chills, low flank pain, pain on urination
3. NC: output, pain management, cognitive assessment, fall risk
Renal Calculi
1. Risk factors: hydration, diet high in salt or calcium or vit D.
2. Clinical p: pain, blood in urine
3. Prevention: hydration
Renal calculi can be formed in kidneys or bladder. ureters are usually the issue. most organs don't have pain receptors for injury but do for stretching.
Urolithiasis (kidney stones)
1. Stones mostly made of Ca
2. Risk factors: previous stones, urinary status, gout, male, lifestyle, diet, excess body weight.
3. Clinical p: pain, lower flank pain, waves of pain, burning with urination, frequency issues, discolored urine, fevers, chills.
4. Stag horn kidney stones require surgical intervention.
Extracorporeal Shock Wave Lithotripsy (ESWL)
ESWL is a noninvasive procedure that breaks down stones in parts of the urinary system, in the pancreas and in the bile ducts. It uses shock waves that are aimed at stones, with the help of X-rays or ultrasound. Stones in the kidneys and ureter often pass on their own after EWSL.
Renal Calculi Nursing Considerations
1. Pain
2. Monitor urine amount and character
3. Increase fluids
4. Strain all urine
Tx: ultrasound shockwave or surgery
Acute Kidney Injury (AKI)
1. RF: utis, trauma
2. CM: increased creatine ≥0.3 mg/dL within 48 hrs, or increased serum creatine x1.5 times the baseline in past 7 days, or a urine volume of less than 0.5mL/kg/hr for 6 hours
Causes of AKI
1. Decreased blood flow
2. Direct damage to kidneys
3. Blockage of urinary tract
AKI treatments
1. Prerenal: correct hemodynamic derangements, fluids or diuretics
2. Intrarenal: treat the underlying disease
3. Postrenal: relieve obstruction, through foley, nephrostomy tube, antibiotics
Four Phases of AKI
1. Onset (hours to days): renal blood flow 25% of normal, urine output < 0.5mL/kg/hour
2. Oliguric/anuric (8-14 days): output < 400mL in a day, increase in BUN and creatine. Electrolyte disturbances, fluid overload since kidneys can't excrete water
3. Diuretic phase (7 to 14 days): Occurs when AKI cause is corrected, increased GFR, daily urine output > 400 mL, Possible electrolyte depletion from excretion of more water and osmotic effects of high BUN.
4. Recovery phase (months to 1 year): decreased edema, normal fluid/electrolyte balance, return of GFR to 70-80% of normal
AKI Nursing Considerations
1. Prevent further injury
2. Treat underlying cause
3. Correct fluid/electrolyte imbalance (diuretics, treat hyperkalemia)
4. Avoid nephrotxic drugs, NSAIDs, contrast dyes
5. Good assessment (resp, cardiac, skin)
6. Nutrition (sodium and calorie restriction)
7. Monitor I/O and VS
Prerenal, Intrarenal, and Postrenal concerns practice
Prerenal: decreased cardiac output, hypovolemia,
Intrarenal: calculi, nephrotoxic drugs, acute glomerulonephritis
Postrenal: , calculi, prostate cancer
Chronic Renal Failure
1. RF: HTN, DM, NSAIDs, genetics, previous kidney injuries, age
2. CM: electrolyte/fluid imbalance, anemia, acidosis
3. Prevention: life choices, prevent utis
4. Stages: 1=normal 2= mild 3= moderate 4= severe 5= failure
Dialysis
1. Preserve kidney function for as long as possible with medications.
2. Peritoneal dialysis: abdominal catheter, slow movement of waste (homeostasis), peritoneal membrane is semipermeable, 3-5 times a day.
3. Hemodialysis: implanted shunt, outpatient procedure, 3 times a week for 3-4 hours.
Renal Failure Nursing Considerations
1. Daily weights
2. Monitor electrolytes and renal labs
3. Dietary restrictions: Reduced sodium, potassium, and phosphorus (SPPP), reduced protein, fruits and veggies.
4. nutritional support
5. Monitor for infection
6. Encourage activity
7. Psychosocial support
Breast disorders
1. Mastitis: infection/inflammation of breast tissue
2. Cysts: fluid formed can be drained, 5-10mL
3. Pain
4. Cancer: very common in breasts
Breast Cancer Risk Factors
1. Advanced age
2. Alcohol
3. Female
4. Nulliparity (no pregnancies)
5. Ashkenazi Jewish heritage
6. Late menopause
7. Recent HRT
8. Genetics
(not malnutrition)
Breast Assessment
1. Lumps
2. Skin dimpling
3. Change in skin color or texture
4. Change in how nipple looks, like pulling of nipple
5. Clear or bloody fluid leaks from nipple
Breast Diagnostics Tools
1. Mammography
2. Biopsy
3. Ultrasound
something show up on US but not on mammo. Biopsy takes core sample of tissue, huge risk for hematoma afterwards, pressure for first 24 hrs is helpful.
Modified Radical Mastecotomy
1. Once cancer is in lymph nodes it can spread anywhere. Prostate cancer matasizies to the bone.
2. Staging of cancer helps determine level of treatment.
3. Large incision with lots of drainage to remove breast tissue. JP drains to remove fluid
4. Teach JP drains, when to empty (starts to loose suction), concerning colors (green/yellow), clip to shirt, showering, outline infections and date it
5. Elevate arm after mastectomy
Post Mastectomy Care
1. Elevate affected side w/ distal joint higher than proximal joint.
2. No BP, injections on affected side.
3. Psychological concerns
4. Maintain pressure dressings
5. Watch for edema and infection
6. Arm exercise within 24 hrs after surgery.
Mastectomy Discharge Teaching
1. Pt goes home within 24 hrs usually
2. Silicon implants have risks
3. Lymphedema, lymph doesn't have pump, needs movement to move blood.
4. Arm exercises
5. Pain management.
Menstural Disorders
1. Purpose of mensuration: slough off lining of uterus when not pregnant.
2. Premenstrual syndrome: body reacts to ebb and flow of different hormones being released. mood swings/discomfort
3. Dysmenorrhea: lower abd pain, just before or during menstruation.
4. Amenorrhea: absence of menstruation
Contraception / Abortion
1. Types of contraception: hormonal, barrier, rhytm/withdrawl
2. Abortion: spontaneous (before 20th week), emergency, induced
Infertility Pregnancy complications
1. Female Factors: egg levels
2. Male Factors: lack of mature sperm
3. Pregnancy complications: ectopic pregnancies, fertilized egg but implants in fallopian tube, is an emergency, gets bigger until it ruptures.
Infectious disorders / Structural Disorders women reproductive
1. Bacterial vaginosis: can be fungal as well
2. STI
3. fistula is a connecting hole
4. Loose ligaments
5. uterine prolapse, not threating but surgery can be done to correct.
Malignant disorders of menopause
1. Older women rf
2. Cessation of mensturation
cancer can affect any internal strucutres
Benign Prostatic Hyperplasia (BPH)
1. RF: over 50 yrs old
2. S/s: frequency, nocturia, hesitation, difficulty starting stream
3. Dx tests: Rectal digital test, transdermal ultrasound, checking PSA levels (PSA will be high with BPH)
4. Complications: flank pain, decreased urine output.
BPH Meds
1. Alpha adrenergic agonists: relax the smooth muscle, ex: tamsulosin (flomax), terazosin (hyrtrin), doxazosin (cardura).
2. Alpha reductase inhibitors: inhibit enzyme responsible for formation of androgen, ex: finasteride (proscar), dutasteride (avodart)
Transurethral Resection of the Prostate (TURP)
x. Go in through the penis urethra, not surgical
1. CBI
2. Close observation of drainage system, maintain catheter patency
3. Bladder spasms
4. Pain control w/ analgesics limit activity first 24 hours
5. Avoid straining with BMs, high fiber and laxatives
6. Complications: hemorrhage go to light pink urine in 24 hrs, urinary incontinence, infections, DVTs
7. do not elevate pelvis
8. There should be NO PSA after removal of prostate, if there is that means cancer.
Continuous Bladder Irrigation (CBI)
1. Threeway catheter: Irrigation, Balloon, Drainage
2. Use sterile irrigation solution
3. Blood clots are expected
4. Ideal color is light pink, no clots
5. remove 2-4 days post op
6. Do not elevate pelvis
Other Male Reproductive disorders
1. Erectile dysfunction: physical or hormonal dysfunction.
2. Cancer: can affect any of the structures, penile, testicular, prostate, fast growing easy to detect easy cure.
3. Infection: prostatitis, infection of prostate, ependymitis=infection of testicles.
Chlamydia and Gonorrhea
1. Chlamydia - most common STI, gonorrhea 2nd most common
2. Both are bacterial infections
3. Antibiotics to cure
4. S/s: vaginal/penile discharge, bleeding, pain, fever chills n/v, pelvic inflammatory disease (PID). can cause sterility in women, can prevent sperm getting through in men.
5. RF: poor hygiene, multiple sex partners, unprotected sex, history of STIs. Discontinue IUD.
Herpes
1. Oral or genital
2. Viral infection treated with antivirals. Not a cure.
3. S/s: dormant vs outbreaks, itching, pain, ulcerations contagious.
4. Stages: prodroma, vesicular (blister) ulceration (lesion rupture)
5. Medical management: cannot be cured, anti virals to control symptoms and discomfort, keep lesions clean.
6. Prevention: avoid contact
7. Pregnancy risk: can be passed on birth, antibiotic eye drops soon as born.
Syphilis
1. Was considered fatal, unethical study with tuskgee airmen
2. Bacterial, can be treated with antibiotics at chance for cure if caught early.
3. Stages:
primary = chancre,
secondary = rash,
latent = asysptomatic
tertiary = multisystem, brain heart bones
4. Antibiotics and curable for most
5. Prevention: avoid skin contact, sexual contact, keep clean.
Human Papillomavirus
1. Most common virus in US = HPV
2. basically warts not curable because viral, causes CANCER
3. s/s: genital warts, painful, emotional distress
4. mm: treat warts if present with ablation with cyrotherapy, can go away on its own
5. Prevention: avoid skin contact, sexual contact, vaccine series available
HIV (human immune deficiency virus)
1. Virus attacks CD4 immune cells
2. Stages:
stage1 = flu symptoms then asymptomatic
stage2 = opportunistic infections
stage3 = AIDs
3. mm: not curable, antiviral therapy life long multiple drugs, pill fatigue
4. prevention: avoid sexual contact until virally suppressed, not contagious with viral suppression.
Adrenal Function
1. Adrenal glands regulate many hormones.
2. Cortisol regulates: stress response, metabolism, fluid balance
Addison's Disease (Adrenocortical Insufficiency)
1. Not enough cortisol
2. Often caused by autoimmune or feedback loop issues
3. Increased excretion of sodium, chloride, and water
4. Dx: physical assessment (often start nonspecific), labs for cortisol levels, CT can give insight
5. S/s: weight loss, darken skin, BP lower, fainting, salt cravings, muscle cramping, joint pain, hypoglycemia, n/v
Corticosteroid Therapy
1. Used to: suppress inflammation, allergic reactions, reduce swelling control autoimmune disorders, Addison's Disease
2. Common drugs: Hydrocortisone, Prednisone
3. Allows for better stress responses
4. Needs to be tapered off
Cushing Syndrome
1. Too much cortisol
2. Causes: long term use of corticosteroids, adrenal tumors (comes with prolonged use)
3. S/s: high glucose, poor wound healing, weight gain, easy bruising, cardiac hypertrophy, osteoporosis, weakness
4. NI: skin assessment for bruise/tears, wound healing. Monitor pulse, orthostatic BP, BGL, energy levels, weight
Addison's / Cushing syndrome teaching
1. Mood changes mental health
2. impact of long term corticosteroid use
3. treatment is life long
4. health maintenance; diet and exercise
5. Watch fluid balance, daily weights, sodium and water balance.
Diabetes Risk Factors
1. Obesity
2. Family history
3. Age
4. Ethnicity
5. Gestational diabetes
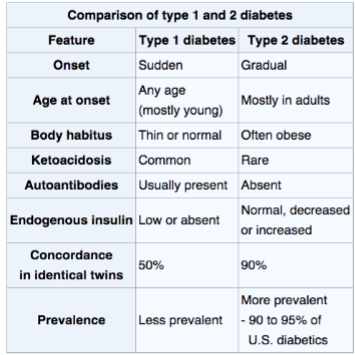
Type 1 vs. Type 2 Diabets
Diabetes Diagnostics
1. Fasting blood glucose levels, >126 is diabetes
2. Symptoms of hyperglycemia (thirst, hunger, peeing alot, tired)
3. Oral Glucose Tolerance test (OGTT) - screens for type 2, measures sugar tolerance
4. HgbA1C - couple month average of sugars
Hypoglycemia vs. Hyperglycemia
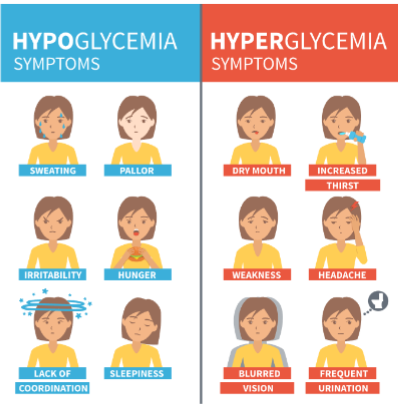
Hypoglycemia Treatment
1. Give apple or orange juice, 15 carbs with no fat or protein if able to swallow.
2. If not able to swallow, IV D50 or glucagon (IM).
3. Recheck sugars in 15 minutes
4. Repeat until at normal levels
5. At normal BGL, give long acting carb and protein.
Type II Diabetes
1. Insulin resistance
2. Usually older than 30
3. Reduced Insulin production
4. Slow progression
5. Vascular damage
6. Can be preventable
7. manage: exercise, monitoring, education, diet, pharmacologic therapy.
Diabetes Labs to Watch
1. Blood Labs: Potassium, Ketones, Glucose, Renal function, Lipids
2. Urine: albumin, ketones, glucose
Common Diabetes Medications
1. Glyburide: take at breakfast, watch for hypoglycemia, GI upset
2. Metformin: take twice a day with meals, watch for hypoglycemia, GI upset, avoid imaging contrast dyes
3. Glucagon: for seriously low BG levels.
Insulins
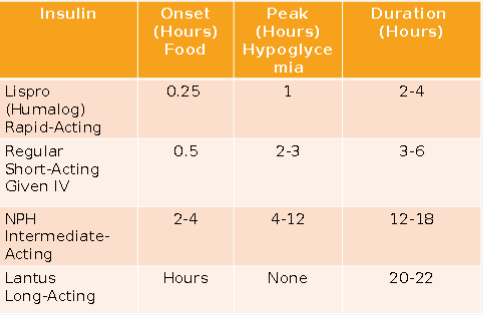
Mixing insulin
1. Draw up Clear (regular) before Cloudy (Long acting/ NPH)
Insulin delivery
1. Rotate sites
2. Give before meals if possible
3. Teach how to give injections
4. Carb counting orders: 1 unit of insulin per 15-grams of carbohydrate.
Sick days in Type 1+2 Diabetes
1. Emotional and physical stress can result in hyperglycemia.
2. Maintain diet/fluid intake
3. Do NOT withhold medications
4. Supplement intake with carbohydrate containing fluids.
5. Check BGL every 4 hours
6. Check urine for ketones if BGL > 240 mg/dL
Diabetes and Exercise
1. Improves insulin sensitivity
2. Best to do after meals but not when insulin peaks
3. Individualized
4. Monitor BGL before, during, and after exercise
5. Carry fast-acting source of carbohydrate.
6. Don't exercise if ketones are present in urine.
7. If BGL < 100 mg/dL, eat a 15-gram snack
Diabetes Complications
1. Ulcers/Wounds
2. Stroke
3. MI
4. Peripheral Edema
5. Neuropathy / PAD
6. Testing for sensation in those with diabetes especially in feet, talk about appropriate footwear.
7. Semmes-Weinstein monofilament is used to assess feet of diabetics it weighs 10 grams
8. Periodontal disease
9. Retinopathy, glaucoma, cataracts
10. Kidney disease
Type I Diabetes
1. Destruction of the pancreatic islet cells
2. Causes: gentics, environment
3. Onset: often younger people
4. Produce little to no insulin
5. Not preventable
Diagnosing Type II Diabets
1. Usually diagnosed with a1c test.
2. <5.7% is normal, 5.7 to 6.4% is prediabetic, and >6.5 indicates diabetes.
3. Fasting bgl test >126 diabetes
4. Random BGL. >200 diabetes
5. Oral glucose tolerance test: >200 diabetes
Management of Type I diabetes
1. Insulin dependent, use insulin pumps
2. Continuous glucose monitoring
3. diet and exercise
4. avoid alcohol
5. watch for DKA
Diabetic Ketoacidosis (DKA)
1. Medical emergency
2. Ketones in blood or urine
3. S/s: fatigue, confusion, stomach pain, pee more, blurred vision, thirsty, SWEET BREATH, high BGL
4. Tx: IV fluids, insulin, electrolyte replacement
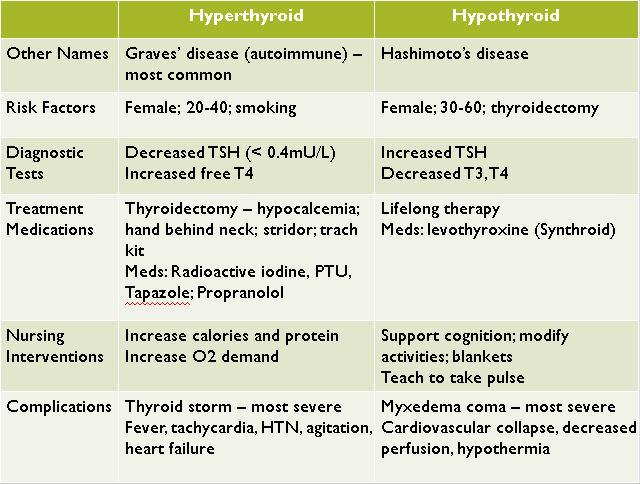
Thyroid disorders
1. T3 and T4 needed to increased the rate of metabolism.
2. Oxygen consumption, tissue function in every major organ system, Ca level balance (inc w/ parathyroid syndrome with hypothyroidism)
3. Hypothyroidism = suboptimal levels of thyroid hormone (myxedema coma)
4. Hyperthyroidism = excessive levels of thyroid hormone (thyroid storm)
Hypothyroidism
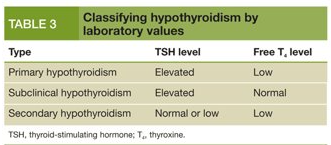
1. Classified as : adult-risk for myxedema with severe standing, Juvenile (1-2 yr), Congenital: occurring at, or around birth
2. Causes: thyroidectomy, autoimmune thyroiditis (Hashimoto's disease)
3. Most common in women 30-60 years old.
4. S/s: slowed metabolism, hair loss, fatigue, sensitivity to COLD, dry skin, constipation, sore muscles
5. Dx: TSH and T4 levels, blood test, TSH avg 0.5-5 mL
Hypothyroidism Treatment
1. Replace missing thyroid hormones
2. Levothyroxine: synthetic form of t4, take on EMPTY stomach at same time each day. Do not change brands, life long treatment, follow up thyroid labs, may take 4-6 weeks for effect, watch for hyperthyroid
Hypothyroid complications
1. Of hypo: myxedema coma, low energy, cardiac dysfunction, slow metabolism, hypotension
2. Of treatment: hyperthyroidism, thyroid storm, HTN and tachycardia.
3. Teaching: monitor O2 levels, routine for taking meds, s/s of both hyper/hypothyroid, lifelong treatment, follow-up appointments for t4 levels
Hyperthyroidism
1. Overexcretion of thyroid hormone
2. Causes: Graves disease, toxic multinodular goiter, toxic adenoma, thyroid tumors
3. Much more common in women.
4. s/s: overactive metabolism, heat insentivity, tremors, BM more frequent, goiter (swelling at neck), irritability
5. Dx: enlarged thyroid (goiter), elevated thyroid hormone levels, increase uptake of radioactive iodine (thyroid uses iodine to make t4).
Hyperthyroidism Management
1. Antithyroid meds
2. Cardiac meds for arrythmias (propanolol)
3. Radioactive iodine to kill off thyroid
4. Surgery - to remove most of thyroid
5. Treat HTN
Thyroidectomy Post OP Care
1. Head of bed semi-fowler's, neck aligned
2. Possible Ca supplement if parathyroid was accidently taken.
3. Possible levothyroxine treatment for life.
4. Pain management
5. JP drains, monitor incision for infection
6. Should not exercise strenuously for 3 weeks, do not overextend neck backwards, can shower after drain has come out
Hyperthyroidism Complications
1. Of hyperthyroid: thyroid storm, blurred vision, heart failure, osteoporosis
2. Of treatment: hypothyroidism, Iodine toxicity (if using using radioactive iodine)
Hypothyroid vs. Hyperthyroid
Overview of Eye
1. Eye assessment: CN 3,4,6 , PERRLA, Ptosis(drooping), Nystagmus(involuntary movement), Redness/discharge, visual acuity.
Common Eye Medications
1. Anesthetic agents (numbness) (-caine): Proparacaine, tetracaine.
2. Mydriatic (dilators/diagnostic testing): epi, tropicamide
3. Antiallergy: -olopatadine
4. Anti-inflammatory: Corticosteroids, NSAIDs
5. Anti-infectives: Antibiotics=penicillin, Antifungals=amphotericin B
Glaucoma
1. Group of conditions related to increase in intraocular pressure (IOP). Cause damage to ocular nerve. Slow onset cannot be cured.
2. Classifications: open, acute, congenital
3. S/s: blurred vision, headaches, sudden or serve pain, n/v (acute), loss of peripheral vision, halos around lights.
4. In acute see more severe HA, blurred vision, n/v, redness in eye.
Glaucoma Treatments / NI
1. Meds: betablockers (timolol) reduce aqueous humor production, cholinergic (pilocarpine) promote fluid outflow.
2. Surgery to promote outflow of fluids
3. Goal: lower IOP, stable optic nerve
4. NI: pain, safety, teach proper med admin, diet LOW salt
Cataracts
1. Lens become cloudy, gradual loss of vision
2. Causes: aging, trauma, UV rays, smoking
3. S/s: painless, blurred vision, loss on contrast, double vision
4. Half all muricans >80 have cataracts
Cataract Treatment
1. Surgery: removal of lens, lens replacement options implants or glasses/contacts
2. Goal: restoration of visual function
3. NI: post op eye drops: anti-inflammatory and antibiotics; teach cleanliness signs of infection; avoid lying on affected side; avoid IOP (don't strain with BM, don't bend over)
Retinal Detachment
1. When part of the retina pull away from neurosensory layer, can lead to retinal tear
2. Ocular emergency
3. Causes: trauma, diabetic retinopathy, eye surgeries
4. Symptoms: visual disturbances
5. Tx: surgery, reattach retina through contact with neurosensory layer
6. NI: post op eye drops, anti-inflammatory, antibiotics, teach s/s of IOP, avoid lying on affected side.
Macular Degeneration
1. Related to aging
2. Irreversible visual impairment
3. Can lead to total blindness, people lose vision in center of eye as macula thins.
4. Wet: abnormal blood vessel growth and leakage
5. Dry (more common): thinning of macula with aging.
6. Tx: Wet inject VEGF inhibitors, Dry there is no treatment, can slow progression through healthy lifestyle.
7. NI: safety, ability for selfcare, avoid lying on operative side, avoid IOP (straining, bending over)
Emergency Eye Treatment
1. Apply eye patch
2. HOB elevated
3. Removal of foreign bodies
4. Low light
5. Pain management
6. Antibiotics, aseptic techinques.
Anatomy of Immune system
1. bone marrow (wbc) produced
2. Spleen releases leukocytes
3. Barrier organs, skin/mucous membranes
Function of immune system
1. Defends body, antigens trigger a response, injury triggers a response (antibodies)
2. Immune responses: increased respiratory secretions and/or inflammation
3. Immune system learns to make antibodies for diseases.
Types of Immunity
1. Natural/Active = acquired immunity your body learns how to defend, vaccine or actually getting disease
2. Passive immunity = breast milk or IV antibodies
3. Herd immunity = majority of people immune through vaccine or having disease, wont spread
Disfunction of Immune System
1. Neoplastic disorders: cancer we form cancer cells all the time but immune system gets rid of them.
2. Autoimmune disorders: immune system attacks healthy cells and tissues. More than 80 diseases, genetic component to some, women, symptoms depend on tissue attacked.
Lupus
1. Immune system identifies part of cell nucleus as foreign
2. Has immunological, genetic, hormonal, environmental
3. Affects many systems
4. Characterized by exacerbations
5. Inflammatory response - joint swelling and pain
6. Tx: corticosteroids, monoclonal antibodies.
7. S/s: butterfly rash, deep ulcerative, Raynaud's phenomena, red skin
Rheumatoid Arthritis
1. Autoimmune disorder, joints in body are attacked and actual degeneration of the joint occurs.
2. Most obvious in hands and fingers. ULNAR drift
3. Can be systemic as well: fever, weight loss, fatigue, anemia
4. more common in women
Allergies
1. Normal immune response: antibodies react to antigens
2. Abnormal response: harmful response to harmless substance
3. Allergies: symptoms of a reaction
4. Hypersensitivity: immunological process in body
Treating Mild Allergies
1. Remove allergen
2. Monitor airway
3. Antihistamines - diphenhydramine (help later but will take hours to filter out histamines)
4. Steroids- Flonase, hydrocortisone cream
5. Allergy history
6. Teach to avoid allergens
7. Desensitization therapy
Anaphylactic Shock
1. Severe allergic reactions
2. Potent vasoactive substance released: histamine, bradykinin.
3. Widespread vasodilation and capillary permeability
4. Huge drop in BP, arrythmias
5. Dyspnea - laryngeal edema
6. S/s: LOC, hives, swelling
Treating Anaphylactic shock
1. Remove allergen
2. Airway support, check mouth
3. Epi
4. Benadryl/antihistamine
5. Albuterol inhaler or nebulizer
6. BP support, fluid management
7. Monitor cardiac function.
HIV (Human Immune deficiency)
1. Virus that replicates inside CD4 cells
2. Non curable (viral)
3. HIV - acquired immune deficiency
4. AIDS - acquired immune deficiency syndrome
HIV Diagnosing and progression
1. Stages: Initial infection, Equilibrium to symptomatic, AIDS
2. Dx: antibody/antigen testing, viral load, cd4 cell count, s/s of opportunistic infections
3. Transmission: person to person, unprotected sex, pregnancy, needles, blood
4. 90-90-90: aware, on treatment, virally suppressed
5. Meds: anti viral (ART), multidrug treatment, life long
Osteoporosis
1. Osteopenia starts, Osteoporosis
2. Loss of bone density
3. more common in women
4. Osteoclasts = break down bone
5. Osteoblasts = build up bone
6. RF: age >50, low Ca, sedentary lifestyle, smoking, family history, short stature, Vit. D levels, corticosteroid use, Low estrogen
7. CM: fractures, postural changes
8. Dx: DEXA scan, quantitative CT
9. Management: weight exercises, eliminate smoking/alcohol, good nutrition.
10. Meds: biphosphonates (fosamax), pth stimulants, estrogen, vit d, Ca supplments
Osteoarthritis
1. Degeneration of the joint
2. Damage not caused by inflammation.
3. By age 40, 90% of population has some degeneration
4. Degen from: mechanical factors, genetic factors, biochemical factors
5. RF: female, obese, repetitive motion, genetics
6. CM: loss of cartilage w/ osteophyte formation, weight bearing joints, Bouchard's and Heberden's nodes, increased pain with activity, swelling, crepitus, decreased ROM, instability.
Progression of Degeneration in Osteoarthritis
1. Bones changes in weight bearing joints.
2. Cartilage damage
3. Synovitis
4. Osteophyte formation
Management of Osteoarthritis
1. Prevention
2. Pharmalogical: NSAIDs/ acetaminophen, duloxetine (cymbalta), cortisone or lubrication injection into joints, vit D and Ca supplement
3. Joint replacement
4. PT/OT
5. Transcutaneous electrical nerve stimulation (TENS)
6. Weight bearing exercise
7. Weight loss
RA vs OA
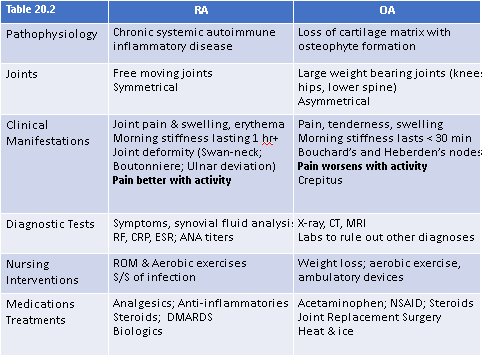
1. OA = big joints, unilateral, not deformative.
2. RA = little joints, bilateral, deformative, autoimmune
Rheumatoid Arthritis
1. Degeneration of joint due to autoimmune response
2. Damage caused by inflammation
3. Stages: Immune attack, swelling begins, joint deformity, fused joint.
4. RF: autoimmune disease, female, genetics
5. CM: bilateral degeneration of small joints, synovial membrane, chronic joint pain, swelling, erythema, morning stiffness, decreased rom,
6. Positive C-reactive protein
7. Positive ESR labs
8. Tx: nsaids, DMARDS, steroids, antidepressants, heat, exercise, splints, braces, good sleep and nutrition
Orthopedic Surgery
1. to repair or stabilize broken bones
2. To replace dislocated joints
3. To stabilize weak or degenerated joints
4. Can include addition of hardware, internal or external
Trauma Care ortho surgery
1. Pain management
2. stabilize the bone or joint
3. Waiting for swelling to go down
4. List of meds, diagnoses, and allergies
5. Contact person
6. Emotional support
Cast Care
1. Do not: get cast wet or dirty, pull out padding, place objects inside cast, apply powder, use hair dryer to dry cast
2. Do: cover cast for bathing, watch for swelling, keep elevated, monitor circulation.
Brace Care
1. Designed to support an already surgically stabilized fracture, used as reminder
2. Do: ensure on correctly, keep clean, check skin underneath, wear as long as recommended.
Hip Precautions
1. Prevent hyperflexion of hip no more than 70 degrees.
2. Prevent falls
3. Elevated toilet seat
4. Keep legs straight and separated (abducted)
Knee surgery
1. Risk for: infection, blood clots, nerve damage.
2. No pillow under the knee
3. Encourage ROM
4. Pain managmenet/ good neuro assessment
Risks of Orthopedic Surgeries
1. Blood clots
2. Fat embolisms
3. infection
4. New fracture
5. dislocation
6. nerve damage
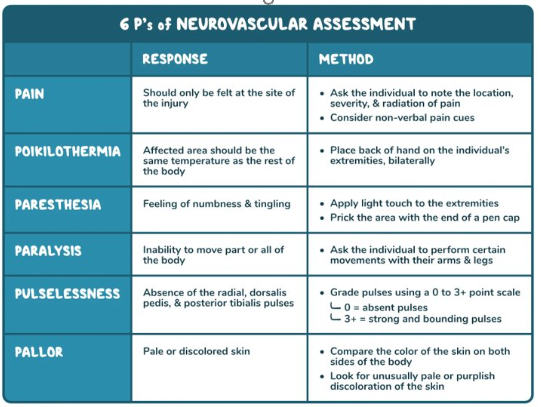
6 P's of Neurovascular assessment
PT vs OT
1. PT: lower extremity and mobility
2. OT: upper extremity and living (doing things)
Orthopedic surgery watch for
1. Wound infection
2. Venus thromboembolism
3. Fat embolism syndrome
4. Atelectasis
5. Dislocation
Amputation
1. Reasons: trauma, nonhealing wounds (diabetes), deformities, PVD, osteomyelitis
Amputation: Pre-Op or Traumatic
1. Priority assessments or cues: bleeding, hemodynamic status, emotional state, oxygenation.
2. Priority labs: arteriogram, venogram, and doppler, CBC
3. Priority interventions: control bleeding, compression bandages surgical TQ, prevent infection, control pain
4. Post OP: infection control, wound care, pain management, pt/ot
Path to a prosthetic
1. healing time
2. residual limb shaping
3. pain management
4. muscle strengthen
5. contracture prevention / ROM
Types of Shock
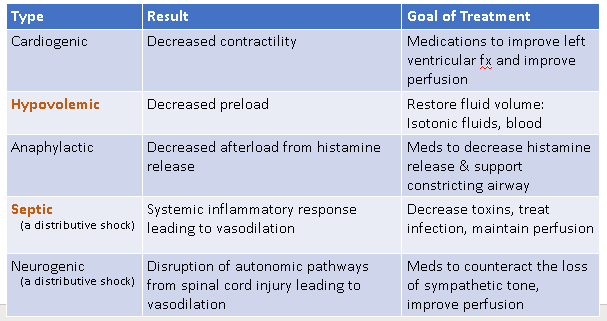
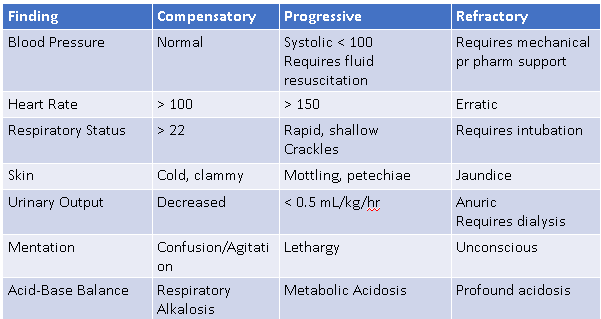
4 Stages of Shock
1. Initial stage: no noticeable changes, changes to cellular level
2. Compensatory: neural SNS, endocrine RAAS; increase glucose, chemical- tachypnea
3. Progressive: failure of compensatory mechanisms
4. Refractory: irreversible cell death
Shock Symptoms
1. Increased HR
2. Increased RR
3. Increased glucose
4. Decreased urine
5. Decreased blood flow to internal organs
6. Cool skin
Shock Stages Findings
Hypovolemic Shock
1. major loss of blood or fluid
2. trauma, burns, pancreatitis, gi bleed, excessive sweating, abnormal diuresis (diabetes insipidus), vomiting, diarrhea.
Diabetes Inspidius
A disorder of salt and water metabolism marked by intense thirst and heavy urination.
Diabetes insipidus occurs when the body can't regulate how it handles fluids. The condition is caused by a hormonal abnormality and isn't related to diabetes.
In addition to extreme thirst and heavy urination, other symptoms may include getting up at night to urinate or bed-wetting.
Pathophysiology of Hypovolemic Shock
1. Hypovolemia -> venous return declines -> declined preload -> low cardiac output -> hypotension -> perfusion failure -> tissue hypoxia -> organ disfunction -> multiorgan failure
Clinical manifestations of Hypovolemic shock
1. Hypotension
2. tachycardia
3. dry oral membranes
4. decreased tissue perfusion
5. Labs: BUN UP, sodium down, urine gravity up, HCT/HGB up,
Treatment of Hypovolemic shock
1. Maximize oxygen delivery
2. Restore intravascular volume, fluid resuscitation, blood transfusion
3. Control further blood loss with TQs, surgical intervention
4. Treat underlying cause
5. Support hypotension, vasoconstrictors/vasopressors
6. Monitor electrolytes and lactate
Sepsis
1. Body's extreme response to infection, spreads from original location to other tissues and can progress to organ failure then death.
2. Sepsis is curable if caught early
Stages of Sepsis
1. Stage 1 (compensatory): systemic inflammatory response, SOB, tachycardiac, extreme pain, clammy sweaty skin, clot formation.
2. Stage 2 (progressive): severe sepsis, organ dysfunction begins, confusion/disorientation, decreased urine output, abnormal cardiac function, respiratory distress.
3. Stage 3 (refectory): septic shock, dangerous drop in BP, skin pale, mottled.
Sepsis TIME
1. Temperature- higher or lower than normal
2. Infection - may have s/s of infection
3. Mental decline- confused, sleepy, difficult to rouse
4. Extremely ill - severe pain, discomfort, shortness of breath
Septic Shock and Labs and Meds
1. Labs: high or low WBC, positive blood cultures, Elevated urine gravity, Hyperglycemia
2. Meds for Sepsis: antibiotics, vasopressors, iv fluids, corticosteroids, insulin, pain meds
Treatment of sepsis
1. Prevention
2. early recognition: changes in VS
3. Send cultures: blood, urine, sputum
4. aggressively treating infection w/ antibiotics
5. aggressive fluid replacement (usually crystalloids)
6. support BP (vasopressors - norepinephrine, dopamine)
7. Monitor labs: lactate levels, glucose, WBC
8. support resp and cardiac function.
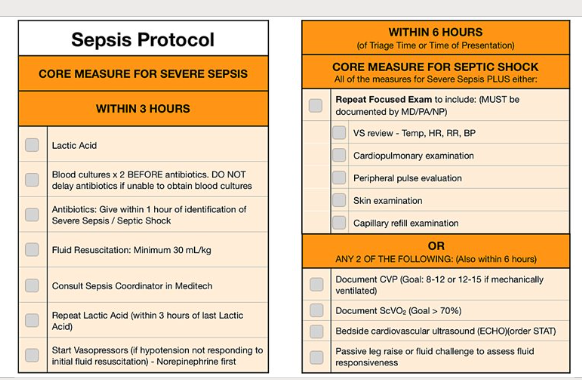
Sepsis Protocol
Post sepsis syndrome
1. affects up to 50% of sepsis survivors, physical/psychological long term effects
2. Fatigue, sleep disturbances, sob, disabling muscle joint pain, repeat infections, poor appetite, reduced organ function, hallucinations, panic attacks, depression, memory loss, difficulty concentrating.