-
post partum period
Transition period for woman and new born and family physiologically and psychologically (birth of placenta to 6 weeks)
-
Puerperium
the time from the delivery of the placenta through approximately the first 6 weeks after the delivery
-
Involution of the uterus
contraction of muscle fibers; catabolism; regeneration of uterine epithelium.
-
Lochia
Vaginal discharge after childbirth
-
Ruba
Occurs right after child birth lasting 3-4 days bright red dark red with small clots similar to a period flow
-
Serosa
Lasts 3-10 days after child birth pinkish brown consistency with a lighter flow
-
Alba
Lasts 10-14 days after child birth Whitish yellow consistency little to no blood
-
Urinary System Adaptations
Increase Glomular filtration rate increased renal flow
-
Voiding sensation is affected by
1.Perennial laceration
2. Hematomas
3. decreased bladder Tone
4. Generalized swelling and bruising of perineum and tissues surrounding the meatus
-
What are some causes of Post Party Diuresis ?
1. Large amount of Iv fluid given during labor
2. decreased Antidiuretic effect of oxytocin
3. Build up and retention of extra fluids during pregnancy
4. Decreased production of Aldosterone
-
What is Postpartum diuresis ?
Excessive production of urine after child birth .
-
Lactation Hormones
progesterone, estrogen , prolactin
-
The New born sucking on breast stimulates the pituitary gland to release
prolactin / oxytocin
-
how is breast engorgement Relieved ?
frequent emptying warm showers cold compress between feedings
-
Normal Lactating breast should
Be soft and the mother should be comfortable
-
Engorgement
Painful swelling of breast tissue as a result of rapid increase in milk production and venous congestion causing interstitial tissue edema; impaired milk flow results in accumulation of milk in breasts; most often occurs between the third and fifth postpartum days
-
ovulation postpartum
interplay of hormones estrogen prolactin oxytocin
-
Non lactating women get menstrual cycle
7-9 weeks after birth
-
Breast feeding frequency and duration last
2-18 months
-
Factors influencing attachment
-environmental circumstances-newborn health-quality of nursing care
-
mood disorders
-baby blues-post-partum depression-post-partum psychosis
-
Risk Factors for Postpartum Infection
-Operative procedure (forceps, cesarean birth, vacuum extraction)
-History of diabetes, including gestational-onset diabetes
-Prolonged labor (more than 24 hours)
-Use of indwelling urinary catheter
-Anemia (hemoglobin <10.5 mg/dL)
-Multiple vaginal examinations during labor
-Prolonged rupture of membranes (>24 hours)
-Manual extraction of placenta
-Compromised immune system (HIV-positive)
-
Risk Factors for Postpartum Hemorrhage
• Precipitous labor (less than 3 hours)
• Uterine atony
• Placenta previa or abruptio placenta
• Labor induction or augmentation
• Operative procedures (vacuum extraction, forceps, cesarean birth)
• Retained placental fragments
• Prolonged third stage of labor (more than 30 minutes)
• Multiparity, more than three births closely spaced
• Uterine overdistention (large infant, twins, hydramnios)
-
POST PARTUM DANGER SIGNS
• Fever >100.4°F (38°C)
• Foul-smelling lochia or an unexpected change in color or amount
• Large blood clots or bleeding that saturates a peripad in an hour
• Severe headaches
• Visual changes, such as blurred vision or spots
• Calf pain with dorsiflexion of the foot
• Swelling, redness, or discharge at the episiotomy, epidural, or abdominal sites
• Dysuria, burning, or incomplete emptying of the bladder
• Shortness of breath or difficulty breathing without exertion
• Depression or extreme mood swings
-
baby blues
a mild postpartum mood disorder that goes away on its own lasts 4-5 days resolve 10 days
-
postpartum depression
a mood disorder characterized by feelings of sadness and the loss of pleasure in normal activities that can occur shortly after giving birth Lasting longer
-
post partum depression may lead to
poor bonding alienation from loved ones violent thoughts and actions
-
Carboprost
treats postpartum uterine Hemorrhage works by contracting the uterus
-
REVA ROBINS THREE PHASES
taking in phase taking hold phase letting go phase
-
Taking in phase
-Time immediately after birth when the client needs others to meet her needs and relives the birth process first 24 hrs (range 1-2 days)
-Woman is passive – prefers nurse doing care and making decisions
-
Taking hold phase
-Second phase characterized by dependent and independent maternal behavior (lasts 10 days to several weeks)
-strong interest in caring for baby
-insecurity if ability to care for baby
-
Letting go phase
-reestablishes relationships with other people
-accepts role of motherhood not fantasy
-
Four stages of becoming a mother
Commitment, attachment to unborn baby, preparation for delivery and motherhood during pregnancyAcquaintance/attachment to infant, learning to care for infant, and physical restoration 2 to 6 weeks postbirthMoving toward a new normalAchievement of a maternal identity through redefining self to incorporate motherhood (around 4 months)
-
3 Stages of Role Development
ExpectationsRealityTransition to mastery
-
Engrossment: Partner Psychological Adaptation
strong attachment to baby increased self esteem visual awareness perception that the new born is perfect
-
Risk Factors for Postpartum Infection
Operative procedure (forceps, cesarean birth, vacuum extraction)
• History of diabetes, including gestational-onset diabetes
• Prolonged labor (more than 24 hours)
• Use of indwelling urinary catheter
• Anemia (hemoglobin <10.5 mg/dL)
• Multiple vaginal examinations during labor
• Prolonged rupture of membranes (>24 hours)
• Manual extraction of placenta
• Compromised immune system (HIV-positive)
-
Risk Factors for Postpartum Hemorrhage
• Precipitous labor (less than 3 hours)
• Uterine atony
• Placenta previa or abruptio placenta
• Labor induction or augmentation
• Operative procedures (vacuum extraction, forceps, cesarean birth)
• Retained placental fragments
• Prolonged third stage of labor (more than 30 minutes)
• Multiparity, more than three births closely spaced
• Uterine overdistention (large infant, twins, hydramnios)
-
POST PARTUM DANGER SIGNS
• Fever >100.4°F (38°C)
• Foul-smelling lochia or an unexpected change in color or amount
• Large blood clots or bleeding that saturates a peripad in an hour
• Severe headaches
• Visual changes, such as blurred vision or spots
• Calf pain with dorsiflexion of the foot
• Swelling, redness, or discharge at the episiotomy, epidural, or abdominal sites
• Dysuria, burning, or incomplete emptying of the bladder
• Shortness of breath or difficulty breathing without exertion
• Depression or extreme mood swings
-
BUBBLE – EE
Breast
Uterus
Bladder
Bowel
Lochia
Episiotomy/Perineum/
Epidural
Extremities
Emotional Status
-
POSTPARTUM ASSESSMENT
-During the first hour: every 15 minutes
-During the second hour: every 30 minutes
-During the first 24 hours: every 4 hours
-After 24 hours: every 8 hours
-
INVOLUTION
Uterus should be midline and firm
If boggy or off to side –
1)massage till firm,
2)express any clots
3)empty bladder
Encourage breastfeeding
-
NURSING INTERVENTIONS (involution)
Labor and Pregnancy History
Bladder status
Anesthesia
Involution is enhanced by:
Uncomplicated labor and birth
Complete expulsion of placenta or membranes,
Breastfeeding
Early ambulation
-
LOCHIA
-Uterus rids itself of debris remaining after birth through discharge called lochia
-Each day the amount of lochia should be less and lighter in color
-Women who have had a c/section have less lochia
-Continues for approximately 4-8 weeks post birth
-
Lochia changes:
Bright red at birth
Rubra – dark red
Serosa – pink
Alba – white
Clear
If blood collects and forms clots within uterus, fundus arises and becomes boggy (uterine atony)
-
LOCHIA SHOULD NOT
¡Have a foul odor
¡Have large clots
¡Saturate a pad in less than ½ hour
-
AFTERPAINS
-Contractions that occur after birth
-May be increased in pregnancies where uterus was -overdistended
-More increased in multiparas
-Afterpains are usually stronger during breastfeeding
-Pain should be assessed with other vital signs
-Provide comfort measures
-Consider premedicating
-Check for other reasons for pain
-
CERVIX AND VAGINA
-Cervix returns to prepregnant state by 6 weeks post partum
-Internal os closes by 2 weeks postpartum
-External os has permanent changed appearance
-
PERINEUM
Ask to woman to turn to side with her back towards you
Gently lift the upper buttock and inspect the perineum
Look for :
Ecchymosis
Hematoma
Erythema
Edema
Intactness of skin edges or sutures
Drainage
Bleeding
Odor
-
using sitz bath
-Close clamp on tubing before filling bag with water
-Fill sitz bath basin and plastic bag with room-temperature water
-Place the filled basin on the toilet with the seat raised and the overflow opening facing toward the back of the toilet.
-Hang the filled plastic bag on a hook close to the toilet or an IV pole.
-Attach the tubing to the opening on the basin.
-Sit on the basin positioned on the toilet seat and release the clamp to allow warm water to irrigate the perineum.
-Remain sitting on the basin for approximately 15 to 20 minutes.
-Stand up and pat the perineum area dry. Apply a clean peripad.
-Tip the basin to remove any remaining water and flush the toilet.
-Wash the basin with warm water and soap, and dry it in the sink.
-Store basin and tubing in a clean, dry area until the next use.
-Wash hands with soap and water
-
Epiostomy care
-Kegel exercises. These exercises strengthen the muscles in the pelvic area. To do Kegel exercises, squeeze the muscles that you use to stop yourself from passing urine (peeing). Hold the muscles tight for 10 seconds and then release. Try to do this at least 10 times in a row, three times a day.
-Put a cold pack on your perineum. Use ice wrapped in a towel.
-Sit on a pillow or a donut-shaped cushion.
-Soak in a warm bath.
-
BLOOD VALUES
-Decreased blood volume and cardiac output
-B/P returns to pre- pregnancy by 6 weeks pp
-White blood cell count often elevated after birth for first 4 to 6 days
Activation of clotting factors predispose to thrombus formation – hemostatic system reaches nonpregnant state in 2to 3 weeks postpartum
-Risk of thromboembolism lasts 6 weeks
-
EXTREMITIES
Pregnancy is a hypercoagulable state
-Increased risk of venous thromboembolism ( VTE)
-Pulmonary Embolism ( PE)
-Deep Vein Thrombosis ( DVT
Factors that Increase Risk of Clot Formation
1.Stasis
2.Altered Coagulation
3.Localized Vascular damage
-
EXTREMITIES risk factors
•Anemia
•Diabetes mellitus
•Cigarette smoking
•Obesity
•Preeclampsia
•Hypertension
•Severe varicose veins
•Pregnancy
•Multiple pregnancies
•Cardiovascular disease
•Sickle cell disease
•Postpartum hemorrhage
•Oral contraceptive use
•Cesarean birth
•Severe infection
•Previous thromboembolic disease
•Multiparity
•Bed rest or immobility for 4 days or more
•Maternal age older than 35
-
URINARY ISSUES
-Difficulty feeling sensation to void
-Perineal lacerations
-Swelling and bruising
-Hematomas
-Decreased bladder tone
-Urinary system usually returns to normal by 6 weeks postpartum
-
BLADDER
-Patient may void up to 3,000 ml a day from 12 hours after birth for several days
-Single void may be 500 ml or more
-Important to check for full bladder
-Monitor for s/s of UTI
-Assess for bowel sound, flatus, undistended abdomen
-
GASTROINTESTINAL SYSTEM
•May have decreased bowel tones for several days
•Decreased peristalsis
•Constipation
•Fear of having a bowel movement
•May not have spontaneous BM for 1-3 days after birth
•Assess for bowel sound, flatus, undistended abdomen
-
Vital Signs
•TEMPERATURE
• May be elevated to 100.4 because of dehydration or epidural first 24 hours
• Should return to normal after 24 hours
•PULSE
• 60-80 bpm after birth normal 1st week
•RESPIRATIONS
• WNL – 12- 20
•B/P
• Should be in patient’s normal range
-
MUSCULOSKELETAL SYSTEM
-Joints return to normal by 6 to 8 weeks postpartum
-Diastasis recti responds to exercise
-
INTEGUMENTARY SYSTEM
•Linea nigra, melasma, areola darkening fade
•Hair loss
•Striae gravidarum fade to silver
•Diaphoresis
-
RESPIRATORY SYSTEM
•Diaphragm returns to normal position
•Abdominal organs resume their nonpregnant position
•Returns to normal prepregnant state 1 to 3 weeks
-
ENDOCRINE
•Estrogen and Progesterone changes with delivery of placenta
•Non Breastfeeding Estrogen increases 2 weeks postpartum
•Prolactin levels decline within 2 weeks for the woman who is not breastfeeding, but remain elevated for the lactating woman
-
BREAST EXAM
•Checks breasts for symmetry
•Engorgement
•Erythema
•Check Nipples
•Filling, Full, Engorged
•Colostrum, Foremilk
-
LACTATION
•Lactation is the secretion of milk by the breasts. It is thought to be brought about by the interaction of progesterone, estrogen, prolactin, and oxytocin.
•Breast milk typically appears within 4 to 5 days after childbirth.
•First 2 days postpartum breast soft non tender
-
TEACHING FOR BREASTFEEDING
•Select a quiet corner or room where you won’t be disturbed.
•Use a rocking chair to soothe both you and your infant.
•Take long, slow deep breaths to relax before nursing.
•Drink water while breastfeeding to replenish body fluids.
•Listen to soothing music while breastfeeding.
•Cuddle and caress the infant while feeding.
•Set out extra cloth diapers within reach to use as burping cloths.
•Allow sufficient time to enjoy each other in an unhurried atmosphere.
•Involve other family members in all aspects of the infant’s care from the start.
•Contact a local La Leche League or a nursing mothers’ group for continued guidance and support
-
BREASTFEEDING POSITIONS
•Cradle hold position: The mother’s arm cradles the baby close to the breast with their abdomens against each other and supports the baby’s head and neck with the mother’s other hand supporting the breast.
•Cross- cradle hold position: Similar to the cradle hold, but the baby is supported with the mother’s opposite arm
•Football/clutch hold position: (cesarean, large breast, small/premature, or mum with twins) Potion baby at your side in a semi sitting position facing mom with baby’s legs under mum’s arm. Use pillow to bring the baby up to the level of your nipple.
•Side lying position: (middle of night) Position baby on your side facing you, tummy to tummy. mouth in line with nipple.
-
BREASTMILK SAFETY
1.Wash your hands before expressing milk or handling breast milk.
2.Find a quiet, clean place to express milk if returned to workplace. Use clean containers to store expressed milk. Use sealed and chilled milk within 24 hours.
3.Discard any milk that has been refrigerated for more than 24 hours.
4.Use any frozen expressed milk within 3 months.
5.Do not use microwave ovens to warm chilled milk.
6.Discard any used milk; never refreeze it.
-
TYPES OF FORMULAS
•Cow milk protein based formulas: This formula contains cows milk that has been altered to resemble to breast milk. The formula has a lot of nutrients within it that is easier for babies to digest. The only downfall however is some babies are allergic to protein in now milk so that would require a different type of formula such as protein or soy milk etc.
•Soy Based Formulas: This formula contains protein found in soybeans. This is especially great for babies who wish to exclude animal proteins in his/her diet. It is a great option for babies who intolerant and/or allergic to cow milk formula and lactose which is a natural carbohydrate found in cow milk.
•Protein Hydrolysate Formulas: This formula contains protein that has been broken down (hydrolyzed) into tiny sizes than are those in cow milk and soybean formula. Protein hydrolysate formula are meant for babies who have a protein allergy.
-
ENGORGEMENT
•Heat or Cold
•Cabbage Leaf Compress
•Breast Massage
•Hand expression of milk
•Anti-inflammatory medication
-
NON BREASTFEEDING
•Wear a supportive snug bra 24 hours daily
•May take 5-7 for milk to be suppressed
•Take mild analgesics
•Don’t stimulate breasts
•Drink fluids
•Reduce salt intake
•Ice packs inside bra - change q 30
-
MASTITIS
•Infection or inflammation
•Lactating or engorged breasts
•Management
• Heat
• Rest
• Empty Breast
Antibiotics as needed
-
OVULATION AND RETURN OF MENSTRUATION
•Nonlactating women, menstruation may resume as early as 7 to 9 weeks after giving birth, but the majority take up to 3 months
•Lactating women, menstruation return depends on frequency of breastfeeding and length of time
•Ovulation can return before menstruation
-
SEXUAL ACTIVITY
•Sleep deprivation, vaginal dryness, and lack of time together may impact resumption of sexual activity
•Usually sexual intercourse is resumed once episiotomy has healed and bright red lochia has stopped (about 3 to 6 weeks)
•Breastfeeding mother may have leakage of milk from nipples with sexual arousal
•Contraceptive choices
• Barrier with spermicide
• Combined Oral Contraceptives should not be used until 6 weeks pp and until lactation is established
-
Factors associated with the health care facility or birthing unit can also hinder attachment
These include:
•Separation of infant and parents immediately after birth and for long periods during the day.
•Policies that discourage unwrapping and exploring the infant.
•Intensive care environment, restrictive visiting policies.
•Staff indifference or lack of support for parent’s caretaking attempts and abilities.
-
PP exercise
•Abdominal Breathing
•Head Lift
•Modified Sit-Ups
•Double Knee Roll
•Pelvic Tilt
-
RH IMMUNE GLOBULIN
•For prevention of Rh Isoimmunization
•If mother is Rh negative she receives an IM injection of Rhogam at 28 weeks gestation
• and
•If mother is Rh negative and has a spontaneous birth, abortion ( Spontaneous or Operative, Bleeding in Preganancy, Ectopic, Trauma, External Version, Amniocentisis, Chorionic Villus Sampling , Placenta Previa or Abruption she receives an IM injection of Rhogam within 72 hours of event to prevent sensitization of the mother
•The standard dose of RhoGAM is 300 mcg given intramuscularly,
-
RH ISOIMMUNIZATION
•If Rh sensitization occurs fetus can develop Hydrops
• Fetalis
• Fetal Edema
• CHF
• Jaundice ( icterus gravis)
• Neurological Damage ( Kernicterus)
Erthroblastosis Fetalsis ( severe hemolytic syndrome)
-
ENCOURAGE REST
•Nap when the infant is sleeping
•Reduce participation in outside activities, and limit the number of visitors
•Determine the infant’s sleep–wake cycles and attempt to increase wakeful periods during the day so the baby sleeps for longer periods at night.
•Eat a balanced diet to promote healing and to increase energy levels.
•Share household tasks to conserve energy.
•Ask the partner or other family members to provide infant care during the night periodically so that mothers can get an uninterrupted night of sleep if they are not breastfeeding.
•Review the family’s daily routine, and try to “cluster” activities to conserve energy and promote res
-
Newborn vital signs
Respiration: 30-60 (avg 40)
Temp-Rectal: 90-99.5
Axillary: 97.6-98.6
HR: 110-160
BP-Systolic: 60-80
Diastolic: 40-50
-
Respiratory adaptions to birth
◦Initiation of respirations: adjusting from a fluid filled intrauterine environment to gaseous extrauterine environment
◦Role of surfactant: surface tension redacting lipoprotein that prevents alveolar collapse
◦Respirations: 30-60 breaths per minute; irregular, shallow, unlabored; short periods of apnea (<15 secs); symmetrical chest movements
-
Cardiovascular changes (fetal to neonate)
1.Increased aortic pressure and decreased venous pressure
2.Increased systemic pressure and decreased pulmonary artery pressure
3.Closure of foramen ovale
4.Closure of the ductus arteriousus
5.Closure of ductus venous
-
Characteristics of Cardiac Function
◦Blood Pressure:
◦varies with birth weight, gestational age, & changes in blood volume
◦average mean is 5 to 55 mm Hg, full term 3 kg newborn. (70/45 to 50/30 mm Hg)
◦Crying may elevate both systolic & diastolic blood pressure
◦Heart Murmurs: 90% of murmurs are transient, not abnormalities
◦Caused by turbulent blood flow through: narrow opening, across an abnormal valve, stenosed valve
◦Atrial or ventricle septal defect (ASD or VSD)
◦Some serious murmurs not recognized for a few weeks until patent ductus arteriosus closes
-
Renal system changes
◦Limited ability to concentrate urine until about 3 months of age (urine has a low specific gravity)
◦6-8 voids a day is normal
◦Low glomerular filtration rate and limited excretion and conservation capability: affect newborn’s ability to excrete salt, water loads, and drugs
-
G I changes
◦Intestines sterile at birth
◦Capacity of newborn stomach varies
◦Newborns prone to regurgitation, vomiting, reflux
◦Meconium formed during fetal life
◦Term newborns pass meconium first 24-48 hours after birth
◦Thick , tarry black or dark green
-
Immune System changes
◦Activates after birth
◦Immature – so s/s of infection may be subtle
◦Fever is not reliable indication of infection
◦Hypothermia or irregular temperature status more reliable sign of infection!!!
◦Infants active passive acquired immunity in utero from mothers response to illness or immunization
-
Hepatic changes
◦At birth infant as iron stores for 4-6 months
◦At birth infants is cut off from maternal glucose
-
Newborn stools
◦Meconium, then transitional stool, then milk stool
◦Breast-fed newborns: yellow-gold, loose, stringy to pasty, sour smelling
◦Formula-fed newborns: yellow, yellow-green, loose, pasty, or formed, unpleasant order
-
Neutral Thermal Environment-Newborn
◦Infant stressed by change from warm, moist environment of uterus to dry, drafty environment of delivery room and nursery
◦Neutral thermal environment needed to prevent need for increased oxygen and calories
-
Heat loss for newborns
◦Thin skin; with the blood vessels close to the surface
◦Lack of shivering ability; limited reserve of metabolic substrates (glucose, glycogen, fat)
◦Limited use of voluntary muscle activity
◦Large body surface area relative to body weight
◦Lack of subcutaneous fat; little ability to conserve heat by changing position
-
THERMOREGULATION
◦Dry immediately with warmed blankets beginning with the head
◦ Skin to skin contact with mother or partner
◦Radiant warmer
◦Stocking cap
◦ Heat regulation is second most critical to the newborn’s survival
◦Hypothermia is a common and dangerous problem
-
Mechanisms of heat exchange
◦Conduction: transfer of heat from object to object when the two objects are in direct contact with each other
◦Convection: flow of heat from body surface to cooler surrounding air or air circulating over a body surface/ also from drafts
◦Evaporation(most common): loss of heat when liquid is converted to a vapor
◦Radiation: loss of body heat to cooler solid surfaces in proximity but not in direct contact (cold weight)
-
Consequences of Cold Stress
◦Increased Metabolic Use of Calories
• Failure to gain weight or weight loss
◦Increased Oxygen Consumption
• May lead to hypoxia, acidosis and respiratory distress
◦Rapid Depletion of Glycogen
• Resulting in hypoglycemia
If allowed to continue the baby may develop shock and disseminated intravascular coagulation (DIC) leading ultimately to death.
-
Behavioral patterns of newborns
First period of reactivity
•Birth to 30 minutes to 2hours after birth
•Newborn is alert, moving, may appear hungry
Period of decreased responsiveness
•30-120mins old
•Period of sleep or decreased activity
Second period of reactivity
•2-8hrs old
•Newborn awakens and shows an interest in stimuli
-
PRIORITIES OF CARE OF THE NEWBORN
•Establish and maintain an airway and respirations
•Provide warmth and prevent hypothermia
•Provide a safe environment and routine preventive measures
•Promote maternal-infant attachment
-
Initial newborn assessment
•Apgar scores
•Length/ Weight
•Vital signs
•Physical maturity
Neuromuscular maturity
-
Signs indicating a problem during Assessment
•Signs indicating a problem
•Nasal flaring, chest retractions
•Grunting on exhalation, labored breathing
•Generalized cyanosis, flaccid body posture
•Abnormal breath sounds, abnormal respiratory rates
•Abnormal heart rates, abnormal newborn size
-
Newborn Classification Neonatal Mortality Risk Chart
•Preterm: <36.6 (completed) weeks
•Late preterm: 34–36.6 weeks (common respiratory problems)
•Term: 38–41 (completed) weeks
•Postterm: >42 weeks
•Large-for-gestational-age (LGA) (larger than expected)
•Appropriate-for-gestational-age (AGA)
•Small-for-gestational-age (SGA)
-
Apgar scoring system
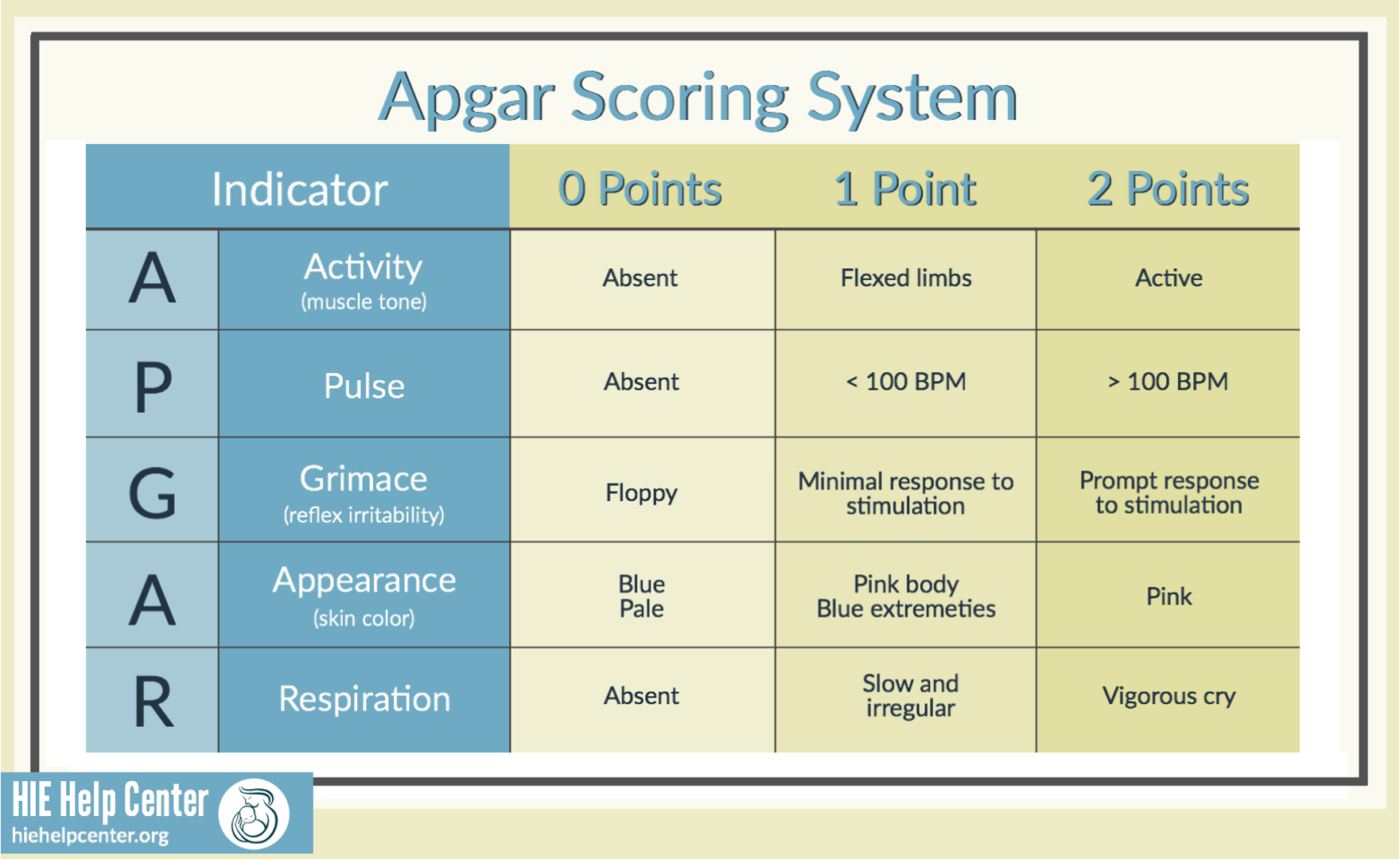
Activity
Pulse
Grimace
Appearance
Respiration
(do 1st and 5th minute of life)
8-10 = an uncompromised or distress free
4-7 = moderately compromised or asphyxiated
0-3 = severely compromised or asphyxiated
Less than 7- do it again in 10 minutes
-
Nurse’s Responsibility (newborn)
•Initiate Neonatal Resuscitation if necessary
•Assign Apgar score ( if pediatrician not present)
•ID bracelets for baby & mother
•Footprints of baby & mother’s finger print
•Vital signs of baby (30 minutes X4)
•Assist with skin/skin & breastfeeding
•Administer Vitamin K (IM)
•Apply antibiotic eye ointment (or drops)
-
•Physical assessment of newborn (abbreviated version)
–Size & contours of head, including fontanels, relationship to body
–Assess breathing for flaring of nares, grunting or retractions of chest
–Posture & tone of body
–Symmetry of face, including eyes, ears, nose,
–Arms & legs equal in length, digits on hands & feet.
–Any visual abnormalities
–Obtain height & weight of newborn
-
Normal Newborn Appearance
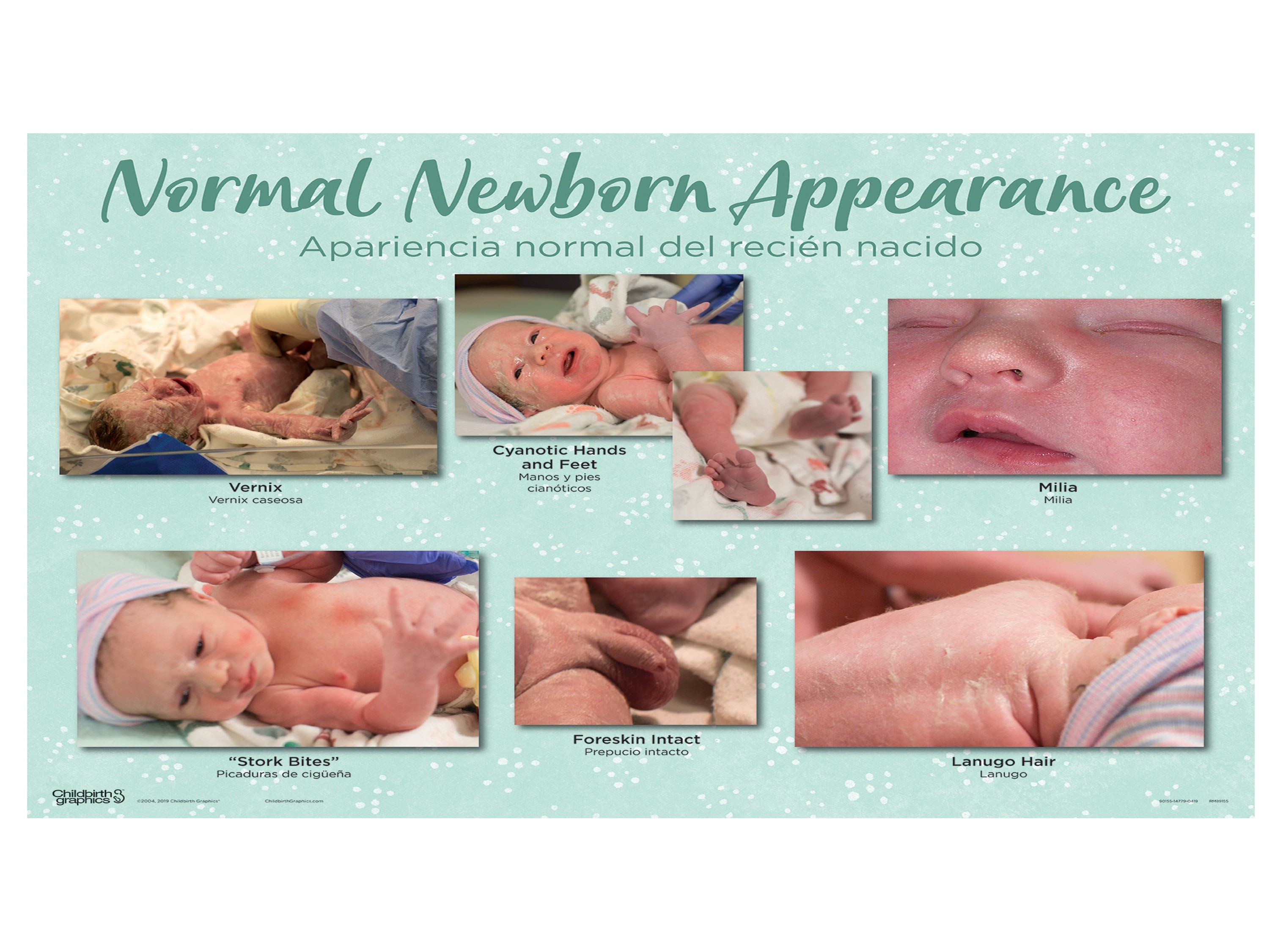
Vernix- protection when baby in utero (not every baby)
Cyanotic hand and feet
Milia- little sebaceous glands
Stork Bites
Foreskin intact
Lanugo hair
Mongolian spots
Erythema toxicum
Harlequin sign
Nevus flammeus
Nevus vasculosus

