-
difference between and resident and transient microbes.
Transient- occupy body for short period. Skin surface
Resident- more permanently. Fluctuate with health, age, hormone, drugs
Microbial antagonism- microbes against intruder microbes
Deep of epidermis, gland, follicle
Staphylococcus, corynebacterium, propionibacterium, yeast
-
microbs who colonize on human vs infection
Resident microbiota/indigenous microflora/ commensal
colonized on outer surface without penetrating sterile tissue
Infection- microbe penetrated sterile tissue and multiplied. Microbe is now a pathogen
Infectious disease- cause damage to tissue/organ
-
Sterile body part vs resident population
Sterile
heart, ovaries, bones, lung, muscle
Resident microbs
skin, vagina,GI tract, respitatory
-
when human being to acquire microbiota and things that change microbiota
When water breaks
Baby:First solid food, teeth erupt,
Adults: puberty/menopause, long antibiotic, diet, disease
-
location and kinds of microbs on skin
on epidermis, gland follicle, not dermis
•Staphylococcus, Streptococcus, Pseudomonas, Micrococcus, Propionibacterium, corynebacterium
Fungi: Candida, malassezia
Arthropods: demodex mite
-
location and kinds of microbs on GI tract(mouth, L intestine, stomach/esophagus)
Mouth: Very diverse environment
Streptococcus
S. mutans & S. sanguinis = cavities sticky dextran slime
Large intestine
Obligate anaerobes (no air), Clostridium, bacteroides, bifidobacterium
Coliform (gram - , Facultative anaerobes that ferment lactose) E. coli, enterobacter, citrobacter in small #
Little microbiota in Esophagus/stomach/small intestine- digestive enzyme and violent swallowing
-
location and kinds of microbs on respiratory
Pharynx- oral streptococci.
Nasal entrance- Staphylococcus aureus
in mucous membrane of nasopharynx- Neisseria
None in bronchi and lung
-
location and kinds of microbs on female genitourinary track female/male
Kidney, ureter is sterile through urine
Female- Vagina and urethra
Urethra- nonhemolytic streptococci, staphylococci,
diphtheroid, escherichia, gardnerellla, corynebacteria
Vagina shift to acid producing lactobacilli
Males- outer urethra
-
true pathogens versus opportunistic pathogens and ex based on virulence
•True pathogens (primary): Capable of making a person with a functioning immune system
flu, plague, cold, malaria, rabies
(high virulence factor)
Opportunistic pathogens: Only capable of causing disease in a weakened host or they are established somewhere not natural to them
Old age, organ transplant, chemotherapy
Pseudomonas, candida albican (
(low virulence factor)
Virulence- ability of microb to establish into host and cause damage
-
steps in the development of an infection
Finding a portal of entry,- skin GI
attaching firmly- fimbriae, capsules
surviving host defense- avoid phagocytosis
cause of damage and disease- direct(enzyme) and indirect (host response is inappropriate)
existing host- respiratory tract, fecal
-
different portals of entry into the human body and ex
Streptococcus and staphylococcus, S. aureus s can enter multiple ways, some need specific
Conjunctiva/ broken skin- chlamydia trachomatis, staphylococcus
Gastrointestinal- salmonella, shigella, hept A
Respiratory- mumps, streptococcal sore throat
Urogenital- UTI, STD, STI
Pregnancy through placenta- STORCH(syphilis, toxoplasmosis, (HIV,hepB), rubella, cytomegalovirus, herpes) common for infants
-
Exogenous vs Endogenous
Exogenous- microb enter from environment
Endogenous- microb already in body
-
infectious dose
Infectious Dose: The number of individual microbes needed to initiate infection
low- locally and immediately; high need to travel through body
salmonella need high ID to cause infection (acid kills)
-
how microbes attach to their host cells what what helps
adhesion: fimbriae, capsules, spike, hooks etc.
Virus- specialized receptors.
Can’t bind= non infectious
Virulence factor- microbe characteristics that help(antiphagocytic, enzyme, toxin)
Antiphagocytic factor- how pathogen avoid/kill phagocytes.
Ex. strep and staph produce leukocidins that are toxic to WBC.
-
Antiphagocytic factor of some microbs
pathogen avoid/kill phagocytes.
Ex. strep and staph produce leukocidins that are toxic to WBC.
Thick capsules (streptococcus pneumoniae) difficult for WBCs to engulf
Some pathogens can live inside WBC (Listeria, HIV)
-
differentiate exotoxins and endotoxins
Exotoxin- toxin secreted by living bacteria
Toxic in small doses, specific cell type
die in heat
Eg. Hemolysins found in Staphylococcus and Streptococcus cause lysis of red blood cells
Endotoxins- toxin released after damaged/lysed
•Toxic only in high doses, not specific
toxin on lipopolysaccharide (LPS) layer of the gram -cell wall
does not stimulate antibody
fever, shock, pain…
-
Exoenzyme
bacteria produce this to disrupts the structure of tissue
-
what occurs during incubation period, prodromal stage, invasion, convalescent period
incubation period- portal of entry to first symptom ~2-30 days
prodromal stage- discomfort, headache
Invasion - multiplies at high level, greatest toxicity, well established (fever, cough)
convalescent period- recover
-
types of infection (local, systemic, focal, mixed) and ex
Local: Infection is restricted to a specific location(boils, skin infection, wart)
Systemic: Infection spreads throughout body(viral: measles, aids, chickenpox)(bacterial:brucellosis, anthrax, syphilis)(rabies)
Focal: Infection is local but effects are systemic (often due to toxins)(tuberculosis, streptococcal pharyngitis) (toxemia- localized infection but toxin carried by blood to target)
Mixed infection- infection contains more than one microb (dental caries, wound infection)
-
primary vs secondary infections
Primary: First of multiple infections
Secondary: Only occurs because primary infection weakens the host defenses
Eg. Chicken pox then gets Staphylococcus aureus
-
acute vs chronic infections.
Acute infection- severe but short lived effects
Chronic infection- persist over long period of time
-
signs and symptoms
Signs are objective evidence- fever, bacteria in urine, increase heart rate (more precise)
Symptoms are subjective felt by patient - chills, itching,
-
portals of exit ex
cough/sneezing, epithelial, diarrhea, semen, insect bite, remove blood
-
•Latency
recurrent disease)- herpes
-
Sequelae
(long term damage•Long covid
-
•Reservoir: v •Source
•Reservoir: Primary habitat of a microbe (cow)
•only reservoir of Shigella = feces, soil and water
•Source:l source of infection acquired ex.Contaminated burger
-
epidemiology
tudy of frequency and distribution of disese in human population
Centers for Disease Control (CDC)
World Health Organization
MMWR (Morbidity Mortality Weekly Report
National Notifiable Disease Surveillance System
Occurrence of disease is tracked using two measures, Prevalence and Incidence
-
asymptomatic, chronic, convalescent and passive carriers.
Carriers-People who carry pathogens without showing overt signs of disease but may pass the pathogen to others.
Asymptomatic- carrier but no symptoms, can spread to others
Chronic- carry infection for a long time after recovery (herpes, hepatitis)
Convalescent- recovering patient without symptoms. But can still spread
passive carriers- transfer of infectious agent through contact(hospital)
-
mechanical and biological vectors.
Vector- animals that transmit pathogens
Biological vectors: Animals that participate/ multiply a pathogen, (malaria)
Mechanical vector: Animals that transport pathogen without being infected (E. coli, house fly)
-
Zoonotic infections
Infection normally found in animals but may be spread to humans (rabies)
Sick animals reported via sentinel animals
-
direct and indirect transmission
Direct infection: microb spread through skin or mucous membrane contact. Sex, kissing, sneezing or coughing on someone
Indirect spread: microb spread from host to object then another person.(Food, water, fomites, air)
-
communicable, contagious infections, non-communicable,
Communicable: May be spread person to person (colds, sexually transmitted disease)
Contagious: Easily spread person to person (measles, chicken pox) very communicable
Non-communicable: Not spread person to person (Tetanus)
-
vertical and horizontal transmission
Horizontal transmission: spread from Person to person
Vertical transmission: Parent to child (birth, nursing…)
-
oral-fecal route
indirect transmission, vehicle is contaminated with fecal and transported to mouth
-
•Droplet nuclei
pellets of mucus/ saliva from mouth and nose,extend the survivability of pathogens
-
Aerosols-
fine dust/moisture in air that contain live pathogen
-
how epidemiologists track cases
Surveillance- collecting, analyzing, reporting data on rate of occurrence, mortality, morbidity, and transmission of infection. Reportable and notifiable disease.
-
calculate prevalence and incidence
Prevalence: # case/ total # people
Incidence: # new case/ # at risk people
Mortality rate- # death
Morbidity- # people afflicted with disease
-
endemic, sporadic, epidemic or pandemic.
Endemic: Disease with a steady frequency in specific geographic
Sporadic: Occasional cases are seen at irregular intervals in different locations
Epidemic: New cases rise beyond what is expected
Pandemic: spread of epidemic across continents
-
epi-curve and different kinds
- # cases per # of days
Point source- infectious agent came from a single source(bbq)(1 peak)
•Common,source epidemic- all cases came from exposure to same course (restaurnat workers everytime he works)(multiple peak)
-Propagated epidemic- disease transmitted person to person. (gradual growth in spikes overtime)
-
Koch’s postulate
Used to link specific organisms to specific disease
Infection of unknown etiology is isolated, pure culture is created, inoculate of test animal, observe for disease, obtain pure culture. Microbes from inital and after disease must match for postulate to be satisfied
-
healthcare associated
Healthcare associated infection-disease acquired/developed in hospital
-
potable water why water quality is generally harder to maintain than
•Water needs to be potable: No pathogens, toxins, turbidity, odor, taste
Water pick up pathogens, snow, lake, therefore it is open
•Water is tested for indicator organisms like E. coli
•Presence of E. coli likely means other enteric organisms are present as well Giardia, Shigella, hepatitis A
-
indicator species and what a coliform is.
•Water is tested for indicator organisms like E. coli (intestinal resident of bird)
•Coliforms (Gram negative, facultative anaerobes that ferment lactose) are indicative of fecal contamination, but testing for E. coli is best
-
viable plate count,
Viable plate count- •Quick and easy but supplies minimal information, not sure bacteria
•Selective or differential media make the test more useful
-
•Membrane filtration:
Used for “clean” water where you wouldn’t expect to find many microbes
-
Most Probable Number (MPN) Method:
combination of microbiology and statistics to estimate the coliform count
•Presumed, Confirmed, Completed tests
•Takes three days
-
treatment of drinking water, from reservoir to tap.
1.Water is pumped from reservoir and screened.
3.Particles aggregate, settle, and Mg+ and Ca+ are reduced, pH is lowered.
8.Water is filtered through gravel, sand, anthracite.
9.Chlorine, corrosion inhibitors, fluoride (maybe) is added.
10.Storage.
-
three stages of sewage treatment.
•Primary: Trash is removed, smaller particles settle
•Secondary: Microbial decomposition of sludge
•Tertiary: Filtering, chlorination, disposal
-
treatment of sewage from home to dispersal of treated sewage
1.Water arrives and is screened to remove trash.
3.Solids settle and fat/oil/grease rises to top.
5.Solids and oils are decomposed, dried and disposed of in landfill.
6.Liquid waste is decomposed, allowed to settle, and chlorinated or treated with UV light.
7.Treated water may be allowed to seep into ground, pumped to ocean, or put for industrial use.
-
food infection and food intoxication.
•Food infection: The ingestion of live cells that grow within the intestine, undercooked food. Hard to track
•Typically involves diarrhea, vomiting
•Salmonella, E. coli, hepatitis A
2 weeks, hard to track
•Food intoxication: Illness is due to the ingestion of toxins in food
•Microbes may be dead but toxins remain
•Illness may occur throughout body
•Staphylococcus aureus, Clostridium botulinum
•Food intoxication more quickly than food infection
-
safe temperatures for cooking and storage
4°C or above 60°C
-
pasteurization
•Flash pasteurization 72°C for 15 seconds
•Ultra high temperature (UHT) pasteurization 138°C for 2 seconds
-
ionizing and non-ionizing radiation on food;
•Irradiation: UV (serilize surfaces)
Ionizing (penetrates meat, vegetables)pathogens
-
desiccation of food
•Addition of salts, acids, nitrates = Desiccation (keep things from growing) not reliable microbicidal method
-
Four steps to food safety
•Clean: Clean hands, surfaces and food
•Separate: Reduce cross-contamination
separate utensils on raw meat, poultry, seafood, eggs
•Cook: Temperatures high enough to kill cells (145°-165°F)
•Mixed food (casseroles, ground beef) requires higher temperatures than whole cuts
•Toxins may still be present after cooking
•Botulism toxin can be destroyed by boiling for a few minutes
•S. aureus enterotoxin impossible to destroy
•Chill: within 1-2 hours to prevent growth of microbes
-
three lines of host defense
First- physical(skin, coughing), chemical (Ph, lysozyme, digestive) genetic barrier, block portal of entry. Nonspecific
Second- inflammation and phagocytosis. (fever, interferon, complement)
Third-. Foreign substance encounter lymphocyte. Acquired immunity, very specific. Develops memory (B and T lymphocyte, antibodies)
-
physical, chemical and genetic aspects of the body’s defenses
•Physical: Skin desquamated, coughing, sneezing, ciliated epithelial cells
•Chemical: Stomach acid, skin ph,Tear has lysozyme hydrolyze peptidoglycan in cell wall of bacteria. Saliva has defensin are peptide that damage/ lyse cell
•Genetic: Humans are immune to many animal viruses.•Sickle cell disease protects against malaria•A genetic mutation against HIV
-
what cells in the body carry out immune surveillance
WBC or leukocyte survey tissue for pathogen with their receptors (patern recognition receptors PRR) (Toll like receptor TLR) feel for (pathogen associated molecular pattern PAMP) that are common on pathogen protein
-
four body compartment of immune system
1.Mononuclear phagocyte system (MPS)- network of fibers that allows white blood cells to pass through “solid” organs.
2.Extracellular fluid- (ECF) bathes cells in the body and allow communication
3.Bloodstream- 45% cells, in 55% liquid (plasma)
4.Lymphatic system- part of circulatory system. Lymph thansport through lymph node
-
makeup of blood
3.Bloodstream- 45% cells, in 55% liquid (plasma)
•Plasma: liquid clotted blood, produced in liver, 92% water, protein, clotting
•Serum: liquid that lacks cloting
•Red cells (erythrocytes) 45%: Transport oxygen and carbon dioxide
•White cells (leukocytes) 1%: Immune function
-
where is blood is produced as a fetus, newborn, and adult.
Hematopoiesis: in embryonic membrane, liver as a fetus, red bone marrow as an adult. Form from stem cell in bone barrow
-
•Neutrophils, structure, function, %
•Five lobed nucleus, Small purple horseshoe granules
•Primary phagocytes (numbers increase during bacterial infection)
•50%-90% of WBCs
-
•Eosinophils structure, function, %
•Bilobed nucleus orange granules
•Attack large eukaryotes (worm)
•1%-3% of WBCs
-
•Basophils, structure, function, %
•Constricted nucleus, 2 Large blue/black granules
•allergy
•0.5% of WBCs
-
•Mast cells structure, function, %
•Similar in form/function to basophils(•Constricted nucleus, 2 Large blue/black granules)
•allergy
•Non-motile
First defense
-
•Monocytes, shape, mature into, %
•largest size, Kidney-shaped nucleus
•Primary phagocytes
• present foreign molecules to lymphocytes
Mature into:
Macrophage-specific phagocytic function
Dendritic- early immune reaction
•Secretion of compound that control the immune system
•3% - 7% of WBCs
-
Lymphocytes
Nucleus fills most of cell
•20% - 35% of WBCs
•T lymphocytes (T cells): Cell mediated immunity- kill foreign cell directly
•B lymphocytes (B cells): Humoral (antibody mediated) immunity
active=plasma cell that produce antibodies to find to invaders
-
Natural killer
no specificity for single antigen
-
three primary roles of macrophages.
-specific and non specific phagocytic killing, housekeepers
-process and present foreign substance to lymphocyte
-secret compound that assist/ attract immune cells
-
three functions of the lymphatic system
•Return extracellular fluid to the circulatory system
•Drain fluid that from inflammatory response
•Provide an additional route through body for cells of the immune system
-
•Lymphatic fluid-
same as blood plasma except rbc(water, WBs, salt, protein, debris)
-
•Lymphatic vessels-
lymphatic capillaries thin walls and parallel cardiovascular system
. 1 way flow contraction of skeletal muscle to heart, high in hands, breast
swelling is from blockage from filarial worm and prevent going to circulatory system
-
between primary and secondary lymphoid organs.
•Primary Lymphoid Organs- origin
Bone marrow
Site of development for all blood cells
Thymus
•Site maturation of T lymphocytes, children need it for immunity
Release into secondary
•Secondary Lymphoid Organs- encounter microbs
•Spleen: protection against encapsulated bacteria like Streptococcus. filter blood
•Lymph nodes: Filter lymph to remove foreign particles and WBCs that have phagocytized pathogens, located especially in armpit, groin and neck
-
thymus
tip of sternum
•Site maturation of T lymphocytes, children need it for immunity
-
lymph nodes
Filter lymph to remove foreign particles and WBCs that have phagocytized pathogens, located especially in armpit, groin and neck
-
spleen
filter for blood
protection against encapsulated bacteria like Streptococcus. filter blood
-
MALT, BALT, and SALT
MALT- mucosal associated lymphoid tissue-bundle of lymphocyte(breast, tonsils, rapid response to microb entering)
Galt- lymphoid tissue- in appendix, peyer’s patch in small intesting
SALT- skin associated lymphoid tissue
BALT- bronchial associated lymphoid tissue
-
•Inflammation is marked by
•Rubor: Redness
•Calor: Heat
•Tumor: Swelling
•Dolor: Pain
-
purpose of inflammation
•Recruitment of cells and chemicals to the site of injury
•Repair of damage and removal of damaged tissue
•Preventing further invasion by microbes
-
what happens when infectious agent enters the body
Immediate Reactions
•Vasoconstriction
•mast cell release Cytokines, chemokines(affect white blood cell
•C Reactive protein (CRP)- early indicator of inflammation, attaches to PAMP. released by liver
•Vascular reactions
•Blood vessels dilate
•Repair of damage and removal of damaged tissue
•Preventing further invasion
Late stages
•Swelling (edema) due to fluids and neutrophils (pus)
•Dilute toxins
•Deliver WBCs, oxygen, and fibrin to the site of the injury
•Resolution
•Wound is ‘cleared by macrophages
•Swelling gradually decreases as fluid is drained by lymphatic system
•if bad infection: B and T lymphocytes may be engaged
-
chemotaxis and diapedesis.
•Chemotaxis: Movement of WBCs in response to chemicals
•This allows WBCs to travel through the bloodstream toward the site of an infection
•Diapedesis: The ability of WBCs to pass between the endothelial cells of the blood vessels and enter the tissues.
-
benefits of a fever
•Fever: Body temperature is regulated by the hypothalamus and temp may be reset by pyrogens.
•Inhibition of temperature sensitive microbes
•Reducing availability of iron from macrophages
•Increases metabolism/immune reaction
-
three primary activities of phagocytes
Survey tissue and target microb
Ingest materials
Extract antigens from foreign matter
-
happens to a cell that is phagocytized.
Professional” phagocytes
•Neutrophils (bacterial infection)
•NETS (neutrophil extracellular traps)- death of neutrophil,
•Monocyte become Macrophages and Dendritic : Circulating and fixed
•Phagocytes engulf foreign particles(PAMP) and then fuse phagosome (pocket) with a lysosome= phagolososome, destroying the contents
•Respiratory burst (oxidizing agents)- punch
•Hydrolytic enzymes- injure bacteria cell membrane
•DNase
•RNase
Proteases
-
what causes a cell to produce interferon,
.Cell dies from virus/ cancer but Prevent translation of viral protein by sending IFN to nearby cell
•alpha, by lymphocyte
-
three main steps of the complement system
-Membrane attack complex- kill pathogen directly
-Coating of pathogen with molecule that makes them attractive to phagocytes (opsonization
-Recruitment of inflammatory cell
-
memory and specificity of third line of defense
Third line of defense- long term protection. B T lymphocyte against antigens
Acquired immunity is specific- antibodies against chicken pox won’t work for other
Memory- lymphocyte can recall the first engagment
-
where you would find HLA (MHC) markers
•HLA human leukocyte antigen aka MHCs (major histocompatibility complex) molecules determinant of self
unique to each individual
•Class I HLA are found on all nucleated cells
•Class II HLAs are found on antigen presenting cells
•B cells
•Macrophages
•Dendritic cells
-
how antibody diversity is generated
•Each antibody is made of protein and consists of two (identical) heavy chains and two (identical) light chains variable region and a constant region
•Antibody genes are found in segments within the DNA of the cell randomly combined
•Variable
•Diversity
•Joining
Constant
-
typical antibody
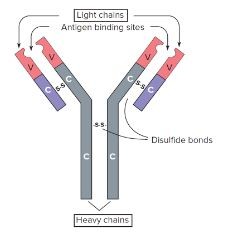
image
-
clonal selection and clonal expansion
•Clonal selection involves the receptor on a cell recognizing an antigen
•Clonal expansion involves the selected clone multiplying and differentiating into cells that can fight back against a pathogen
-
differences between T cells an B cells
T cells
Mature in thymus, high #, T cell receptors, require MHC, produce helper and cytotoxic t cell, kill foreign cell
B cells- mature in bone marrow, low #, does not require MHC, produces plasma and memory, produce antibodies to target antigen
-
antigen and epitope
Antigen- Anything that can induce an immune response in the body
Good antigens are •Big•Complex
•Bad antigen are small and/or repetitive
Epitope- •An antibody only recognizes a this small portion of an antigen,
-
•Alloantigens: •Superantigens
•Alloantigens: Found on only some members of a population (blood type)
Superantigens Bacterial proteins that cause extreme stimulation of T-cells
-
cell mediated immunity.
Response of subset T cell for backup
TH1, TH2, TH17, Treg, Tc
-
how a T cell is selected
•Antigen Presenting Cells (APCs) engulf an antigen, display epitopes on the outside of the cell (dendritic cells, macrophages, or B cells)
•Selection of a specific T cell requires
1.Binding of the antigen/MHC complex on the APC by the T cell receptor
2.Release of IL-12 by the APC
Antigen presenting cell engulf microb. Combine with MHCII receptor to display to T cell (T receptor and CD4 that recognizes self/nonself). Release interlukin 12 activates T cell
-
CD4 T cell differentiates into
Depending on interleukin from APC, a bound T cell displaying CD4 receptors may differentiate into
•Memory T cell: Maintains memory of the antigen for many years
•T helper 1 cell (TH1): Increases stimulation of T cells. Tumor necrosis and macrophage (increase immune system)
•T helper 2 cell (TH2): Decreases T cell activity, stimulates B cells.increase antibody Drives B cell( decrease immune system)
•T helper 17 cell (TH17): Promotes inflammation and secrete IL-17 (increase immune system)
•T regulatory cell (T reg): Prevents overactive immune reaction. Development of immune tolerance (decrease immune)
T cytotoxic TC- destroy cancer
-
CD8 T cell differentiates into
•With a signal from APC and TH1 cells, T cells with CD8 receptors may differentiate into
•Memory CD8 cells
•Cytotoxic T cells (TC cells)
•TC cytotoxic cells destroy self cells that have become cancerous or infected with a virus by releasing perforins (destroy membranes) and granzymes (induce apoptosis, genetically programmed death of nucleus)
-
target of natural killer cells.
Natural killer target cancer and virus infected cell, lack antigen receptor, so not specific

