-
Anatomical position

Standard reference position --> dorsiflexion, palms forward, etc,
-
Pronated

down
-
Supinated

-
Median plane

divide left and right equally (in the middle)
-
Sagittal plane

anywhere but middle (flexion and extension)
-
Frontal plane
divide back and front (adduction and abduction)
-
Transverse plane
divide top and bottom (rotation)
-
Posterior vs. anterior
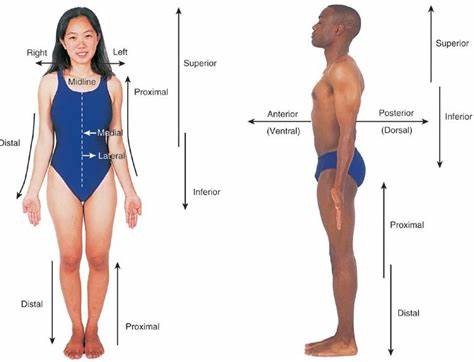
Posterior = behind
Anterior = in front
*divided by frontal plane
-
Superior vs. inferior
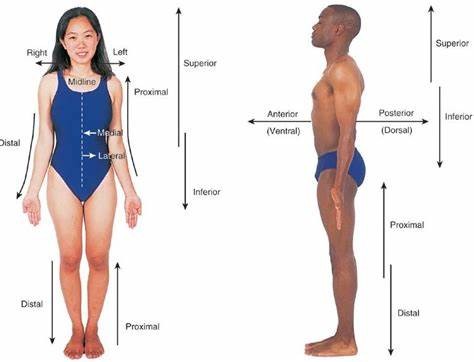
relative to something
*divided by transverse plane
-
Lateral vs. Medial
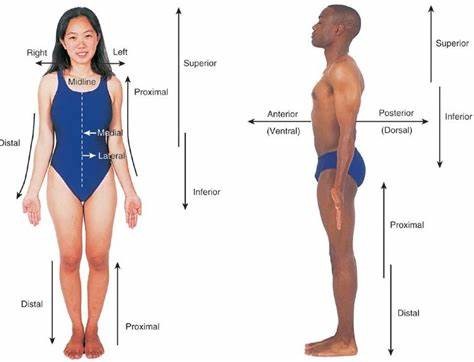
Medial = towards center
Lateral = away from center
*divided by median plane
-
Proximal vs. distal
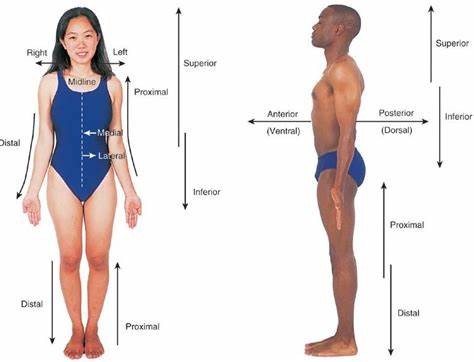
often related to limbs
- relative
-
Deep vs. superficial
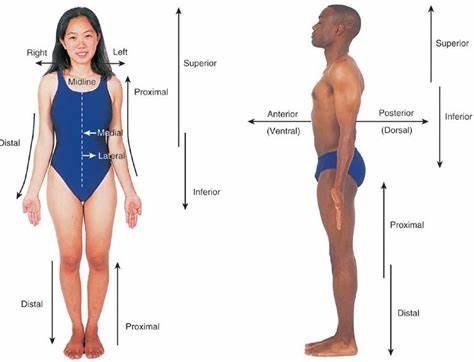
Inwards vs. outwards
-
Varus

"bow leg"
-
Valgus

"knock knee"
-
Sections of the spine
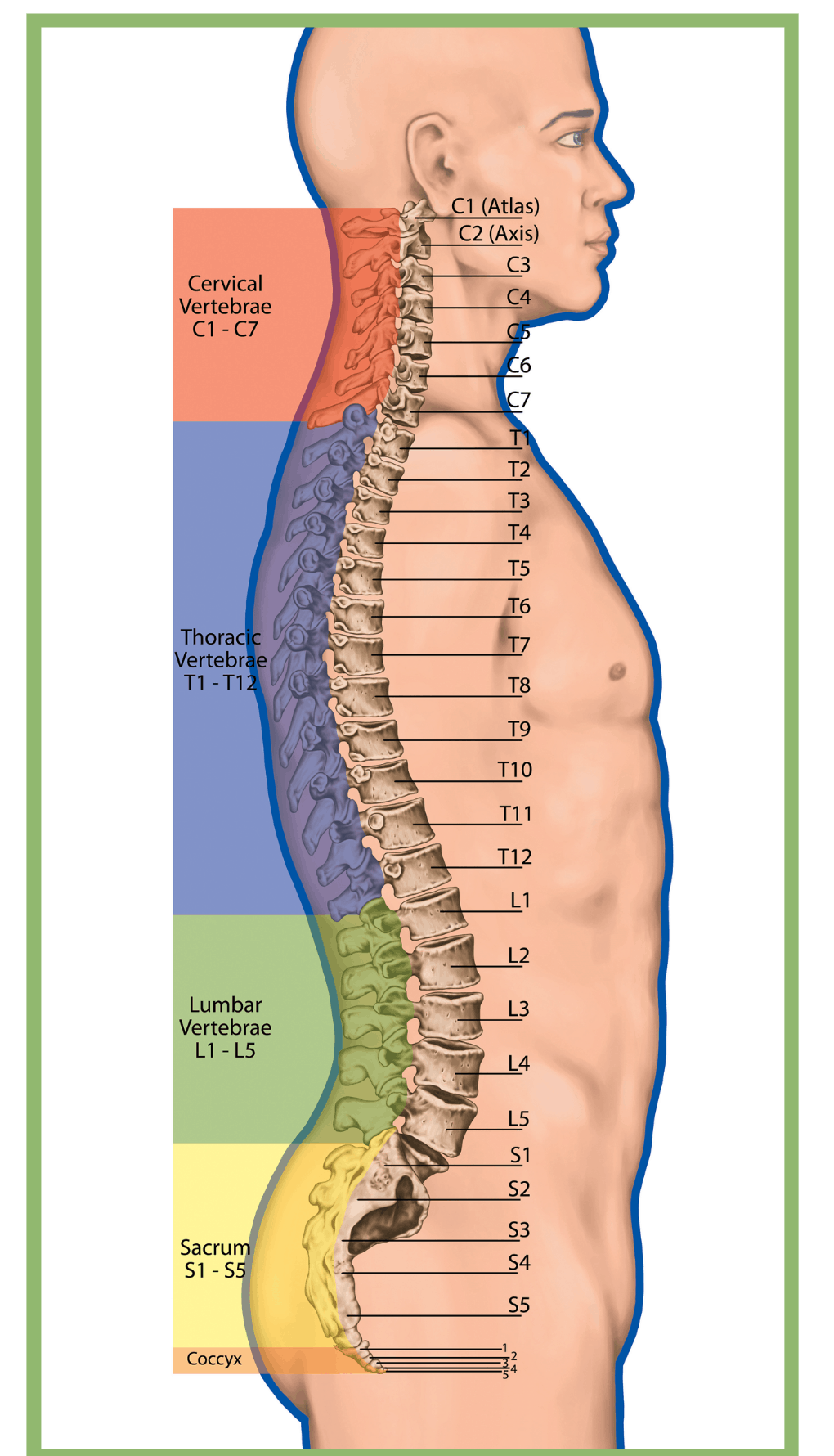
Lumbar - 5
Thoracic - 12
Cervical - 7
Sacral - 1
Coccyx - 1
-
Hyperlodosis

Excessive curve of the lumbar region
-
Kyphosis

a dorsqally excessive thoracic curve
-
What is the bending of a joint?

Flexion
-
Movement of body segment away from the midline

Abduction
-
Rotation

Occurs only in one plane (e.g. supination vs. pronation) e.g. head
-
Circumduction

multiple planes
-
Dorsiflexion

flexed foot
-
Plantarflexion

pointed foot
-
Inversion
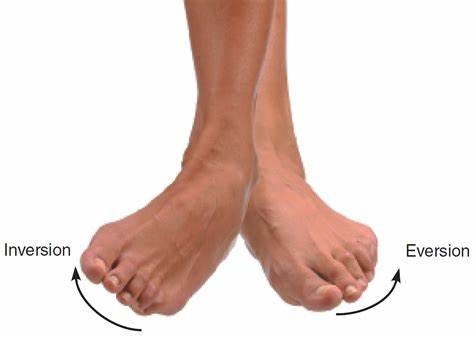
toward midline
-
Eversion
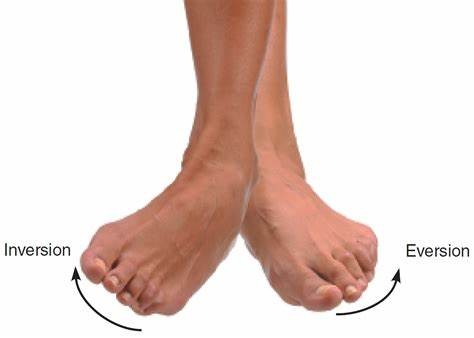
away from midline
-
Is eversion/inversion the same as supination/pronation?
NO
-
Supination
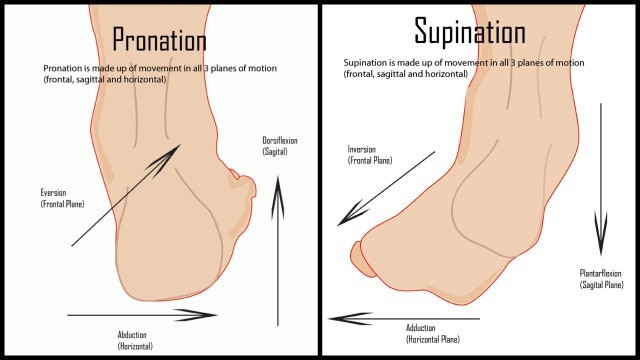
Combination of inversion (frontal plane), adduction (horizontal plane), plantarflexion (sagittal plane)
*Sickle foot
-
Pronation
Combination of eversion (frontal plane), abduction (horizontal plane), dorsiflexion (sagittal plane)
*Sickle foot
-
Bending of a joint
A. Circumduction
B. Flexion
C. Extension
D. Rotation
B
-
Movement of a body segment away from the midline.
A. Abduction
B. Adduction
C. Supination
D. Opposition
A
-
Circumduction vs. rotation
Rotation: a kind of movement around a single point, away or towards midline
Circumduction: combination of movement to make circular movement
-
Is circumduction only from ball and socket joints?

No, but mostly (e.g. ankle)
-
Sport and exercise medicine (SEM) team

AKA: integrated support team (IST)
• Multi-disciplinary team of sport science, sport medicine and sport performance professionals.
• The goal is to ensure that athletes are healthy, fit and mentally ready for optimal performance.
-
Who may be apart of an SEM team?
- Physician, Therapist, Strength and conditioning coach, Exercise physiologist, Sport psychologist, Biomechanist, Nutritionist, etc.
-
Role of physician on SEM team
Diagnosing the athletes condition and prescribing the treatment
-
Role of athletic therapist on SEM team
prevention, management, treatment and rehabilitation of injuries
-
Role of physiotherapist on SEM team
Rehabilitation of more serious injuries/rehabilitation after surgery
-
Role of strength and conditioning coach on SEM team
Establishing and maintaining a strength and conditioning program
-
Role of exercise physiologist on SEM team
exercise prescription and testing
-
Role of sport psychologist on SEM team
helping athletes to cope with competitive fears, mental skills, preparing for RTS, how to handle emotions after setbacks, etc.
-
Role of biomechanist on SEM team
biomechanical assessments to enhance performance and prevent injury
-
Role of nutritionist on SEM team
education of athletes and support staff on how nutrition can enhance performance, recovery and health
-
What do SEM specialist must follow?
the scope of practice and standard of care.
-
Scope of practice
describes the services that a qualified healthcare professional is deemed competent to perform and permitted to undertake
– in keeping with the terms of their professional license.
-
Standard of care
Medical treatment guideline.
It specifies appropriate treatment based on scientific evidence and collaboration between medical and/or psychological professionals involved in the treatment of a given condition.
-
What is one of the most important components of SEM team?
Teamwork!
Communication between athlete and coach is extremely important
- 1st part of injury prevention lies with the coach
- coach is influenced by money, winning, etc. (must communicate well for mutual benefit)
-
What is the main goal of the SEM team?
SEM team should be there for the player's health and safety, but will also have a secondary goal of winning (NEVER at the athlete's expense)
-
What are some potential consequences of a lack of teamwork?
- Injury/re-injury
- reduced team or individual performance
- career loss (player and staff)
- interpersonal conflicts
- broken trust (athlete or coach)
- mental health issues
- set-back in rehab
- medical-legal
-
How would an SEM team look for a youth community club?
- much less people apart of the team: parents, student volunteers, coaches
- if injured = parent/athlete are in charge of themselves
- go to your own physio/doctor (money barriers)
- much less communication
-
On large/mature teams what benefits are there over youth?
- everyone is involved even in minor injuries
- intense injuries require much more mental health support through fear of returning/contact (that is possible)
-
Risk management in sports
The process of identifying risks (assessment, evaluation, control)
-
What are the 3 levels of risk management in sports?
1. Within/across sport: policies
2. Club/team level: train for risk prevention, equipment, training safety
3. Individual level: train to treat injuries
-
Risk assessment
is a process of measurement/estimation of risks to teams and athletes
-
Risk evaluation
involves determining the significance and acceptability of the risks
-
Risk control
is a process of identifying and implementing methods to control the risks and the consequences
-
How do we create an effective risk management system for a team?
- Injury surveillance
- Pre-season screening
- Monitor "at risk" team members
- Education
- Emergency Action Plan (EAP)
-
3 sections of everyday risk management
1. environment
2. equipment
3. athlete
-
Environment risk
- Field and surroundings
- Weather conditions
- EAP
-
Equipment risk
- protective equipment
- special training equipment
- first aid kit
- AED
-
Athlete risk
- medical issues
- previous injuries
- training history
- age
- sex
-
Risk compensation
describe a possible change in behavior in an athlete when they use protective equipment.
- The theory is that the person will assess the level of risk, and if they assess that the protective equipment reduces that risk, they will simply undertake more extreme activities to return the risk to a level they are comfortable with.
-
What to do when a medical problem arises?
- BE PREPARED!
- Emergency action plan is critical to facilitate a rapid and effect response to an emergency
- EAP should be prepared for practice and competition sites
-
Emergency medical plan basic layout
• Charge person (designated for action and can ask for help = most capable for injuries)
• Call person
• Cell phone - Important phone numbers (EMS, facilitymanager)
- Instructions to EMS how to reach thefacility
• First Aid Kit
• Automated External Defibrillator (AED)
• Ambulation aid (crutches, wheelchair, spineboard)
-
What are 3 important components of a first aid kit?
1. Communication sheet (plasticized)
• Important phone numbers
• Address of facility, access(directions/map)
• Nearest hospital directions
2. Information where AED, spine board, etc. are located
3. Player/staff medical profile cards
• Name and emergency contact information
• Medical profile (e.g.,asthma, allergies)
-
Activate EAP immediately, if the person...
• Is not breathing
• Does not have a pulse
• Is bleeding profusely
• Has impaired consciousness
• Has injured the back, neck or head
• Has a visible major trauma
• Cannot move arms or legs (or has lost feeling in them)
-
EAP layout for sudden cardiac arrest in sport
- EAP coordinator (charge person)
- Immediate AED access
- Trained personnel and annual practice
- Communication system
- Venue-specific EAP
- Medical timeout before each competition (between home and visiting team)
- Maintenance and monthly checks of AEDs (and document it! = prevent medical lawsuit)
-
Where are some AEDs located in KNES
Kinesiology A
• Main, Floor, across from Client Services Desk
• Main Floor, Aquatic Centre, next to change rooms
Kinesiology B
• Basement floor, Jack Simpson Gym entrance, next to emergency help phone
• 2nd floor, Jack Simpson Gym entrance, beside west elevator
• Main floor, near east main fire panel, MacEwan Hall link entrance
• Main floor, across from Sports Medicine
• Main floor, Racquet Centre, next to emergency help button
• Main floor, Human Performance Lab, outside B103
• 2nd floor, Human Performance Lab, outside B2225
-
SOAP
Method of documentation
- standardized way to store medical info.
-
What does SOAP stand for?
S (subjective information/history) = what player told you
O (objective information) = what you see, measurable
A (assessment) = what you conclude
P (plan) = what you do about it
*prevents medical lawsuits and helps SEM team
-
Why is sport injury prevention important?
- happier
- play more
- common in sports = best you can
- burden on the healthcare system
-
How many Canadians were hospitalized for sport injuries?
17, 655
-
Injuries in youth sport and recreation (stats/sport specifics)
• 1 in every 3 youth (aged 11-18) in Canada seek medical attention for a sport-related injury every year
• Lower extremity injuries (60%) and concussions (20%)
- LE injuries: 60% knee and ankle
- Concussions: Hockey and rugby over 50%
• Highest burden –> hockey (10%), basketball (10%), soccer (10%)
-
What are some consequences of sport injuries?
• Participation in S&R (decrease)
• School/work attendance (decrease)
• Physical activity (decrease)
• Overweight/obesity + other health implications (increase)
• Osteoarthritis (ankle & knee joint injuries) (increase)
• Psychosocial consequences
• Health care and indirect costs are high
-
Example of why an injury costs so much (ACL)
- Primary physio/doc appointment
- referral to sports med doc.
- imaging
- surgical consult
- pre-surgical physio
- surgery
- etc.
-
Long term consequences of ACL injury
• Sport mastery and associated opportunities (U Sports, NCAA, Pro)
- 65% with ACL reconstruction for a total rupture played at the same level 3 years after (*in professional male Soccer).
- In elite athletes, at 2 years after ACLR surgery, 79.6% were still playing, 51% at the same level
-
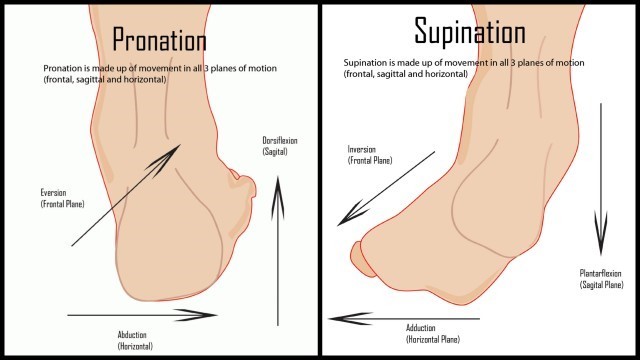
4 step model of injury prevention research
-
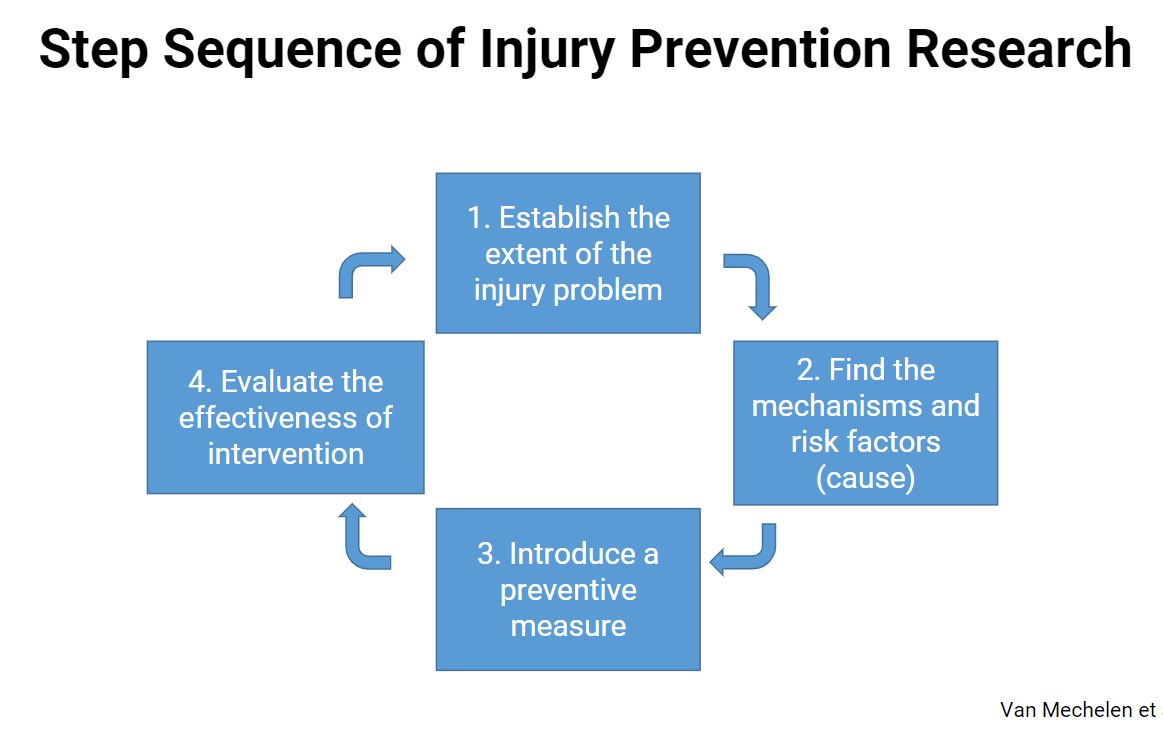
Intrinsic vs. extrinsic risk factors
Intrinsic: physical characteristics, skill level, risk level
Extrinsic: exposure, training, opponents, environment, equipment, etc.
-
Modifiable vs. non-modifiable risk factors
Modifiable risk factors
• E.g., equipment, training, body weight, flexibility
Non-modifiable risk factors
• E.g., weather, growth, age, sex, previous injury
-
Primary prevention
prevent injury before it even starts to occur (decrease injury chance)
-
Secondary prevention
detecting injury in early stages to prevent worsening
-
Tertiary prevention
arresting the progression of injury and addressing the issues
-
Evidence based sport injury prevention strategies
• Training strategies
• Rule modification
• Equipment
-
Strategies used in sport injury prevention studies
• Training programs to improve fitness/movement quality (n=64)
• New or modified sport equipment (n=33)
• New or modified rules (n=19)
• Education (n=14)
• Training programs to improve psychological and/or cognitive skills (n=6)
• Policy change (n=5)
• Multi-component/multiple interventions (n=14)
-
Most effective injury prevention strategies
Training programs to improve fitness/movement quality
-
What are the aims of neuromuscular training?
- prevent injury
- improve skills, coordination and control
- increase reaction speed and power
- increase joint stability
-
Neuromuscular training programs
- foundational movement
- warm up
- e.g. ACL is not fatigued based = neuromuscular
-
Effectiveness of neuromuscular training
Regular neuromuscular training (NMT) can reduce injury rates up to 70%
-
Why is technique important?
Tissue loading = don't want to overload joints/ligaments = want to use proper muscles
-
What characteristics do we see in an ACL injury
Valgus, external rotation
- includes meniscus, MCL injury
-
Critical teaching points of forward run with direction changes
- slow down in direction change
- bend knees for direction change
- avoid valgus position (use abductors/glutes)
-
Critical teaching points of squat
- knees above toes = joint safety
- straight spine
- heels on ground
- head directly forward
-
Critical teaching points of lunges
- 90 degree angle
- slow lower
- maintain straight line (no pronation, no valgus)
-
Training load and injury
Associations between injuries and:
• Rapid increases in training loads
• Insufficient practice vs. competition
• Too little variation in training load (monotony)
• Spikes in training load
*don't increase too quickly
*periodization = phases of training
-
What is internal vs. external training load?
External: work performed (quantifiable: intensity, duration, and frequency of exercise)
Internal: body's response (specific to the exercise type)
-
Structure specific training load
Sum of movement and structure specific loads (e.g. step, throw, jump, direction change)
- different between individuals
-
Why are their training load differences between individuals?
- strength capacity, injury history, biomechanics, size/weight
-
Sport specialization and injury
- Better to be multisport
- DONT early specialize
- increasing chance of injury
Athletes are classified as
• Low (score = 0-1)
• Moderate (score = 2), or : 2.61
• High (score = 3) specialization. :4.74
-
Sport Injury

• Tissue damage / derangement of normal physical function
• Generally due to external forces (transfer of kinetic energy)
• Sport injury can apply to all tissues - Vessels, muscle, ligament, cartilage, nerve, etc.
-
What are the 3 modes of sport injury onset?
Injury may result from a clear acute mechanism (acute injury), clear repetitive mechanism (overuse injury), or from a combination of both mechanism.
• Acute injury → Sudden onset (single event)
• Overuse injury → Gradual onset (repetitive)
• Overuse injury → Sudden onset (single event / repetitive)
-
Direct contact injury

• Contact with another athlete
• Contact with an object

