Anatomical position

Standard reference position --> dorsiflexion, palms forward, etc,
Pronated

down
Supinated

Median plane

divide left and right equally (in the middle)
Sagittal plane

anywhere but middle (flexion and extension)
Frontal plane
divide back and front (adduction and abduction)
Transverse plane
divide top and bottom (rotation)
Posterior vs. anterior
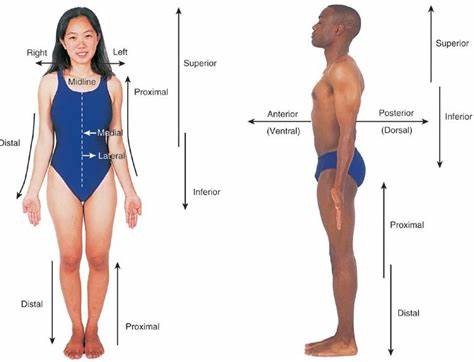
Posterior = behind
Anterior = in front
*divided by frontal plane
Superior vs. inferior
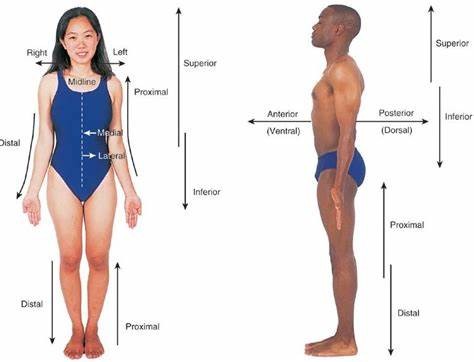
relative to something
*divided by transverse plane
Lateral vs. Medial
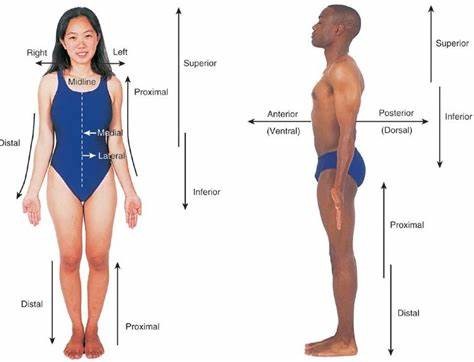
Medial = towards center
Lateral = away from center
*divided by median plane
Proximal vs. distal
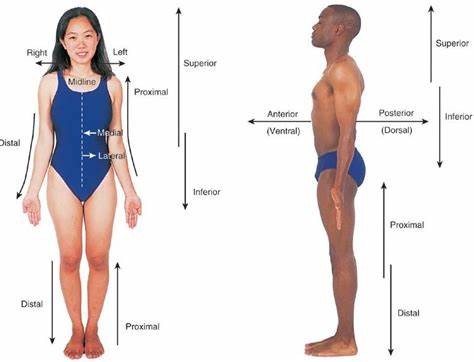
often related to limbs
- relative
Deep vs. superficial
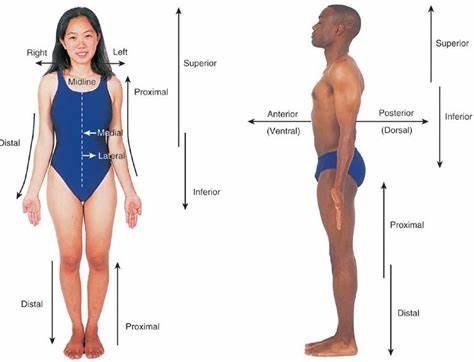
Inwards vs. outwards
Varus

"bow leg"
Valgus

"knock knee"
Sections of the spine
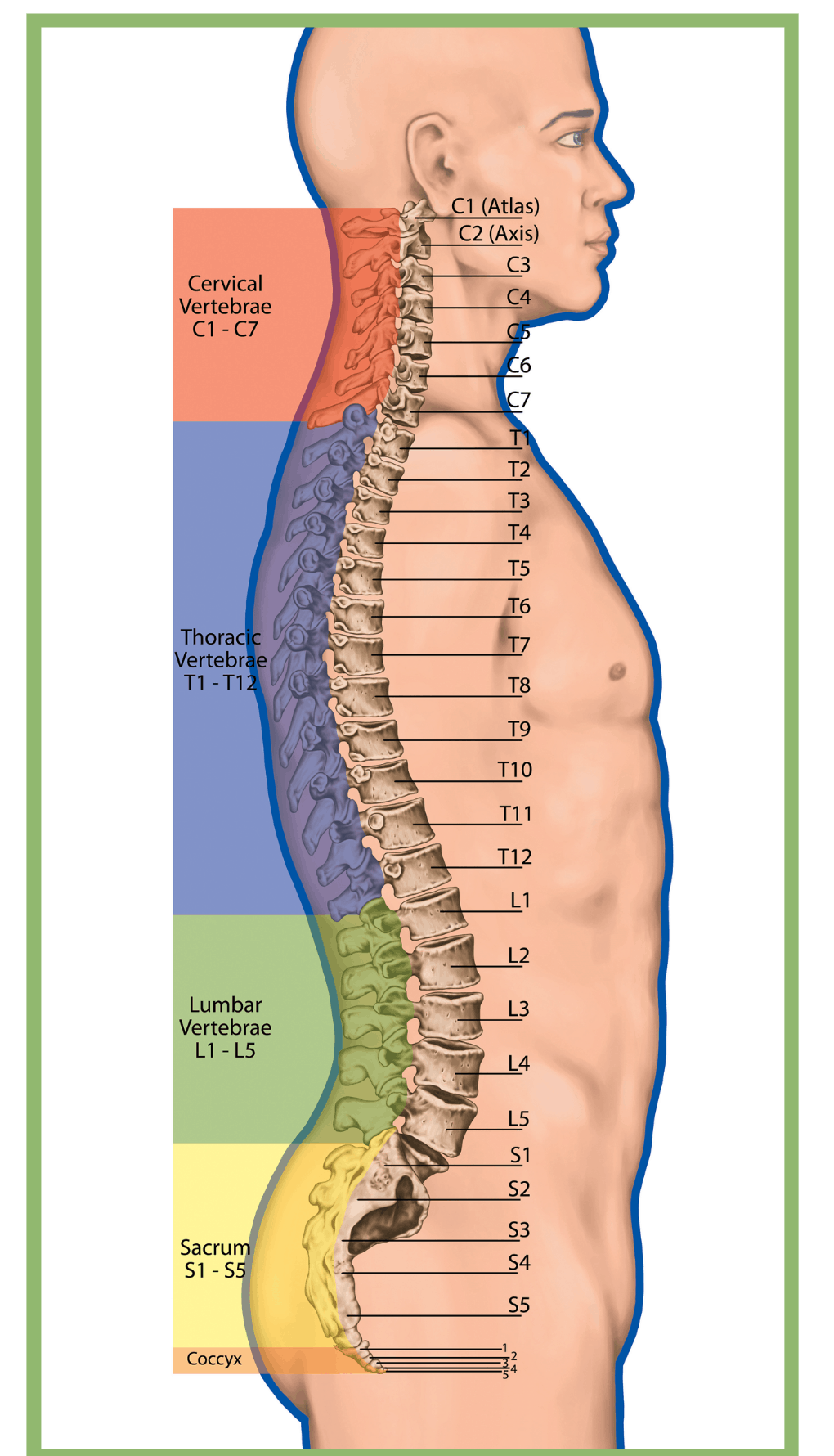
Lumbar - 5
Thoracic - 12
Cervical - 7
Sacral - 1
Coccyx - 1
Hyperlodosis

Excessive curve of the lumbar region
Kyphosis

a dorsqally excessive thoracic curve
What is the bending of a joint?

Flexion
Movement of body segment away from the midline

Abduction
Rotation

Occurs only in one plane (e.g. supination vs. pronation) e.g. head
Circumduction

multiple planes
Dorsiflexion

flexed foot
Plantarflexion

pointed foot
Inversion
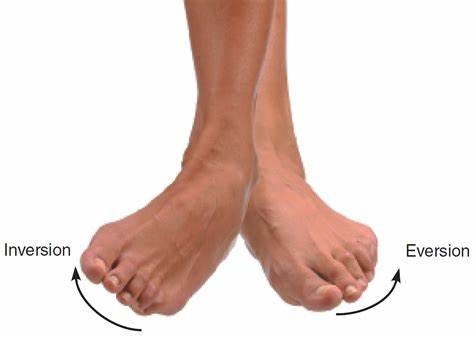
toward midline
Eversion
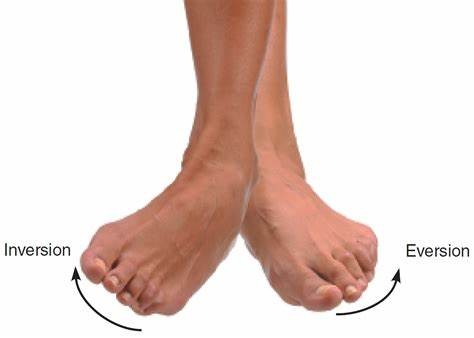
away from midline
Is eversion/inversion the same as supination/pronation?
NO
Supination
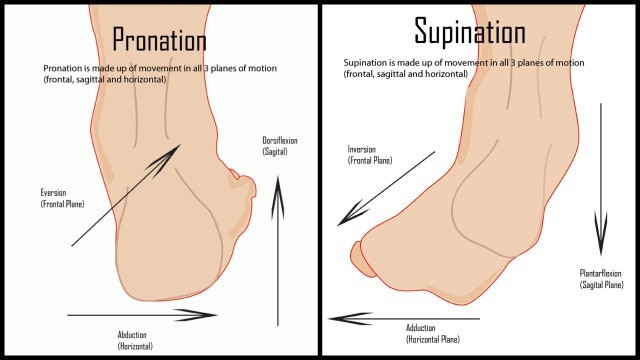
Combination of inversion (frontal plane), adduction (horizontal plane), plantarflexion (sagittal plane)
*Sickle foot
Pronation
Combination of eversion (frontal plane), abduction (horizontal plane), dorsiflexion (sagittal plane)
*Sickle foot
Bending of a joint
A. Circumduction
B. Flexion
C. Extension
D. Rotation
B
Movement of a body segment away from the midline.
A. Abduction
B. Adduction
C. Supination
D. Opposition
A
Circumduction vs. rotation
Rotation: a kind of movement around a single point, away or towards midline
Circumduction: combination of movement to make circular movement
Is circumduction only from ball and socket joints?

No, but mostly (e.g. ankle)
Sport and exercise medicine (SEM) team

AKA: integrated support team (IST)
• Multi-disciplinary team of sport science, sport medicine and sport performance professionals.
• The goal is to ensure that athletes are healthy, fit and mentally ready for optimal performance.
Who may be apart of an SEM team?
- Physician, Therapist, Strength and conditioning coach, Exercise physiologist, Sport psychologist, Biomechanist, Nutritionist, etc.
Role of physician on SEM team
Diagnosing the athletes condition and prescribing the treatment
Role of athletic therapist on SEM team
prevention, management, treatment and rehabilitation of injuries
Role of physiotherapist on SEM team
Rehabilitation of more serious injuries/rehabilitation after surgery
Role of strength and conditioning coach on SEM team
Establishing and maintaining a strength and conditioning program
Role of exercise physiologist on SEM team
exercise prescription and testing
Role of sport psychologist on SEM team
helping athletes to cope with competitive fears, mental skills, preparing for RTS, how to handle emotions after setbacks, etc.
Role of biomechanist on SEM team
biomechanical assessments to enhance performance and prevent injury
Role of nutritionist on SEM team
education of athletes and support staff on how nutrition can enhance performance, recovery and health
What do SEM specialist must follow?
the scope of practice and standard of care.
Scope of practice
describes the services that a qualified healthcare professional is deemed competent to perform and permitted to undertake
– in keeping with the terms of their professional license.
Standard of care
Medical treatment guideline.
It specifies appropriate treatment based on scientific evidence and collaboration between medical and/or psychological professionals involved in the treatment of a given condition.
What is one of the most important components of SEM team?
Teamwork!
Communication between athlete and coach is extremely important
- 1st part of injury prevention lies with the coach
- coach is influenced by money, winning, etc. (must communicate well for mutual benefit)
What is the main goal of the SEM team?
SEM team should be there for the player's health and safety, but will also have a secondary goal of winning (NEVER at the athlete's expense)
What are some potential consequences of a lack of teamwork?
- Injury/re-injury
- reduced team or individual performance
- career loss (player and staff)
- interpersonal conflicts
- broken trust (athlete or coach)
- mental health issues
- set-back in rehab
- medical-legal
How would an SEM team look for a youth community club?
- much less people apart of the team: parents, student volunteers, coaches
- if injured = parent/athlete are in charge of themselves
- go to your own physio/doctor (money barriers)
- much less communication
On large/mature teams what benefits are there over youth?
- everyone is involved even in minor injuries
- intense injuries require much more mental health support through fear of returning/contact (that is possible)
Risk management in sports
The process of identifying risks (assessment, evaluation, control)
What are the 3 levels of risk management in sports?
1. Within/across sport: policies
2. Club/team level: train for risk prevention, equipment, training safety
3. Individual level: train to treat injuries
Risk assessment
is a process of measurement/estimation of risks to teams and athletes
Risk evaluation
involves determining the significance and acceptability of the risks
Risk control
is a process of identifying and implementing methods to control the risks and the consequences
How do we create an effective risk management system for a team?
- Injury surveillance
- Pre-season screening
- Monitor "at risk" team members
- Education
- Emergency Action Plan (EAP)
3 sections of everyday risk management
1. environment
2. equipment
3. athlete
Environment risk
- Field and surroundings
- Weather conditions
- EAP
Equipment risk
- protective equipment
- special training equipment
- first aid kit
- AED
Athlete risk
- medical issues
- previous injuries
- training history
- age
- sex
Risk compensation
describe a possible change in behavior in an athlete when they use protective equipment.
- The theory is that the person will assess the level of risk, and if they assess that the protective equipment reduces that risk, they will simply undertake more extreme activities to return the risk to a level they are comfortable with.
What to do when a medical problem arises?
- BE PREPARED!
- Emergency action plan is critical to facilitate a rapid and effect response to an emergency
- EAP should be prepared for practice and competition sites
Emergency medical plan basic layout
• Charge person (designated for action and can ask for help = most capable for injuries)
• Call person
• Cell phone - Important phone numbers (EMS, facilitymanager)
- Instructions to EMS how to reach thefacility
• First Aid Kit
• Automated External Defibrillator (AED)
• Ambulation aid (crutches, wheelchair, spineboard)
What are 3 important components of a first aid kit?
1. Communication sheet (plasticized)
• Important phone numbers
• Address of facility, access(directions/map)
• Nearest hospital directions
2. Information where AED, spine board, etc. are located
3. Player/staff medical profile cards
• Name and emergency contact information
• Medical profile (e.g.,asthma, allergies)
Activate EAP immediately, if the person...
• Is not breathing
• Does not have a pulse
• Is bleeding profusely
• Has impaired consciousness
• Has injured the back, neck or head
• Has a visible major trauma
• Cannot move arms or legs (or has lost feeling in them)
EAP layout for sudden cardiac arrest in sport
- EAP coordinator (charge person)
- Immediate AED access
- Trained personnel and annual practice
- Communication system
- Venue-specific EAP
- Medical timeout before each competition (between home and visiting team)
- Maintenance and monthly checks of AEDs (and document it! = prevent medical lawsuit)
Where are some AEDs located in KNES
Kinesiology A
• Main, Floor, across from Client Services Desk
• Main Floor, Aquatic Centre, next to change rooms
Kinesiology B
• Basement floor, Jack Simpson Gym entrance, next to emergency help phone
• 2nd floor, Jack Simpson Gym entrance, beside west elevator
• Main floor, near east main fire panel, MacEwan Hall link entrance
• Main floor, across from Sports Medicine
• Main floor, Racquet Centre, next to emergency help button
• Main floor, Human Performance Lab, outside B103
• 2nd floor, Human Performance Lab, outside B2225
SOAP
Method of documentation
- standardized way to store medical info.
What does SOAP stand for?
S (subjective information/history) = what player told you
O (objective information) = what you see, measurable
A (assessment) = what you conclude
P (plan) = what you do about it
*prevents medical lawsuits and helps SEM team
Why is sport injury prevention important?
- happier
- play more
- common in sports = best you can
- burden on the healthcare system
How many Canadians were hospitalized for sport injuries?
17, 655
Injuries in youth sport and recreation (stats/sport specifics)
• 1 in every 3 youth (aged 11-18) in Canada seek medical attention for a sport-related injury every year
• Lower extremity injuries (60%) and concussions (20%)
- LE injuries: 60% knee and ankle
- Concussions: Hockey and rugby over 50%
• Highest burden –> hockey (10%), basketball (10%), soccer (10%)
What are some consequences of sport injuries?
• Participation in S&R (decrease)
• School/work attendance (decrease)
• Physical activity (decrease)
• Overweight/obesity + other health implications (increase)
• Osteoarthritis (ankle & knee joint injuries) (increase)
• Psychosocial consequences
• Health care and indirect costs are high
Example of why an injury costs so much (ACL)
- Primary physio/doc appointment
- referral to sports med doc.
- imaging
- surgical consult
- pre-surgical physio
- surgery
- etc.
Long term consequences of ACL injury
• Sport mastery and associated opportunities (U Sports, NCAA, Pro)
- 65% with ACL reconstruction for a total rupture played at the same level 3 years after (*in professional male Soccer).
- In elite athletes, at 2 years after ACLR surgery, 79.6% were still playing, 51% at the same level
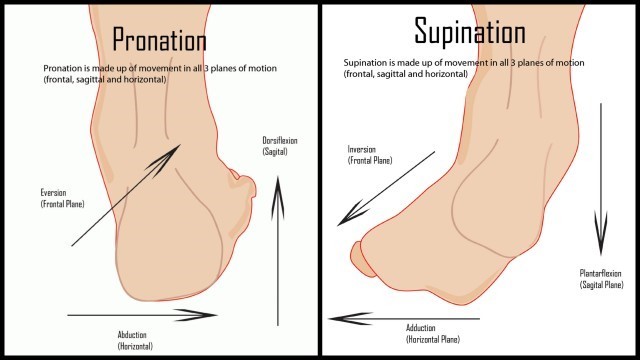
4 step model of injury prevention research
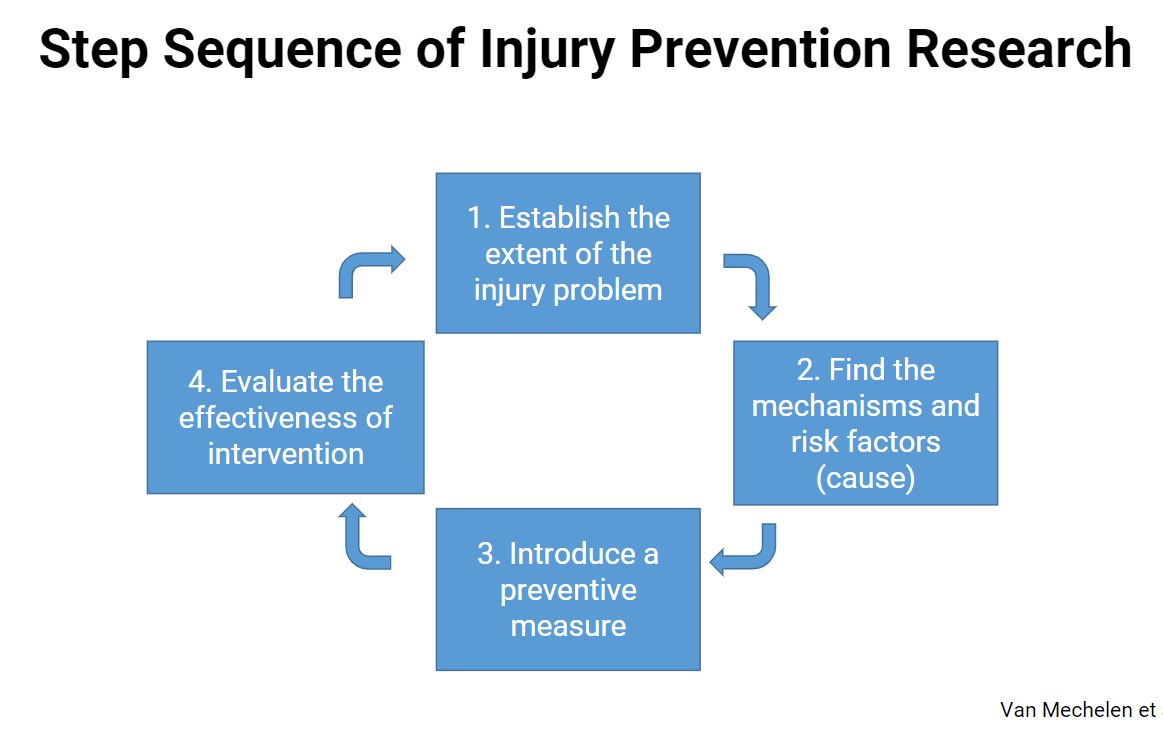
Intrinsic vs. extrinsic risk factors
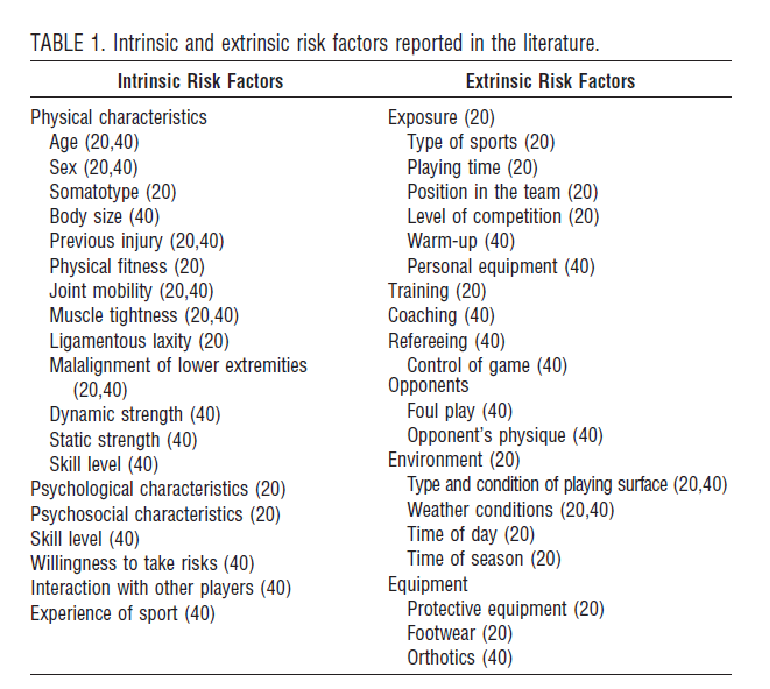
Intrinsic: physical characteristics, skill level, risk level
Extrinsic: exposure, training, opponents, environment, equipment, etc.
Modifiable vs. non-modifiable risk factors
Modifiable risk factors
• E.g., equipment, training, body weight, flexibility
Non-modifiable risk factors
• E.g., weather, growth, age, sex, previous injury
Primary prevention
prevent injury before it even starts to occur (decrease injury chance)
Secondary prevention
detecting injury in early stages to prevent worsening
Tertiary prevention
arresting the progression of injury and addressing the issues
Evidence based sport injury prevention strategies
• Training strategies
• Rule modification
• Equipment
Strategies used in sport injury prevention studies
• Training programs to improve fitness/movement quality (n=64)
• New or modified sport equipment (n=33)
• New or modified rules (n=19)
• Education (n=14)
• Training programs to improve psychological and/or cognitive skills (n=6)
• Policy change (n=5)
• Multi-component/multiple interventions (n=14)
Most effective injury prevention strategies
Training programs to improve fitness/movement quality
What are the aims of neuromuscular training?
- prevent injury
- improve skills, coordination and control
- increase reaction speed and power
- increase joint stability
Neuromuscular training programs
- foundational movement
- warm up
- e.g. ACL is not fatigued based = neuromuscular
Effectiveness of neuromuscular training
Regular neuromuscular training (NMT) can reduce injury rates up to 70%
Why is technique important?
Tissue loading = don't want to overload joints/ligaments = want to use proper muscles
What characteristics do we see in an ACL injury
Valgus, external rotation
- includes meniscus, MCL injury
Critical teaching points of forward run with direction changes
- slow down in direction change
- bend knees for direction change
- avoid valgus position (use abductors/glutes)
Critical teaching points of squat
- knees above toes = joint safety
- straight spine
- heels on ground
- head directly forward
Critical teaching points of lunges
- 90 degree angle
- slow lower
- maintain straight line (no pronation, no valgus)
Training load and injury
Associations between injuries and:
• Rapid increases in training loads
• Insufficient practice vs. competition
• Too little variation in training load (monotony)
• Spikes in training load
*don't increase too quickly
*periodization = phases of training
What is internal vs. external training load?
External: work performed (quantifiable: intensity, duration, and frequency of exercise)
Internal: body's response (specific to the exercise type)
Structure specific training load
Sum of movement and structure specific loads (e.g. step, throw, jump, direction change)
- different between individuals
Why are their training load differences between individuals?
- strength capacity, injury history, biomechanics, size/weight
Sport specialization and injury
- Better to be multisport
- DONT early specialize
- increasing chance of injury
Athletes are classified as
• Low (score = 0-1)
• Moderate (score = 2), or : 2.61
• High (score = 3) specialization. :4.74
Sport Injury

• Tissue damage / derangement of normal physical function
• Generally due to external forces (transfer of kinetic energy)
• Sport injury can apply to all tissues - Vessels, muscle, ligament, cartilage, nerve, etc.
What are the 3 modes of sport injury onset?
Injury may result from a clear acute mechanism (acute injury), clear repetitive mechanism (overuse injury), or from a combination of both mechanism.
• Acute injury → Sudden onset (single event)
• Overuse injury → Gradual onset (repetitive)
• Overuse injury → Sudden onset (single event / repetitive)
Direct contact injury

• Contact with another athlete
• Contact with an object
Indirect contact injury

• Through another athlete
• Through an object
Noncontact injury

• Without any contact from another external source
Soft-tissue vs. skeletal vs. acute injuries
• Soft-tissue injuries → cartilage, muscle, tendon, ligament
• Skeletal injuries → bone
• Acute injuries → bleeding (hematoma)
Articular vs. fibrocartilage
• Articular cartilage: flexible cartilage, provides smooth surface for joint movement (end of bones)
• Fibrocartilage: a tough cartilage, able to absorb loads (e.g., discs of the spine,meniscus)
Tendon vs. Enthesis vs. ligament
Tendon: muscle to bone
Enthesis: where a tendon or ligament attaches to bone
Ligament: bone to bone
Sprain vs. Strain vs. Fracture vs. Rupture
Sprain: stretching or tearing of ligaments/joint capsule
Strain: stretching or tearing of muscle/tendons
Fracture: partial or complete break in a bone
Rupture: severe injury in which a part of your body (often internal) tears or bursts open
Tissue Properties/Stress-Strain curve
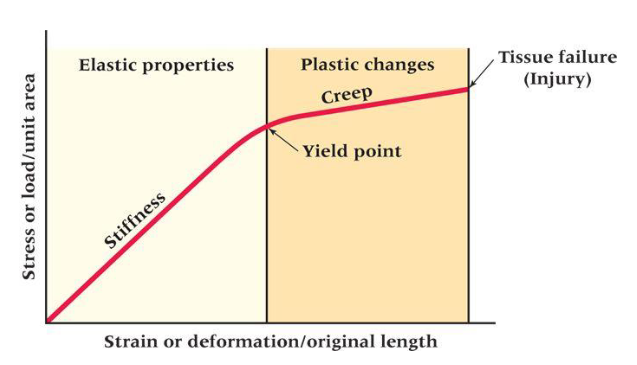
Stiffness
• Ability of a tissue to resist a load
Yield point
• Indicates the limit of elastic behavior and the beginning of plastic behavior
Creep
• Deformation in the shape/properties of a tissue that occurs under the influence of persistent mechanical stresses
What are the 4 stages of the healing process?
1. Hemostasis: Stop the leak
2. Inflammation: Clean Up!
3. Proliferation: Rebuild!
4. Remodeling: Increase tissue strength!
Hemostasis
Stop bleeding (clot)
• Process to prevent and stop bleeding when injury occurs → Results in formation of a clot
• Steps:
a) Vascular spasm
b) Formation of platelet plug
c) Blood clotting (coagulation cascade)
d) Formation of the final clot
• Platelet release growth factors
*min/hrs
Inflammation
• Defensive response of tissues to a physical or chemical injury, or bacterial infection
• Recruitment of cells to destroy debris and bacteria:
a) Neutrophils – for the first 48 hours
b) Macrophages – peak around 48–72 hours
c) Lymphocytes – appear after 72 hours
• Indicated by redness, warmth, swelling, pain, and dysfunction
*days
Proliferation (4 things)
Angiogenesis
• Formation of new blood vessels
• Restore blood flow
Fibroblast migration
• Fibroblasts produce collagen fibers and elastin
• Result = granulation tissue which replaces the clot
Epithelialization
• Epithelial cells cover denuded epithelial surface
Wound retraction
• Contraction of the wound
*weeks
Remodeling
• Granulation tissue matures into scar
• This stage may last several months-years (Important implications for return to sport!)
• Form & function of the scar tissue depend on loading during this stage
• Never achieve the same level of tissue strength than before injury! (~80%)
*months/years
Rehabilitation
- Bone & soft tissue respond to loading → remodel accordingly
- Healing structures need to be exposed to progressive loads.
What are some important factors in Wound Healing
• Nutrition
• Hypoxia
• Infection
• Immunosuppression
• Chronic disease
• Wound management
• Age
• Genetics
• Surgical technique
Early treatment goals
Goals:
• Limit bleeding (Too much bleeding slows healing)
• Limit swelling
• Relieve pain
- Improve conditions for subsequent treatment and healing
Acute injury management (soft-tissue)
PEACE and LOVE
PEACE
1. Protect
• Unload or restrict movement for 1-3 days
2. Elevate
• Elevate the limb higher than the heart
3. Avoid
• NSAIDs
• Ice
4. Compress
• Helps limit edema and hematoma
5. Educate
• Educate patients on the benefits of active approach to recovery
*EARLY
LOVE
1. Load
- Active approach with movement and exercise benefits most patients
2. Optimism
- Optimistic patient expectations are associated with better outcomes
3. Vascularisation
- Cardiovascular activity is a cornerstone in the management of injuries
4. Exercise
- Exercises help to restore mobility, strength and proprioception early after injury
*Subsequent
Stages of tissue and what to do
1. Acute stage
- Days
• PEACE
• (PRICE, POLICE)
2. Subacute stage
- (Rehabilitation stage)
- Weeks
• LOVE
3. Chronic stage
- (Training stage)
- Months
• LOVE
Acute stage
• DO NO HARM!
• ESSENTIAL that treatment begins as soon as possible!
• In the 3 days following acute injury, avoid:
- Heat – hot baths, hot showers, saunas, heat packs
- Moderate-Vigorous-strenuous activity – e.g. walking briskly, running
- Massage
Why not use ice?
Can disrupt inflammation
- only used to help pain management
What are different modes of onset?
Injury may result from a clear acute mechanism (acute injury), clear repetitive mechanism (overuse injury), or from a combination of both mechanism.
• Acute injury → Sudden onset (single event)
• Repetitive injury → Gradual onset (repetitive)
• Repetitive injury → Sudden onset (single event / repetitive)
What are overuse injuries now called?
repetitive injuries
- can be either gradual onset or sudden onset repetitive injuries'
- sudden onset occurs when they have a preexisting condition that causes the injury to occur right then
When should we use ice?
• It has been suggested that ice could disrupt the inflammation as well as the proliferation phases.
• Therefore, potentially, impairing tissue repair.
• BUT ice can effectively relieve pain
Wound healing
• Tissue never achieve the same level of tissue strength than before injury!
- It can reach up to 80% of it’s original strength.
• Form and function of the scar tissue depend on loading the tissue during this stage
– injured area needs proper loading!
• Don’t confuse the tissue strength of the injured area and function!
Re-injury
• Re-injury most often in the same location
• If the injury has gained enough strength, then the biomechanical weak-point becomes the interface between the scar tissue, and regenerating skeletal muscle fibre (weak point is the perimeters of scar tissue/where scar tissue meets regular tissue)
Subjective history
- Age; Sex
- Details of injury
- Training program & training history
- Diet
- History of previous injury General health
- Work/and leisure activities
- Other predisposing factors
Physical exam
- Inspection
- Palpation
- ROM testing
- Strength testing
- Ligament testing
- Neural testing
- Spinal examination
- Bio-mechanical examination
Active vs. Passive ROM testing
Active: patient moving on their own
Passive: clinician moving joint for the patient
*single leg squat is a good way to check biomechanics (look for valgus/over pronation)
Biomechanical examination imaging
X-ray (Radiography)CT (Computed Tomography)US (Ultrasound)MRI (Magnetic resonance imaging)
*imaging may overreport so its not 100% reliable
- what imaging finds may not be relevant to the patient
- delaying imaging may be more effective (less overreporting)
- this is why an effective SEM team is important
What are the stages of rehabilitation related to?
The healing process NOT time
1. Acute
2. Rehabilitation
3. Training
Acute Stage in acute vs. repetitive injury
Acute injury:
• PEACE/PRICE/POLICE
Repetitive injury:
• Partial unloading of the injured structure
• The loading pattern must be altered!
*PPP may also be effective
Rehabilitation stage
1. Monitor pain and swelling
2. Ensure normal ROM
3. Ensure normal strength
4. Ensure normal neuromuscular function
5. Ensure normal aerobic capacity
Rehabilitation Stage: Monitor Pain and Swelling
- It is necessary to tolerate some pain
*Gradually increasing pain and/or swelling needs to be reduced
Rehabilitation Stage: Re-establish ROM
• Normal ROM is a prerequisite for returning the athlete to normal technique
• Reduced ROM limits ability to do strength and other training!
Ensure normal strength
• Often Manual Muscle Test
– The Oxford Scale (0-5) (very subjective :()
• Consider, what is normal? (each person is unique)
• Sport, Limb Dominance etc.
• Strength v Endurance
• Equipment v No Equipment
• 10-15% often used as marker
Rehabilitation Stage: Neuromuscular training to regain normal neuromuscular function
• Painful conditions may result in reflex inhibitions → changes in movement patterns → unfavorable loading pattern → INCREASED RISK OF RE-INJURY
• Acute ligament injuries may also result in reduced joint position sense and coordination → INCREASED RISK OF RE-INJURY
• Proprioceptive training
• Progressive strength training (injured structures)
Normal aerobic capacity
• Sport specific aerobic fitness
• Modifiable intrinsic risk factor for injury. . . Remember?
Rehabilitation Stage: Alternative Training
• Maintaining general strength and endurance
• Well performed alternative training will allow the athlete to return to sport sooner
Rehabilitation Stage: Specific Training
• Training that affects the injured structures
• The amount, intensity, frequency, duration and exercises depend on the injury
• Highly repetitive training
• Weekly consultation with a physiotherapist
Rehabilitation Stage: Other Therapies
• Manual treatments: e.g., massage, manipulation, dry needling, vacuum cupping
• Taping, bracing
• Electrophysical agents: e.g., therapeutic ultrasound, laser, shockwave therapy
• Medication: e.g., NSAIDs, corticosteroids
• Dietary supplements: e.g., vitamin D, glucosamine
Training Stage: Sport Specific Training
1. Gradual transition from controlled rehabilitation exercises to sport specific training
2. Functional and sport specific testing to determine whether an athlete can tolerate sport specific training loads
3. Necessery that at least 85-90% of original strength is regained before being allowed to compete again
Return to sport
- each RTS process should be defined according to sport and level of participation
What are 3 elements of the RTS continuum?
- return to participate
- return to sport
- return to perform
What evidence do we have to inform the clinician’s contribution to the shared RTS decision?
• Functional and sport-specific conditioning tests play an important role in RTS decision-making
• Assessing readiness to RTS
• Tests assessing the athlete’s readiness to RTS should consider both closed (fixed environment) and open (less predictable) skills
• Psychological readiness is also an important element for optimal RTS
• RTS criteria: acute knee injuries, acute hamstring injuries, groin injury, Achilles tendon injuries, and shoulder injury
*RTS is a SHARED decision
*athletes often think they are further along in rehab than they truly are
Low back pain in youth athletes
low back pain occurs in ~10% of youth athletes
*spine extensions (back arch) puts pressure on spine and youth athletes are more likely to fracture
*pars interarticularis is the spine segment typically affected
What is the continuum of back pain?
1) Bone stress reaction (Posterior element overuse syndrome)
2) Fracture (Spondylolysis)
3) Slipping of vertebra (Spondylolisthesis)
Risk Factors for Spondylolysis & Spondylolisthesis
- Excessive extension and rotation loads
- Improper technique
- Hyperlordosis
Posterior Element Overuse Syndrome: Diagnosis and Treatment
• History, physical and neurological examination
• Imaging: e.g., X-ray, MRI, single-photon emission computed tomography (SPECT)
• Pain management*
• Pain free activities – avoiding extension
• Physiotherapy: core strength, anti-lordotic exercises, hamstring and iliopsoas stretching
• Return to sport within 4-8 weeks
*early detection is essential (don't want it to become a stress factor)
Spondylolisthesis surgical timeline
- Week 1: short walks and stretching
- Weeks 2-9: static stabilization exercises (core)
- Weeks 6-12: dynamic strength exercises
- Weeks 9-12: low impact aerobic training
*RTS between 6 months and 1 year
Prevention of Low Back Pain in Youth Athletes
• Recognition of risk factors
• In youth athletes → reduced training during rapid growth
• Proper techniques!
• Core strength
• Hamstring and hip flexor flexibility
Groin region
Where the abdomen meets the lower limbs via pelvis
Adductor-Related Groin Pain
• Most common groin injury
• Pain during sprinting, direction changes, and kicking
• Pain in the insertion of the adductor longus
Adductor-Related Groin Pain Diagnosis and Treatment
• History and physical examination (palpation and resisted adduction test)
• MRI is used to grade the injury extent from 0 to 3:
0 = no acute injury
1 = edema only
2 = structural disruption
3 = complete tear
• Exercise therapy programs
- Hölmich Exercise program (chronic groin pain)
- Progressive groin exercise program (acute groin injury)
The Hölmich Exercise program (8-12 weeks)
Treatment of Chronic Adductor-Related Groin Pain
• Isometric and dynamic exercises to reactivate the adductor muscles (2 weeks)
• Heavier resistance training, balance and coordination (6-10 weeks)
• Jogging is allowed after 6 weeks (if pain free)
• No stretching of the adductor muscles during this period!
*Sport specific training progressively after the program
Progressive groin exercise program
- Nine groin exercises
- Alternate days 3 times a week
- No groin pain allowed during the exercises
Return to sport after injury
• Three milestones:
1. Clinically pain free
2. Controlled sports training
3. Full team training → RTS
• Athletes with an MRI grade 0-2 adductor injury
- Usually return to full team training after 3 weeks
• Athletes with an MRI grade 3 adductor injury
- Usually return to full team training within 3 months
Structure of a ligament
• Dense bands of collagen tissue
• Collagen, elastin, proteoglycan, and other proteins
• Vary in size, shape, orientation and location
Function of ligaments
• Connect one bone to another → Passive stabilization of the joints
• Ligaments can creep
• Serve important proprioceptive function
Ligaments' response to injury
• Healing follows the constant pattern
• Ligament scars have inferior creep properties
• Ligament injury → decreased proprioception
What does joint stability depend on?
the interaction between the passive, active and neural subsystems
Passive subsystem of joints
consists of non-contractile connective tissues (ligaments, bones, cartillage)
Active subsystem of joints
controlled by the neural subsystem to provide dynamic joint stability (tendon and muscle) (dynamic joint stability)
What are the 3 types of ligaments?
1. Intra-articular ligaments (within joint) e.g. cruciate ligaments of the knee
2. Extra-articular ligaments (additional support structure) e.g. calcaneofibular ligament
3. Capsular ligaments (thickening of joint capsule) e.g. anterior talofibular ligament
What type of ligament is best at healing vs. the worst?
Best: capsular ligament
Worst: Extra-articular ligament
How do ligaments adapt to training?
1. Adapt slowly to increased loading, but weaken very rapidly as a result of immobilisation
2. Adapt to loading by increasing the cross-sectional area3. Normal everyday activity is sufficient to maintain mechanical properties4. Systematic training can increase ligament strength by 10-20%
Stress-strain curve of a ligament
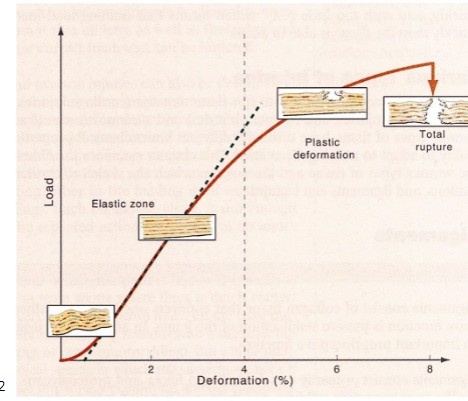
If force causes more than a 4% change of length, the collagen fibers will start to rupture
Ligament injuries acute vs. repetitive
*TYPICALLY INJURED BECAUSE OF ACUTE TRAUMA
- REPETITIVE INJURIES RARE, BUT CAN OCCUR AS THE LIGAMENT IS GRADUALLY STRETCHED OUT
e.g. UCL repetitive pitching injury
General mechanism of ligament injuries
SUDDEN OVERLOAD → LIGAMENT IS STRETCHED (JOINT IN AN EXTREME POSITION)
What are the 3 grades of ligament injuries?
Grade 1• Mild• Structural damage on the microscopic level• No instabilityGrade 2• Moderate• Partial tear• Swelling & Pain• No/limited instability
*LaxityGrade 3• Severe• Full rupture• Significant swelling• Instability
Laxity
Joint play, implies movement, but ligament is still intact
Evulsion fracture

bone tearing
Description: Felt my knee-cap go out
Implication: Patellar dislocation/subluxation
Description: Hit from lateral side - valgus
Implication: MCL +/- ACL
Description: Valgus/external rotation - with or without contact
Implication: ACL +/- MCL +/- lateral meniscus +/- bone bruise
Description: Direct blow to anterior tibia
Implication: PCL
Description: Hyperextension injury
Implication: ACL
Description: Minor twist in older individual
Implication: Degenerative Meniscal tear
What are some questions to ask the patient that may help determine the injury?
1. Did you feel or hear a rip, pop or tear?
2. Did something come out of place?
3. Knee or Knee-cap?
4. Where is the pain?
When did the swelling occur? Min? Hours?
Valgus mechanism of injury
• ACL injury• MCL sprain• Lateral dislocation of patella• Meniscus injury• Lateral tibial plateau fracture or bone bruise
Hemarthrosis
bleeding into the joint
What injuries cause hemarthrosis vs. don't
Do: ACL tear; Peripheral meniscus tear; Osteochondral injuries; Fractures
Don't: MCL tear; Central meniscus tear; PCL tear; Cartilage injury
What are the two bundles in the ACL?
1. Anteromedial bundle resists tibial anterior translation2. Posterolateral bundle resists tibial rotation• No pain fibers, but has proprioceptive fibers (usually traumatic e.g. bone bruise which makes it painful)
What are two tests to test for an ACL injury?
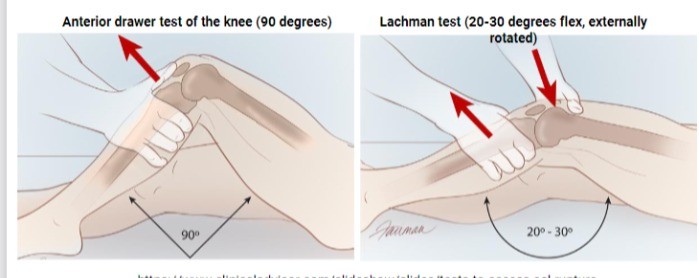
1. Anterior drawer test of the knee (90 degrees)
2. Lachman test (20-30 degrees flex, externally rotated)
*may be difficult to determine with hamstring spasm
What is the most effective test to determine an ACL injury?
Pivot shift test!
- or an MRI, but they often are only used with a locked knee (torn fibrocartilage in the meniscus)
ACL complications
- Osteochondral injury- ACL injury and Meniscus tear- Osteoarthritis in 15-20 years- Unhappy Triad (MCL, ACL, lateral meniscus)
Bucket-handle rupture of the meniscus
causes a locked knee
- 20% of repairs fail
ACL treatment goal
To prevent subsequent injuries, such as osteochondral injuries and meniscus injuries
ACL options for joint instability
• Modification of activity (no twisting activity)• Bracing for light twisting activity• ACL reconstruction (although functional – never normal)
ACL reconstruction
- the graft is weakest at 3-6 months
- high re-injury rates over 2 years after reconstruction
*can use hamstring tendon or patellar tendon
In Calgary which tendon do we primarily use for ACL reconstruction?
hamstring tendon = skiing (patellar tendon is used lots when skiing and is much more invasive)
*doesn't use bone = has a higher chance of being lax :(
In Soccer which tendon do we primarily use for ACL reconstruction?
patellar tendon
*more invasive surgery
What can reduce reinjury risk by 84% after ACL reconstruction?
Simple decision rules
What usually happens after returning to sport after ACL reconstruction?
Returning to Level 1 sport after ACL reconstruction leads to a more than 4-fold increase in reinjury rates over 2 years
Why are women more prone to ACL injury?
- pelvis larger
- flexible
- strength
- biomechanical
- hormones
- training (modifiable)
What are some modifiable risk factors of ACL injuries?
• Weak hip abductors an external rotators• Increased knee abduction moments during cutting and landing
Knee control training program
• Adolescent female soccer players (n=4600)• 64% reduction in the rate of ACL injury was seen in the intervention group
Are ACL injuries decreasing?
- Although current ACL injury prevention training programs have been successful in reducing injuries in controlled research settings, the real-world ACL injury rate remains high, and even continues to increase- The ACL injury rate for girls/women has not changed in over 20 years, and they remain up to 6 times more likely to experience injury compared with boys/men- In addition, as many as 40% sustain a recurrent ACL injury in the same knee or new ACL injury in the contralateral knee
Why are ACL prevention programs working in controlled research settings, but not the real world?
Due to poor athlete and coach buy-in!
What are the 3 main ligaments in the glenohumeral joint?
1. coracoacromial ligament
2. coracohumeral ligament
3. glenohumaral ligaments
*stability formed from the rotator cuff
Dislocation
complete separation of articulating bones
Subluxation
partial dislocation of articulating bones
Typical mechanism of shoulder injury
- Direct blow to the posterior aspect of the shoulder
- Landing on outstretched arm• Anterior dislocation• Fracture dislocation
Diagnosing and treatment of shoulder injury
1. History & Physical examination2. Imaging3. Reduction of the shoulder (after confirmed diagnosis)4. Protection from re-injury5. Rehabilitation period prior return to sport
Recurrence of shoulder
- 50-90% depending the type of sport and shoulder dominance- Surgical management (in high-risk population)- Rehabilitation of the shoulder is critical to long-term function
Prevention of Shoulder Dislocations & Subluxations?
- strength
**Neuromuscular control
Tendon basic facts
• Collagen tissue• Connects muscle to bone• Transfer force from muscles into skeletal system• Excellent tensile properties
Tendon breakdown
1. Tendon
2. Tertiary fiber bundle
3. Fascicle
4. Subfascicle
5. Collagen fiber
6. Collagen fibril
Enthesis
• Junction between a tendon and a bone• Fibrocartilage• Enthesopathy (disorder)
Myotendinous junction (MTJ)
• Connection between tendon and muscle• Susceptible for injury
Tendon: stress strain curve
• Relationship between stress and deformation of tendons is the same as for ligaments
Tendons adaption to training
- Tendons adapt to training by increasing cross-sectional area- Tendon loading every 2-3 days- Compared to muscles, it takes longer time to gain tendon strength
2 types of tendon injuries
Repetitive tendon injuries
• Tendons are most often affected by repetitive injuriesAcute tendon injuries• Direct trauma• Rupture
Tendinopathy
Umbrella term used for tendon problems
Tendinopathy mechanism
• Repetitive tensile (or compressive) loading (e.g., sprinting, jumping, changing direction) → repetitive microtraumas• Inadequate recovery between loadings
Tendon Pathology: Cook–Purdam Model (3-stages)
1. Reactive tendinopathy• Non-inflammatory, structural changes & thickening of stressed tendon area2. Tendon disrepair• Worsening tendon pathology, tendon structure becomes disorganized3. Degenerative tendinopathy• Chronic stage
• Can't recover
***Need to catch EARLY
Intrinsic tendinopathy risks
- adiposity
- pre-existing conditions (e.g. diabetes)
- age
- menopause
- previous injuries
Extrinsic tendinopathy risks
- extra weight (loading)
- uneven ground
- type of sport
- periods of deconditioning (e.g. covid)
How do we diagnose tendinopathy?
History: Symptoms often progress (start low)• First pain after exercise• Then pain at the start of an activity• Finally pain both during and after activity
Physical Examination• Palpation – tenderness
Imaging: US, MRI (not very usuful)
Management of tendinopathy
- Education of patients (long time to recover, pathology may still exist in the absence of pain)- Load monitoring - Pain monitoring (will still have)- Exercise based progressive rehabilitation program
****DO NOT REST for tendon injury (except acute)
Exercise Based Rehabilitation Programs for Lower Limb Tendinopathy
Stage 1: Isometric exercises (joint doesn't move, allogenic in nature/pain relief)
Stage 2: Isotonic & Heavy slow resistance exercises (movement with contraction. Concentric (muscle shortens) or eccentric (muscle lengthens))
Stage 3: Increase in speed and energy storage exercises (if pain = decrease level)
Stage 4: Energy storage and release & Sport specific exercises
Other treatments for tendinopathy
• Shock wave therapy, laser, and ultrasound• Medications (e.g. anti-inflammatory)• Injectable therapies (can be bad for tendon cells)• Passive treatments• Experimental treatments (e.g. STEM cell)• Surgery
*Conservative treatment
Tendon rupture
• Acute rupture of a normal and healthy tendon is rare• Commonly occur in athletes and recreational exercisers aged 30-50 years
Tendon rupture causes
Eccentric force generation:
•Mid-tendon area•Bone-tendon junction
Achilles tendon, Supraspinatus tendon:
•Partial rupture•Complete rupture
Achilles Tendon Rupture
- Active mid-aged recreational athletes- High risk of injury: rapid direction changes, jumps- Usually occur without warning (degenerative changes)
Achilles Tendon Rupture mechanism
Strong contracture of the lower leg musculature, with simultaneous extension• ECCENTRIC LOADING of the tendon
Diagnosis Achilles Tendon Rupture
- Acute, intense pain
- Audible ‘SNAP’
- Reduced power in plantar flexion
- ‘Gap’ in the tendon tissue
- Bruise and swelling
- Ultrasound/MRI
Treatment and rehabilitation of torn tendon (Achilles)
- Conservative vs. Surgical repair (end-to-end suture)- Cast- Rehabilitation- Return to Sport
Why do we put the foot in plantar flexion when healing the Achilles tendon?
takes pressure off, so that tendon heals in the shortest position (still elastic after recovery)
NFL players and RTP from achilles injury
61.3% of NFL players were able to successfully RTS at a mean 11.90 months following a primary AT rupture.
What are some injury prevention strategies for the achilles tendon?
- neuromuscular training
*Proper loading
Muscle function
Generate power
- muscle cells (fibers)
Isometric
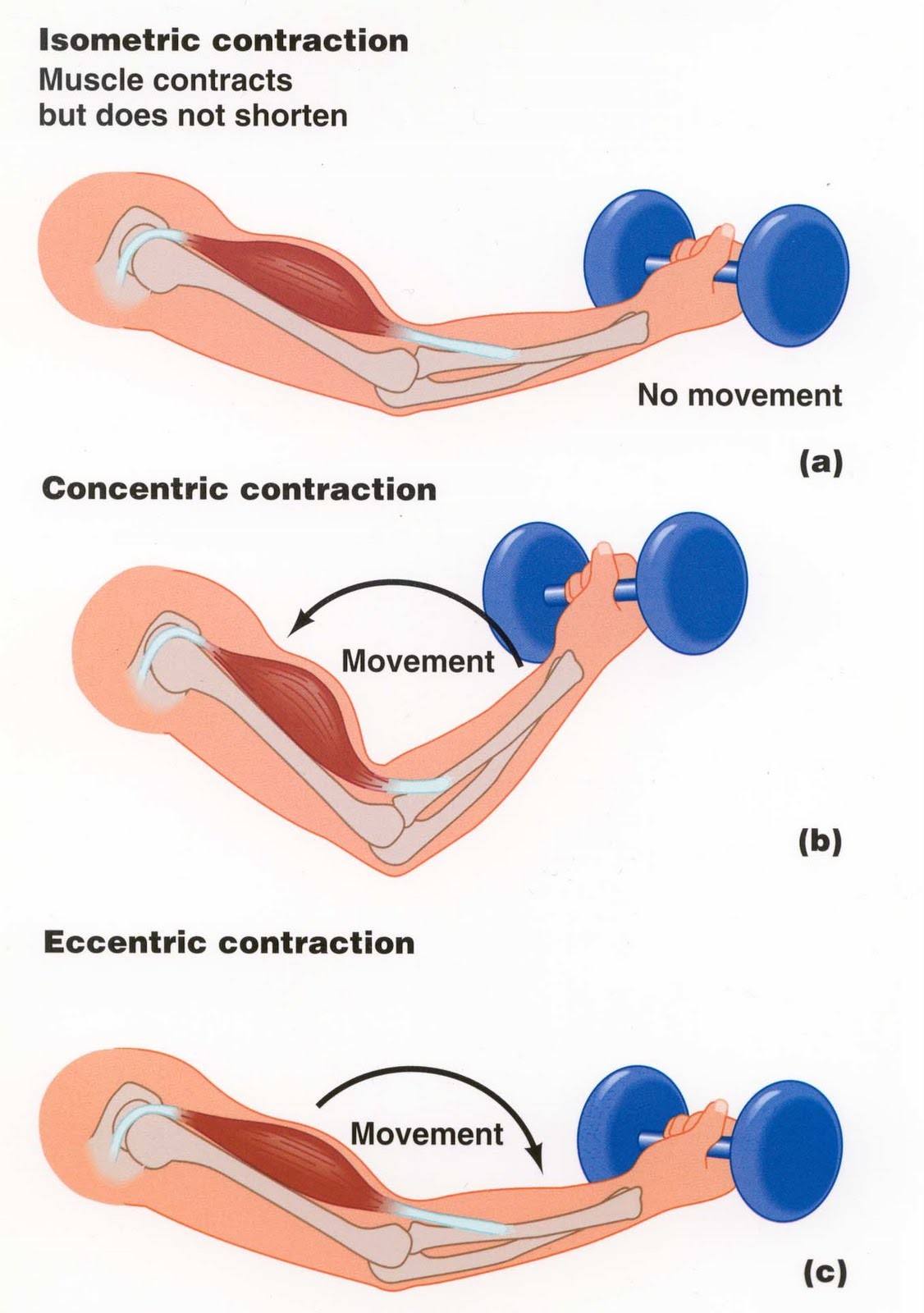
No change in muscle length
Isotonic
muscle shortens to overcome resistance
(concentric and eccentric)
Concentric
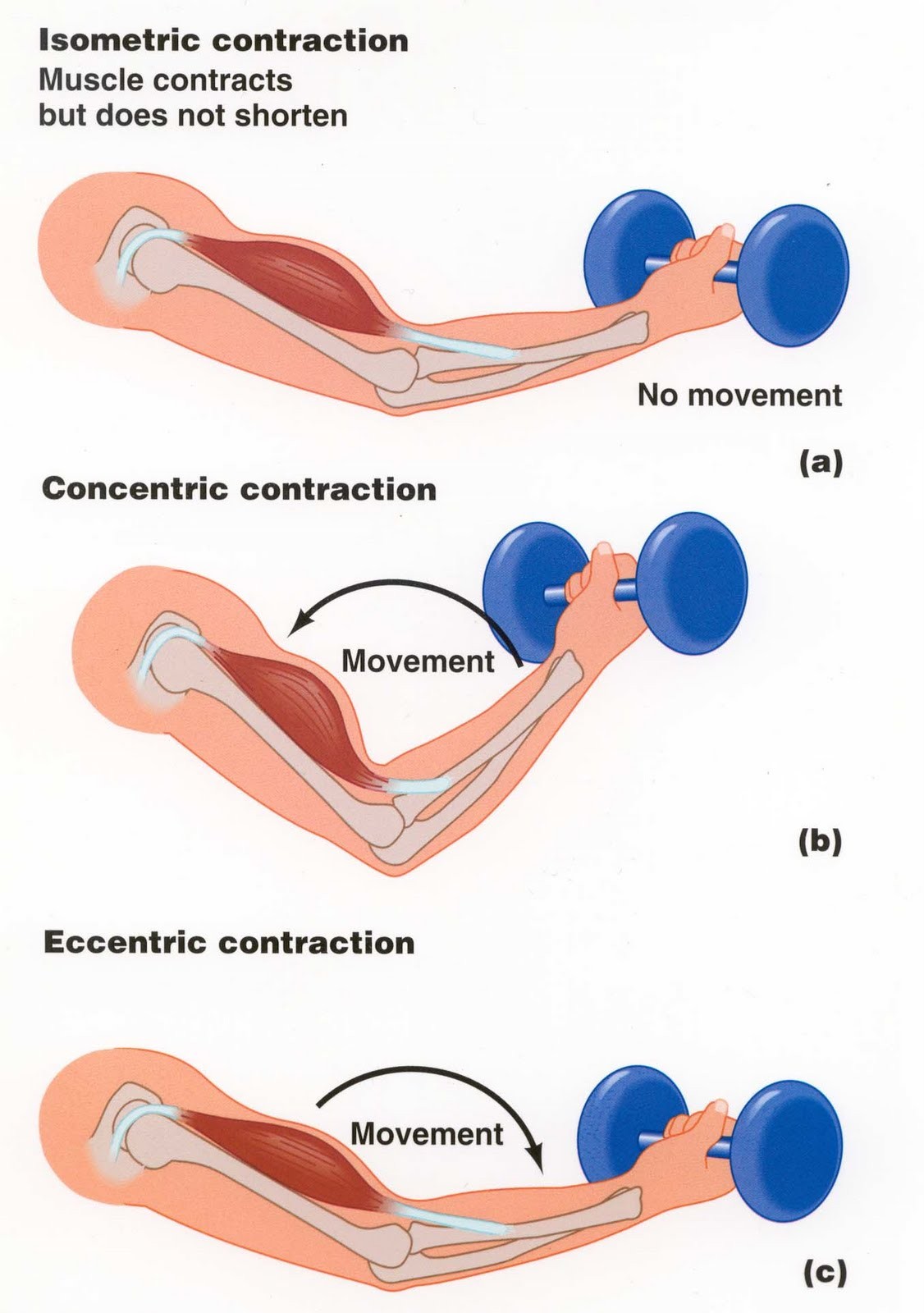
shortening of muscle
Eccentric
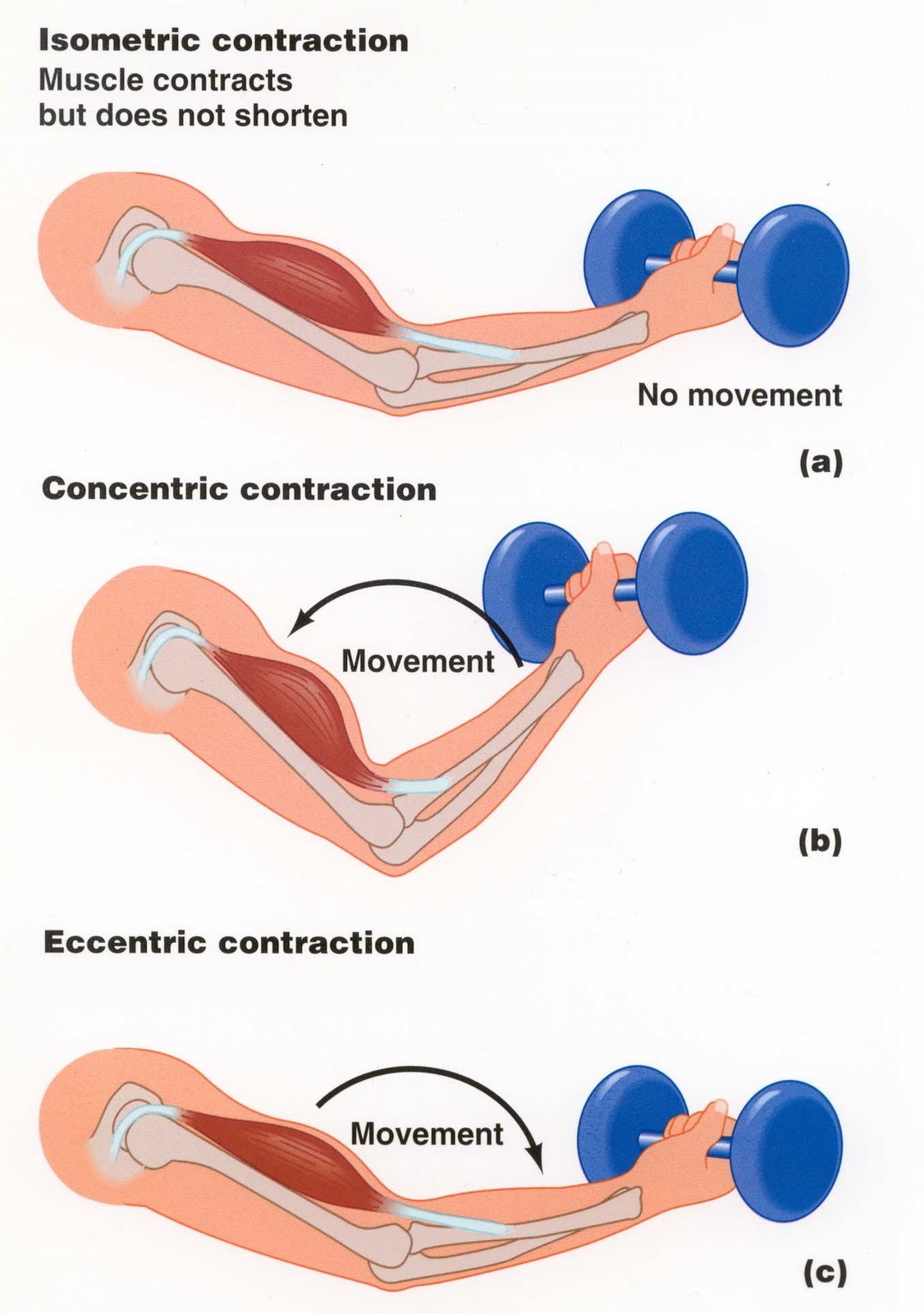
lengthening of muscle
Muscle: Adaptation to Training
- rapid response to training
- neural and muscular factors (neural 1st)
- muscle fibers increase their cross-sectional area (hypertrophy)
Muscle injury types
1. Direct trauma
• Contusion• Muscular laceration
2. Distension ruptures
• Muscle strain
3. Other
• DOMS• Myositis ossificans (calcification of muscle tissue, caused from trauma)• Muscle cramps
Muscle Contusion
- Muscle bruise- External force- Contact sports, team ball sports- Most common site is the quadriceps
Muscle Strain
- Tensile forces- Usually close to MTJ- Hamstrings, quadriceps, gastrocnemius- Pop, bump, swelling*Pain on active contraction and passive stretch, reduced contraction strength, decreased ROM and loss of function
Clinical Grading of Muscle Strains
Grade 1 – Mild• ‘Few fiber’ injury, minimal loss of strength and motionGrade 2 – Moderate• Tissue damage, decreased ability to contract and decreased ROM (large spectrum)Grade 3 – Severe• Complete tear, complete loss of muscle function
2 types of hamstring rupture
• Type I – Sprinting-related hamstring strain (biceps femoris)• Type II – Stretching-related hamstring strain (semimembranosus)
Type I hamstring rupture– Diagnosis
• History & Physical examination- Mechanism- Palpation• Imaging- MRI
Type II hamstring rupture– Diagnosis
• History & Physical examination- Mechanism- Palpation• Imaging- MRI
**Higher up
Muscle Injury: Healing
• Destructive Phase (Hemostasis & Inflammation)• Repair Phase (Proliferation)• Maturation Phase (Remodeling)
Rehabilitation of muscle injury
1. Mobilization2. Progressive strengthening (concentric)3. Functional exercises (e.g., running program)4. Other body regions (other muscles help do tasks, want to work effectively)
What proves most effective in hamstring rehab
High reinjury = decrease by doing lengthening (eccentric) during rehab = more beneficial compared to concentric
**No evidence stretching helps
How do we prevent hamstring injuries?
- LOADING
- no evidence on stretching
*eccentric training (new and recurrent prevention)
bone functions
• Protects our internal organs• Provides the body its basic shape• Facilitates movement• Provides a framework for support
3 types of fractures
• Traumatic fracture (e.g., accidents and sports) - major trauma
• Pathological fracture (e.g., osteoporosis and cancer) - 2nd to disease
• Fatigue fracture (e.g., stress fracture and atypical femoral fracture) - stress
Types of bone
1. long bone
2. short bone
3. flat bone
4. irregular bone
Long bone
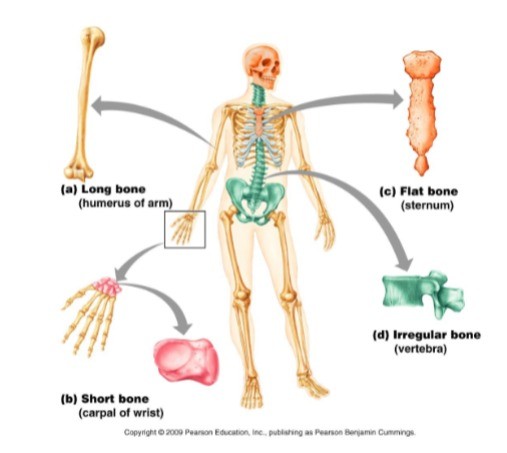
longer than wide, having a cylindrical shape
e.g. humerus, tibia, fibula
Short bones
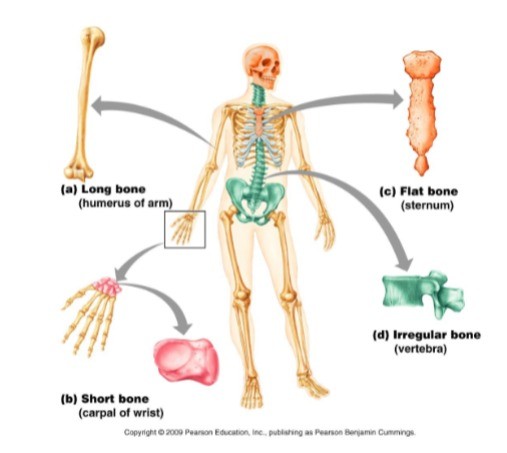
Smaller cube-shaped bones have more or less similar lengths and widths.
e.g. carpal bones, tarsal bones
Flat bones
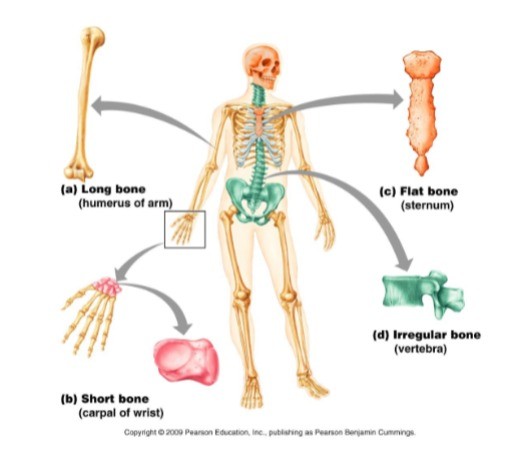
These bones are thin, broad, and usually curved.
e.g. sternum, cranial bones, scapula
Irregular bones
these bones do not have a definite shape like the previous three types.
e.g. vertebra, pelvis
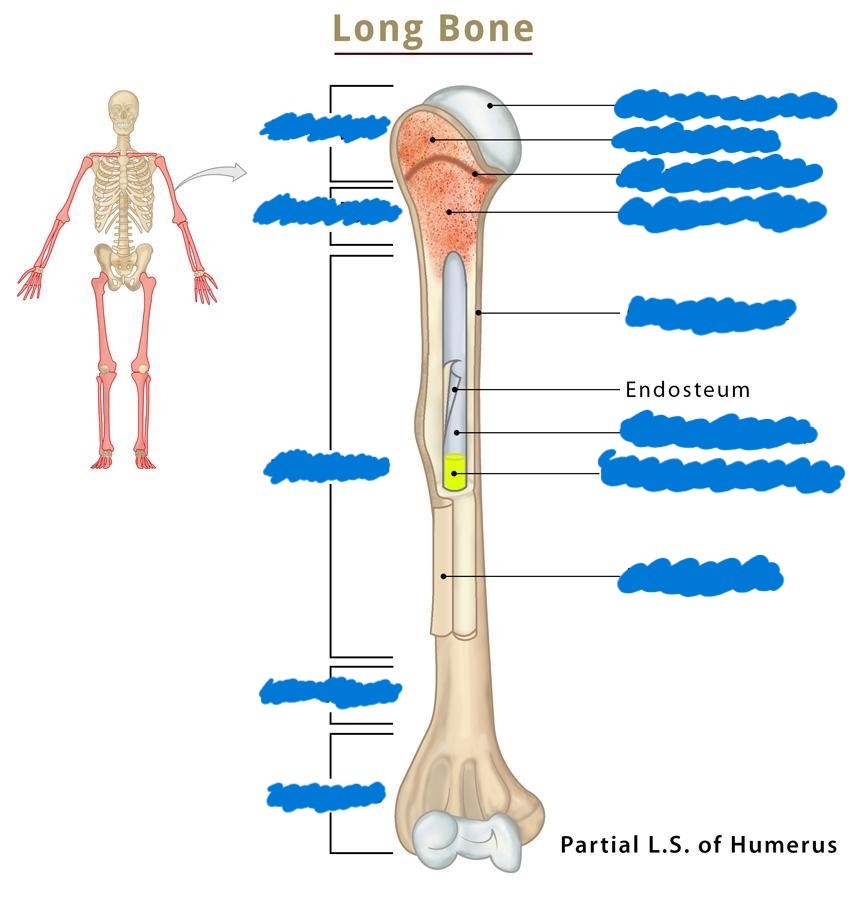
Long bone anatomy
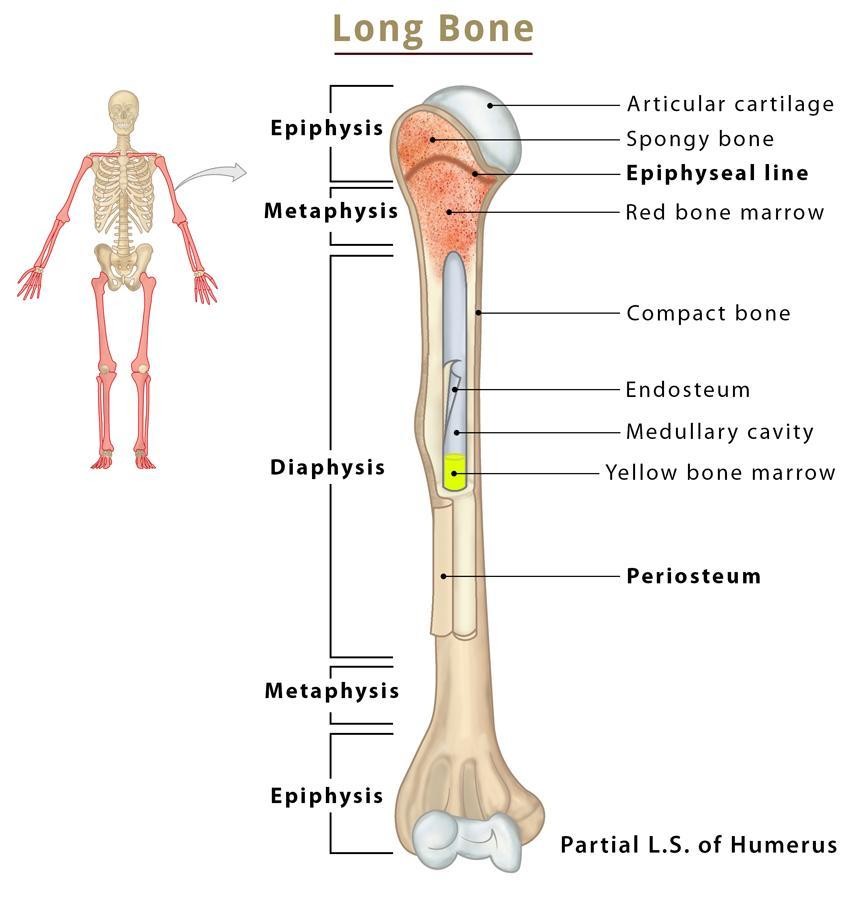
*Cortical (hard) bone
Bone marrow
In MEDULLARY CAVITY
- Yellow: fat storage
- Red: create RBCs
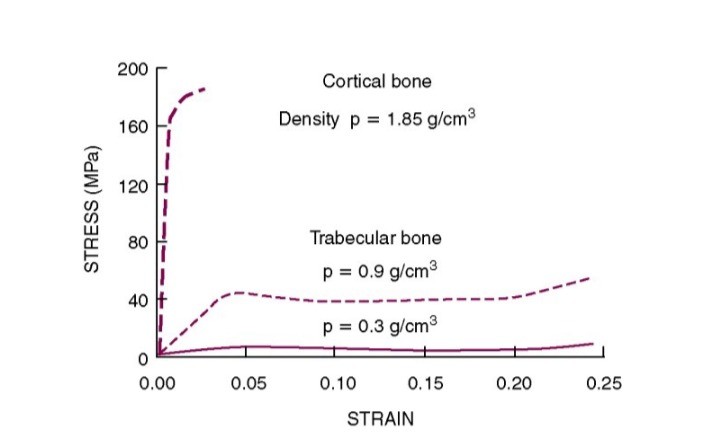
Trabecular bone

- spongy bone
- highly porous
- found in the end of long bones
- trabecula are random
- 40% porosity
- very light
Cortical bone

- denser
- found in long shaft of long bones
- 5-10% porosity
Lamellar vs. woven bone
• Lamellar bone– Slowly formed, highly organized– Parallel layers of anisotropic matrix of mineral crystals and collagen fibers• Woven bone– Quickly formed, poorly organized– Randomly arranged mineral and collagen fibers– Sites of fracture healing, tendon/ligament attachments
Bone composition
25% water, 32% organic matrix (collagen), 43% apatite mineral
Bone: (re)modeling dynamics
• Bone is a dynamic tissue• Constantly remodeling in response to its mechanical environment• Adapts to best resist the loads experience during habitual activity• Mechanical stimuli = bone strain (or some consequence thereof)
Functional adaptation
Load causes bone to develop cortical bone and withstand pressure
3 rules to bone adaptation
1. Driven by dynamic, rather than static, loading2. Only a short duration of loading is necessary; extended loading durations have diminishing adaptive returns3. Bone cells accommodate to customary loading making them less responsive to routine loading signals
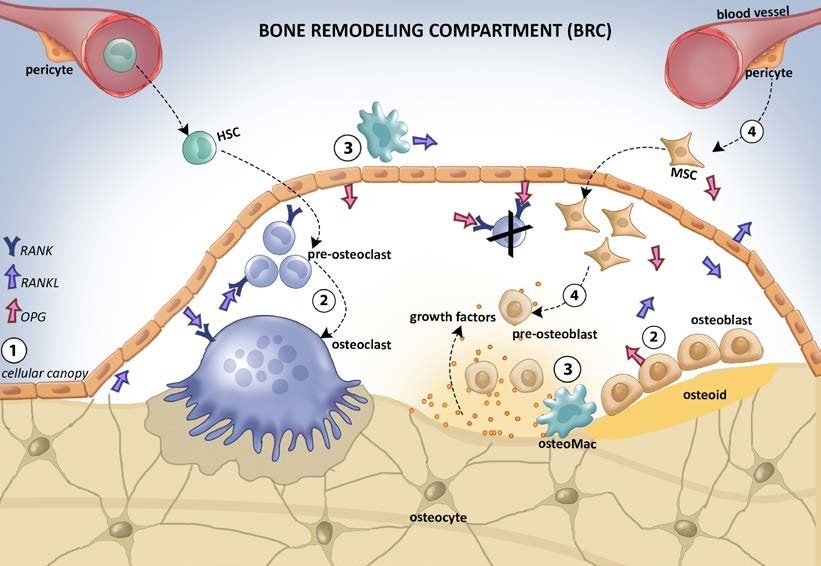
Osteoclast
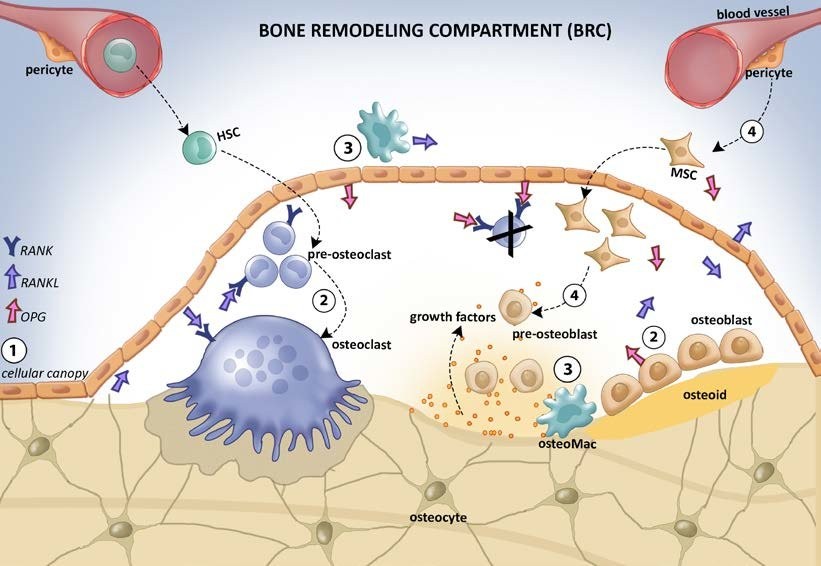
large multinucleated cells that resorb bone tissue.
Osteoblasts
specialized cells that synthesize and mineralize bone matrix.
Bone modelling vs. remodeling
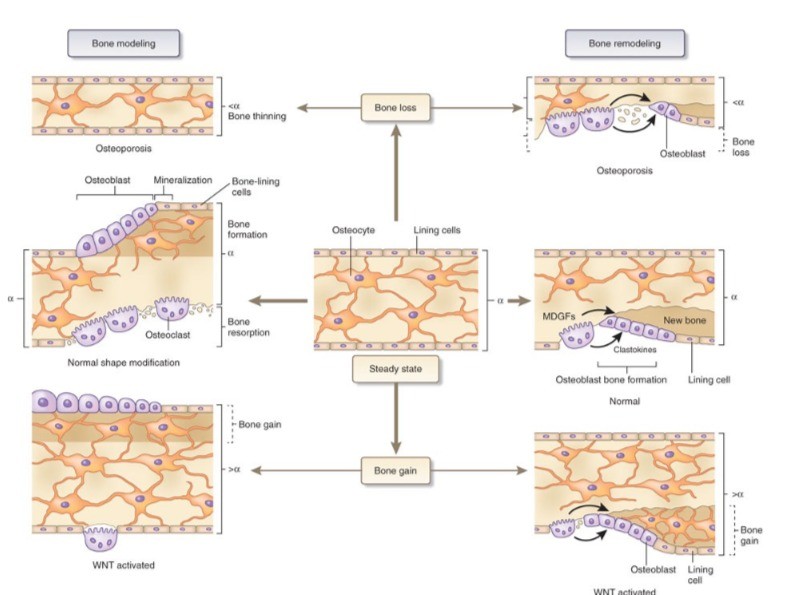
Modelling: refers to the process of bone turnover that alters the shape of the bone. Bone modeling adapts structure to loading by changing bone size and shape and removes damage, preserving bone strength
*bone formation then bone reabsorption, to achieve normal state
Remodeling: is the turnover that recycles bone without changing its shape. It shapes the bones of the skeleton as a child grows, and it repairs tiny flaws in the bone that result from everyday movements. Remodeling also makes bones thicker at points where muscles place the most stress on them
*bone loss 1st then osteoblast
Mechanical properties of bone / stress-strain curve
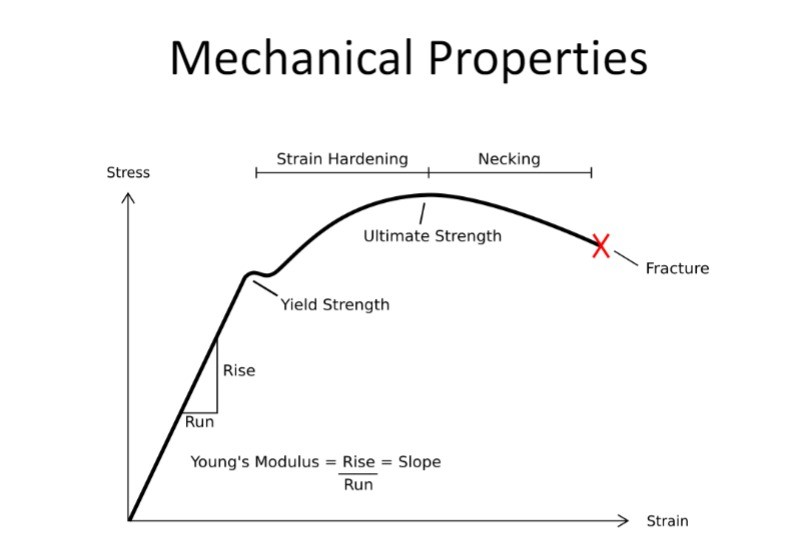
Young Modulus: slope
Yield strength: point of no return
Cortical vs. Trabecular bone stress-strain curve
3 types of fracture classification and how each occurs
• Traumatic fracture – caused by acute high energy trauma
• Pathologic fracture – caused by minimal trauma in a weak, diseased, or fragile bone
• Fatigue fracture – caused by accumulation of microtrauma associated with repetitive loads
* Traumatic and pathological fracture when the applied load exceeds the bone’s strength* Fatigue fracture when number of repetitive loads exceeds the bone’s fatigue life
Fractures are _______ events
biomechanical
Closed vs open fracture
• Closed fracture – bone does not break through skin• Open fracture/Compound fracture – bone breaks through skin. These carry high risk of infection
Fracture patterns
Transverse: straight across
Linear: in the middle
Oblique non-displaced: angle attached
Oblique displaced: angle detached
Spiral: from rotational force
Greenstick: side
Comminuted: shattered
Fluctuating loads vs. monotonic loads
Fluctuating loads are MORE detrimental than monotonic loads
Human cortical bone– Monotonic load failure = 190 MPa– Cyclic load failure = <30 MPa (107 cycles)
*increasing magnitude of stress, greatly decreases the number of cycles to failure
Three stages of fracture healing
1. Inflammatory phase2. Reparative phase3. Remodeling phase
*overlap
Inflammatory phase of fracture healing
• Immobilizes the fractured bone and activates cells for repair• Hematoma formation• Vasodilation and serum exudation• Infiltration of inflammatory cells• 3-7 days
Reparative phase – soft callus of fracture healing
• Primary callus response• Inflammation triggers cell division and growth of new blood vessels• Chondrocytes secrete collagen and proteoglycans to form fibrocartilage• 2 weeks
Reparative phase – hard callus of fracture healing
• Endochondral ossification• Direct bone formation by osteoblasts• Soft callus turns to hard callus made of woven bone• 2 weeks
Remodeling phase of fracture healing
• Modeling and remodeling of fracture site• Gradually restores original shape and internal structure• Woven bone replaced by secondary lamellar bone• Can last for many years
Spotting the signs of a fracture
• Pain and tenderness• Swelling and bruising• Deformity and loss of motion/function• Protruding bone
Conservative treatment of fracture
*Reduction and Immobilization• Splinting and bracing• Plaster or fiberglass casting• Bandages and orthoses
Surgery of a fracture
When conservative treatment fails or fracture is highly displaced or unstable– Intramedullary rods– Locking and stabilizing plates
Surgery internal vs external fixation
Internal: placed inside the bone, or on the outside of the bone
External: outside of the skin holding bone on the inside
Speeding up or improving repair of fracture
• Bone grafts
• Stem cell therapy
• Mechanical stimulation
– Ultrasound
– Electricity and magnetic fields
*Not tested
*Efficacy?
Is it arthritis or not?
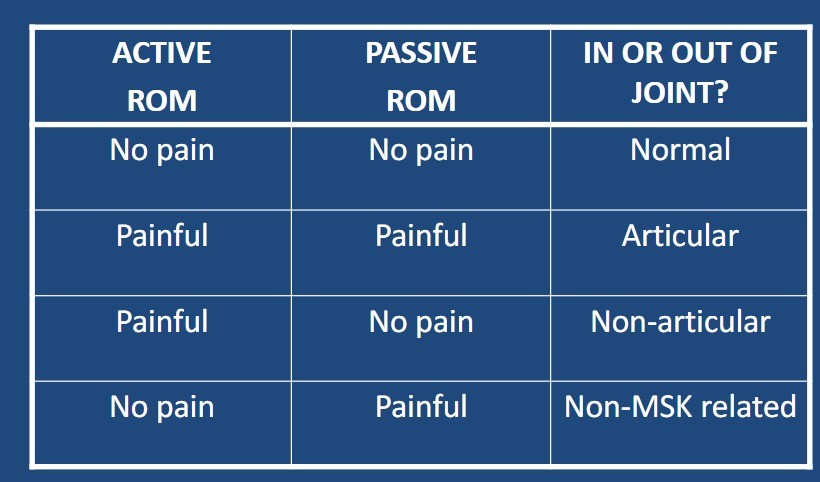
Is it in the joints, or outside the joints?– Active vs. passive range of motion.– Active (done solely by patient), both joints and muscle/tendons move.– Passive (done by physician), joints move, but no muscle/tendon contraction or force developed
Is it inflammatory or not?
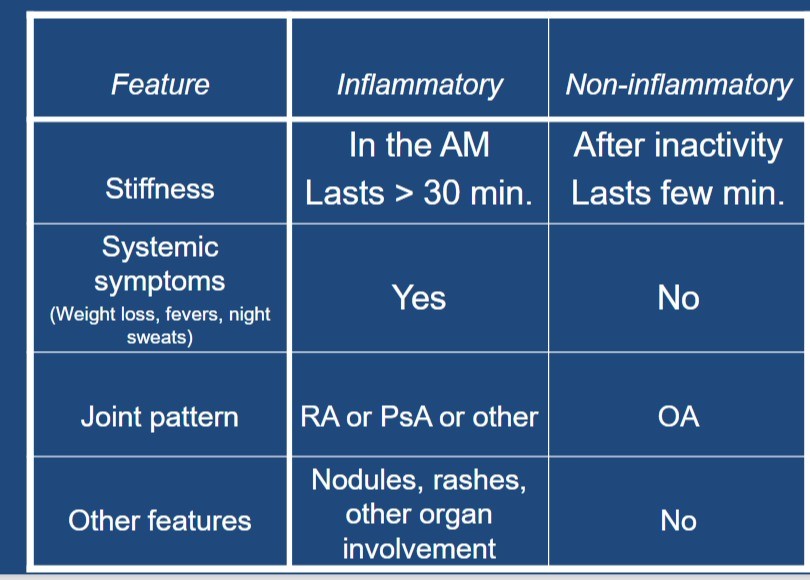
The “classic” inflammatory arthritis
rheumatoid arthritis
– Arthro – joint– -itis – inflammation– Rheuma - fluid
Clinical presentation of RA
– Fluctuating joint pain and swelling– Morning stiffness, usually > 1 hour, better with moving and heat.– Systemic symptoms (weight loss, fatigue)– Joints affected MCP + wrist > PIP + MTP > knees + shoulders + ankles > elbows + hips >> other
- Rheumatoid nodules
Pattern of joint involvement in RA
- May start as a monoarthritis, but often evolves into a small joint, symmetrical, polyarthritis.- 90 % of all affected joints will be affected in the first year.
RA has systemic features:
a. Weight loss.b. Fevers .c. Night sweats.d. Morning stiffness.e. Fatigue
Extra-articular disease in RA
a. Subcutaneous nodules in 20 %.b. Pulmonary involvement in 50 %.c. Cardiac involvement in 5 %.d. Eye involvement in up to 35 %.e. Neurologic, rare to common findings.f. Renal, rare.g. Muscular, disuse atrophy very common.h. Rheumatoid vasculitis, rare.
RA is an ____________ disease
autoimmune
– Refers to diseases in which the patient’s own immune system is at the centre of the disease process– The immune system is stimulated to act against ‘self’– When the immune system is stimulated it can produce antibodies to self antigens, and inflammatory mediators which cause tissue damage
Proposed triggers of RA?
– Infections• Viruses eg. Cytomegalovirus, Herpes virus, Rubella, EBV• Bacteria eg. Staph, Strep, Borelia (Lyme disease)• Mycoplasma– Autoantigens-Type 2 collagen- Proteoglycans- Chondrocyte- Immunoglobulins (IgG)
Risk factors of RA
• Genetic factors are responsible for 50-60% of the risk associated with RA, HLA-DRB1 and HLA-DR4 genes are associated with an increased risk of RA or more severe disease.• Environmental factors such as smoking and sex hormones also play a role
What are the goals of treatment?
1. To prevent or control joint damage.2. To preserve or prevent loss of function.3. To decrease pain and swelling.
What are the approaches to treating RA?
– Non-pharmacological– Pharmacological– Surgical– Alternative
Non-pharmacological treatments:
– Lifestyle adjustments– Physiotherapy– Occupational therapy
Non-pharmacological treatments: lifestyle adjustments
• Rest• Smoking cessation ( risk of RA in smokers)• Reduced stress• Healthy eating (?anti-inflammatory diets, fish oils).• Education– patient needs to learn about their illness and needs to play arole in its management
Non-pharmacological treatments: physio and exercise
• Decreases joint pain and stiffness.• Improves ability to carry out activities of daily living.• Enables better sleep and relaxation.• Strengthens muscles and tendons to take stress off of joints.
• Helps to maintain a healthy weight, obese patients have worse RA than non-obese patients.• Improves sense of well being.• Decreases likelihood of medical complications.• Enables participation in “fun” activities with friends and family
Non-pharmacological treatments: physio and exercise different types
• Range of motion.• Endurance/aerobic exercise.• Strengthening exercise.
Physio and exercise treatment during active joint inflammation
- Performed at least once a day– Gentle assisted movement through the joint’s normal range, to prevent contracture– Isometric “static muscle contraction” exercises to maintain muscle tone without increasing inflammation– These exercises should not be pushed into pain & any discomfort felt after exercising should settle within one hour– Build up new exercises gradually so that you can differentiate between the ‘normal’ amount of pain you get and pain from overusing a joint– The acute phase is when joints are most vulnerable to damage, so adjust the number of exercises or how far you move each joint for how you feel that day
Physio and exercise treatment during chronic (non-acute) joint inflammation
– Can progress the above exercises to include use of light resistance– Postural / core stability exercises/ swimming / walking / cycling to maintain cardiovascular fitness– Gentle stretches for areas that can become tight, such as knees & calves – try to regain any lost range of motion
Non-pharmacological treatments: Occupational therapy
Therapeutic modalities1. Heat2. Parraffin – wax baths3. Cold4. TENS machines
Joint protection *benefits of joint protection include less pain and greater ease in doing tasks.• 4 main techniques for joint protection:» Pacing» Positioning» Using assistive devices» Weight Control
Joint protection
means using your joints in ways to avoid excess stress, it includes:– Avoiding repetitive activities that will damage joints.– Using a brace or splint to protect the joint and provide more stability.– Using a cane or walking stick to unload the joint.
What is a typical repetitive injury?
Pathological process is often under way for a period of time before the athlete notices symptoms
*gradual and sudden onset
What are some alternative names to repetitive injuries?
•Gradual onset injury•Chronic injury•Overuse syndrome•Sports disease•Cumulative trauma disorder•Repetitive strain injury•Overuse injury
Types of repetitive bone injuries in sport
Bone stress reaction, Stress fracture, Osteitis, Apophysitis, Enthesopathy
Sever’s Disease vs. Achilles Tendon Enthesopathy
Sever's disease: an irritation of the back of the calcaneus, on the growth plate (inflammed)
Achilles Tendon Enthesopathy: irritation of the tendon which attaches to the calcaneus bone, pulling on the growth plate.
*ALWAYS in adolesence
*During growth
Traction apophysitis
Inflammation and pain at the growth plates of bones
- e.g. OSD
- adolescents, pubertal growth (overload the apophysis (growth plate))
Enthesis
junction between tendon and bone
- fibrocartilage
- enthesopathy = inflammation, compression, autoimmune, etc.
PARS
- largely in adolescents
- load through spine with too much extension (repetitive)
- can lead to fracture
- pain, affects nervous system
Types of repetitive tendon sport injuries
tendinopathy
Tendinopathy
Umbrella term used for tendon problems
- Mechanism:• Repetitive tensile (or compressive) loading (e.g., sprinting, jumping, changing direction) → repetitive microtraumas• Inadequate recovery between loadings
Tendon Pathology: Cook–Purdam Model
- Reactive tendinopathy• Non-inflammatory, structural changes & thickening of stressed tendon area- Tendon disrepair• Worsening tendon pathology, tendon structure becomes disorganized- Degenerative tendinopathy• Chronic stage
Types of repetitive joint/ligament injuries
Labrum repetitive (overuse) injury, Ligament degeneration, Synovitis, Chondropathy
Synovitis of the Knee vs. Chondromalacia Patella
Synovitis: inflammation of the synovial membrane, necessary for joint lubrication
Chondromalacia patella: "runner's knee" softening and degeneration of the cartilage on the underside of the patella
- biomechanical reasons
Types of repetitive muscle/fascia injuries
DOMS, Fasciitis, Chronic compartment syndrome
Chronic Compartment Syndrome
• Exercise induced condition of muscle- Repetitive impact activity (e.g., running), overloading- Swelling and increased pressure causing reduced blood flow and pain• Most commonly in the lower legs- The lower leg has four compartments, and any one or all of them can be affected• Aching, burning, tightness, numbness, weakness• Typically treated conservatively
Types of repetitive bursa injuries
bursitis
Bursitis
- repetitive compression of nerve = inflamed
- bursa: fluid filled sac = cushion = decrease friction
Types of repetitive nerve injuries
Altered neuromechanical sensitivity
Risk Factors for Repetitive Injury (intrinsic and extrinsic)
Intrinsic factors• Previous injury• Biomechanics• Leg length discrepancy• Muscle imbalance• Muscle weakness• Lack of flexibility• Sex• Body composition• Genetic factors
Extrinsic factors• Training load errors• Surfaces• Shoes• Equipment• Environmental conditions• Inadequate nutrition
Treatment of Repetitive Injuries
- Treatment is not only managing the injury.- Essential to address the factors that have contributed to the development of injury!
*EDUCATE: just because symptoms are gone = don't ignore
Prevention of Repetitive Injuries
- Gradually increase training load
- Cross-training- Strength training for the major muscle groups- Correct form & technique- Nutrition- Sleep Rest days- Proper equipment
- Exercise regularly
Medial Tibial Stress Syndrome (MTSS)
• Running and jumping sports• Risk factors (female, increase BMI, too quickly increase loads)• Pain and inflammation along middle-distal third of posteromedial aspect of tibia• Diffuse pain
MTSS: Diagnosis and Treatment
1. History and physical examination (palpation)2. Alternative training3. Correction of malalignment & training problems4. Exercise therapy: strength and flexibility5. Prognosis is good if treated early!
Tibial Stress Fracture
• Running and jumping sports• Risk factors (female, decrease nutrients)• Significant pain during running, often disappears during rest, returns when athlete starts running again• Focal pain
Tibial Stress Fracture: Diagnosis and Treatment
- History and physical examination (Palpation & hop test)- X-ray; MRI- Crutches & Brace & Alternative training- When pain free –> Progressive training- Prognosis is good if diagnosed early!
Low Back Pain (LBP) in the general population
Lifetime prevalence 85%→ Up to 20-30% can become persistent
Low Back Pain (LBP) in athletes
Lifetime prevalence 1-94%→ Time-loss from sport, limitations to performance, decreased quality of life, high costs of treatment
LBP in Adult Athletes
• Non-specific low back pain• Complex combination of intrinsic and extrinsic risk factors
Risk Factors for LBP
• Previous back injury• Family history of LBP• Anatomical structure of the spine• Improper technique• Sleep deficits• Nicotine use• Overloading the structures of the spine• Stress
Degenerative Disc Disease (DDD)
• Heavy stress to the spine• Intervertebral disc degenerates→ pain and other symptoms
DDD: Diagnosis and Treatment
• History, physical and neurological examination• Imaging (e.g., x-ray, MRI)• Conservative treatment = physiotherapy (exercise therapy, e.g., core strength, flexibility)
Ankle Sprain
- Most common sporting injury- Around 80% of ankle injuries are ligamentous caused by sudden inversion/supination
Lateral Ankle Sprain muscles
Lateral structures put under stress• Anterior talofibular (ATF) ligament• Posterior talofibular (PTF) ligament• Calcaneofibular (CF) ligament• Peroneal tendons
Lateral Ankle Sprain grades
• Grade I: partial rupture of ATF, PTF or CF• Grade II: total rupture of one of the three ligaments or partial rupture of two ligaments• Grade III: total rupture of two ligaments
Mechanism of Lateral Ankle Sprain
• Sudden excessive supination• Sudden excessive inversion• 130 – 180 ms after initial foot contact
Diagnosis and Treatment of lateral ankle sprain
• History and physical examination (Palpation)• X-ray• Weight bearing after 24-48 hours (using crutches or brace)• Grade I and II: brace, taping• Grade III: immobilization• Early functional treatment• Progressive exercise therapy
Medial Ankle Sprain
Medial structures put under stress• Deltoid ligament• Sometimes combination with malleolar fractures or syndesmosis injury• Tibialis posterior and toe flexor tendons
Medial Ankle Sprain mechanism
excessive eversion
Diagnosis and Treatment medial ankle sprain
- History and physical examination (palpation)- X-ray
- Brace, sometimes medial arch support- Functional treatment in the same manner that for lateral ankle - ligament injuries- Prognosis is good, but healing takes about twice as long (or more) than for lateral ankle sprains
Prevention of Recurrent Ankle Sprains
Braces?
EXERCISE (proprioception, strength)
Balance training programs/NMT and ankle sprains
- Balance training programs 36% in ankle injuries- NMT programs 50%
Syndesmosis Injury
• High ankle sprain• External rotational trauma• Sprain of syndesmotic ligaments that connectthe tibia and fibula- Partial or complete rupture of syndesmosis- Sometimes rupture of anterior tibiofibular ligament
Mechanism of High Ankle Sprain
• Forced external rotation• High-risk sports: Downhill skiing, football, rugby
Diagnosis and Treatment syndesmosis injury
• Diagnosis: History & Physical examination (palpation); X- ray, MRI• Partial rupture – Walking cast/boot (2 weeks or more)• Complete rupture – surgery, cast/boot (6 weeks)• Progression of rehabilitation when near pain free
*pain in the front and external rotation = HAI
Sprained Ankle Complications
- Increased risk for recurrent injuries- An unstable joint (chronic ankle instability)- Ankle joint osteoarthritis- Persistent pain
Chronic Ankle Instability
• Instability from repeated inversion trauma• Feeling that the ankle is ‘giving way’ on the lateral side• Treatment- Brace- Balance and strength- Surgery
*usually conservative treatment
Osteochondral Fractures and Chondral Injuries
• Usually occur in association with ankle sprains
• Recurrent pain, stiffness and or locking
• MRI• Cast/brace (6-8 weeks) and rehabilitation
• Surgery
• May progress to ankle joint
- osteoarthritis
Osteoarthritis (OA)
- Degeneration of articular cartilage in synovial joints
- Disease of the whole joint (cartilage, bone, ligaments, tendons, synovium and meniscus)
*pain, stiffness, decrease mobility, joint failure
*bone thickens, osteoformation (extra bone), degeneration of ligament
Facts about OA
- OA is the most common arthritis- Found in Hip, knee and ankle- More common in females than males- Prevalence increases with age- Popping/cracking, stiffness, loss of flexibility, pain, swelling, bone spurs- Disability, inactivity, comorbidities, poor quality of life, mortality- There is no cure for OA
Causes of OA
OA is a multifactorial disease
**Aging and trauma are the main risk factors
Other contributing factors:
- genetics
- obeisity
- sex/hormones
- environment
Why are more and more younger adults getting OA?
intraarticular injuries are on the rise.
Economic impact of OA
- The number of total hip & knee replacements is increasing → severe challenge to healthcare system (costs)- In Canada, from 2010 to 2031 the total direct costs of OA is estimated to increase from $2.9 Billion to $7.6 Billion – 2.6-fold increase !
The cost components that will constitute the total direct cost of OA in 2031 are:
• Hospitalization cost $2.9 billion• Outpatient services $1.2 billion• Rehabilitation after surgery $0.7 billion• Drugs & Side-effects of drugs $1.6 billion• Physiotherapy & complementary $1.2 billion care
Diagnosis of OA
- History & Physical examination- Clinical criteria: pain, stiffness, crepitus, bony tenderness and bony enlargement- X-ray (MRI)
Kellgren-Lawrence Grading Scale
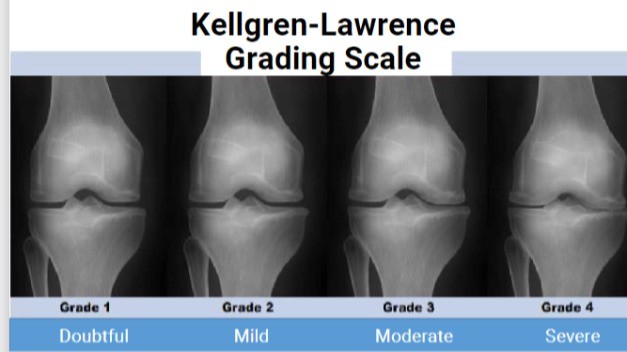
- watch progression
- watch bone get closer (joint narrowing)
Treatment pyramid of OA
Few: surgery
Some: Pharmacological pain relief, orthoses/aids, and passive treatments given by a therapist
All: Education, exercise and weight loss
What is the most effective OA treatment?
Exercise (only treatment to show moderate effect)
**Exercise Therapy is Evidence-based OA Treatment !!!
- helps health care system and patient
- less pain and functional disability at 1yr
- is cost-effective and can delay surgery
Osteoarthritis Bracing
- Also called offloading/unloading bracing- Is used to reduce symptoms such as inflammation and pain in the knee joint
GLA:D
Components• 2-day course for clinicians• 8-week exercise and education program for patients• Data registry
*increase in QOL, decrease pain (27%), 30% increase in PA
Results – One year after GLA:D
Pain: 28% knee, 26% hip
Physical activity: 20% knee, 22% hip
Sick leaves: 42% knee, 21% hip
What is the GLA:D program
Neuromuscular exercises which focus on the muscles controlling the joint as it moves• 10min warm-up & Four exercise stations (two exercises at each station):- Leg strength- Core strength- Functional exercises- Positional exercises (Alignment)• Program is different for each person
Is joint loading harmful for OA?
NO!
• Knee joint loading exercise seems to not be harmful for articular cartilage in people at increased risk of, or with, knee OA (proper loading is critical)• More studies needed
Why is exercise used more for OA?
- Only a few with OA have tried exercise therapy & education prior to surgery- Treatment guidelines and best evidence are not sufficiently applied- WHY ?
• surgeon guidelines
• pain while exercising
• its a buisness
Total knee replacement stats
- Relieves pain in 8/10 patients- 1/10 experience a severe adverse event- Current 90-day care cost for total knee replacement is about $12,000 CAD (Ontario)
*don't last forever = deteriorate = revisal surgery
*muscles surrounding the knee have to support knee joint and stabilize it
Exercise therapy or surgery?
Exercise first approach can delay or avoid surgery
- build muscle strength to support knee before surgery
- knees are worse than hips
- surgery only lasts about 10yrs
Post-Traumatic Osteoarthritis (PTOA)

- PTOA arises after joint injury and/or repetitive joint trauma and is associated with recurrent instability- Trauma-initiated joint degeneration that results in permanent and often progressive joint pain and dysfunction- Primarily affects the knee and ankle joints- PTOA causes about 12% of all osteoarthritis cases
What is PTOA triggered by?
- Acute ligament strain- Chronic ligamentous instability- ACL rupture- Meniscus injury- Fracture- Cartilage damageor a combination of these
PTOA after ACL Injury
• Eight years after an ACL injury, 50% of patients display radiological signs of OA• After 15 years, 80% of patients display radiological signs of OA• Within 20 years, nearly all patients display radiological signs of OA• Prevalence of OA does not seem to depend on whether an ACL reconstruction was performed or not
PTOA risk profile
- intra-articular injury, re-injury
- early return to sport
- obesity
- physical inactivity
- poor diet
- muscle weakness
- inaccurate beliefs
- joint dysplasia
Role of exercise in PTOA
- Pain management- Increasing physical activity- Reducing the risk of comorbidities- Improving strength- Improving alignment and gait
Prevention of PTOA
Prior to injury (primary prevention): prevent joint injuries in susceptible populations
Injury to PTOA (secondary prevention): identify and slow down PTOA onset after joint injury
PTOA (tertiary prevention): slow progression and improve function in those with PTOA
Current problems with PTOA treatment/prevention
• Injury prevention is not happening (Primary prevention)!- Injury prevention training programs (strength & technique) can reduce the riskof severe acute knee joint injuries by 50%- Only 3% of coaches apply these programs• Most with ACL injury have immediate surgery
- Only a few with OA have tried exercise therapy & education prior to surgery• Current treatment is to wait until the joint is destroyed and replace it with metal and plastic
Summary of OA
- OA is characterized by degeneration of articular cartilage in synovial joints. Disease of the whole joint.- Symptoms and outcomes: Pain, disability, poor quality of life, comorbidities, mortality- Risk factors: Intra-articular injury, early RTS, obesity, physical inactivity, muscleweakness, fear of movement, poor diet, unrealistic expectations,insufficient exercise therapy, joint dysplasia- Treatment: Education, exercise, weight loss, pharmacotherapy, orthosis, surgery- Role of exercise: Method for reducing pain and comorbidities; exercise can improvestrength, physical activity, alignment and gait