
Hormone synthesis and action (Physiology)
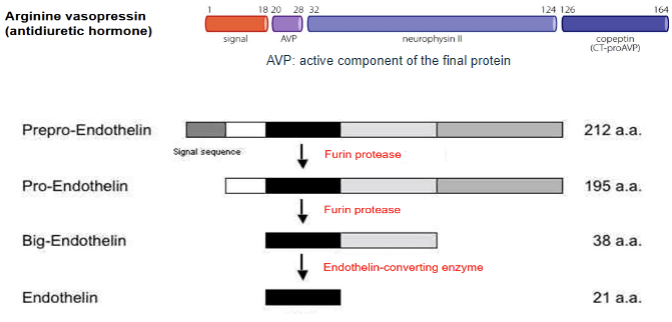
Hormone synthesis and action - Dr Karima Zitouni Session summary In this session we turn to hormone synthesis and action in more detail. We'll cover the three main types of hormones: proteins/peptides, steroids and amino acid derivatives and look at how they are produced in cells and receptor-mediated mechanisms of action. We'll also look at some disorders of hormone signalling to illustrate what can go wrong when normal physiology is disrupted. One example, shown in the image on the right, is a goitre (swelling of the thyroid gland in the neck) which occurs as a result of abnormal thyroid hormone signalling. We'll look at this and also other examples, such as abnormalities resulting from peptide and steroid hormone action, too. Learning outcomes By the end of the lecture, you should be able to: Outline the synthesis of peptide, steroid and thyroid hormones Know that peptide hormones act on cell surface receptors and stimulate cell signalling pathways Know that steroid and thyroid hormones cross cell membranes and act on intracellular receptors Understand that peptide, steroid and thyroid hormones can activate gene transcription Know selected examples of diseases resulting from abnormalities in hormone synthesis and action for peptide, steroid and thyroid hormones Session resources Download the slide set here: KZHormone Synthesis and Action 23-24-1.pptxDownload KZHormone Synthesis and Action 23-24-1.pptx Session Resources: The lecture is divided into 2 recordings Lecture Recording part 1 Lecture Recording part 2 Additional resources The textbook Clinical Endocrinology by Saffron Whitehead (Scion Publishing) is a useful text and is available from the library. Session conclusion Check you've understood important concepts from this unit by answering these questions. Can you describe, in outline only, the synthesis of peptides, steroid and thyroid hormones? Do you know how these three classes of hormones act on their receptors, in outline? Can you explain what can go wrong with hormone synthesis and action, using the examples provided in the unit, for peptides, steroids and thyroid hormone signalling? You've now finished the three introductory sessions on Endocrinology!
-
What are the two main categories of hormones based on their chemical structure and synthesis? (2)
✿Peptides and proteins: These hormones are water-soluble and synthesized from large precursor molecules known as prohormones.
✿Steroids and iodinated tyrosines: These hormones are lipid-soluble and synthesized from low molecular weight precursors.
-
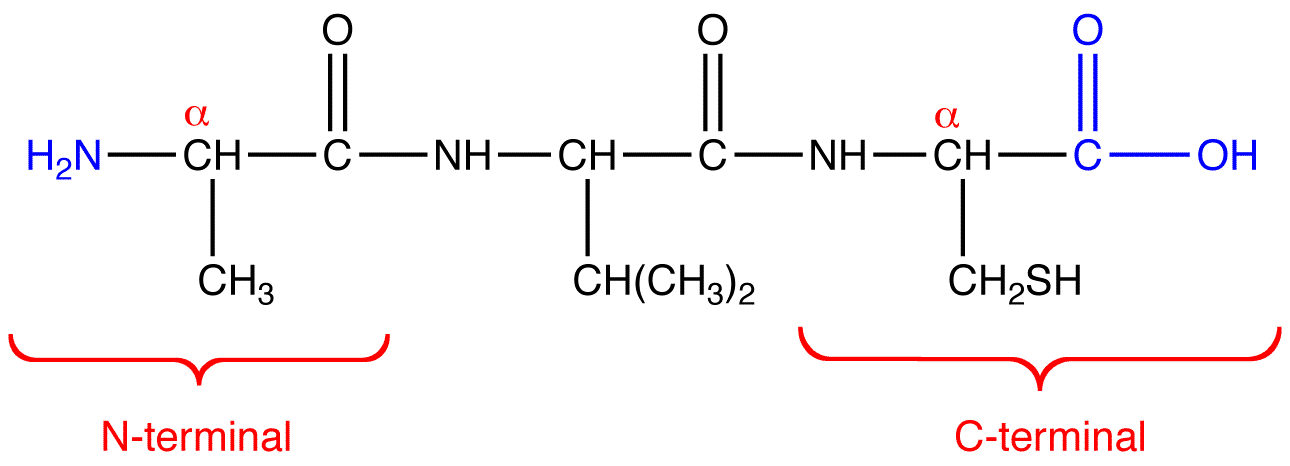
Describe the process of synthesizing protein/peptide hormones by transcription. (4)
a) Transcription of DNA to RNA
b) Post-transcriptional processing RNA -> mature RNA – modifications of 3’ and 5’ ends and excision of introns (splicing)
c) Translation of mature RNA into protein using tRNA to transfer amino acids
d) Post-translational processing cleavage of large pre-prohormones, folding of proteins, addition of sugars (glycosylation)
-
Describe the synthesis of insulin. (5)
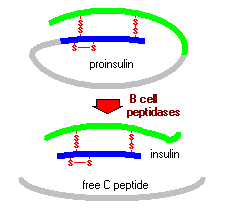
a) Transcription to mRNA: Insulin is transcribed from INS (Insulin) gene within the cell by a complex process of RNA splicing.
b) Excision of introns to messenger RNA.
c) Removal of signal sequence and formation of disulphide bonds in RER.
d) Pre-proinsulin → proinsulin: The signal sequence directs the protein to the rough endoplasmic reticulum, where finally the protein is being produced.
e) Transfer to Golgi apparatus, excision of C peptide and packaging into secretory granules.
-
Picture demonstrating Prohormone processing to active peptide:
-
Explain the synthesis process of large precursor proteins into active hormones. (5)
✿The pre-hormone polypeptide may contain a signalling sequence directing it to the Golgi apparatus.
✿Pre-hormone includes signal peptides at the N-terminus and/or C-terminus, along with hormones and amino acids.
✿The prohormone consists of hormones and amino acids.
✿Pre-hormone acts as the precursor to one or more pro-hormones.
✿Cleavage of proteins varies based on their signal peptides.
-
Describe the synthesis of insulin. (5)
a) Transcription to mRNA: Insulin is transcribed from INS gene within the cell by a complex process of RNA splicing.
b) Excision of introns to messenger RNA.
c) Removal of signal sequence and formation of disulphide bonds in RER.
d) Pre-proinsulin → proinsulin: The signal sequence directs the protein to the rough endoplasmic reticulum where finally the protein is being produced.
e) Transfer to Golgi apparatus, excision of C peptide and packaging into secretory granules.
-
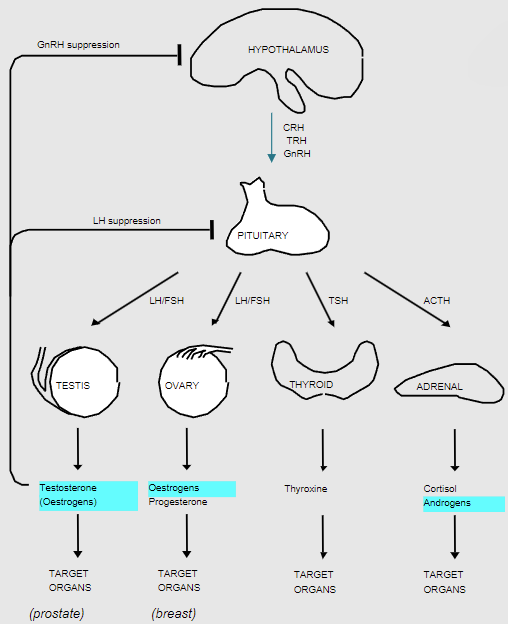
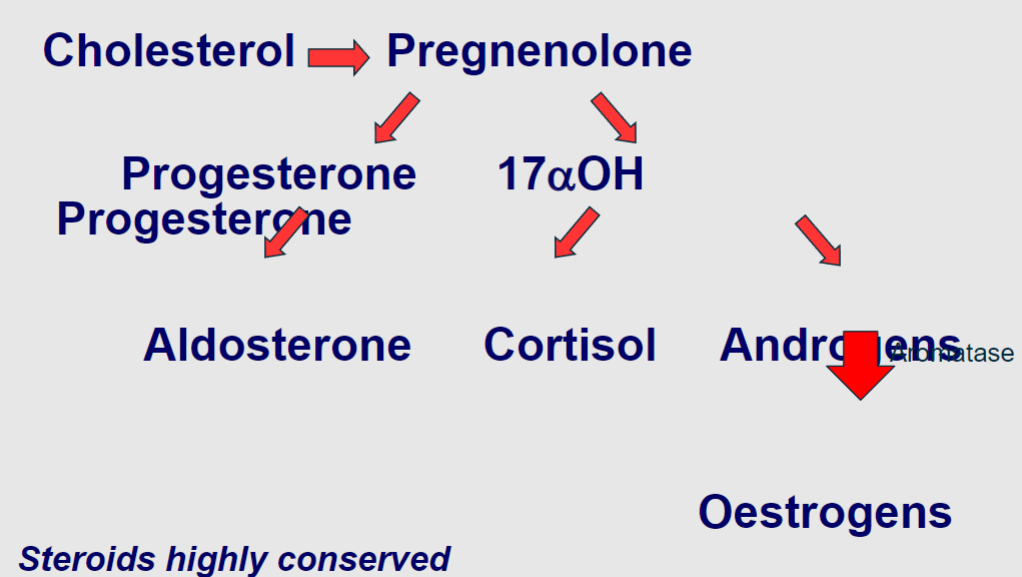
Explain the control of steroid synthesis from cholesterol. (6)
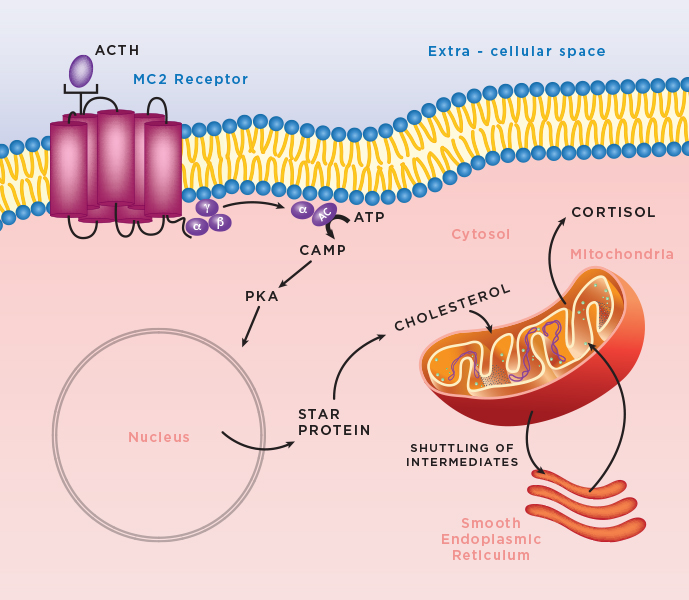
✿Steroidogenesis occurs in Steroidogenic cells.
✿Cholesterol bound to sterol carrier protein is transported to mitochondria.
✿StAR protein transports cholesterol to inner mitochondrial membrane (rate limiting).
✿Cholesterol is converted to pregnenolone by side chain cleavage enzyme, P450scc (rate limiting).
✿Between mitochondria and smooth endoplasmic reticulum, steroids are synthesized by hydroxylase enzymes.
-
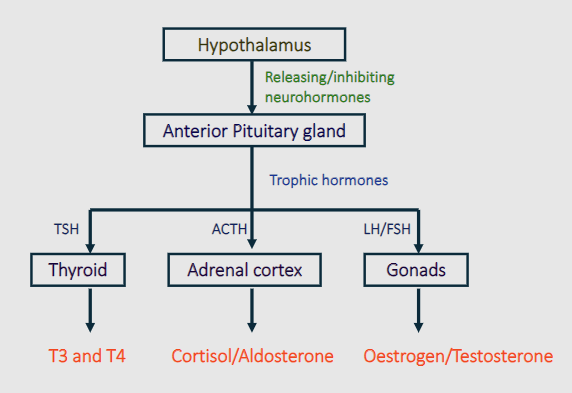
Picture demonstrating how glands are controlled by the hypothalmic-pituitary axis:
-
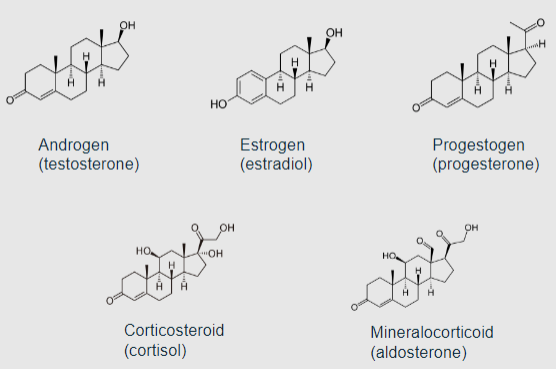
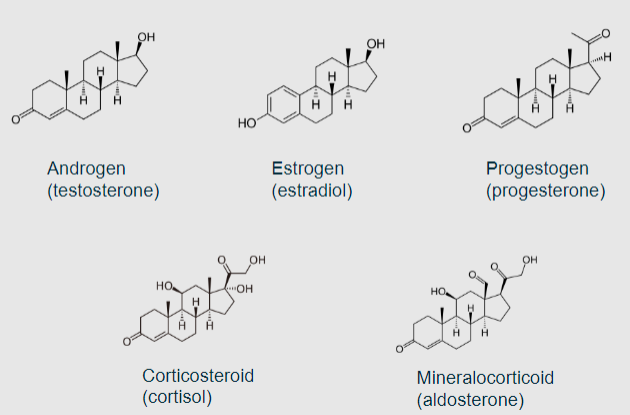
Picture demonstrating Examples of steroid hormones:
-
Picture demonstrating Control of steroid hormone production:
-
Picture demonstrating Steroid synthesis simplified:
-
Describe the synthesis of thyroid hormones. (5)
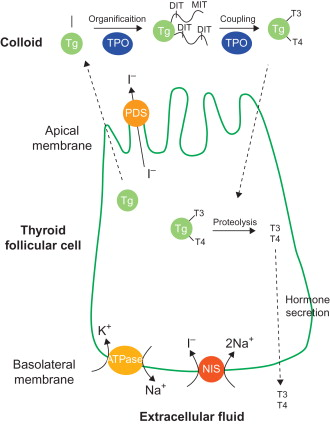
✿Thyroglobulin synthesis: Tyrosine is converted into glycoprotein thyroglobulin.
✿Iodine Trapping: Active uptake of I- across basolateral membrane by Na/I symporter (NIS), stimulated by TSH.
✿Iodide Oxidation: Iodide is oxidized to iodine and covalently bound to tyrosine residues within thyroglobulin, requiring thyroid peroxidase (TPO) and peroxide (H2O2).
✿Iodination of thyroglobulin: Tyrosine residues may be iodinated to form mono-iodotyrosine (MIT) or di-iodotyrosine (DIT).
✿Coupling of iodotyrosine residues: By TPO produces T4 (DIT-DIT) and a smaller amount of T3 (MIT-DIT).
-
Summarize the synthesis of thyroid hormones. (6)
✿Active uptake of iodide into follicular cell
✿Oxidation of iodide by thyroid peroxidase (TPO)
✿Iodination of tyrosine residues of thyroglobulin and apical-colloid interface
✿Storage of thyroglobulin molecules in colloid
✿Uptake of thyroglobulin droplets into follicle cell
✿Release and secretion of T3 and T4 stimulated by TSH
-
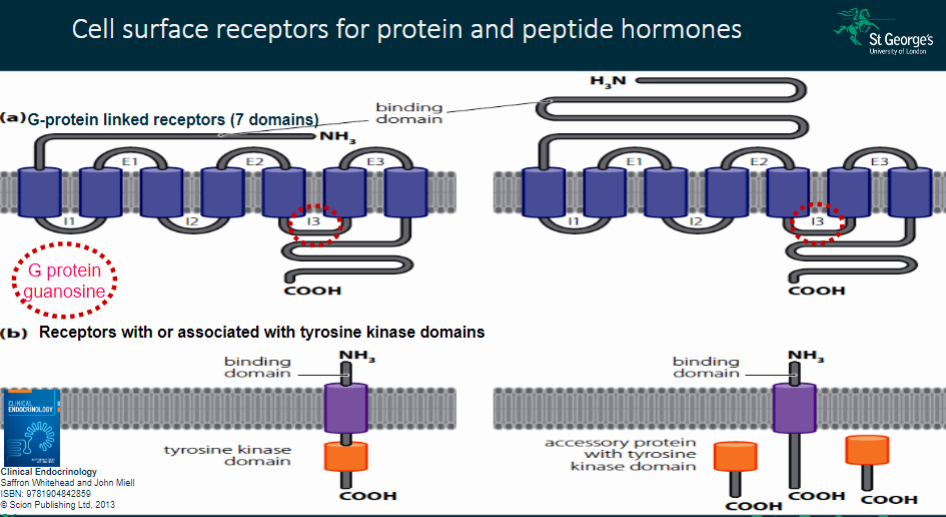
Explain the action of peptide and protein hormones on cell signaling. (3)
✿Water soluble hormones act on cell surface receptors
✿Activate second messengers and/or enzymes
✿Result in cytoplasmic and nuclear effects
-
Picture demonstrating Cell surface receptors for protein and peptide hormones:
-
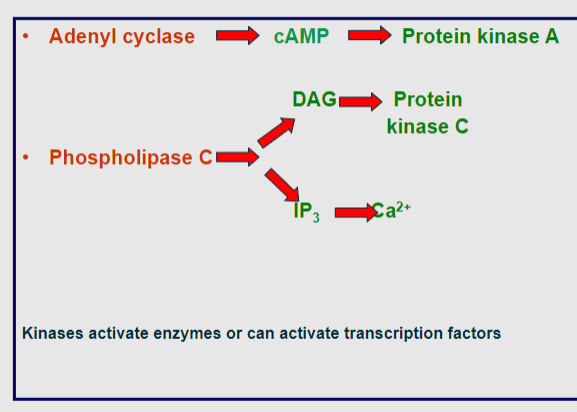
Describe the cell signaling pathway for protein and peptide hormones. (7)
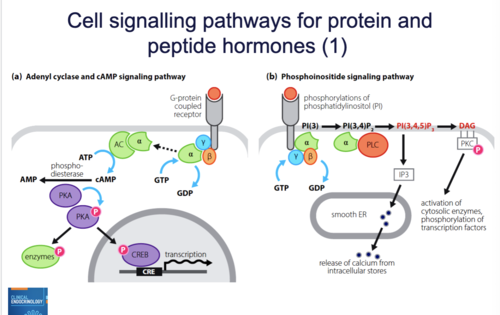
✿Hormone binds to G protein receptor
✿G protein is activated
✿Converts GTP to GDP
✿Alpha subunit dissociates and activates adenylate cyclase (AC)
✿AC produces cyclic AMP (cAMP)
✿cAMP activates protein kinase A (PKA)
✿PKA activates cellular proteins or transcription factors, leading to transcriptional responses
-
Describe the Raf/MEK/ERK pathway in the tyrosine kinase receptor signaling. (5)
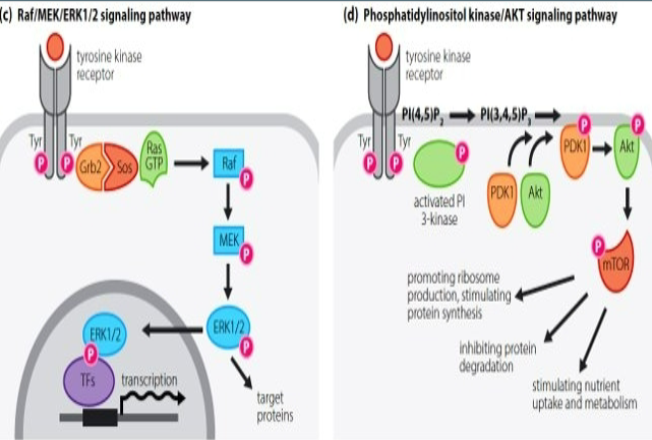
✿Tyrosine residues of the receptor become phosphorylated
✿Intracellular accessory proteins are activated
✿Ras is phosphorylated and activates Raf
✿Raf phosphorylates MEK, which in turn activates ERK
✿Phosphorylated ERK translocates into the nucleus
✿Activates downstream transcription
-
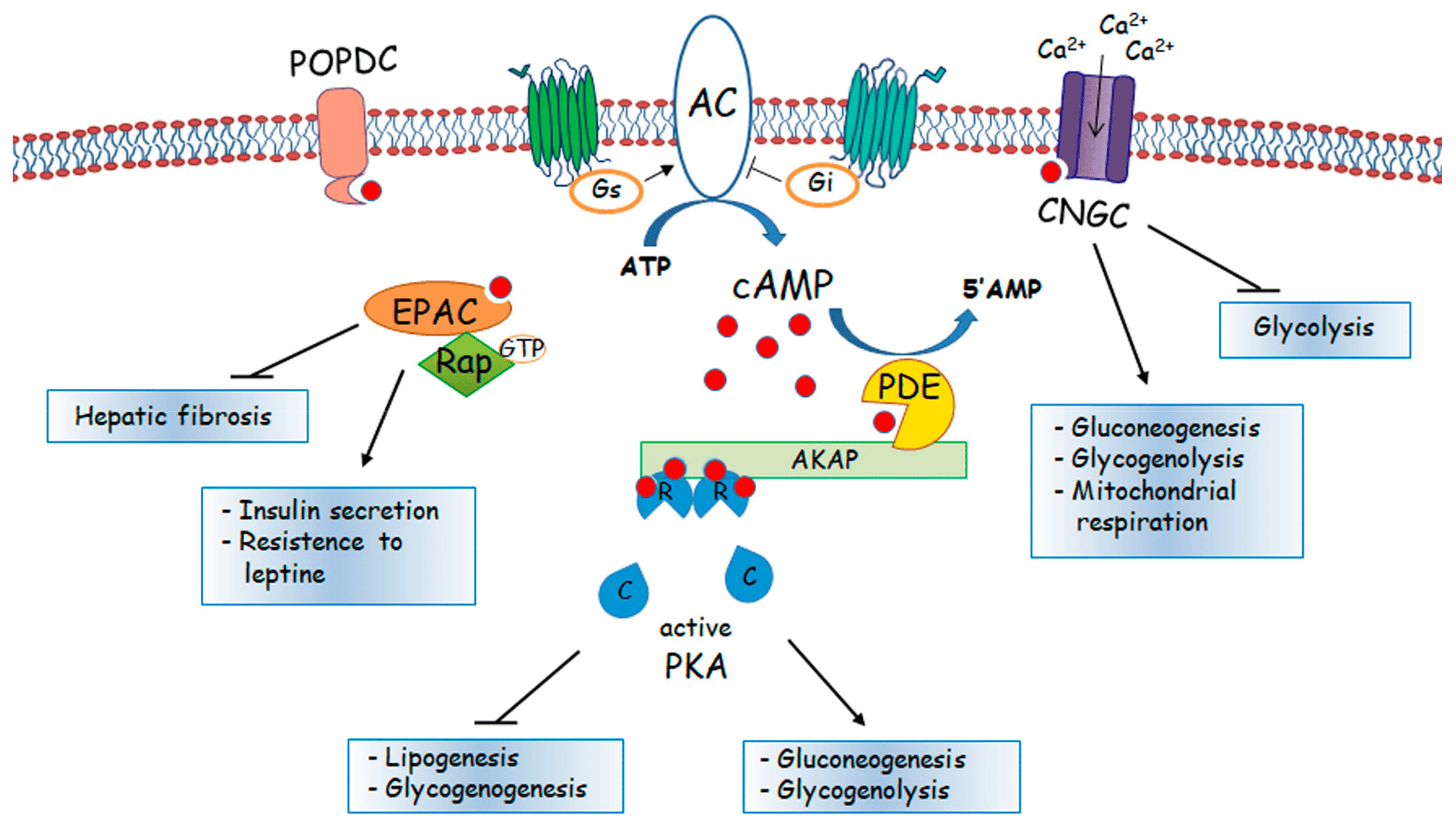
Picture demonstrating the action of cyclic AMP:
-
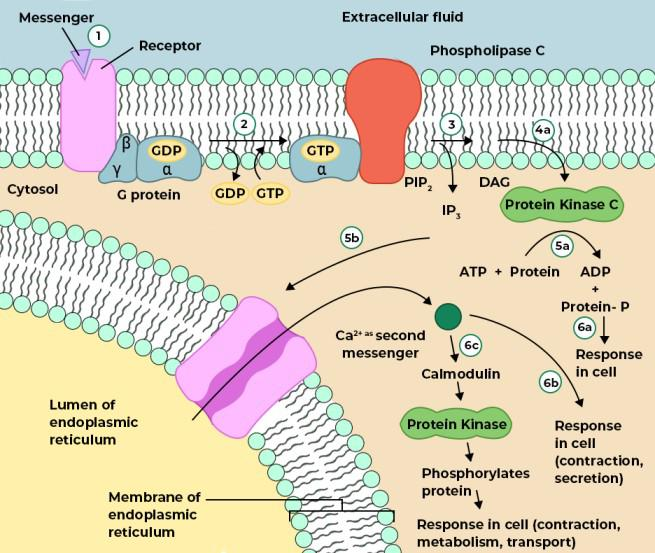
Picture demonstrating the production of IP3 and DAG
-
Picture demonstrating the second messengers in G-protein linked receptors:
-
What are the three Signalling pathways for receptors with tyrosine kinase activity? (3)
• Raf/MEK/ERK pathway
• PI3-Kinase/Akt pathway
• JAK STAT pathway
-
Describe the characteristics of steroid hormones. (2)
✿Steroid hormones are small molecules with a multi-ringed structure.
✿They are lipophilic, allowing them to easily penetrate cell membranes.
-
Picture demonstrating examples of steroid hormones:
-
How do steroid hormones exert their effects once inside the cell? (2)
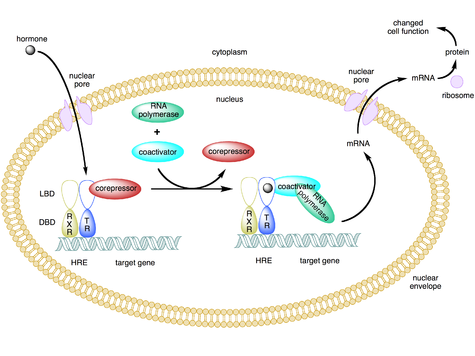
✿Steroid hormones bind to receptors, known as nuclear receptors.
✿These receptors may initially be found in the cytoplasm or nucleus, but their effects are exerted in the nucleus.
-
What are the systemic effects of steroid hormones? Provide examples for both females and males. (4)
✿In females, estrogen controls the menstrual cycle, breast tissue development, fertility, reproductive organ development, secondary sexual characteristics such as body hair, etc.
✿In males, testosterone controls reproductive and supportive organs like the prostate, development of sexual characteristics such as deepening of the voice, body hair, etc.
✿Corticosteroids regulate various physiological and immune pathways.
✿Mineralocorticoids regulate salt and water balance.
-
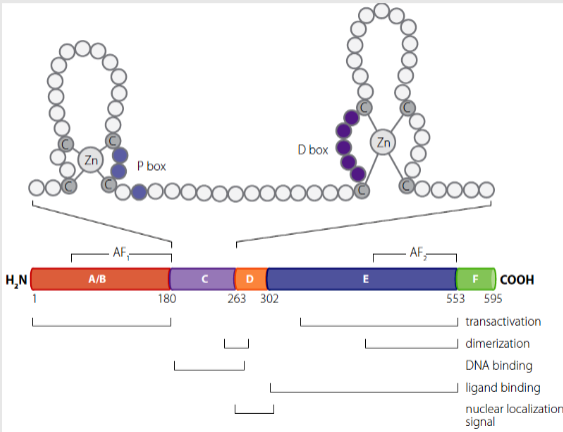
Describe the structure and function of steroid hormone receptors. (5)
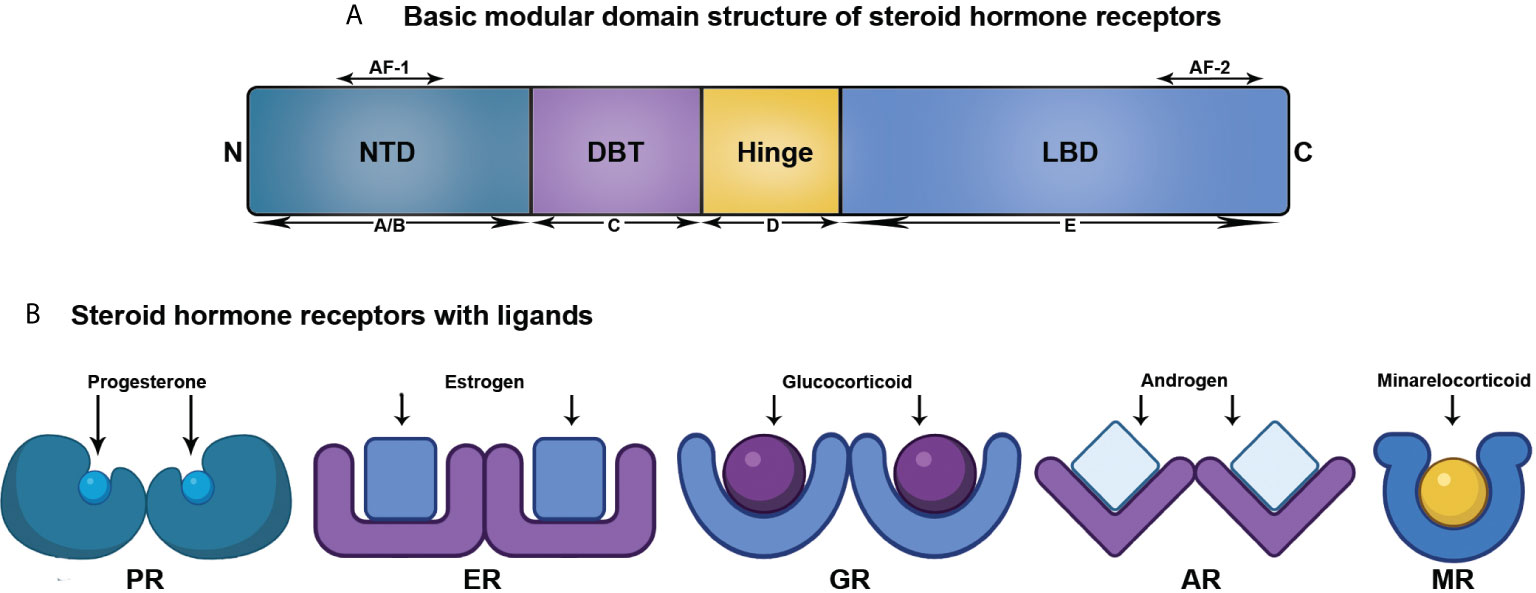
✿Steroid hormone receptors are transcription factors.
✿They possess different functional domains, labelled A to F.
✿The C domain serves as the DNA binding region and is highly conserved.
✿Both the A/B domains and E/F domains exhibit transcriptional activity (AF-1/AF-2).
✿Continual discovery of different steroid receptors is ongoing.
-
What are the key characteristics of the Nuclear Receptor? (4)
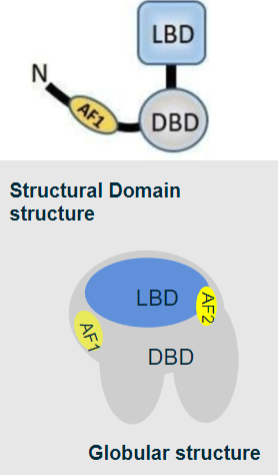
✿Ligand binding domain (LBD): Binds specific steroid molecules with high affinity.
✿DNA binding domain (DBD): Binds specific DNA sequences.
✿Activation function domain (AF1 & 2): Recruits gene activation machinery; some receptors have a secondary AF2 domain towards the C-terminal.
✿Shared basic domains and structure among major nuclear receptors.
-
Picture demonstrating the basic structure of steroid receptors:
-
Describe the structure of the DNA binding region in the C domain. (2)
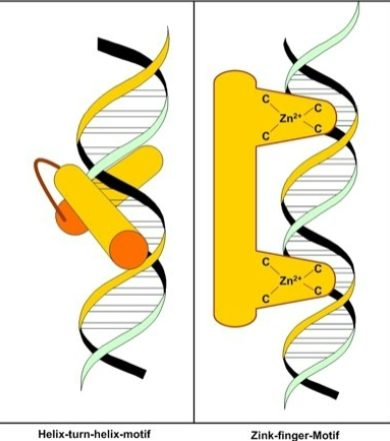
✿The DNA binding region consists of 2 zinc fingers.
✿These zinc fingers can slot into the helix of the DNA.
-
Outline the process of hormone action for receptors located within the cytoplasm. (8)
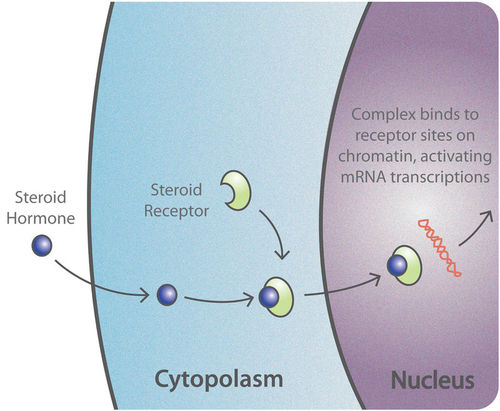
✿Hormone crosses cell membrane through diffusion or facilitated transport.
✿Heat shock proteins, which chaperone the receptor, dissociate from the receptor upon hormone binding.
✿Hormone binds to the receptor in the cytoplasm, leading to conformational changes in the receptor.
✿Dimerization occurs when two hormone-bound receptors come together to form a functional complex.
✿The dimerized receptors, now activated, translocate from the cytoplasm to the nucleus.
✿Within the nucleus, the receptor complex binds to specific DNA sequences called hormone response elements (HREs) located in the promoter regions of target genes.
✿This binding initiates transcription of the target genes, facilitated by the recruitment of additional transcription factors and coactivators.
✿Transcription of the target genes results in the synthesis of mRNA, which is subsequently translated into proteins, ultimately mediating the cellular response to the hormone.
-
Describe the synthesis and action of protein and peptide hormones compared to steroids and thyroid hormones. (4)
✿Protein and peptide hormones are synthesized from genes encoded in the genome, while steroids and thyroid hormones are synthesized from other chemical compounds like tyrosine, cholesterol, and fatty acids.
✿Protein and peptide hormones function as chemical messengers.
✿Steroids and thyroid hormones also function as chemical messengers.
✿Protein and peptide hormones typically act through cell surface receptors, while steroids and thyroid hormones often act through intracellular receptors.
-
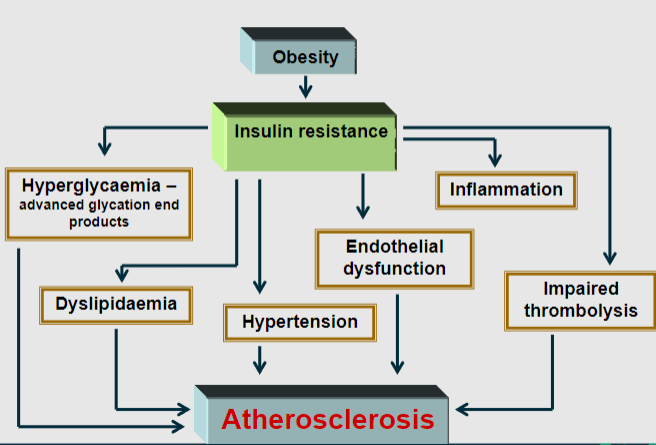
Explain the cascade of events linking obesity to cardiovascular risk factors and atherosclerosis. (6)
✿Obesity is a primary driver of insulin resistance, characterized by diminished responsiveness of tissues to insulin.
✿Insulin resistance often leads to hyperinsulinemia, elevated insulin levels in the blood.
✿Hyperinsulinemia contributes to hypertension, or high blood pressure, through various mechanisms including increased sodium reabsorption and sympathetic nervous system activation.
✿Insulin resistance and hyperinsulinemia also promote endothelial dysfunction, impairing the ability of blood vessels to relax and dilate properly.
✿Endothelial dysfunction leads to impaired thrombolysis, making blood clots more likely to form.
✿Insulin resistance is associated with dyslipidemia, an abnormal lipid profile characterized by elevated triglycerides and decreased high-density lipoprotein (HDL) cholesterol.
-
Picture demonstrating how Obesity drives the development of insulin resistance, which is associated with cardiovascular risk factors and atherosclerosis:
-
Discuss the consequences of aromatase deficiency in both men and women. (4)
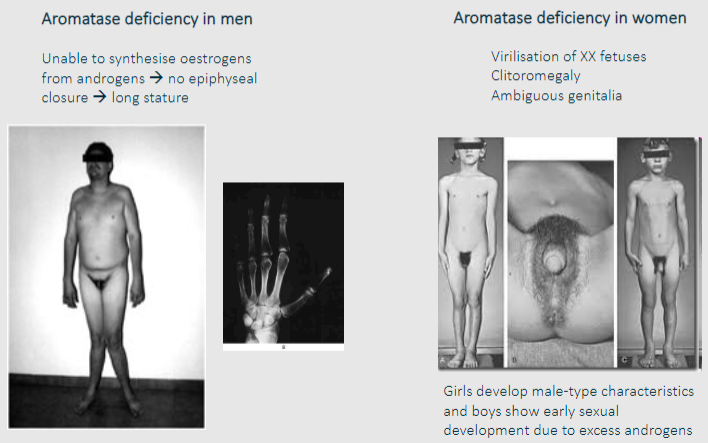
✿In men with aromatase deficiency, the inability to convert androgens into estrogens leads to a lack of estrogenic effects. This results in a failure of epiphyseal closure, leading to abnormally long stature.
✿Due to excess androgens in aromatase-deficient individuals, girls may develop male-type characteristics such as increased body hair growth (hirsutism) and deepening of the voice, while boys may experience early sexual development.
✿In XX fetuses with aromatase deficiency, excess androgens can cause virilization, leading to clitoromegaly (enlarged clitoris) and ambiguous genitalia.
✿However, the consequences of aromatase deficiency in women may vary depending on the severity and timing of the deficiency, potentially leading to a spectrum of phenotypes ranging from mild to severe virilization.
-
Explain the concept of resistance to hormone action and provide an example disorder caused by inactivating mutations of a steroid receptor. (3)
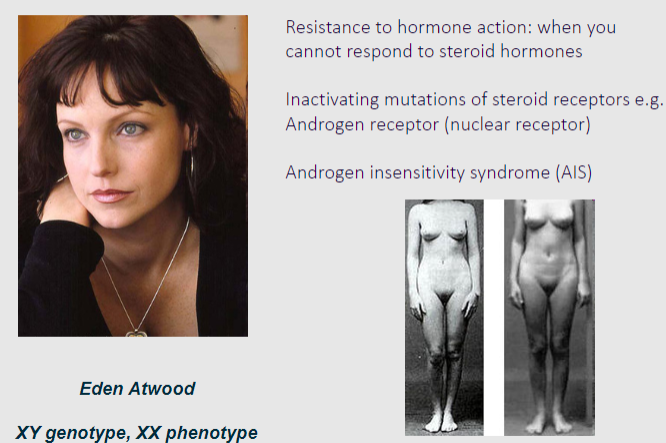
✿Resistance to hormone action refers to the inability of cells to respond to the effects of steroid hormones despite normal hormone levels.
✿This resistance can occur due to inactivating mutations in steroid receptors, which prevent the receptors from properly binding to their hormone ligands and initiating the downstream signalling cascade.
✿One example of a disorder resulting from inactivating mutations of a steroid receptor is Androgen Insensitivity Syndrome (AIS), which is caused by mutations in the androgen receptor gene.
✿In AIS, individuals with XY chromosomes have impaired responsiveness to androgens, leading to incomplete masculinization of external genitalia and, in severe cases, development of female secondary sexual characteristics.
-
Explain the disorders associated with thyroid hormone signalling and the causes of goitre. (4)

Hypothyroidism:
✿Lack of iodine in the diet results in a deficiency of thyroid hormones T3 and T4.
✿Symptoms may include fatigue, weight gain, cold intolerance, and goitre (enlargement of the thyroid gland).
Hyperthyroidism:
✿Conditions such as Graves' disease and thyroid adenoma lead to excessive production of thyroid hormones.
✿Symptoms may include weight loss, rapid heartbeat, heat intolerance, and goitre.
Goitre Causes:
✿Iodine deficiency: Prevents the synthesis of thyroid hormones, leading to goitre.
✿Autoimmune disorders: Conditions like Graves' disease can cause the immune system to produce antibodies that stimulate the thyroid gland, resulting in goitre.
✿Thyroid adenoma: Benign tumours of the thyroid gland increases thyroid hormone production.
-
Describe Graves' disease and its impact on thyroid hormone signaling. (2)
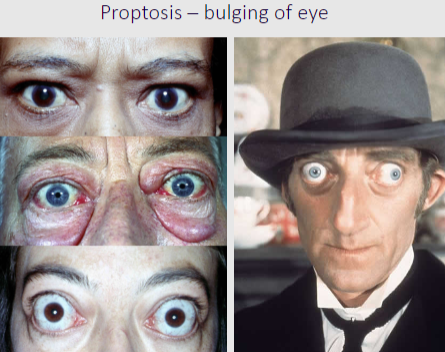
✿Graves' disease is an autoimmune disorder characterized by the production of autoantibodies that target the thyroid-stimulating hormone (TSH) receptor.
✿These autoantibodies mimic the action of TSH, leading to excessive stimulation of the thyroid gland and subsequent overproduction of thyroid hormones (hyperthyroidism).
✿In addition to hyperthyroidism, Graves' disease can also cause eye problems, known as Graves' ophthalmopathy, due to inflammation and swelling of tissues behind the eyes.
-
Explain the impact of an activating mutation of the TSH receptor on thyroid hormone signalling. (3)
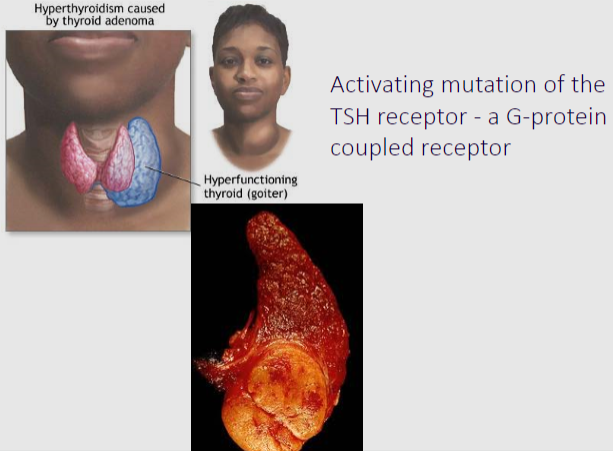
✿An activating mutation of the TSH receptor results in its continuous stimulation, regardless of the presence of TSH.
✿This constant activation leads to uncontrolled production and release of thyroid hormones, causing hyperthyroidism.
✿The mutation essentially bypasses the normal regulatory mechanisms of thyroid hormone synthesis and secretion, resulting in dysregulated thyroid function.
-
Explain the importance of hormone balance for maintaining homeostasis. (4)
✿Hormone balance is crucial for maintaining homeostasis, as both hormone deficiency and overactivity can lead to developmental abnormalities and disease.
✿Hormones regulate various physiological processes in the body, including growth, metabolism, reproduction, and immune function.
✿Loss of hormone action due to deficiency or receptor insensitivity can result in developmental abnormalities and diseases, while excessive hormone levels can also lead to disorders.
✿Therefore, maintaining a fine balance of hormone levels is essential for optimal health and proper functioning of the body's systems.
-
Explain Androgen Insensitivity Syndrome (AIS) in terms of aetiology, symptoms, and hormone levels. (3)
Androgen Insensitivity Syndrome (AIS):
✿Aetiology: Lack of functional androgen receptors, resulting in a complete lack of response to testosterone.
✿Symptoms: XY embryos develop as phenotypic females, with underdeveloped or absent external genitalia. Some individuals may not realize they are genetically male until internal examination reveals developmental anomalies. Often associated with infertility.
✿Hormone Levels: Testosterone levels are typically normal or high.
-
Explain Androgen Deficiency (Hypogonadism) in terms of aetiology, symptoms, and hormone levels. (3)
Androgen Deficiency (Hypogonadism):
✿Aetiology: Insufficient production or action of androgens.
✿Symptoms: In pre-pubertal males, it can cause delayed puberty and developmental abnormalities such as lack of secondary sexual characteristics (e.g., voice deepening, muscle growth). In older males, symptoms may include loss of libido, impotence, and loss of muscle mass.
✿Hormone Levels: Testosterone levels are low.

