-
Homeostasis
1. Any self-regulating process by a biological system to maintain stability.
2. Adjusting conditions that are optimal for survival.
5. 5 Functions: Temp, BGL, BP, Toxins, pH
-
Homeostasis Considerations
1. Balance of fluids and electrolytes, body is making constant adjustments to maintain balance.
2. Recognize changes early. May be obvious or subtle.
3. Timely assessments important.
-
Fluid
1. Adults approx 60% of weight is fluid
2. 2/3 = intracellular
3. 1/3 = extracellular
4. Plasma is intravascular, including lymph
5. Transcellular is any fluid in epithelial-lined spaces such as pericardial, CSF, synovial, pleural, intraocular.
-
Fluid Functions
1. Regulate temperature
2. Moisten tissues in eyes, nose, mouth
3. Protects body organs and tissues.
4. Carries nutrients and oxygen to cells.
5. Lubricates joints
6. Lessens burden on kidneys and liver by flushing out waste.
7. Dissolves minerals an nutrients for accessible to your body.
-
Fluid Balance
1. Intake: 2500mL per 24 hours
2. Output: Sensible loss: 500-1000mL per 24hr, Insensible loss: 1500mL per 24 hr
3. Sensible can be measured and tracked.
4. Insensible is unable to track/measure.
-
Fluid Gain and Loss: Healthly Adult
1. Kidneys: average output 1mL/kg/hr
2. Skin: sweat can be affected by fever, exercise, burns more fluid loss
3. Lungs: give off fluid in vapor, RR, dry/wet environment, exercise
4. GI tract: lose about 200 mL daily in GI tract, diarrhea or surgery
-
Fluid Transport Mechanisms
Diffusion – particles move from area of high concentration to low concentration
Osmosis – water particles move from area of high solute concentration to low concentrations
Filtration – response to pressure, hydrostatic pressure exerted on walls of vessels pushes fluid inside cells
Osmotic pressure – pressure exerted by solutes, minimum pressure which needs to be applied to a solution to prevent the inward flow of its pure solvent across a semipermeable membrane, pulls fluid out of intracellular into extracellular
-
Fluid Spacing
1. First - normal fluid distribution
2. Second - Excessive accumulation of fluid in interstitial spaces. (Edema, fluid collecting in-between cells)
3. Third - Fluid shifts from intravascular to a "third" transcellular space (serous cavity), ascites, pleural infusions, *can be dehydrated with fluid spacing
-
Water Balance Regulation
Hypothalamic Regulation: changes in blood osmolality and triggers thirst or antidiuretic hormone (ADH) release in response to imbalances.
Pituitary Regulation: pituitary gland, specifically the posterior pituitary, in releasing antidiuretic hormone (ADH) to conserve water by reducing urine output when the body's water levels are low.
Adrenal-Cortical Regulation: relates to the influence of the adrenal cortex, which secretes aldosterone to increase sodium reabsorption and water retention in the kidneys, thus helping maintain water balance.
-
Water Balance Regulation 2
Renal System: regulating water balance by filtering blood, reabsorbing essential water and solutes, and excreting excess water as urine, under the control of hormones like ADH and aldosterone.
Cardiovascular System: water balance regulation by ensuring adequate blood circulation to maintain blood pressure and transport hormones like ADH and aldosterone, which affect water reabsorption in the kidneys.
GI System: water balance regulation by absorbing water from ingested fluids and eliminating excess water through feces, contributing to overall fluid balance in the body.
-
BNP (B-type natriuretic peptide)
a hormone produced by the heart in response to stretching of the heart muscle cells, especially in the ventricles. It plays a crucial role in regulating fluid balance and blood pressure. When there is an increase in blood volume or pressure in the heart, the heart releases BNP to promote natriuresis, which is the excretion of sodium and water by the kidneys. This helps to reduce blood volume and lower blood pressure.
-
Hypovolemia versus Hypervolemia
1. Hypovolemia: fluid volume deficit, loss of ecf exceeds intake, increased osmolality, concentrated labs, dehydration
2. HYPERvolemia: fluid volume excess, abnormal retention of water and sodium led to expansion of ecf, decrease osmolality, dilute labs.
-
Hypovolemia verus Hypervolemia Findings
1. Hypervolemia – high intake low output, HTN, tachyC, wob inc, fluid in pleural space (crackles), High Na diet, edema/moist skin, HCT lower (diluted)
2. Hypovolemia – low intake, low output, hypoBP, tachyC, inc RR, confusion, Not enough fluid intake, dry poor skin turgor, thirst, thready pulse, HCT elevated
3. To start to have peripheral edema = 5 Liters gains. Puffy edema = 10 Liters gain
-
Electrolyte Composition
1. Electrolytes dissociate or split into ions when placed into water.
2. Ions - electrically charged.
3. Cations - positively charged (Na, K, Ca, Mg)
4. Anions - negatively charged (HCO3, Cl, PO4)
5. ECF - main cation is Na and main anion is Cl-.
6. ICF - main cation is K+ and main anion is PO4-.
-
Electrolyte Maintenance
1. Determine those at risk / manage underlying cause.
2. Assessment: VS, HR, rhythm, LOC, i/o, muscle strength and movement, weight
3. Lab (serum and urine): electrolytes, osmolality, bun/creatine, BNP (elevation indicates need to removal excess fluid)
-
Healthy Electrolyte Balance versus Abnormal
1. Healthy: VS wnl, AxO4, equal i/o, strength/movement wnl, stable weight
2. Abnormal: tachycardia, dysthymias, irregular rhythm, confusion/disorientation, weak, muscle twitching, seizure and unresponsiveness. Inadequate or excessive output. Weight gain or loss.
3. Confusion and weight gain first clues of abnormal electrolyte imbalance.
-
Potassium
1. K = 3.5-5 mEq/L
2. Regulates ICF
3. Promotes nerve impulse transmission
4. Skeletal, smooth, and cardiac muscle contractions
5. Acid/base balance: hydrogen ions exchange with potassium ions in ICF.
6. Allows glycogen to be deposited in muscle and liver cells.
7. Excess K eliminated, 80% kidneys daily, 20% bowel movements and sweat.
8. Daily replacement K for those on wasting diuretics.
-
Hypokalemia causes
1. K < 3.5 mEq/L
2. Decreased intake
3. Increased renal excretion / kidney disease
4. Movement of K from ECF to ICF (glucose metabolism)
5. GI disturbances (diarrhea/vomit)
6. Meds - (insulin, diuretics, laxatives, digoxin)
7. Low Mg levels (when mg or k gets low, lower together)
-
Hypokalemia s/s
1. Kalemias do the same as prefix, except HR and urine output.
2. Usually appears at < 3.0 mEq/L
3. Cardiac arrhythmias and EKG changes.
4. Decreased DTR.
5. Polyuria and nocturia
6. Priority: Lethal cardiac dysrhythmias, cardiac arrest, coma
-
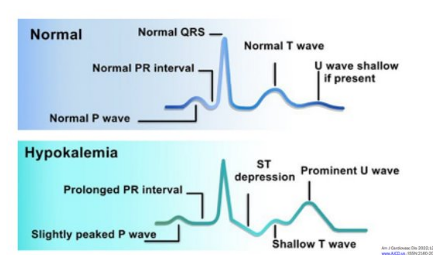
Hypokalemia EKG presentation
-
Hypokalemia Interventions
1. Oral / diet replacement (fruits, bananas, spinach, salt substitutes are high in K)
2. Salt sub w/ K
3. Parenteral replacement: can only give 10mEq/hr , peripheral IV potassium must be diluted usually 1liter of fluid, concerns with burning swelling irritation.
-
Hyperkalemia causes
1. K > 5.0 mEq/L
2. increased intake
3. impaired excretion (renal failure, dehydration)
4. Movement from ICF to ECF (cell lysis, cancer/burns)
5. Acidosis
6. Potassium sparing diuretics
7. Adrenal insufficiency (low aldosterone, which promotes the excretion of dietary potassium)
-
Hyperkalemia S/s
1. Kalemias do the same as the prefix except for HR and urine output.
2. EKG changes, irregular pulse, arrhythmias
3. Anxiety, irritability
4. Muscle weakness, flaccid paralysis, paresthesia
5. GI: abnormal cramping, diarrhea
6. Metabolic acidosis
7. Priority: V fib, respiratory arrest, cardiac arrest
-
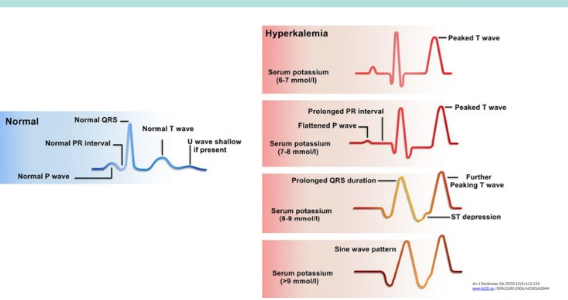
Hyperkalemia EKG
-
Hyperkalemia Interventions
1. Prevent by identifying those at risk / identify underlying cause
2. Decrease oral / parenternal intake
3. Meds: diuretics, kayexalate (potassium binding, works in Large intestine)
4. IV insulin with glucose forces K into cells.
5. Calcium gluconate IV to decrease cardiac excitability
6. Dialysis
-
Calcium
1. 8.2 - 10.2 mg/dL
2. 99% located in skeletal system
3. Daily intake needed
4. Maintains bones and teeth
5. Essential component of nerve/muscle/cardiac contractions
6. Blood clotting: converts prothrombin to thrombin
-
Hypocalcemia causes
1. < 8.2 mg/dL (Vit D and Ca coincide)
2. Renal failure
3. Decreased intake, malabsorption, Vit D deficit
4. Loss of Ca: alcoholism, excessive diarrhea, aggressive diuretic therapy
5. Endocrine disorders and parathyroidectomy
6. Low Mg (reduces amount of PTH released)
7. Hyperphosphatemia (inverse relationship with Ca)
8. Meds - aminoglycosides, anticonvulsants, loop diuretics, bisphosphonates (tx osteop)
-
Hypocalcemia S/s
1. Calcemias do the OPPOSITE as the prefix, no exceptions.
2. Below 7 is critical, tetany and stridor, 6 can cause death.
3. Convulsions: involuntary jerking/contractions/spasms- cramps and tetany.
4. VS, arrhythmias, hypotension, ECG
5. Seizures
6. Trousseau's sign - bp cuff, Chvostek's sign-face
7. Increased peristalsis and diarrhea
8. Numbness and tingling of lips and extremities
9. Osteoporosis
10. Priority: seizures, laryngospasm w/ stridor, ventricular tachycardia
-
Hypocalcemia Interventions
1. Correct level and treat cause, recheck q4-q6.
2. Administer IV calcium gluconate.
3. Increase dietary intake of Ca and Vit D.
4. Monitor EKG
5. Validate albumin level - if low may not need calcium. (when albumin is low, skews Ca results, ionized Ca level for more accurate results)
-
Hypercalcemia Causes
1. Increased intake
2. Metastatic disease processes affecting bones
3. Endocrine disorders: hyperparathyroidism, adrenal insufficiency
4. Kidney disease, decreased excretion
5. Meds: Antacids, Thiazide diuretics, glucocorticoids
-
Hypercalcemia S/s
1. Calcemias do the OPPOSITE as the prefix, no exceptions
2. Weakness - can be profound
3. Lethargy, confusion, personality changes
4. Decreased reflexes
5. Constipation
6. N/v
7. Bone pain, fracture
8. Polyuria, polydipsia, calcium stones
9. ECG changes - arrhythmias, bradycardia, shortened QT/ST intervals
10. Priority: coma, death
-
Magnesium
1. 1.6-2.6 mEq/L
2. 1/3 bound to proteins
3. Essential for metabolism of carbs and proteins
4. Regulates neuromuscular function and electrolyte balance
5. Cardiovascular: acts peripherally to produce vasodilation and decrease peripheral resistance
6. Balances phosphorus and calcium levels.
-
Hypomagnesemia causes
1. < 1.6
2. Symptoms usually start at <1.3
3. Alcoholism
4. Prolonged GI issues: diarrhea, starvation, vomiting's, malabsorption
5. NG tube with prolonged suction
6. Acute pancreatitis
7. Concurrent hypokalemia not responding to replacement
8. Limited intake or increased renal loss
9. Prolonged use of PPIs lead to decreased absorption of Magnesium
-
Hypomag s/s
1. Mag OPPOSITE of prefix without exceptions
2. Neuromuscular irritability (trousseau and chvostek)
3. Tachycardia, HTN
4. hyperactive tendon reflexes
5. Muscle cramps
6. Psychological changes
7. Priority: Seizures, dysrhythmias (torsades de pointes)
-
Hypomag Interventions
1. Administer Mag PO or IV
2. IVP during code (usually 2grams)
3. Increase dietary intake
4. Concurrently correct other electrolyte imbalances.
-
Hypermag causes
1. > 2.6
2. renal failure
3. increased intake to manage eclampsia during pregnancy
4. Hyperparathyroidism
5. Hypothyroidism
6. Excessive intake of antacids or laxatives (esp w/ renal insufficency)
-
Hypermag S/s
1. Mags do OPPOSITE of prefix, no exceptions
2. Muscles too relaxed and weak
3. Vasodilation = hypotension
4. Flushed, warm skin
5. Lethargy, sedation
6. Decreased respirations
7. Decreased deep tendon reflexes
8. Priority: Paralysis, respiratory / cardiac arrest
-
Hypermag Interventions
1. Avoid / decrease Mg containing foods
2. Administer Calcium gluconate.
3. Respiratory support
4. Good renal function- promote excretion (hydration)
5. Impaired renal function = dialysis.
-
Sodium
1. 135-145 mEq/L
2. Regulation / maintenance of fluid balance
3. Maintains body fluid osmolarity
4. Promotes neuromuscular response: transmission of nerve and muscle impulses
5. Regulates acid-base balance: combines chloride and bicarbonate to alter pH.
-
Hyponatremia causes
1. Excessive loss of Na or excessive GAIN of water
2. Excessive skin loss: sweating
3. GI: diarrhea, vomitting, NG suction
4. Meds: diuretics, meds that cause water retention
5. Trauma: blood loss, draining wounds
6. Hormonal: SIADH (fluid ret)
7. Hypotonic IV solutions (0.45% NaCl)
-
Hyponatremia S/s
1. Neuro: HA, confusion, irritable, restless, seizures, coma
2. GI: diarrhea, abd cramps
3. Hypotension (hypovolemic)
4. Muscle weakness, fatigue
5. Priority: seizures, coma, neuro damage
-
Hyponatremia Interventions
1. Treat underlying cause
2. Sodium replacement- mild: po, ng or iv (lactated ringers or .9% NS), DO NOT increase more than 12 mEq/L in 24 hr to avoid neuro damage due to demyelination. Severe: hypertonic fluids (3% NS) - GIVE SLOW and CLOSE OBSERVAITON, considerations for elderly and cardiac pts.
3. Fluid restriction
4. Nursing: strict i/o's, daily weights, neuro assessments
-
Hypernatremia Cause's
1. Water deprivation or loss
2. Hyperosmolar tube feeds and lack of free water
3. Insensible water loss - burns/wounds or hyperventilation
4. Excessive sodium intake without water
5. Excessive IV intake
6. Diabetes insipidus
7. Medications: steroids, antibiotics, sodium bicarb, cough meds
-
Hypernatremia s/s
1. Thirst
2. N/v, anorexia
3. Rough, dry swollen tongue
4. If dehydrated: tachycardia, orthoBP
5. Increased body temp
6. Dry skin, poor skin turgor
7. Decreased LOC, agitation, lethargy
7. FRIED: flushed skin/fever, restless, increased BP, edema, decreased urine output.
8. Priority: seizure, coma, neuro damage
-
Hypernatremia Interventions
1. Gradually lower Na w/ IV hypotonic solutions (0.45% NS)
2. Diuretics - induce water and Na excretion
3. Monitor I/O, daily weights, urine specific gravity
4. Neuro assessments.
-
Electrolyte High level overview
1. Cardiac = potassium
2. Neuromuscular = Ca and Mg
3. Neuro = Sodium
-
Acid base balance
1. Process of regulating pH, bicarbonate and carbon dioxide concentration of body fluids and gases.
2. pH indicates hydrogen ion H+ concentration.
-
Regulation of Normal Acid Base Balance
1. 1st line: Buffer system - acts fast to adjust hydrogen concentration
2. 2nd Line: Respiratory system - acts fast minutes to hours, adjusts pH by using carbon dioxide upon expiration, slows/increases breathing.
3. 3rd Line: Renal system - acts slow, days to compensate, affect pH by absorbing/generating Hydrogen.
-
ABG Values
Normal Values:
pH: 7.35-7.45
PaO2: 80-95 mmHg on room air
PaCO2 (carbon dioxide): 35-45
HCO3 (bicarb): 22-26 mEq/L
Base Excess: -2 - +2
SaO2 – > 95%
Base excess between observed and normal buffer system, number required to return pH to normal range
Measure ABGs through ART line
-
Compensation
pH returns to normal range
The lungs compensate for metabolic system
Almost immediate
If bicarb increases hypoventilation occurs
If bicarb decreases hyperventilation occurs
The kidneys compensate for the lungs
Kidneys slower – up to 48 hours
If CO2 increases kidneys conserve bicarb
If CO2 decreased kidneys excrete bicarb
-
Respiratory Acidosis Causes
1. Primary factor: HYPOVENTILATION retaining CO2 from under ventilation.
2. Pulmonary diseases
3. Oversedation or drug OD
4. Obesity
-
Respiratory Acidosis Assessment
1. Oversedation, hypoxia, dizzy, drowsy, confused, HA, warm flushed skin
-
Respiratory acidosis Interventions
Treat the cause:
Intubate and ventilate to blow off CO2.
Narcan if over sedated
Suction
Wake them up, get them moving, increase respiratory rate
Sit in semi-Fowler’s, turn-cough-deep breath
Turn up the vent
If Pulmonary Edema and Heart Failure – Lasix
-
Respiratory Alkalosis Causes
1. Primary: HYPERVENTILATION
2. Overbreathing on a mechanical vent or secondary to anxiety/fever.
3. Response to hypoxemia in some pulmonary disorders make patient hyperventilate.
-
Respiratory Alkalosis assessment
1. Tachycardia, fast breathing, dysrhythmias, lethargic, confused, HA, dizzy, n/v, epigastric pain, numbness tingling, hyperreflexias
-
Respiratory Alkalosis Treatment
Treat the cause:
DECREASE the respiratory rate, SLOW down breathing
Adjust ventilator settings (decrease RR)
Breathe into a paper bag, hold breath
Treat the anxiety, provide emotional support
Do not provide rescue breaths too fast during a code
-
Metabolic Acidosis Causes
1. Acid accumulation or bicarbonate loss
2. Lactic acidosis - occurs with shock or tramuma, sepsis
3. DKA
4. Renal failure
5. Aspirin OD (salicylates)
6. Starvation
7. Ineffective metabolism of carbs
-
Metabolic Acidosis Assessment
s/s resp distress, kussmals breathing, hypotension, dysrhythmias, drowsy, confusion, HA, warm flushed skin, n/v/d, Abd pain
-
Metabolic Acidosis Treatment
TREAT THE CAUSE
NaHCO3 IV (sodium bicarb)
Diabetic Ketoacidosis – Insulin and hydration
Renal Failure – dialysis, low protein/high calorie diet
-
Metabolic Alkalosis Cause
1. Retention of base or removal of acid from body fluids.
2. Loss of acid: vomitting, NG suction, gastric damage
3. Eating baking soda/ infusion of excess NaHCO3
4. Hypokalemia, K+ depeleting
5. Diuretics
6. Burns
7. Antacids OD
8. Tx the cause, may need to replace K or give Diamox to help excrete bicarb
-
Metabolic Alkalosis Assessment
Inc wob, resp distress, tachycardia, dysrhythmias, dizzy ,drowsy , confused, HA, n/v loss of appetite, cramping muscles/tremors
-
Metabolic Alkalosis Tx
TREAT THE CAUSE
Increase excretion of HCO3 (Diamox)
Replace K+
Reverse overdose
-
Peripherial IV sizes
1. 24 g - pediatrics, small veins
2. 22 g - pediatrics, small adults, poor veins
3. 20 g - standard adult size, best for blood admin
4. 18 g - large adult size for trauma, rapid fluid resuscitation, blood products, surgery
5. 16 g - very large adult size for trauma, fluid resuscitation.
6. 14 g - rarely used, extremely large catheter.
-
IV insertion Analgesia
1. EMLA cream - topical cream left on skin for 1 to 4 hours prior to procedure. Lidocaine 2.5% and Prilocaine 2.5%, Apply cream, cover with tegaderm, wait 1-4 hours, remove cream, start procedure.
2. SQ lidocaine - 1% lidocaine is injected SQ or intradermally as a wheal. Effect in 60 seconds. Lasts 30 to 45 mins. Start IV at wheal site.
-
Peripheral IV Care
1. Site must be changed every 72 hours. (1 week,)
2. Change tubing every 96 hours, every 24 hours if TPN running.
3. Site assessment: skin intact, no drainage, no redness, flushing/blood return. Q4 checks. Flush at beginning of shift.
4. Label lines.
5. Field sticks change out 24 hrs.
-
Midline Peripheral IV Catheter
1. Looks like a PICC on outside but is NOT a central line.
2. Used as a "longer" peripheral access, put in by RN or PICC nurse.
3. Use for 3-4 weeks.
-
Central Line / Central Venous Catheters
1. Long term use
2. Place sterilely in large central vein
3. Inpatient: dressing changes are sterile
4. Used for medications, fluids, blood draws and blood transfusions.
5. Jugular, subclavian, femoral, superior vena cava veins
6. Tip located in the SVC *confirm placement
-
Who needs a central line?
1. patients receiving certain meds or infusions: chemo, tpn, long term antibiotics(endocarditis, osteomyelitis), vasopressors (dopamine, levophed).
2. Pts with no other access choice
3. Pts receiving multiple infusions simultaneously (ICU)
4. Pts who need central venous pressure monitoring (CVP). monitors fluid volume levels (high = hydrated, hypervolemic) (low = dehydrated, hypovolemic)
-
Most Common Types of Central Lines
1. Triple Lumen Central Line
2. Peripherally Inserted Central Catheter (PICC)
3. Implanted Port
-
Non-tunneled versus Tunneled Cath
1. Non tunneled enters directly into the vein
2. Tunneled, cuffs at exit, skin adheres to cuff securing it.
-
Triple Lumen Central Line
1. ICU pts requiring multiple infusions. Trauma pts,
2. Replaced every 7-10 days. May stay in longer if pt is fragile requiring hemodynamic monitoring. Assessed everyday if can be removed due to infection risk.
3. Central Access, blood, vasopressors, heparin drip, continuous fluids
-
PICC Lines
1. Used w/ pts limited peripheral access. Long term IV med use. Continuous admin of vesicants (chemo pts)
2. 2-6 weeks, up to a year potential.
-
Implanted Ports
1. Efficient access for med administration. requiring long term meds. Parenteral nutrition administration.
2. Ports can stay in for years.
-
Intraosseous Central Line
1. Catheter is placed into the bone with a handheld driver and delivers fluid and medication directly into the bone marrow.
2. Placed in proximal humerus, proximal tibia.
-
Central Line Cath Care
1. Dressing and evidence based practice:
2. Transparent dressings - NOT gauze
3. Change dressings Q week or per institution policy or saturated with drainage
4. Defatting the skin with alcohol prior to application. (dry skin)
5. Antimicrobial chlorhexidine "biopatch" under dressing (replaced every dressing change)
6. Stat locks SHOULD replace sutures.
7. For PICC lines use >10 mL syringe when accessing, flush with 20 mL after blood draws. (pressure concerns)
8. Rule: if the line went in under sterile conditions, change the dressing under sterile conditions.
-
Central Line CLABI recommendations for prevention
1. hand hygiene
2. maximal barrier precautions
3. CHF skin antisepsis
4. Optimal site selection (avoid femoral in adults, yeast infections)
5. Daily review of line necessity
-
Recommendations to Prevent infections in central lines
1. Perform freq asessments
2. Cleanse hubs prior to use 10-15 seconds
3. Sterile insertion and adhere to sterile technique for dressing changes
4. Alcohol based catheter caps and biopatches
5. Use clamps
6. Dressing changes q7 days or prn (wet, soiled, disloged)
7. Sutures
8. Mask pt and RN
9. Bathing
10. Sterile devices to access caths
11. Staff education.
-
Catheter Flushes
1. Frequency per hospital and type of central line
2. NS .9%, 99% of the time
3. Ports: NS and Heparin (afterwards)
4. Flushing techniques
5. CAPS
6. Intermittent pressure flushes - push pause method
-
Central Line Catheter Removal
1. Technique of removal: physician, coagulating testing before removal (ensure clotting intact), position insertion site below the patient heart level or Trendelenburg if tolerated. Have pt bear down to prevent air embolus. Cover site with pressure dressing.
2. RNs can remove/place PICCs with special training.
3. Assessment of cath: Tip intact, length, sending tip for culture
-
Complications for Vascular Access Devices
1. Infection
2. Occlusion (thrombotic or nonthrombotic)
3. Thrombus (non compatible meds)
4. Infiltration, extravasation(med outside vein), phlebitis (irritation)
5. Chest pain / cardiac arrhythmias
6. Device malfunction
7. Air embolism
-
Cellulitis
1. Bacterial skin infection
2. Redness, pain, swollen, sometimes shiny
3. Antibiotics tx
4. Line removal options - early identification can potentially save the line
-
Occlusion / Thrombus
1. Clot can happen within the actual catheter
2. Clot around the catheter in the vein.
3. Potential to surgically removal fibrin sheath.
-
Declotting Central Lines
1. Most common drug is Alteplase (tpa), aka Cathflo or activase, powerful antithrombolitic, dosed in 500 mcg/mL (1mL)
2. 70-80% metabolized by oxidation during single pass through lungs
3. Half life of 5-10 minutes
4. Use for indwelling or infusions.
-
Incompatible Medications
1. Top 5 offenders: Bicarb, Lasix, Haldol, Calcium, Dilantin
2. Use micromedex to know combability.
-
Infiltration Complication
1. IV catheter has slipped out of the vein and is infusing into the tissue.
2. Skin is cool, puffy, blanches, usually painful, swollen
3. Tx: remove catheter, assess for circulation, elevate arm, warm compress. Review any special considerations for the fluid/drug that has infiltrated.
-
Extravasation Complication
1. Tissue irritation, ischemia, necrosis
2. Tx: aspirate med, instill antidote
3. Assess and measure daily, photographs
4. Involve dermatology and plastic surgeon
5. Treatments medication dependent.
-
Phlebitis
1. Redness at cath tip and along vein from poor blood flow around the device or caustic solution infused.
2. Nursing interventions: remove the device, apply a warm pack, notify MD.
3. Restart the IV in a bigger vein or use a smaller cath to allow blood flow around IV cath.
-
Litigation w/ IV therapy
1. Most lawsuits filed against nurses with regards to iv therapy had to do with cases of infiltration or phlebitis.
2. Good documentation is key, date time site, type of iv, routine checks, infusion types, blood return.
3. Check at beginning of each shift, check prior to each medication.
-
Central Line Blood Draw
1. turn head, cough, position changes for trouble shooting lab draw, flushing.
2. Considerations: flush amount, waste amount.
3. Cathflow potentially if still wont work, check placement if still doesn't work.
4. Waste amount may need to be more if certain meds stick to inside of line.
-
Correct order for blood draw
1. RBGL
1. red - blood bank
2. blue - coagulation
3. green - electrolytes
4. Lavendar - hematology
5. Gray - glucose
-
D/c IV steps
1. D/c tubing, put sterile cap on it and hang on IV pole
2. Flush IV with 10 mL sterile saline
3. If there is a clamp on the IV pigtail, clamp it
4. Secure tubing on patient
5. Reconnect: scrub the hub, flush IV, reconnect.
-
Patient Controlled Analgesia (PCA)
1. Basal rate - set continuous rate
2. Bolus dose / demand dose - best pain control is the type that the patient has control over.
3. Considerations- oversedation, appropriate use, frequent assessment of pain and use.
-
Epidural Catheters
1. For child birth, post op surgical procedures
2. pros: pain control, non-sedation, steady direct state of pain control
3. Cons: Spinal headaches if miss, doesn't affect full area, HA, hypotension
-
Critical Care Specialty Lines
1. One of the things that separates cc nursing from m/s nursing is the ability to hemodynamically monitor pts.
2. Arterial Lines
3. Central Venous Pressure (CVP) monitoring
4. Pulmonary Artery (PA) lines
-
Hemodynamic Monitoring Basics
1. Hemodynamic monitoring allows the clinician to assess pressures, fluid status and cardiac function in critically ill pts.
2. RN can monitor a pts hemodynamic status continually. Invasive lines and transducer turns pressures into wave forms.
-
Arterial Lines
1. MAP - mean arterial pressure
2. Arterial blood gases ABGs
3. Systemic blood pressure
4. Continuous waveform
5. used in icu, shock sepsis trauma
6. common insertion sites: radial and brachial
-
Zeroing the Arterial Line
1. You must zero all pressurized lines when initiating therapy, when the cable comes disconnected and per hospital policy (usually once per shift)
2. The transducer must be placed at a level equivalent to the right atrium for all hemodynamic measurements. This point is called the PHLEBOSTATIC AXIS and is located at the mid-chest line, fourth intercostal space. MCL-4
-
Maintaining Arterial Lines
1. The standard of practice is to change art line dressing, tubing, and pressure bag every 72-96 hours, depending on policy.
2. Dressing change is sterile.
3. RN assesses distal pulse and color, waveform, and correlation with manual BP cuff every shift.
-
Cardiac Output
1. CO = HR x SV, quantity of blood pumped by each ventricle per minute
2. Normal values: CO = 4-6 L/min
Cardiac index (CI) = 2.2-4.0 L/min/m2 (CO indexed to BSA), based on patient size, lets us know if pt is pumping enough blood
3. HR = 60-100 beats per minute
4. Stroke volume (SV) amount of blood pumped by each ventricle in one cardiac cycle or each heart beat. SV = 50-110 mL ejected with each heart beat.
-
Stroke Volume
1. Stroke volume (SV) is amount of blood ejected with each heart beat
2. SV = CO / HR
3. ex if co = 4.0 l/min and hr = 100, SV = 4/100 = 40mL/min

