Homeostasis
1. Any self-regulating process by a biological system to maintain stability.
2. Adjusting conditions that are optimal for survival.
5. 5 Functions: Temp, BGL, BP, Toxins, pH
Homeostasis Considerations
1. Balance of fluids and electrolytes, body is making constant adjustments to maintain balance.
2. Recognize changes early. May be obvious or subtle.
3. Timely assessments important.
Fluid
1. Adults approx 60% of weight is fluid
2. 2/3 = intracellular
3. 1/3 = extracellular
4. Plasma is intravascular, including lymph
5. Transcellular is any fluid in epithelial-lined spaces such as pericardial, CSF, synovial, pleural, intraocular.
Fluid Functions
1. Regulate temperature
2. Moisten tissues in eyes, nose, mouth
3. Protects body organs and tissues.
4. Carries nutrients and oxygen to cells.
5. Lubricates joints
6. Lessens burden on kidneys and liver by flushing out waste.
7. Dissolves minerals an nutrients for accessible to your body.
Fluid Balance
1. Intake: 2500mL per 24 hours
2. Output: Sensible loss: 500-1000mL per 24hr, Insensible loss: 1500mL per 24 hr
3. Sensible can be measured and tracked.
4. Insensible is unable to track/measure.
Fluid Gain and Loss: Healthly Adult
1. Kidneys: average output 1mL/kg/hr
2. Skin: sweat can be affected by fever, exercise, burns more fluid loss
3. Lungs: give off fluid in vapor, RR, dry/wet environment, exercise
4. GI tract: lose about 200 mL daily in GI tract, diarrhea or surgery
Fluid Transport Mechanisms
Diffusion – particles move from area of high concentration to low concentration
Osmosis – water particles move from area of high solute concentration to low concentrations
Filtration – response to pressure, hydrostatic pressure exerted on walls of vessels pushes fluid inside cells
Osmotic pressure – pressure exerted by solutes, minimum pressure which needs to be applied to a solution to prevent the inward flow of its pure solvent across a semipermeable membrane, pulls fluid out of intracellular into extracellular
Fluid Spacing
1. First - normal fluid distribution
2. Second - Excessive accumulation of fluid in interstitial spaces. (Edema, fluid collecting in-between cells)
3. Third - Fluid shifts from intravascular to a "third" transcellular space (serous cavity), ascites, pleural infusions, *can be dehydrated with fluid spacing
Water Balance Regulation
Hypothalamic Regulation: changes in blood osmolality and triggers thirst or antidiuretic hormone (ADH) release in response to imbalances.
Pituitary Regulation: pituitary gland, specifically the posterior pituitary, in releasing antidiuretic hormone (ADH) to conserve water by reducing urine output when the body's water levels are low.
Adrenal-Cortical Regulation: relates to the influence of the adrenal cortex, which secretes aldosterone to increase sodium reabsorption and water retention in the kidneys, thus helping maintain water balance.
Water Balance Regulation 2
Renal System: regulating water balance by filtering blood, reabsorbing essential water and solutes, and excreting excess water as urine, under the control of hormones like ADH and aldosterone.
Cardiovascular System: water balance regulation by ensuring adequate blood circulation to maintain blood pressure and transport hormones like ADH and aldosterone, which affect water reabsorption in the kidneys.
GI System: water balance regulation by absorbing water from ingested fluids and eliminating excess water through feces, contributing to overall fluid balance in the body.
BNP (B-type natriuretic peptide)
a hormone produced by the heart in response to stretching of the heart muscle cells, especially in the ventricles. It plays a crucial role in regulating fluid balance and blood pressure. When there is an increase in blood volume or pressure in the heart, the heart releases BNP to promote natriuresis, which is the excretion of sodium and water by the kidneys. This helps to reduce blood volume and lower blood pressure.
Hypovolemia versus Hypervolemia
1. Hypovolemia: fluid volume deficit, loss of ecf exceeds intake, increased osmolality, concentrated labs, dehydration
2. HYPERvolemia: fluid volume excess, abnormal retention of water and sodium led to expansion of ecf, decrease osmolality, dilute labs.
Hypovolemia verus Hypervolemia Findings
1. Hypervolemia – high intake low output, HTN, tachyC, wob inc, fluid in pleural space (crackles), High Na diet, edema/moist skin, HCT lower (diluted)
2. Hypovolemia – low intake, low output, hypoBP, tachyC, inc RR, confusion, Not enough fluid intake, dry poor skin turgor, thirst, thready pulse, HCT elevated
3. To start to have peripheral edema = 5 Liters gains. Puffy edema = 10 Liters gain
Electrolyte Composition
1. Electrolytes dissociate or split into ions when placed into water.
2. Ions - electrically charged.
3. Cations - positively charged (Na, K, Ca, Mg)
4. Anions - negatively charged (HCO3, Cl, PO4)
5. ECF - main cation is Na and main anion is Cl-.
6. ICF - main cation is K+ and main anion is PO4-.
Electrolyte Maintenance
1. Determine those at risk / manage underlying cause.
2. Assessment: VS, HR, rhythm, LOC, i/o, muscle strength and movement, weight
3. Lab (serum and urine): electrolytes, osmolality, bun/creatine, BNP (elevation indicates need to removal excess fluid)
Healthy Electrolyte Balance versus Abnormal
1. Healthy: VS wnl, AxO4, equal i/o, strength/movement wnl, stable weight
2. Abnormal: tachycardia, dysthymias, irregular rhythm, confusion/disorientation, weak, muscle twitching, seizure and unresponsiveness. Inadequate or excessive output. Weight gain or loss.
3. Confusion and weight gain first clues of abnormal electrolyte imbalance.
Potassium
1. K = 3.5-5 mEq/L
2. Regulates ICF
3. Promotes nerve impulse transmission
4. Skeletal, smooth, and cardiac muscle contractions
5. Acid/base balance: hydrogen ions exchange with potassium ions in ICF.
6. Allows glycogen to be deposited in muscle and liver cells.
7. Excess K eliminated, 80% kidneys daily, 20% bowel movements and sweat.
8. Daily replacement K for those on wasting diuretics.
Hypokalemia causes
1. K < 3.5 mEq/L
2. Decreased intake
3. Increased renal excretion / kidney disease
4. Movement of K from ECF to ICF (glucose metabolism)
5. GI disturbances (diarrhea/vomit)
6. Meds - (insulin, diuretics, laxatives, digoxin)
7. Low Mg levels (when mg or k gets low, lower together)
Hypokalemia s/s
1. Kalemias do the same as prefix, except HR and urine output.
2. Usually appears at < 3.0 mEq/L
3. Cardiac arrhythmias and EKG changes.
4. Decreased DTR.
5. Polyuria and nocturia
6. Priority: Lethal cardiac dysrhythmias, cardiac arrest, coma
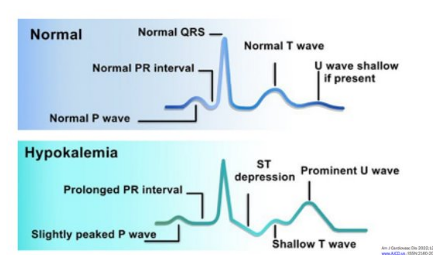
Hypokalemia EKG presentation
Hypokalemia Interventions
1. Oral / diet replacement (fruits, bananas, spinach, salt substitutes are high in K)
2. Salt sub w/ K
3. Parenteral replacement: can only give 10mEq/hr , peripheral IV potassium must be diluted usually 1liter of fluid, concerns with burning swelling irritation.
Hyperkalemia causes
1. K > 5.0 mEq/L
2. increased intake
3. impaired excretion (renal failure, dehydration)
4. Movement from ICF to ECF (cell lysis, cancer/burns)
5. Acidosis
6. Potassium sparing diuretics
7. Adrenal insufficiency (low aldosterone, which promotes the excretion of dietary potassium)
Hyperkalemia S/s
1. Kalemias do the same as the prefix except for HR and urine output.
2. EKG changes, irregular pulse, arrhythmias
3. Anxiety, irritability
4. Muscle weakness, flaccid paralysis, paresthesia
5. GI: abnormal cramping, diarrhea
6. Metabolic acidosis
7. Priority: V fib, respiratory arrest, cardiac arrest
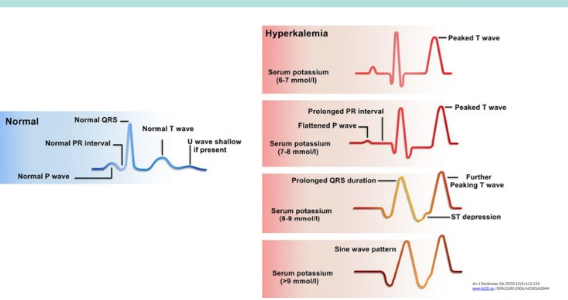
Hyperkalemia EKG
Hyperkalemia Interventions
1. Prevent by identifying those at risk / identify underlying cause
2. Decrease oral / parenternal intake
3. Meds: diuretics, kayexalate (potassium binding, works in Large intestine)
4. IV insulin with glucose forces K into cells.
5. Calcium gluconate IV to decrease cardiac excitability
6. Dialysis
Calcium
1. 8.2 - 10.2 mg/dL
2. 99% located in skeletal system
3. Daily intake needed
4. Maintains bones and teeth
5. Essential component of nerve/muscle/cardiac contractions
6. Blood clotting: converts prothrombin to thrombin
Hypocalcemia causes
1. < 8.2 mg/dL (Vit D and Ca coincide)
2. Renal failure
3. Decreased intake, malabsorption, Vit D deficit
4. Loss of Ca: alcoholism, excessive diarrhea, aggressive diuretic therapy
5. Endocrine disorders and parathyroidectomy
6. Low Mg (reduces amount of PTH released)
7. Hyperphosphatemia (inverse relationship with Ca)
8. Meds - aminoglycosides, anticonvulsants, loop diuretics, bisphosphonates (tx osteop)
Hypocalcemia S/s
1. Calcemias do the OPPOSITE as the prefix, no exceptions.
2. Below 7 is critical, tetany and stridor, 6 can cause death.
3. Convulsions: involuntary jerking/contractions/spasms- cramps and tetany.
4. VS, arrhythmias, hypotension, ECG
5. Seizures
6. Trousseau's sign - bp cuff, Chvostek's sign-face
7. Increased peristalsis and diarrhea
8. Numbness and tingling of lips and extremities
9. Osteoporosis
10. Priority: seizures, laryngospasm w/ stridor, ventricular tachycardia
Hypocalcemia Interventions
1. Correct level and treat cause, recheck q4-q6.
2. Administer IV calcium gluconate.
3. Increase dietary intake of Ca and Vit D.
4. Monitor EKG
5. Validate albumin level - if low may not need calcium. (when albumin is low, skews Ca results, ionized Ca level for more accurate results)
Hypercalcemia Causes
1. Increased intake
2. Metastatic disease processes affecting bones
3. Endocrine disorders: hyperparathyroidism, adrenal insufficiency
4. Kidney disease, decreased excretion
5. Meds: Antacids, Thiazide diuretics, glucocorticoids
Hypercalcemia S/s
1. Calcemias do the OPPOSITE as the prefix, no exceptions
2. Weakness - can be profound
3. Lethargy, confusion, personality changes
4. Decreased reflexes
5. Constipation
6. N/v
7. Bone pain, fracture
8. Polyuria, polydipsia, calcium stones
9. ECG changes - arrhythmias, bradycardia, shortened QT/ST intervals
10. Priority: coma, death
Magnesium
1. 1.6-2.6 mEq/L
2. 1/3 bound to proteins
3. Essential for metabolism of carbs and proteins
4. Regulates neuromuscular function and electrolyte balance
5. Cardiovascular: acts peripherally to produce vasodilation and decrease peripheral resistance
6. Balances phosphorus and calcium levels.
Hypomagnesemia causes
1. < 1.6
2. Symptoms usually start at <1.3
3. Alcoholism
4. Prolonged GI issues: diarrhea, starvation, vomiting's, malabsorption
5. NG tube with prolonged suction
6. Acute pancreatitis
7. Concurrent hypokalemia not responding to replacement
8. Limited intake or increased renal loss
9. Prolonged use of PPIs lead to decreased absorption of Magnesium
Hypomag s/s
1. Mag OPPOSITE of prefix without exceptions
2. Neuromuscular irritability (trousseau and chvostek)
3. Tachycardia, HTN
4. hyperactive tendon reflexes
5. Muscle cramps
6. Psychological changes
7. Priority: Seizures, dysrhythmias (torsades de pointes)
Hypomag Interventions
1. Administer Mag PO or IV
2. IVP during code (usually 2grams)
3. Increase dietary intake
4. Concurrently correct other electrolyte imbalances.
Hypermag causes
1. > 2.6
2. renal failure
3. increased intake to manage eclampsia during pregnancy
4. Hyperparathyroidism
5. Hypothyroidism
6. Excessive intake of antacids or laxatives (esp w/ renal insufficency)
Hypermag S/s
1. Mags do OPPOSITE of prefix, no exceptions
2. Muscles too relaxed and weak
3. Vasodilation = hypotension
4. Flushed, warm skin
5. Lethargy, sedation
6. Decreased respirations
7. Decreased deep tendon reflexes
8. Priority: Paralysis, respiratory / cardiac arrest
Hypermag Interventions
1. Avoid / decrease Mg containing foods
2. Administer Calcium gluconate.
3. Respiratory support
4. Good renal function- promote excretion (hydration)
5. Impaired renal function = dialysis.
Sodium
1. 135-145 mEq/L
2. Regulation / maintenance of fluid balance
3. Maintains body fluid osmolarity
4. Promotes neuromuscular response: transmission of nerve and muscle impulses
5. Regulates acid-base balance: combines chloride and bicarbonate to alter pH.
Hyponatremia causes
1. Excessive loss of Na or excessive GAIN of water
2. Excessive skin loss: sweating
3. GI: diarrhea, vomitting, NG suction
4. Meds: diuretics, meds that cause water retention
5. Trauma: blood loss, draining wounds
6. Hormonal: SIADH (fluid ret)
7. Hypotonic IV solutions (0.45% NaCl)
Hyponatremia S/s
1. Neuro: HA, confusion, irritable, restless, seizures, coma
2. GI: diarrhea, abd cramps
3. Hypotension (hypovolemic)
4. Muscle weakness, fatigue
5. Priority: seizures, coma, neuro damage
Hyponatremia Interventions
1. Treat underlying cause
2. Sodium replacement- mild: po, ng or iv (lactated ringers or .9% NS), DO NOT increase more than 12 mEq/L in 24 hr to avoid neuro damage due to demyelination. Severe: hypertonic fluids (3% NS) - GIVE SLOW and CLOSE OBSERVAITON, considerations for elderly and cardiac pts.
3. Fluid restriction
4. Nursing: strict i/o's, daily weights, neuro assessments
Hypernatremia Cause's
1. Water deprivation or loss
2. Hyperosmolar tube feeds and lack of free water
3. Insensible water loss - burns/wounds or hyperventilation
4. Excessive sodium intake without water
5. Excessive IV intake
6. Diabetes insipidus
7. Medications: steroids, antibiotics, sodium bicarb, cough meds
Hypernatremia s/s
1. Thirst
2. N/v, anorexia
3. Rough, dry swollen tongue
4. If dehydrated: tachycardia, orthoBP
5. Increased body temp
6. Dry skin, poor skin turgor
7. Decreased LOC, agitation, lethargy
7. FRIED: flushed skin/fever, restless, increased BP, edema, decreased urine output.
8. Priority: seizure, coma, neuro damage
Hypernatremia Interventions
1. Gradually lower Na w/ IV hypotonic solutions (0.45% NS)
2. Diuretics - induce water and Na excretion
3. Monitor I/O, daily weights, urine specific gravity
4. Neuro assessments.
Electrolyte High level overview
1. Cardiac = potassium
2. Neuromuscular = Ca and Mg
3. Neuro = Sodium
Acid base balance
1. Process of regulating pH, bicarbonate and carbon dioxide concentration of body fluids and gases.
2. pH indicates hydrogen ion H+ concentration.
Regulation of Normal Acid Base Balance
1. 1st line: Buffer system - acts fast to adjust hydrogen concentration
2. 2nd Line: Respiratory system - acts fast minutes to hours, adjusts pH by using carbon dioxide upon expiration, slows/increases breathing.
3. 3rd Line: Renal system - acts slow, days to compensate, affect pH by absorbing/generating Hydrogen.
ABG Values
Normal Values:
pH: 7.35-7.45
PaO2: 80-95 mmHg on room air
PaCO2 (carbon dioxide): 35-45
HCO3 (bicarb): 22-26 mEq/L
Base Excess: -2 - +2
SaO2 – > 95%
Base excess between observed and normal buffer system, number required to return pH to normal range
Measure ABGs through ART line
Compensation
pH returns to normal range
The lungs compensate for metabolic system
Almost immediate
If bicarb increases hypoventilation occurs
If bicarb decreases hyperventilation occurs
The kidneys compensate for the lungs
Kidneys slower – up to 48 hours
If CO2 increases kidneys conserve bicarb
If CO2 decreased kidneys excrete bicarb
Respiratory Acidosis Causes
1. Primary factor: HYPOVENTILATION retaining CO2 from under ventilation.
2. Pulmonary diseases
3. Oversedation or drug OD
4. Obesity
Respiratory Acidosis Assessment
1. Oversedation, hypoxia, dizzy, drowsy, confused, HA, warm flushed skin
Respiratory acidosis Interventions
Treat the cause:
Intubate and ventilate to blow off CO2.
Narcan if over sedated
Suction
Wake them up, get them moving, increase respiratory rate
Sit in semi-Fowler’s, turn-cough-deep breath
Turn up the vent
If Pulmonary Edema and Heart Failure – Lasix
Respiratory Alkalosis Causes
1. Primary: HYPERVENTILATION
2. Overbreathing on a mechanical vent or secondary to anxiety/fever.
3. Response to hypoxemia in some pulmonary disorders make patient hyperventilate.
Respiratory Alkalosis assessment
1. Tachycardia, fast breathing, dysrhythmias, lethargic, confused, HA, dizzy, n/v, epigastric pain, numbness tingling, hyperreflexias
Respiratory Alkalosis Treatment
Treat the cause:
DECREASE the respiratory rate, SLOW down breathing
Adjust ventilator settings (decrease RR)
Breathe into a paper bag, hold breath
Treat the anxiety, provide emotional support
Do not provide rescue breaths too fast during a code
Metabolic Acidosis Causes
1. Acid accumulation or bicarbonate loss
2. Lactic acidosis - occurs with shock or tramuma, sepsis
3. DKA
4. Renal failure
5. Aspirin OD (salicylates)
6. Starvation
7. Ineffective metabolism of carbs
Metabolic Acidosis Assessment
s/s resp distress, kussmals breathing, hypotension, dysrhythmias, drowsy, confusion, HA, warm flushed skin, n/v/d, Abd pain
Metabolic Acidosis Treatment
TREAT THE CAUSE
NaHCO3 IV (sodium bicarb)
Diabetic Ketoacidosis – Insulin and hydration
Renal Failure – dialysis, low protein/high calorie diet
Metabolic Alkalosis Cause
1. Retention of base or removal of acid from body fluids.
2. Loss of acid: vomitting, NG suction, gastric damage
3. Eating baking soda/ infusion of excess NaHCO3
4. Hypokalemia, K+ depeleting
5. Diuretics
6. Burns
7. Antacids OD
8. Tx the cause, may need to replace K or give Diamox to help excrete bicarb
Metabolic Alkalosis Assessment
Inc wob, resp distress, tachycardia, dysrhythmias, dizzy ,drowsy , confused, HA, n/v loss of appetite, cramping muscles/tremors
Metabolic Alkalosis Tx
TREAT THE CAUSE
Increase excretion of HCO3 (Diamox)
Replace K+
Reverse overdose
Peripherial IV sizes
1. 24 g - pediatrics, small veins
2. 22 g - pediatrics, small adults, poor veins
3. 20 g - standard adult size, best for blood admin
4. 18 g - large adult size for trauma, rapid fluid resuscitation, blood products, surgery
5. 16 g - very large adult size for trauma, fluid resuscitation.
6. 14 g - rarely used, extremely large catheter.
IV insertion Analgesia
1. EMLA cream - topical cream left on skin for 1 to 4 hours prior to procedure. Lidocaine 2.5% and Prilocaine 2.5%, Apply cream, cover with tegaderm, wait 1-4 hours, remove cream, start procedure.
2. SQ lidocaine - 1% lidocaine is injected SQ or intradermally as a wheal. Effect in 60 seconds. Lasts 30 to 45 mins. Start IV at wheal site.
Peripheral IV Care
1. Site must be changed every 72 hours. (1 week,)
2. Change tubing every 96 hours, every 24 hours if TPN running.
3. Site assessment: skin intact, no drainage, no redness, flushing/blood return. Q4 checks. Flush at beginning of shift.
4. Label lines.
5. Field sticks change out 24 hrs.
Midline Peripheral IV Catheter
1. Looks like a PICC on outside but is NOT a central line.
2. Used as a "longer" peripheral access, put in by RN or PICC nurse.
3. Use for 3-4 weeks.
Central Line / Central Venous Catheters
1. Long term use
2. Place sterilely in large central vein
3. Inpatient: dressing changes are sterile
4. Used for medications, fluids, blood draws and blood transfusions.
5. Jugular, subclavian, femoral, superior vena cava veins
6. Tip located in the SVC *confirm placement
Who needs a central line?
1. patients receiving certain meds or infusions: chemo, tpn, long term antibiotics(endocarditis, osteomyelitis), vasopressors (dopamine, levophed).
2. Pts with no other access choice
3. Pts receiving multiple infusions simultaneously (ICU)
4. Pts who need central venous pressure monitoring (CVP). monitors fluid volume levels (high = hydrated, hypervolemic) (low = dehydrated, hypovolemic)
Most Common Types of Central Lines
1. Triple Lumen Central Line
2. Peripherally Inserted Central Catheter (PICC)
3. Implanted Port
Non-tunneled versus Tunneled Cath
1. Non tunneled enters directly into the vein
2. Tunneled, cuffs at exit, skin adheres to cuff securing it.
Triple Lumen Central Line
1. ICU pts requiring multiple infusions. Trauma pts,
2. Replaced every 7-10 days. May stay in longer if pt is fragile requiring hemodynamic monitoring. Assessed everyday if can be removed due to infection risk.
3. Central Access, blood, vasopressors, heparin drip, continuous fluids
PICC Lines
1. Used w/ pts limited peripheral access. Long term IV med use. Continuous admin of vesicants (chemo pts)
2. 2-6 weeks, up to a year potential.
Implanted Ports
1. Efficient access for med administration. requiring long term meds. Parenteral nutrition administration.
2. Ports can stay in for years.
Intraosseous Central Line
1. Catheter is placed into the bone with a handheld driver and delivers fluid and medication directly into the bone marrow.
2. Placed in proximal humerus, proximal tibia.
Central Line Cath Care
1. Dressing and evidence based practice:
2. Transparent dressings - NOT gauze
3. Change dressings Q week or per institution policy or saturated with drainage
4. Defatting the skin with alcohol prior to application. (dry skin)
5. Antimicrobial chlorhexidine "biopatch" under dressing (replaced every dressing change)
6. Stat locks SHOULD replace sutures.
7. For PICC lines use >10 mL syringe when accessing, flush with 20 mL after blood draws. (pressure concerns)
8. Rule: if the line went in under sterile conditions, change the dressing under sterile conditions.
Central Line CLABI recommendations for prevention
1. hand hygiene
2. maximal barrier precautions
3. CHF skin antisepsis
4. Optimal site selection (avoid femoral in adults, yeast infections)
5. Daily review of line necessity
Recommendations to Prevent infections in central lines
1. Perform freq asessments
2. Cleanse hubs prior to use 10-15 seconds
3. Sterile insertion and adhere to sterile technique for dressing changes
4. Alcohol based catheter caps and biopatches
5. Use clamps
6. Dressing changes q7 days or prn (wet, soiled, disloged)
7. Sutures
8. Mask pt and RN
9. Bathing
10. Sterile devices to access caths
11. Staff education.
Catheter Flushes
1. Frequency per hospital and type of central line
2. NS .9%, 99% of the time
3. Ports: NS and Heparin (afterwards)
4. Flushing techniques
5. CAPS
6. Intermittent pressure flushes - push pause method
Central Line Catheter Removal
1. Technique of removal: physician, coagulating testing before removal (ensure clotting intact), position insertion site below the patient heart level or Trendelenburg if tolerated. Have pt bear down to prevent air embolus. Cover site with pressure dressing.
2. RNs can remove/place PICCs with special training.
3. Assessment of cath: Tip intact, length, sending tip for culture
Complications for Vascular Access Devices
1. Infection
2. Occlusion (thrombotic or nonthrombotic)
3. Thrombus (non compatible meds)
4. Infiltration, extravasation(med outside vein), phlebitis (irritation)
5. Chest pain / cardiac arrhythmias
6. Device malfunction
7. Air embolism
Cellulitis
1. Bacterial skin infection
2. Redness, pain, swollen, sometimes shiny
3. Antibiotics tx
4. Line removal options - early identification can potentially save the line
Occlusion / Thrombus
1. Clot can happen within the actual catheter
2. Clot around the catheter in the vein.
3. Potential to surgically removal fibrin sheath.
Declotting Central Lines
1. Most common drug is Alteplase (tpa), aka Cathflo or activase, powerful antithrombolitic, dosed in 500 mcg/mL (1mL)
2. 70-80% metabolized by oxidation during single pass through lungs
3. Half life of 5-10 minutes
4. Use for indwelling or infusions.
Incompatible Medications
1. Top 5 offenders: Bicarb, Lasix, Haldol, Calcium, Dilantin
2. Use micromedex to know combability.
Infiltration Complication
1. IV catheter has slipped out of the vein and is infusing into the tissue.
2. Skin is cool, puffy, blanches, usually painful, swollen
3. Tx: remove catheter, assess for circulation, elevate arm, warm compress. Review any special considerations for the fluid/drug that has infiltrated.
Extravasation Complication
1. Tissue irritation, ischemia, necrosis
2. Tx: aspirate med, instill antidote
3. Assess and measure daily, photographs
4. Involve dermatology and plastic surgeon
5. Treatments medication dependent.
Phlebitis
1. Redness at cath tip and along vein from poor blood flow around the device or caustic solution infused.
2. Nursing interventions: remove the device, apply a warm pack, notify MD.
3. Restart the IV in a bigger vein or use a smaller cath to allow blood flow around IV cath.
Litigation w/ IV therapy
1. Most lawsuits filed against nurses with regards to iv therapy had to do with cases of infiltration or phlebitis.
2. Good documentation is key, date time site, type of iv, routine checks, infusion types, blood return.
3. Check at beginning of each shift, check prior to each medication.
Central Line Blood Draw
1. turn head, cough, position changes for trouble shooting lab draw, flushing.
2. Considerations: flush amount, waste amount.
3. Cathflow potentially if still wont work, check placement if still doesn't work.
4. Waste amount may need to be more if certain meds stick to inside of line.
Correct order for blood draw
1. RBGL
1. red - blood bank
2. blue - coagulation
3. green - electrolytes
4. Lavendar - hematology
5. Gray - glucose
D/c IV steps
1. D/c tubing, put sterile cap on it and hang on IV pole
2. Flush IV with 10 mL sterile saline
3. If there is a clamp on the IV pigtail, clamp it
4. Secure tubing on patient
5. Reconnect: scrub the hub, flush IV, reconnect.
Patient Controlled Analgesia (PCA)
1. Basal rate - set continuous rate
2. Bolus dose / demand dose - best pain control is the type that the patient has control over.
3. Considerations- oversedation, appropriate use, frequent assessment of pain and use.
Epidural Catheters
1. For child birth, post op surgical procedures
2. pros: pain control, non-sedation, steady direct state of pain control
3. Cons: Spinal headaches if miss, doesn't affect full area, HA, hypotension
Critical Care Specialty Lines
1. One of the things that separates cc nursing from m/s nursing is the ability to hemodynamically monitor pts.
2. Arterial Lines
3. Central Venous Pressure (CVP) monitoring
4. Pulmonary Artery (PA) lines
Hemodynamic Monitoring Basics
1. Hemodynamic monitoring allows the clinician to assess pressures, fluid status and cardiac function in critically ill pts.
2. RN can monitor a pts hemodynamic status continually. Invasive lines and transducer turns pressures into wave forms.
Arterial Lines
1. MAP - mean arterial pressure
2. Arterial blood gases ABGs
3. Systemic blood pressure
4. Continuous waveform
5. used in icu, shock sepsis trauma
6. common insertion sites: radial and brachial
Zeroing the Arterial Line
1. You must zero all pressurized lines when initiating therapy, when the cable comes disconnected and per hospital policy (usually once per shift)
2. The transducer must be placed at a level equivalent to the right atrium for all hemodynamic measurements. This point is called the PHLEBOSTATIC AXIS and is located at the mid-chest line, fourth intercostal space. MCL-4
Maintaining Arterial Lines
1. The standard of practice is to change art line dressing, tubing, and pressure bag every 72-96 hours, depending on policy.
2. Dressing change is sterile.
3. RN assesses distal pulse and color, waveform, and correlation with manual BP cuff every shift.
Cardiac Output
1. CO = HR x SV, quantity of blood pumped by each ventricle per minute
2. Normal values: CO = 4-6 L/min
Cardiac index (CI) = 2.2-4.0 L/min/m2 (CO indexed to BSA), based on patient size, lets us know if pt is pumping enough blood
3. HR = 60-100 beats per minute
4. Stroke volume (SV) amount of blood pumped by each ventricle in one cardiac cycle or each heart beat. SV = 50-110 mL ejected with each heart beat.
Stroke Volume
1. Stroke volume (SV) is amount of blood ejected with each heart beat
2. SV = CO / HR
3. ex if co = 4.0 l/min and hr = 100, SV = 4/100 = 40mL/min
Ejection Fraction Defined
1. EF is the ratio of stroke volume to end-diastolic volume
2. The amount of blood squeezed out of the LV compared to the amount of blood left in the LV
3. Measured as a percentage
4. If LV end diastolic volume is 100 mL and SV is 60 mL that means ejection fraction is 60%.
5. Need min of 10% to live, 20% suffering
Determinants of SV
1. Preload: what is the pts volume status and filling pressures? (hyper vs hypovolemic)
2. Afterload: What kind of force does the heart have to work against to get blood out (vasodilation = afterload dec, sv inc vs vasoconstriction = afterload inc, sv dec)
3. Contractility: is heart able to squeeze effectively?
Preload
1. Preload is the maximal stretch of the cardiac muscle prior to contraction
2. A filling pressure, it represents the amount of fluid that is presented to the heart.
3. Preload is measured during diastole, when the MV and TV valves are open so it is assumed that the pressure in the ventricles is equal to the pressure in the atria.
Preload = Central Venous Pressure (CVP)
1. CVP is a measurement of fluid status, equal to the amount of blood found in the right heart at the end of diastole. It tells you one simple thing:
2. If pt is wet or dry
3. Normal healthy person CVP ranges from 2-6
4. Less than 2 = patient is dry/dehydrated
5. Greater than 6 = patient is wet/fluid overloaded
6. Numbers you need to know: 2 = dry, and 20 = fluid volume overload
CVP Monitoring
1. CVP can be monitored through any thoracic central line (usually SC or IJ)
2. CVP can be monitored through a single transducer system or in conjunction with the PA monitoring
How to use CVP to determine tx
1. CHF pt has fluids running at 125 mL/hr all night. When you check the CVP, you get 18.
2. What does the number mean? fluid overload
3. What treatment? Stop fluids, diuretics.
Pulmonary Artery Pressure Monitoring
1. Hemodynamic values obtained are used to evaluate preload, afterload, and contractility (ventricular function)
2. Indications: shock states, evaluating vasoactive drip effects, assessing cardiac function.
Types of Infusions
1. Crystalloid- isotonic or clear fluids, hypotonic/hypertonic, used for fluid replacement and maintenance. (hydrate, esp isotonic fluids)
2. Colloid - blood products, TPN, albumin (stay in blood vessels, expand volume)
Isotonic fluids
1. Isoperfect - no fluid shifts with isotonic fluids. Balanced to look like blood as much as possible
2. Builds blood volume, hydrating.
3. Ex: NS 0.9%, LR (used more with burns, trauma, acute blood loss)
4. Same osmolality and water concentration as blood in body.
Hypotonic versus Hypertonic Fluids
1. Hypotonic - draw fluid into the cells. usually low sodium concentration (0.45% NS, 2.5% Dextrose)
2. Hypertonic - fluid escapes cells (shrink by osmosis), contain higher concentration of solutes than fluid in cells (ICF), high osmolality (NS 3%)
3. Infuse slowly
High Risk Infusions
1. Vesicants, irritants
2. Highly irritating infusions will cause injury to the vein endothelium.
3. Can cause chemical phlebitis, actual tissue damage, thrombosis and necrosis.
4. Should be given through a central line if possible
5. ex: chemo, dopamine, amphotercin
PPN peripheral parenteral nutrition
1. Dextrose 5-10%, amino acids, electrolytes, minerals, vitamins, fat emulsions, short term, <3 weeks of therapy.
2. Provides 1300 to 1800 cals a day
3. Can be given through peripheral IV - has most complications and is LEAST DESIRABLE form of nutrition.
TPN
1. total parenteral nutrition
2. dextrose 20-70%, amino acids, electrolytes, minerals, vitamins, fat emulsions, Long term > 3 weeks of therapy
3. 2000 to 2500 cals a day
4. Only given through central line.
Nursing interventions for TPN
1. Monitor BS q6, cover with SS insulin
2. prevent infection- aseptic technique when dealing with tubing, bag changes. Change tubing/bag q24 hrs. Assess iv insertion site for for s/sx of infection
3. Do not change prescribed rate on TPN
4. If TPN runs out, hang d10w
5. Monitor daily weights, i/o, electrolytes
6. Double check RX with another RN
7. only run on an IV pump w/ inline filter.
Blood product Administration
1. Packed RBCs - most common, used for anemia, requires type and crross, must be ABO compatible, must be in patient within 4 hours.
2. Whole blood - contains RBCs, plasma, wbcs, platelets, requires type and cross, must be ABO Identical.
Blood Admin NC
1. Fresh frozen plasma - used to replace coag factors, DIC, liver disease, coumadin reversal, coagulopathies, cannot be re-frozen, must be given within 6 hrs, ABO testing to verify A or B antibodies only
2. Platelets - used to tx thrombocytopenia and bleeding. Usual dose 6-10 units. ABO compatibility is preferred, but can given mismatched platelets in emergency situations.
Admin of Blood NC cont.
1. Not to be given by students
2. Procedure specific to institution standards, require TWO RN's for check.
3. Verify MD order and pt consent
4. Blood typing and crossmatching the recipient.
5. Equipment - guage needle; sset; filters; warmers.
6. Prepare pt
7. Obtain blood product from blood bank
8. d/c all blood tubing, nothing left behind.
Blood admin policies
1. Must be followed precisely
2. Double check all numbers carefully (unit#, blood bank id, MR#, pt ID)
3. Monitor pt carefully with VS during 15 minutes to one hour.
Complications associated with Blood component therapy
1. Biological reactions - acute hemolytic reactions, delayed hemolytic reactions (14 days after), nonhemolytic reactions, allergic reactions( inc in billirubin), acute lung injury (ARDS), graft versus host disease(bone marrow transplants)
2. Nonimmune reactions - circulatory overload, potassium toxicity, hypothermia, hypocalcemia, bacterial contamination, transmission of infectious disease.
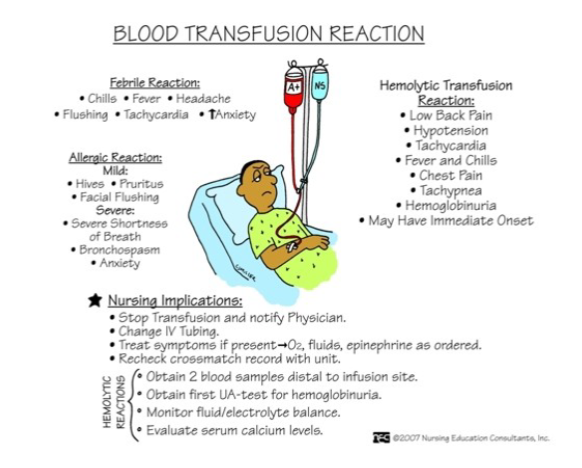
Whenver a reaction is suspected in blood transfusion
1. Terminate the transfusion, d/c the blood and blood tubing and set aside.
2. Maintain patency of the IV cannula by hanging new tubing with NS running.
3. Notify the physician and blood bank
4. Implement interventions as indicated.
Blood Transfusion recommend
1. The recommendation is to only transfuse PRBC's if the H/H is 7/21 AND the patient is symptomatic.
Blood transfusion reaction
9 abdominal regions
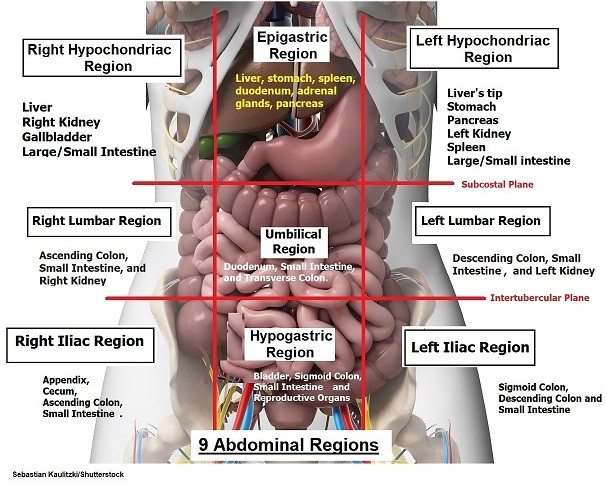
Right Upper Quadrant Organs
1. Liver- blood filter, detoxifies, produces clotting factors, stores ADEK vitamins, creates vile, important in fat,carb,protein metabolism, largest abdominal organ,
2. Gallbladder - stores bile secreted by liver.
3. Duodenum- mixes food with enzymes in digestion process, secretes amylase/lipase/bile from other organs.
4. Pancreas Head- produces enzymes amylase/lipase. Exo/endocrine functions. Endocrine- insulin secretion and glucagon. Exocrine- secretion of amylase/lipase for digestion.
5. Right Kidney / Adrenal Glands, Transverse colon
Right Lower Quadrant
1. Ascending colon
2. Appendix
3. Right reproductive organs
4. Major blood vessels and nerves (GI is % of bloodflow)
Left upper quadrant organs
1. Stomach
2. Spleen - storage site for blood, part of immune system
3. Pancreas (tail)
4. Transverse and descending colon
Left lower quadrant organs
1. sigmoid, left reproductive organs
2. major blood vessels/nerves
Nursing assessment for GI
1. Hx of present illness
2. Dyspepsia most common symptom of any gi issue, includes pain, belching, heartburn
3. GERD- chronic gerd assess for chronic cough (sign of aspiration of stomach contents)
4. Marijuana use, n/v, weight gain or loss, dirrahea/constipation, appetite
GI past health family social history
1. allergies
2. current meds
3. alcohol/drugs/tobacco use
4. nutrition
5. Oral health - toothbrushing, dental visits, lesions, dentures
6. Access to food/ability to prepare
7. Exposure to infectious disease
8. Stress
9. pregnancy
10. family history
Physical GI assessment
1. Characteristics of stool: steatorrhea (oily stool, in pancreatitis, malabsorption of fat), light gray or clay colored, stool with mucus threads (crohns, ibs, uc), small dry rockhard, loose watery stool
2. Weight, height, BMI
3. Cardiac, neurological, endocrine, and psych disorders
4. Autoimmune disorders
5. Oral cavity
6. Labs - cbc (rbc,wbc,electros,albumin-protein/nutrition, prothrombin times, LFT)
Age-related changes in GI system
Table 38-3 pg. 1213
1. Digestion and absorption of nutrients
2. Constipation
3. Decreased new cell growth rate
4. Heartburn - weakened stomach spinchter
5. Cancer rates inc w/ age
6. Ca regulation and changes and bone loss
GI nursing assessment steps
1. General observation - apperance and beahvior (remove dentures and inspect under)
2. inspection
3. auscultation
4. Percussion
5. Palpation
Preparing GI exam
1. provide privacy
2. assist/allow pt to empty bladder
3. supine position
4. expose abdomen
5. warm hands and stethoscope
6. assess painful areas LAST
Inspection - GI exam
1. Overall observation
2. flat? distended? symmetrical
3. Skin color
4. Scars
5. Peristalsis
6. Do NOT press on any visible pulsations
7. Cullen's sign - intrabd bleeding, or leakage of pancreatic enzymes
8. Grey turner's sign - blueish discoloration in flank region, indicates bleeding
9. Spider angiomas- Liver issues, cirrhosis, hepatitis, autoimmune disorder causing dilated blood vessels.
Auscultation - GI exam
1. Auscultate before you palpate
2. Use diaphragm of stethoscope
3. Hypo, Normal, hyperactive
4. Used to determine character location and freq of bowel sounds
5. Can also be used to identify vascular sounds- bruits in aortic, renal, iliac, and femoral arteries
6. Absent previously defined as no sounds in 5 minutes per quadrant, now defined as 1 minute with no sounds per quadrant.
Percussion - GI
1. Used to assess the size and density of abdominal organs
2. Can detect presence of air-filled, fluid-filled or solid massess
3. Tympany = sound of air in gut
4. Resonance = lower pitched and hallow
5. Dullness = flat sound without echoes: liver, ascites, distended bladder, spleen
Palpation - GI
1. light 1 cm, deep 5-8cm
2. Always assess tender areas last
3. Watch patient's expression
4. Tenderness and Massess are abnormal
5. Percussion can confirm palpation findings
6. Firmness or muscle rigidty may be a sign of intraabdominal bleeding or a surgical belly - STOP palpation.
Oral Mucositis
1. Erythema, edema, and ulcerations of the oral mucosa.
2. Red, shiny, or swollen mouth and gums
3. Sore and painful
4. Risk factors: alcohol, tobacco, mouthwashes, drug sensitivity, vit deficiencies (folate, zinc, iron). Side effect of chemo, smoking.
5. Can occur anywhere in GI tract, horribly painful
6. can cause airway obstruction, dysphagia, painful to eat/drink
Hiatal Hernia
1. A portion of the stomach protrudes upward through the esophageal hiatus with widening of the hiatal tunnel allowing stomach acid and enzymes to come into contact with esophageal tissue (barrett's esophagus)
2. Risk factors: Smoking, hx of pregnancy, lack of fiber, straining during bowel movements, obesity, strenuous physical activity
3. endoscopy to confirm hernia, x ray, EGD, barium swallow
GERD
1. Patho: chronic disorder, retrograde flow of GI contents from stomach into esophagus, with or without tissue damage. One of the most common western disease with 10-20% effected.
2. Management: antacids (increase gastric pH), histamine receptor antagonists (decrease acid production), prokinetic medications (increase gastric emptying), proton pump inhibitors (decrease gastric acid production), small number of pts may require surgery.
3. Complications: barret's, malignancy, fibrosis/scarring, strictures
4. RF: pregnancy, obesity, old age, overeating, muscle atrophy, alcohol
Oral pharynx cancer
1. patho: can occur in any part of mouth or throat (curable if discovered early)
2. RF: tobacco or nicotine use, excessive alcohol, HPV inf, and hx of previous head/neck cancer
3. CM: few or no symptoms in early stages
4. Later stages: include painless sore or lesion that bleeds easily and doesn't heal, oral tenderness, diff in chewing, swallowing, or talking, blood sputum, limited rom for jaw, weight loss, neck mass or enlarged cervical lymph nodes.
5. May present as red or white patch in mouth or throat
6. Typical lesion is painless indurated ulcer with raised edges.
Oral pharynx diagnostics and management
1. Dx: oral and cervical lymph node assessment. PET, mri, endoscopy, laryngoscopy, biopsy, hpv status testing
2. Management: surgical resection and chemoradiation.
3. Tx choice depends on location of cancer
4. Metastasis often occurs in neck lymphatic channel and may require neck dissection with reconstructive surgery.
5. Nursing management includes nutrition interventions, assessment of verbal comms, airway management post op with possible suctioning
6. Pt may require a temporary or permanent tracheostomy post surgery.
Esophageal Cancer
1. devasting disease with protracted treatment that diminishes qol and is lethal in a significant number of cases
2. Almost 18.5k new cases are diagnosed a year with about 14k cases mend and 4k are women.
3. The overall 5-year survival rate is about 20%, the cancer can spread beyond the mucosal layers and erode/perforate the mediastinum and great vessels.
4. The 5-year survival rate is caught in early stages is 90%.
Esophageal cancer patho
1. Etiology is unknown. two types
2. Squamous: lining of the esophagus / upper 2/3 of esophagus
3. Adenocarcinoma: glandular tissue distal esophagus and gastroesophageal junction / lower 1/3 of esophagus
4. RF: smoking, etoh, untreated GERD
5. Other risk factors include chronic ingestion of hot liquids or foods, nutritional deficiencies, poor oral hygiene, and some esophageal medical conditions.
Esophageal cancer CM
1. advanced ulceration lesion of esophagus often is present prior to symptom manifestation.
2. Progressive dysphagia (most common symptom)
3. Weight loss
4. Bleeding / hemorrahge
5. Later symptoms include substernal pain, persistent hiccup, resp distress, halitosis
6. Psychosocial assessment
Esophageal Dx tests and Management
1. EGD w/ biopsy, PET for staging, CT of chest/abs, Endoscopic ultrasound, thoracoscopy and laparoscopy
2. Management: nonsurgical- chemo, radiation, nutrition, swallow therapy, esophageal dilation
3. Surgical management: palliative surgical interventions to restore patient's ability to swallow and maintain optimal nutrition. PEG tube placement.
Surgical management of Esophageal cancers
1. Esophagectomy: removal of part or all of the esophagus with use of Dacron graft to replace resected part
2. Esophagogastrostomy: resection of portion of esophagus and anastomosis of remaining portion to stomach.
Nursing Post OP care for esophageal cancer
1. NG tube with blood drainage for 8-12 hours, gradually changes to greenish yellow
2. Do not reposition or reinsert NG tube without surgeon's approval
3. Pulmonary care that includes turning/deep breathe every 2 hours, IS, sitting in chair, possible neb tx
4. Pain control usually PCA and epidural
5. Strict i/o
6. Strict NPO, no sips or chips until pt is cleared
7. Chest tube mangement
8. Trach care
9. May have cardiac complications / require mangement
Gastric Cancer
1. patho: malignant epithelial tumor that infiltrates the mucous producing cells of the stomach, more common in lower socioeconomic groups, males 2x more than women, causes unknown, does have RFs, most frequently found in distal portion
2. CM: often asymptomatic until late in course, indigestion, anorexia, weight loss, vague epigastric pain, vomiting's, abd mass
Gastric Cancer Dx, Management, Complications
1. dx: endoscopy with biopsy, endoscopy, CT of chest/abs, cytological students of gastric secretions, labs, barium x rays of upper GI tract
2. Management: often multimodal- surgery, chemo, radiation. Surgery may include total gastrectomy with reconstruction of the GI tract, partial gastrectomy, and complication management/palliative gastric or esophageal bypass.
3. Complications: dumping syndrome, hemorrhage, bile reflux, gastric outlet obstruction.
GI bleed
1. any form of bleeding that starts in the GI tract from the pharynx to the anus.
2. Symptoms of a disease or condition
3. Bleeding can range from nearly undetectable to acute, massive and life-threatening bleeding.
4. Upper GI bleed(stomach, large intestine), lower gi bleed, acute (sudden massive bleed, hypovolemia) vs chronic (slow, unnoticed)
Incidence and Mortality of UGI bleeding
1. 400k hospitalizations in USA per year
2. Mortality rate 5-10%
3. More than 90% of UGI bleeds are caused by peptic ulcers, erosive gastritis, Mallory-Weiss tears, or esophagogastric varices.
Clinical Manifestations of GI bleeds
1. Occult blood - usually 3 mL's for pos result
2. Hematemesis - blood in vomit
3. Melena - black tarry smelly stool (usually upper) 100-200mL
4. Hematochezia - bright red blood in stool or maroon stool. Most common sign of Lower GI bleed.
5. Distal to the ligament of Treitz - hematemesis and melena above, below hematochezia.
Lower GI bleeds
1. Hematochezia: most common presenting symptom. Overt blood or occult (hidden)
2. Causes: diverticulosis (small pouches develop in large intestine), angiodysplasias (abnormal small blood vessels causing bleeding), colon polyps, tumors, inflammatory bowel disease, hemorrhoids, anal fissures
3. Most cases resolve spontaneously, but with chance for rebleed.
Peptic ulcer disease
1. Most common cause of upper GI bleed
2. Mucosal damage in portion of GI tract exposed to acid-pepsin secretion
3. Risk factors: H. pylori (90% of duodenal ulcers and 75% gastric ulcers) NSAIDs
4. nsaids (15-30% long term users develop ulcers)
CM of peptic ulcer disease
1. pain upper abdomen (intermittent)
2. N/v
3. Anorexia weight loss
Dx of peptic ulcer disease
1. Pt hx
2. Endoscopy
3. Angiography
4. Serologic or breath test for h. pylori
5. Histologic analysis of endoscopic biopsies.
Tx for peptic ulcer disease
1. Combination of antibiotic therapy and PPIs
2. Sucralfate (carafate) to promote mucosal barrier
3. Bismuth subsalicylate
4. Antacids
Upper GI bleeds non-ulcer etiologies
1. Stress related mucosal disease - PUD protocols
2. Erosive of hemorrhagic gastritis
3. Esophageal and gastric varices
4. Mallory-weiss tears
5. Arteriovenous malformation - small mucosal and mucosal blood vessels that bleed
Acute lower GI bleeding
1. Bleeding beyond the ligament of Treitz
2. Causes: diverticulosis or arteriovenous malformations
3. Others: ischemic colitis, internal hemorrhoids, rectal ulcers, and neoplasms.
4. Usually slow and intermittent do not require hospitalization
Nursing management of acute gi bleed
1. Assess the severity of blood loss
2. Administer IV replacement
3. Assist in determining the cause of bleeding (increase in BUN with GI bleed, suggests fluid volume deficit)
4. Planning and implementing treatment (iron and blood products if needed)
5. Provide supportive care and education.
GI resuscitation
1. management of the hemodynamically unstable pt
2. Oxygenation
3. Lactate levels - greater inc = severity of condition
4. Volume resuscitation: 2 IVs, fluids
5. Blood products (keep Hgb >7 and hematocrit > 28%)
6. Monitor for and report: tachycardia, decreased BP, hematemesis, bloody or tarry stools.
ETOH considerations for GI
1. Hemorrhage that is result of chronic alcohol abuse
2. Closely observe for DTs
3. Agitation
4. Uncontrolled shaking, sweating, vivid hallucinations
Pt education for GI bleeds
1. No smoking or alcohol
2. Need for long-term follow up care
3. Instruction if an acute hemorrhage occurs in future
4. Pt/family taught how to avoid future bleeding episodes
5. Made aware of consequences of noncompliance with diet and drug therapy
6. Emphasize that no drugs other than prescribed should be taken.
Source of bleed determinants
1. mouth: bright red = upper gi, maroon = severe lower gi, black/coffee = old slowed or stopped bleed
2. Rectum: red = lower gi, maroon = severe upper GI, black = slow/old lower GI.
Cholecystitis
1. Inflammation of the gallbladder: calculous cholecystitis: inflammation from gallstones (cholelithiasis) that obstruct the bile outflow. (over 90% of cases)
2. Acalculous cholecystitis: inflamm w/o gallstones. Occurs after major surgical procedures, orthopedic procedures, severe trauma, burns, gallbladder, infection, cystic bile duct obstruction, or multiple blood transfusions.
3. bile digests fat, mostly happens in duodenum which sends signal to gallbladder so it can digest fat.
Cholecystitis Patho
1. Calculous cholecystitis: bile remains in the gallbladder due to gallstone blockage creating a chemical reaction.
2. Stone can be made of cholesterol, bile salts (calcium bilirubinate)
3. Autolysis and edema occur with gallbladder vessel compression compromising blood supply.
4. Secondary infection occurs in about 50% of cases
5. RFs, 4F fair skin, fat, fertile, forty
Cholecystitis: CM
1. RUQ pain and tenderness - may occur after eating rich or fatty foods.
2. Rebound tenderness(more pain when released pressure), guarding, restlessness.
3. Fever, tachycardia, elevated WBCs, anorexia, n/v, positive murphy's sign(inhale while doc hooks fingers under liver and presses in, pain = inflam, pos = pause/stop breathin), urine and stool color changes, vitamin deficiencies.
4. EKG to rule out cardiac issue
Cholecystitis Dx
1. Lab- bilirubin, electrolytes, CBC, lft, pancreatic enzymes (amylase/lipase)
2. imaging: ab x ray, ultrasound, oral cholecystography, radionuclide imaging.
3. Endoscopic retrograde cholangiopancreatography (ercp) - can remove gallstones and help dx, combined with upper GI endoscopy/xray, NPO midnight night before tho can take BP meds if needed with water.
4. Percutaneous transhepatic cholangiography - contrast medium injected into bile ducts to better visualize gallbladder.
Cholecystitis Interventions
1. Non-surgical: pharmacological(morphine goto, antibiotics), diet and supportive therapies (avoid fatty/dairy/meats), extracorporeal shock wave lithotripsy (ESWL), intracorporal lithotripsy (laser)
2. Surgical: laparoscopic (most common), small-incision cholecystectomy
3. with gallbladder removal bile drains directly into duodenum
Cholecystitis nursing interventions
1. Pain management (IV pain meds)
2. Hydration and nutrition, during episode pt NPO, let GI rest.
3. Post-op management: pain, resp(IS,TCDB,support incisions w/cough), skin integrity, drains(c-drain helps drain fluid from gallbladder, T-tube- help drain bile and inject dye into tube for imaging, has drainage bag, cap/clamp tube, drain below insertion site in semifowler's), nutrition, complications (bleeding, abd rigidity, signs of infection, gi changes, n/v, loss of appetite )
3a. replace fluids, give antiemetics, start with clear liquids and advance diet (esp low fat)
4. education - post op exp, signs to call for, n/v rigid pain, tube/drain management
Pancreas
1. Exocrine: cells that excrete inactive digestive enzymes into pancreatic duct. Amylase -break down carbs to glucose. Protease (trypsin) - breaks down proteins. Lipase - breaks down fats
2. Endocrine: insulin, glucagon, islets of langerhans
Pancreatitis
1. inflammation of the pancreas
2. Two types: acute / chronic
3. Reversible
4. Autodigestion