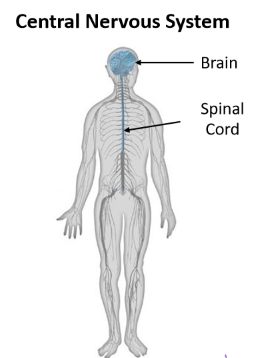
The central nervous system is composed of the ______and __________.
brain; spinal cord
The peripheral nervous system is composed of_____________, _________ and ____________.
sensory receptors, nerves; motor nerves
Brain
the most complex organ in the human body
What is the computing hardware of the brain?
Neurons!
How many neurons does the brain consist of alone?
86 billion
How many synapses are there between brain neurons?
150 trillion synapses
What is the average brain mass?
1.3-1.5kg in adults
What percent of our basal metabolism does our brain use to power itself?
20-25%
**It uses primarily glucose!
Spinal cord
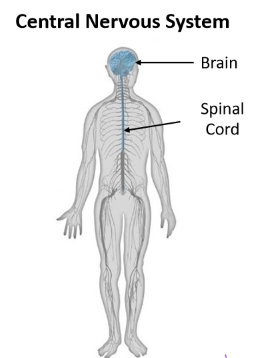
transmits electrical impulses to and from the brain
What are the two types of tracts in the spinal cord?
Afferent and Efferent tracks (also we have sensorimotor integration)

Afferent tracts
transmit electrical impulses from the body to the brain
(inward)
Efferent tracts
transmit electrical impulses from the brain to the body
(outward)
Sensorimotor integration
Transform sensory into basic motor activity (e.g. tendon tap reflex)
-incorporating sensation about one's body and the external environment to shape movement
- link between nerves and muscle
Example of a polysynaptic reflex:
redraw reflex
Nerves

send electrical impulses to and from the spinal cord
Sensory nerves

send sensory information from active sensory receptors to the spinal cord
Motor nerves

send motor commands from the spinal cord to activate skeletal muscle
Receptors

modified ending of sensory nerves. First step in processing that leads to our sense of touch and proprioception (sense of body position, motion and force in the absence of vision)
What are the 4 receptor cells?
Merkle, Meissner, Ruffini, Pacinian
What is in charge of proprioception?
- Muscle spindles
- Golgi tendon organ = force through muscle
What are the two divisions of the peripheral nervous system?
- The autonomic division: controls self-regulated action of internal organs and glands
- Somatic division: controls voluntary movement of skeletal muscles
What does the PNS provide information about? What role does the CNS have?
the state of the body and environment.
**The CNS processes this information and generates appropriate responses
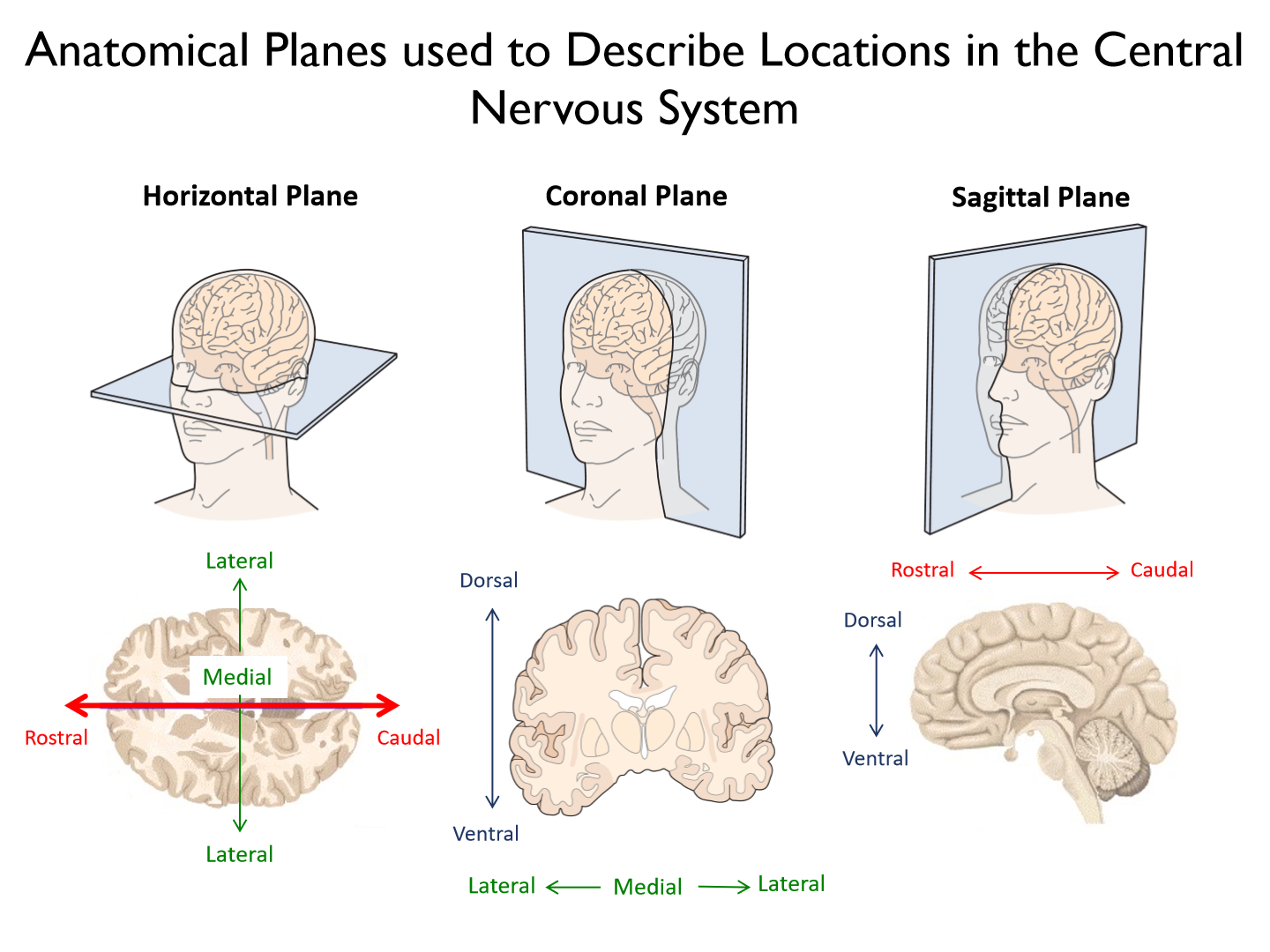
Rostral
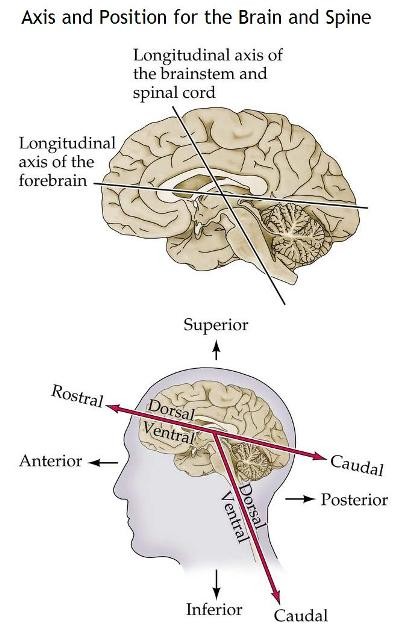
towards the nose
Caudal
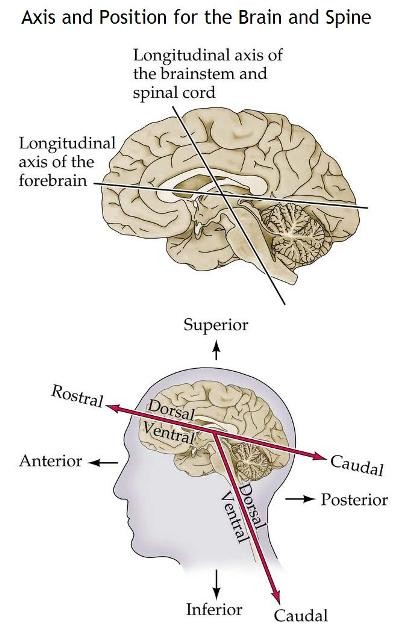
towards the coccyx (tail bone)
Ventral
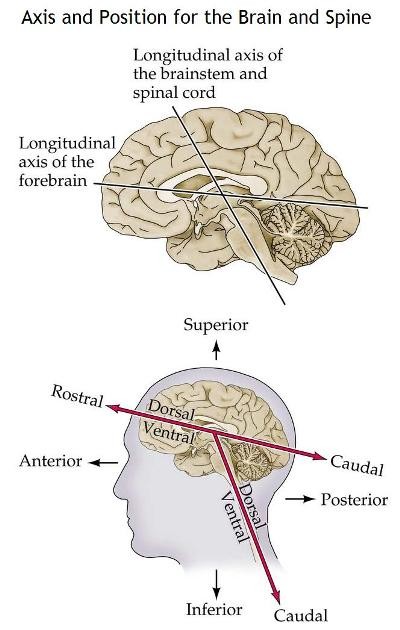
(anterior) towards the belly
Dorsal
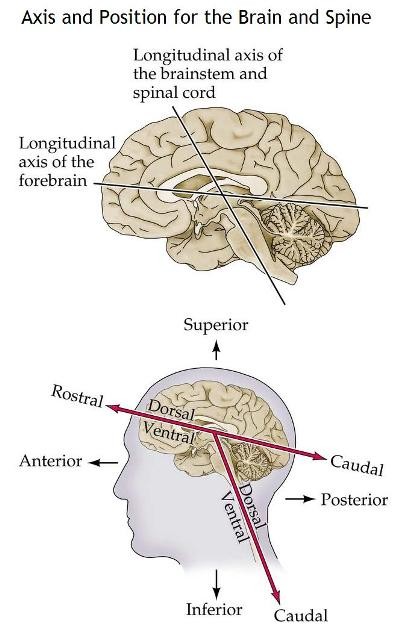
(posterior) towards the back or top of head
Coronal slice
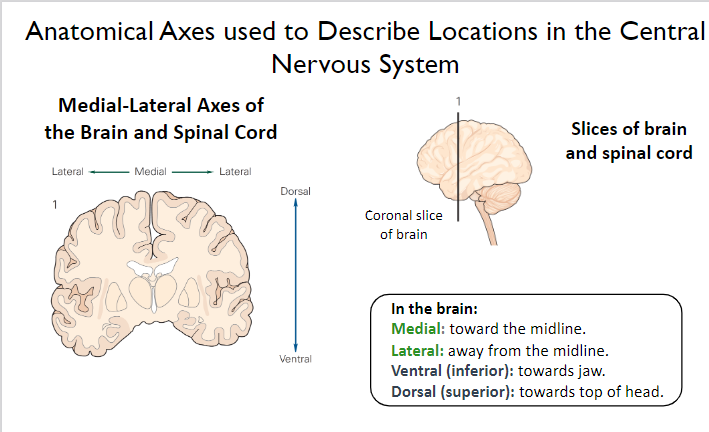
(frontal plane slice)
Medial
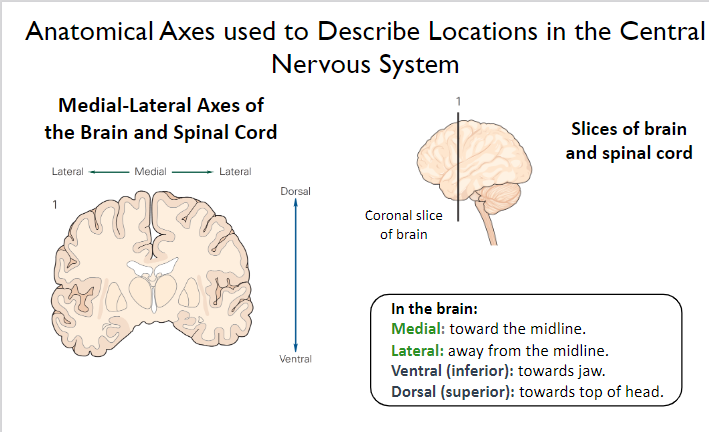
Towards the midline
Lateral
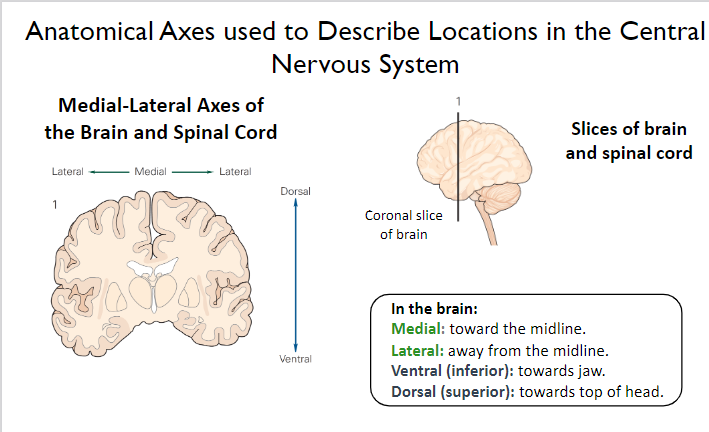
away from the midline
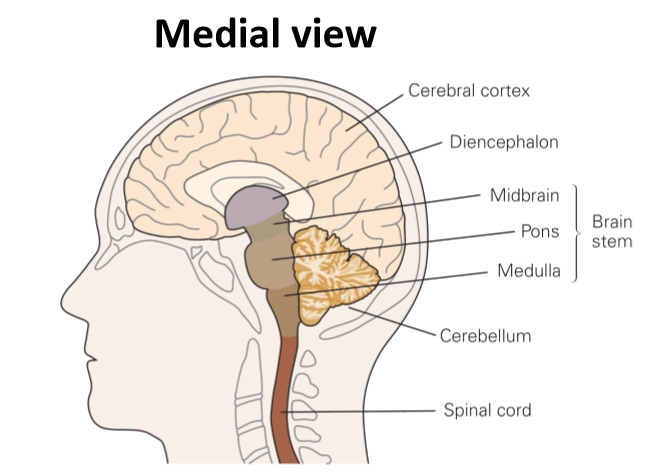
Look at the picture
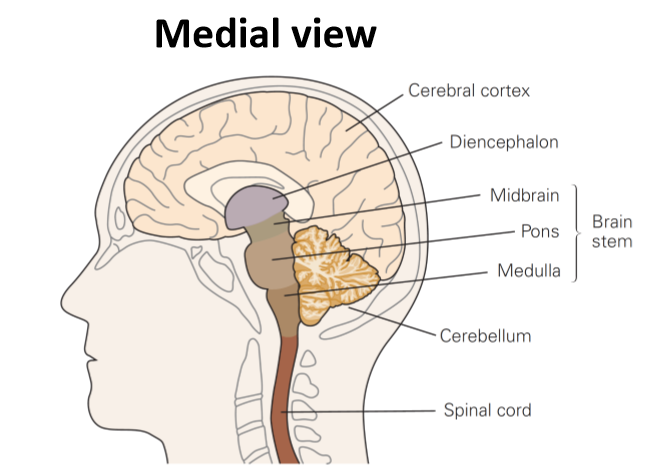
What are the 4 subdivided areas of the brain?
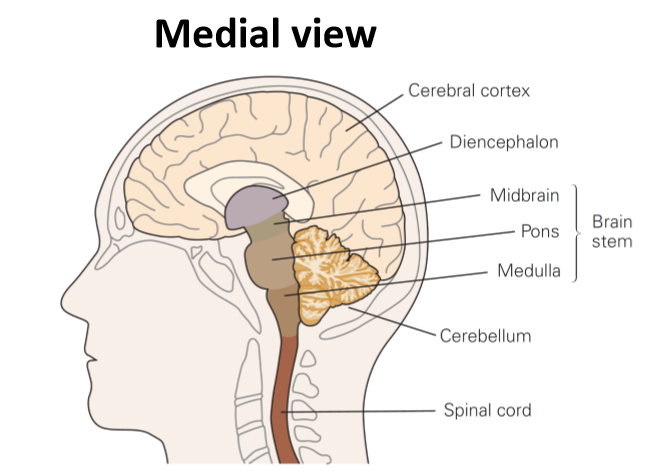
1. Cerebrum (thoughts)
2. Diencephalon (relay center)
3. Brainstem (life functions, e.g. breathing, swallowing)
4. Cerebellum (posture & balance, corrects error)
What does the cerebrum consist of?
1. 2 hemispheres (left - R hand and right - L hand)
2. Cerebral cortex (gray matter - upper level processing)
3. White matter (including corpus callosum)
Corpus callosum
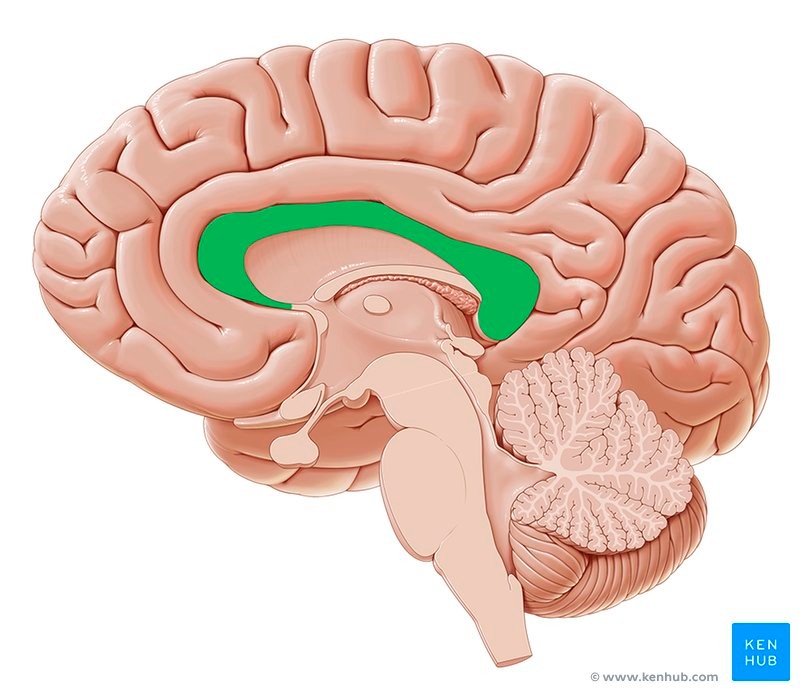
communication between the hemispheres
What are the three deep-lying neural structures of the cerebrum?
1. Basal ganglia
2. Amygdala
3. Hippocampus
Basal ganglia
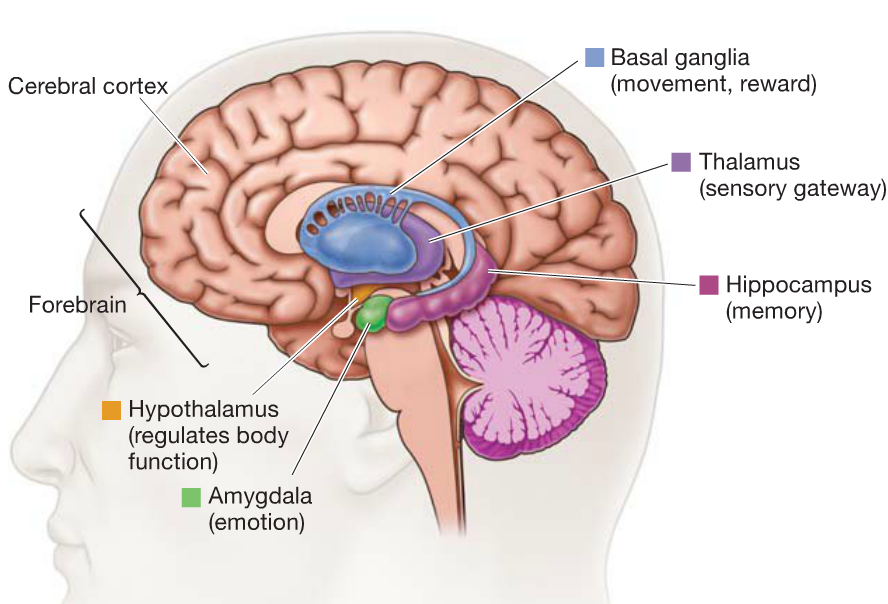
movement (vigor, amplitude) and motor learning
Amygdala
Expression of emotion
Hippocampus
memory formation
Cool fact: there are place cells in the hippocampus to remember familiar environments and when you are reminded of a place (smell, vision, etc) these cells fire
What are the largest part of the brain?
Cerebral hemispheres
What are cerebral hemispheres responsible for?
perceptual, motor (mostly planning) and cognitive function.
Do the subdivisions of the cerebrum only exist in one hemisphere?
NO. All of these structures are in both hemispheres of the brain, with slightbilateral differences (e.g., handedness, especially in cortex). Each structureis subdivided into several anatomically and functionally distinct areas.
- Hand dominance = motor cortex has more connection and larger SA for specific digits
What are the 4 lobes of the cerebral cortex

1. Frontal lobe
2. Parietal lobe
3. Occipital lobe
4. Temporal lobe
What is each lobe named after?
overlying cranial bones that form the skull
Frontal lobe functions
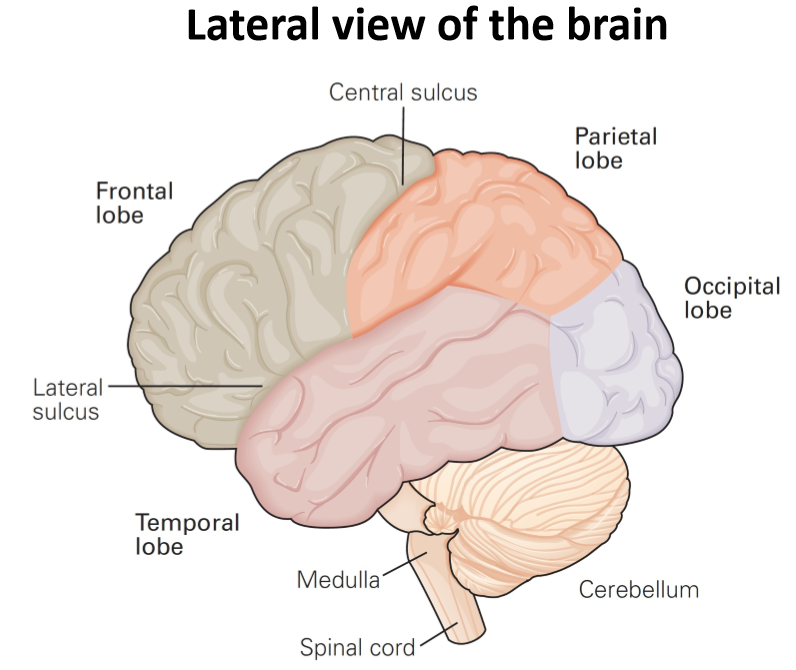
motor planning, organizing behavior, decision making, working memory.
*lots of higher functions
Parietal lobe functions
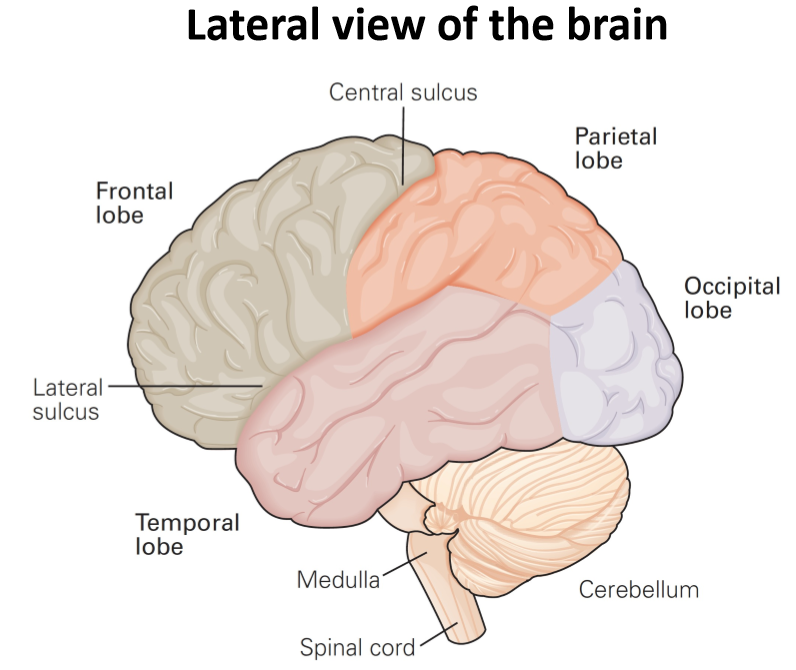
sensory guidance of motor actions, multisensory integration, spatial awareness.
*lots of vestibular cues (balance and spatial orientation for the purpose of coordinating movement with balance)
Occipital lobe functions
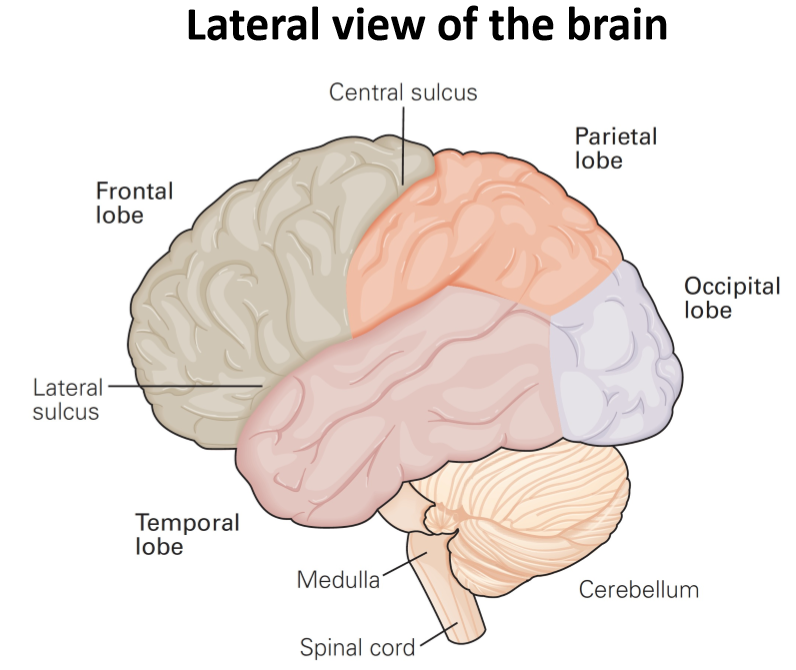
early visual processing (direction, orientation, colour, motion)
Temporal lobe functions
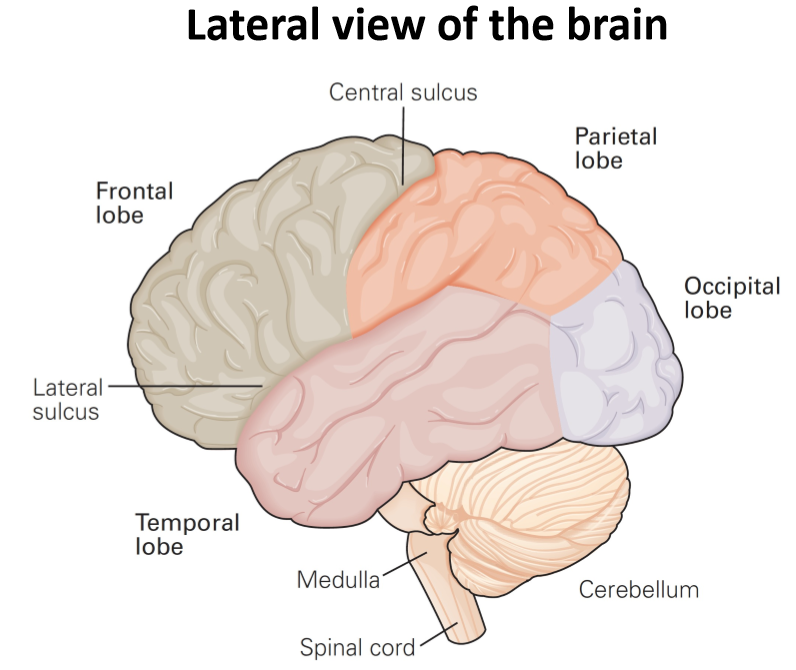
vision, hearing, memory, language
Are the lobes as far as the brain subdivides?
NO. Each lobe of cerebral cortex is further subdivided into several anatomically and functionally distinct regions.
Corpus callosum description
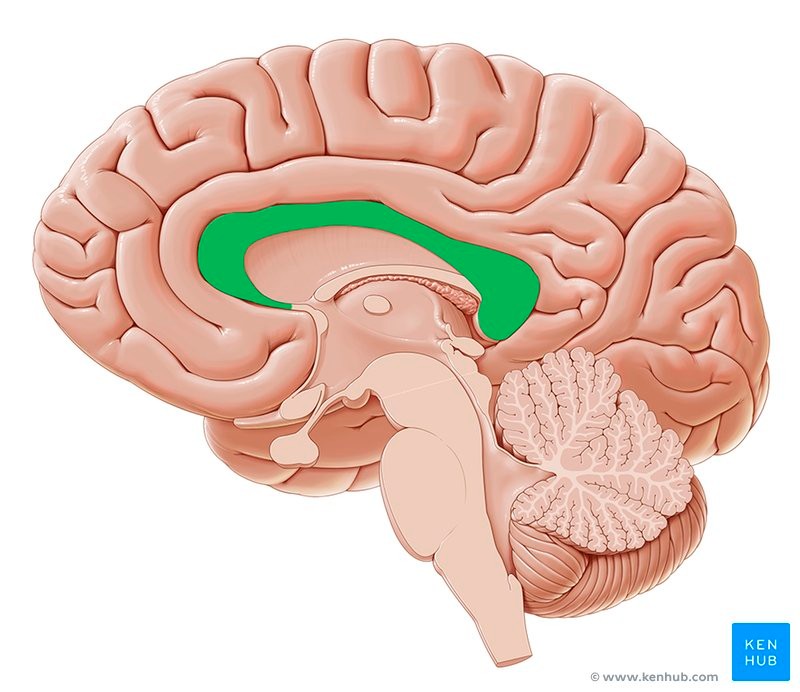
The corpus callosum (also known as callosal commissure) is a wide, flatbundle of axons that connects and allows communication betweenstructures in the two cerebral hemispheres.
* allows for a balance of forces and integrated movement (e.g. belly rub and head pat)
What does the diencephalon consist of?
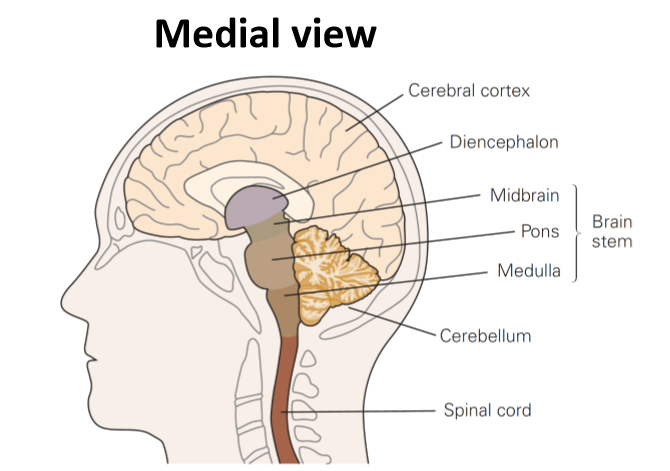
1. Thalamus
2. Hypothalamus
Thalamus
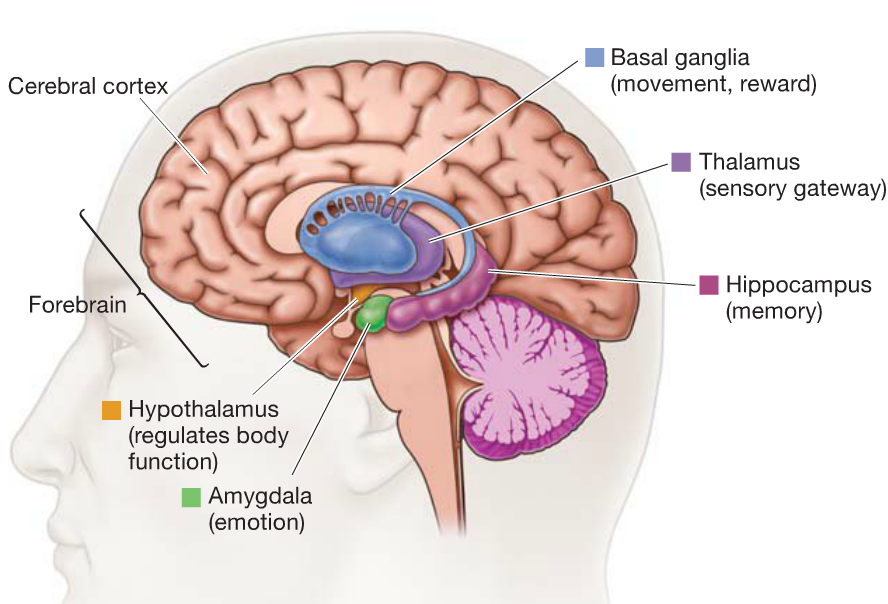
• Essential link in sensory pathways(aside from olfactory receptors) from periphery to brain. (temp., cutaneous, pain, etc.)
• Interconnects cerebellum and basal ganglia with regions of cerebral cortex involved in cognition and movement. (info both in and out)
**Relay center
Hypothalamus
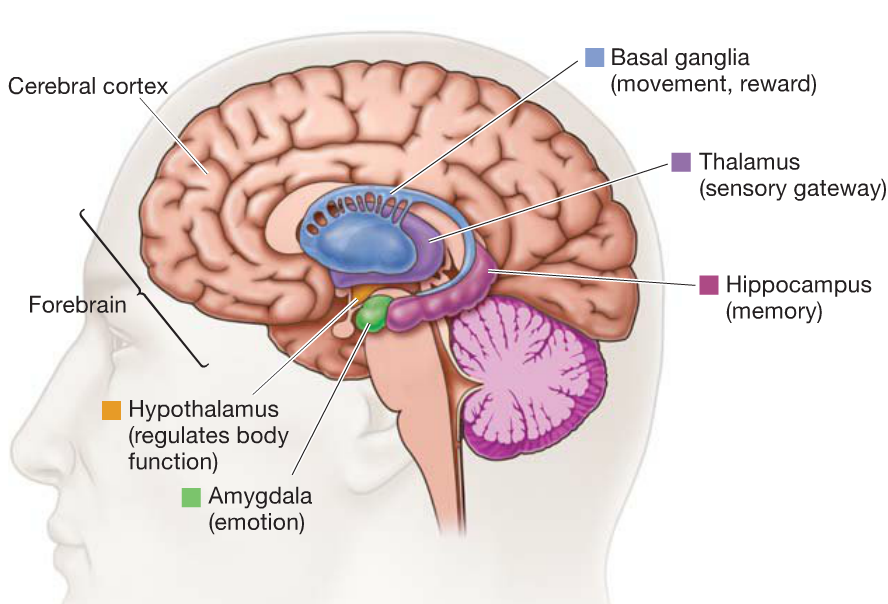
• Somatic growth, eating, drinking.
• Essential component of neuro-endocrine system (pituitary gland). (GH, FSH, etc.)
• Motivation (release dopamine, norepi., epi., etc.) and arousal
What does the brainstem consist of?
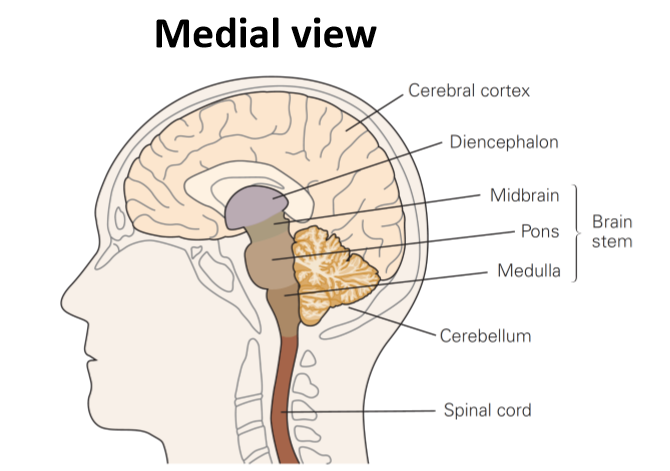
1. Midbrain
2. Pons
3. Medulla
Midbrain
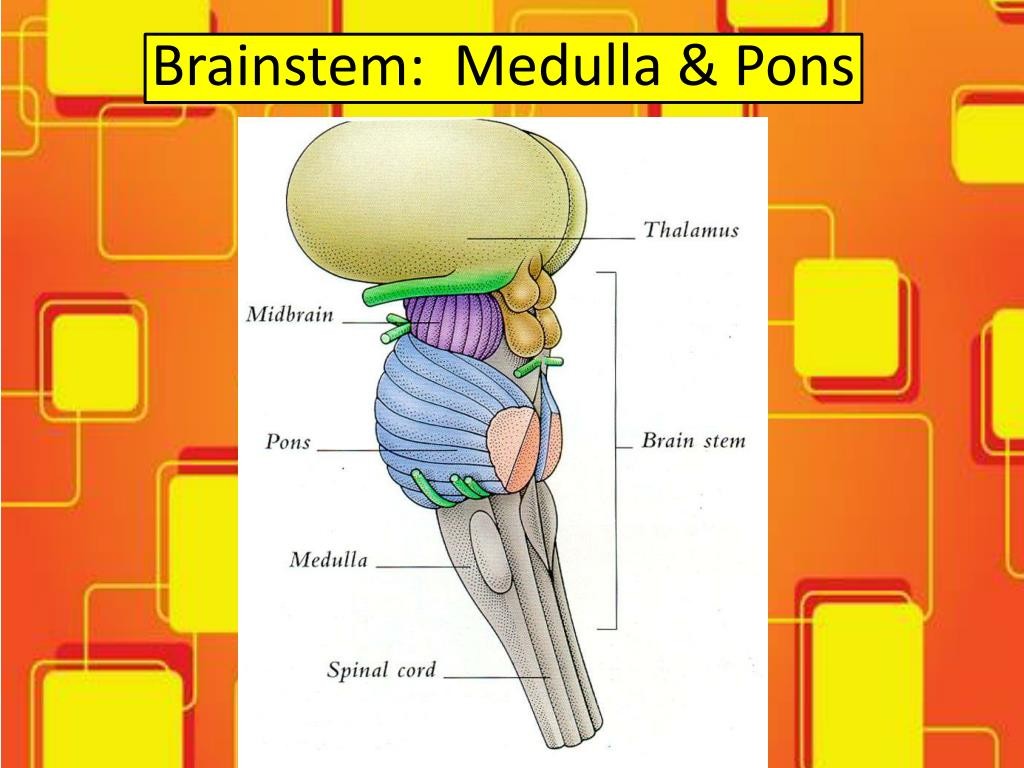
rostral to pons
• Linkages between cerebellum, basalganglia, and cerebral cortex.
• Involved in hearing and control of eye movements (oculomotor control).
(Vestibular function = VOR reflex)
Pons
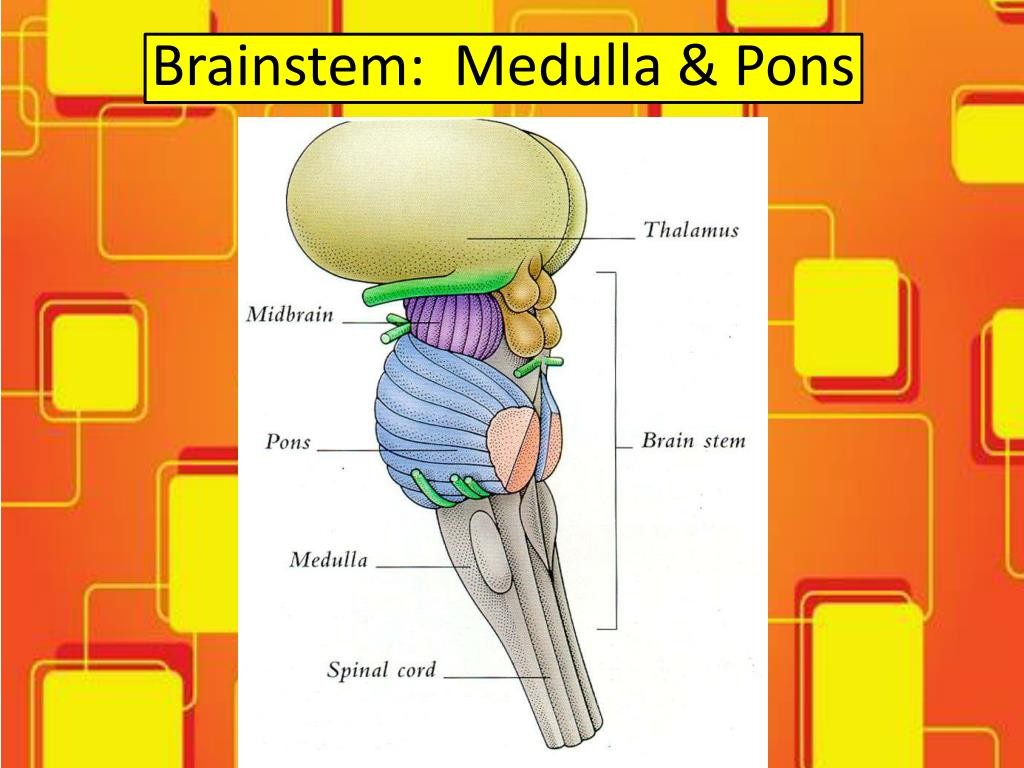
rostral to medulla, protrudes from ventral surface of spinal cord.
• Pontine nucleus: Relay info about sensation and movement from cerebral cortex to cerebellum.
• Sleep, respiration, taste.
Crossing over of controls
Medulla
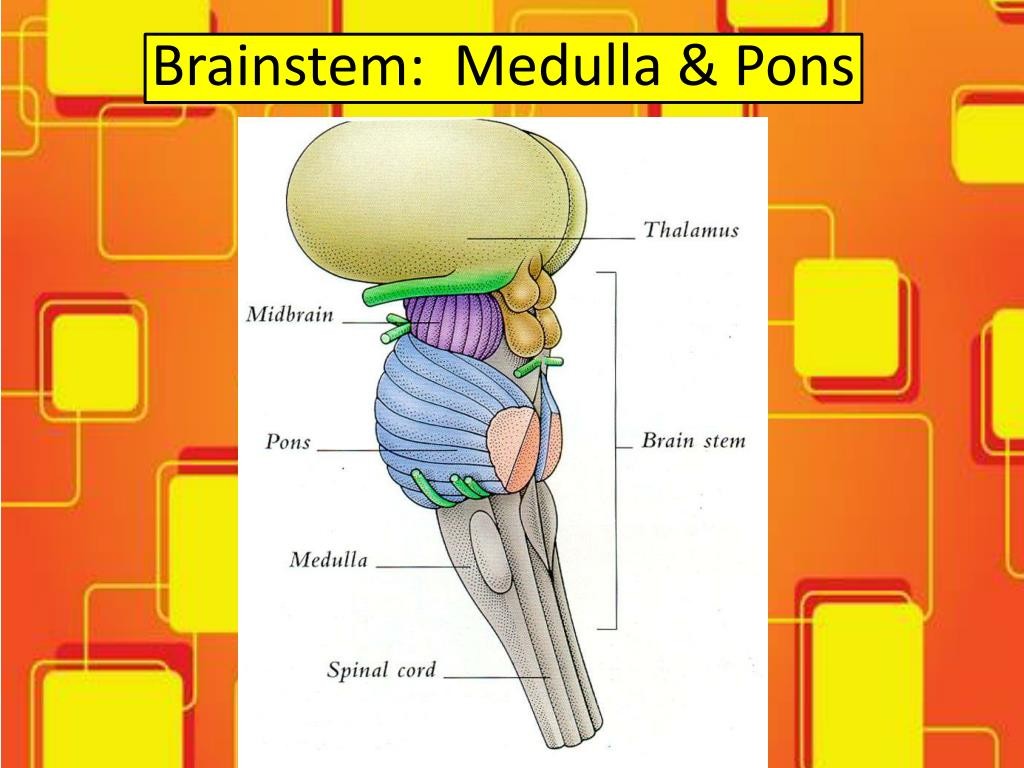
caudal part of brainstem and direct extension of spinal cord.
• Regulates blood pressure and respiration.
• Early pathways of taste, hearing, balance, and control of head, neck and limb muscles.
Cerebellum functions

1. Maintaining posture and balance.
2. Coordinating head, eye and arm movements.
3. Error-based motor learning.
4. Receives somatosensory information from the spinal cord.
5. Receives copies of motor commands from cerebral cortex.
What is a cool fact about neurons in the cerebellum?

Despite accounting for less than 10% of brain volume, the cerebellumcontains more than 50% of the brain’s neurons. It has more neurons thanany other brain structure, including cerebral cortex!
What tells us we have deviated from our initial path?
muscle spindles, golgi tendon organ, eyes and cutaneous receptors
What are the 3 main functions of the spinal cord?
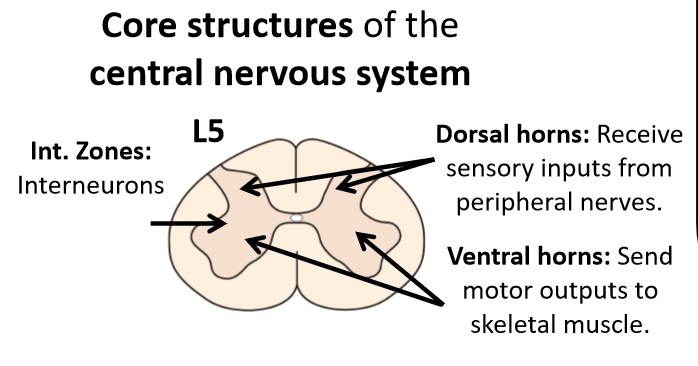
1. Receives sensory information from skin, muscles, and joints. (free nerve endings, thermoreceptors, etc.)
2. Contains motor neurons responsible for voluntary movements. (ventral horn)
3. Performs basic integration of somatosensory feedback and motor responses (reflexes).
- reflex is also integrated and higher centers can override
What are the three divisions of the spinal cord?
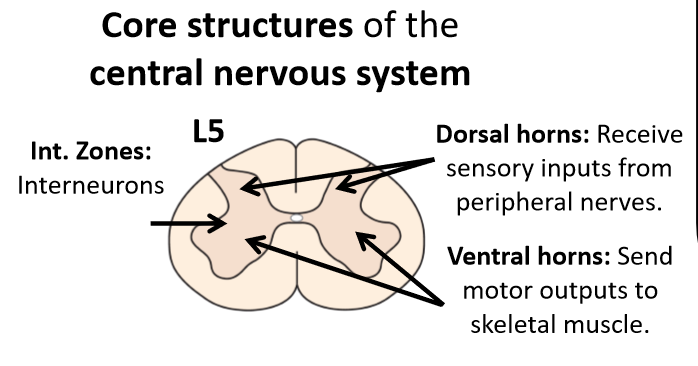
1. dorsal horn
2. ventral horn
3. intermediate zones
Dorsal horn
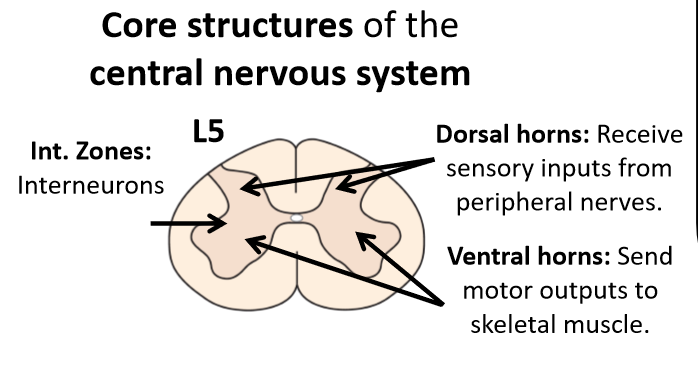
Sensory neurons (cell bodies in the dorsal route ganglia) from muscles and skin terminate in the dorsal horn of the spinal cord. (input)
Ventral horn
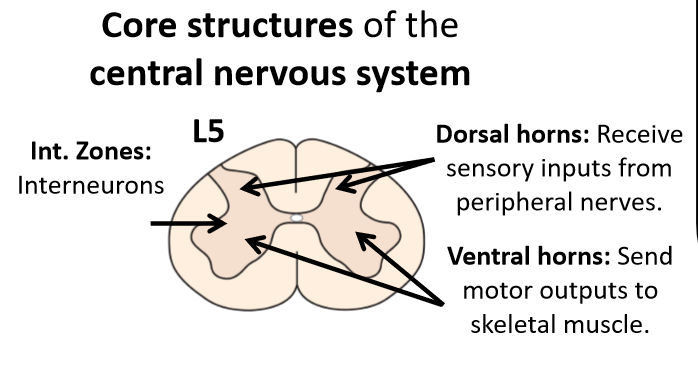
Cell bodies and axons of motor neurons that influence muscle firing patterns. (output)
Intermediate zones
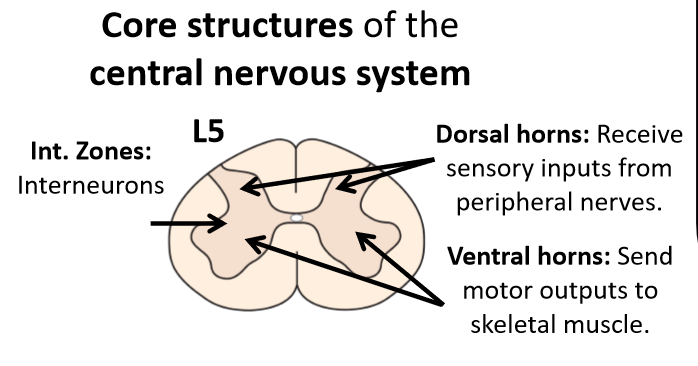
Interneurons that influence firing patterns of sensory (dorsal horn) neurons and motor neurons (ventral horn)
- aid in the decussation of pain and temp. receptors when entering the spine
- aid in polysynaptic reflexes such as the tendon tap (interneuron splits so that alpha motor neuron will cause contraction and inhibitory interneuron will allow other muscle to relax.
Topdown control
prevent reflex through anticipation
What is the largest and simplest component of the CNS
the spinal cord
What is the spinal cord composed of?
31 pairs of sensory and motor nerves
What does sensory division in the spine carry?
somatosensory, touch, pain, temp., and information from visceral sensory organs
What are spinal motor neurons?
the 'final common pathway' through which all higher brain areas controlling movement must act
does the thickness of the spinal cord vary?
Yes! it varies along its length
What is cervical enlargement caused by?
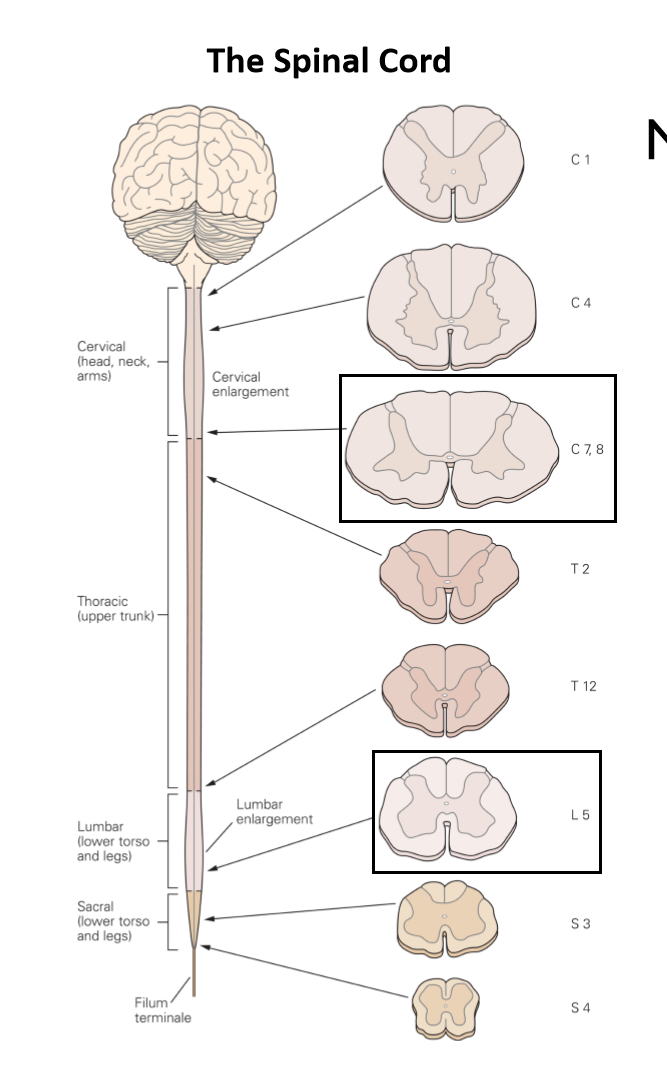
Large number of sensory and motor fibers entering and leaving the spinal cord to innervate the upper limbs
What is lumbar enlargement caused by?
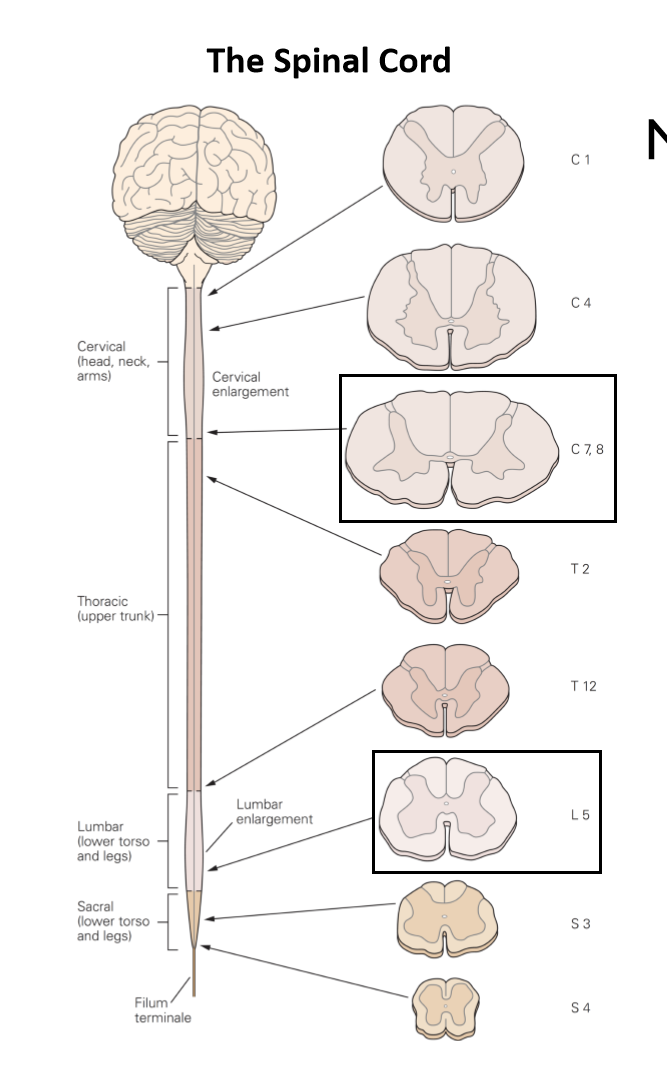
Large number of sensory and motor fibers entering and leaving the spinal cord to innervate the lower limbs
As you move up the spine, what do you see?
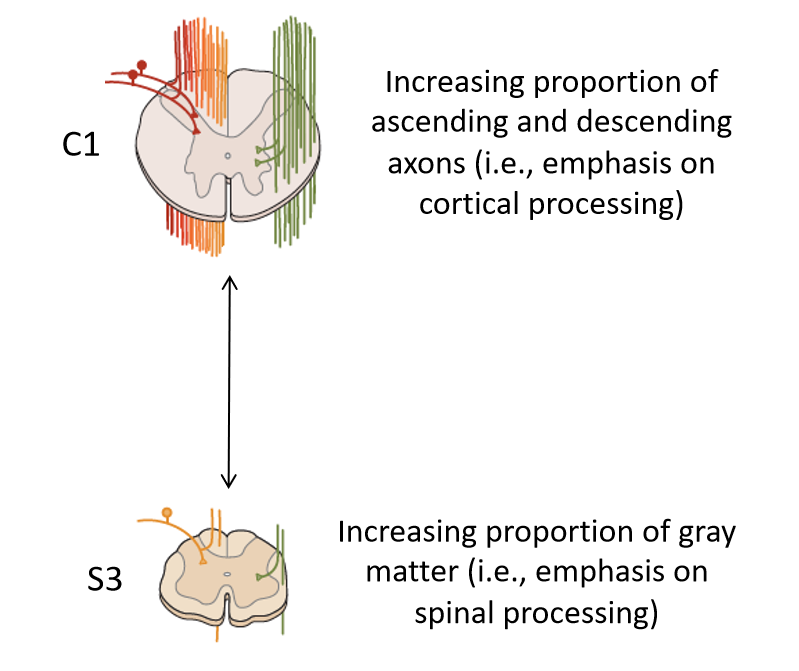
An increasing proportion of ascending and descending axons (i.e. emphasis on cortical processing)
- based on level of spine
- more and more information as it also must carry lower portion
- more white matter to carry all the nerves
As you move down the spine what
increasing proportion of gray matter (i.e. emphasis on spinal processing)
Why does the cerebellum receive copies of motor commands from the cerebral cortex?
So that we consciously know what the motor plan was so that we may fix mistakes by comparing it to our somatosensory information being received from the spinal cord.
Reciprocal inhibition
e.g. reflex: one muscle contracts, the opposing one relaxes
- The interneuron turns the excitatory impulse into an inhibitory through GABA neurotransmitter
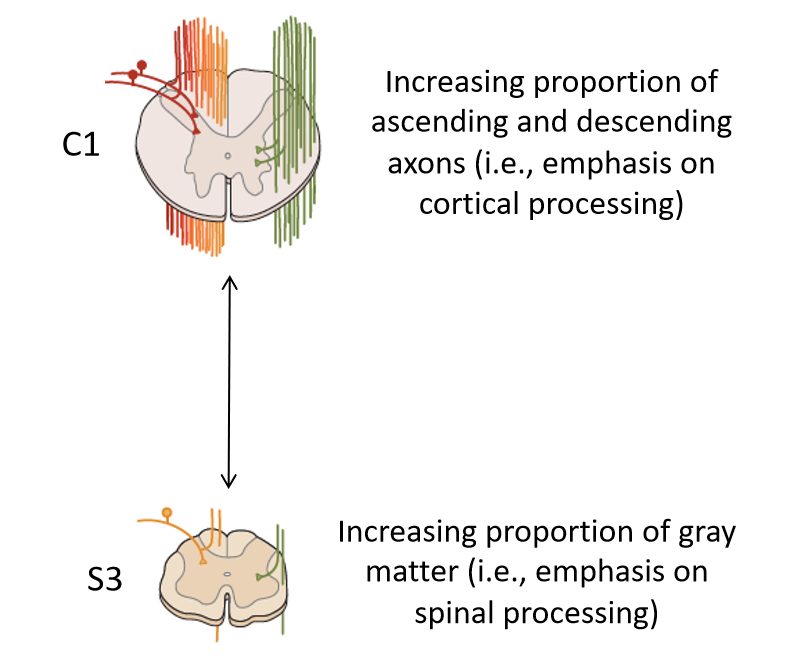
What are some tools/techniques to understand the sensorimotor system?
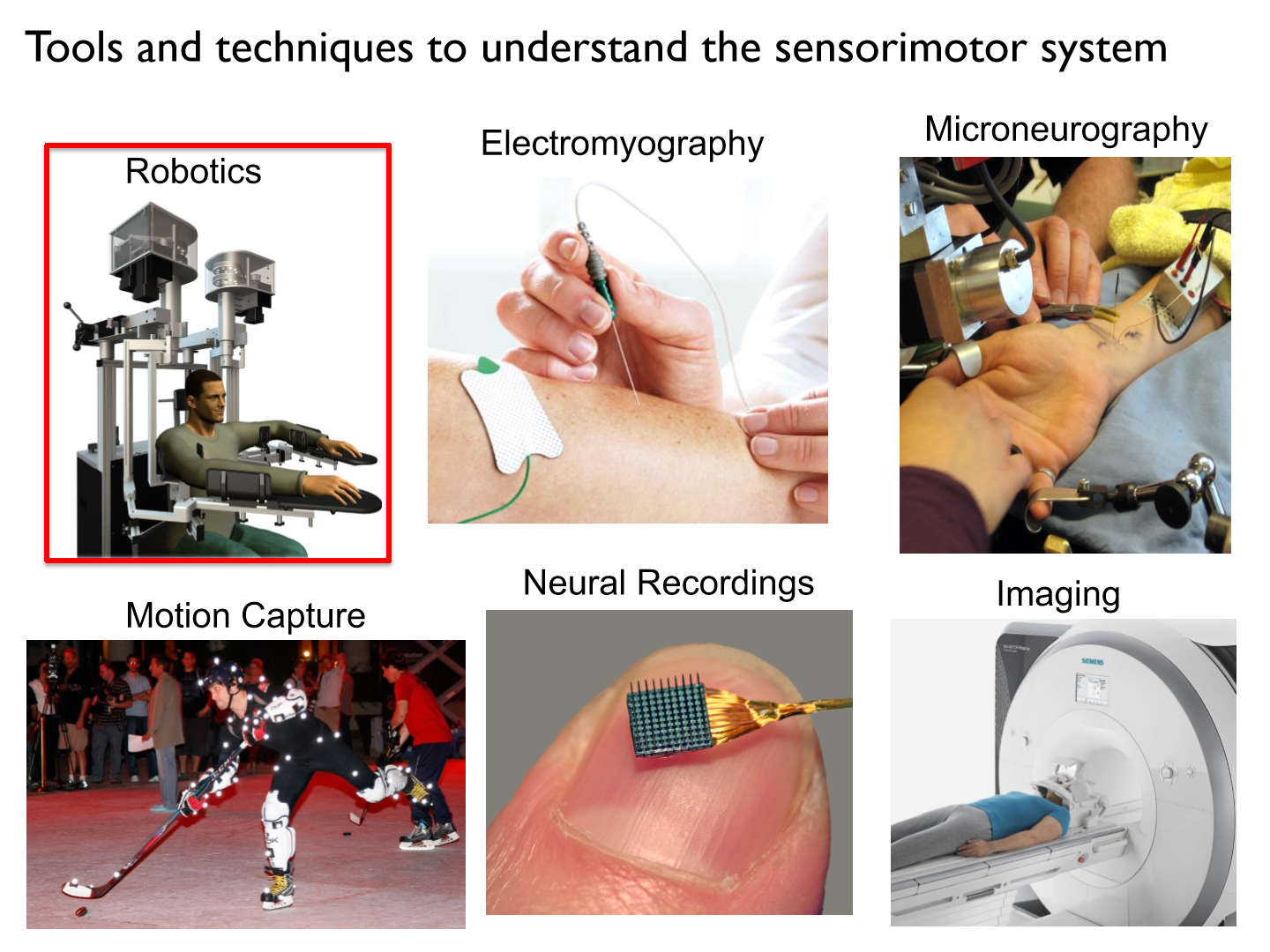
Robotics
a non-invasive tool that can be used to monitor and perturb movements to examine sensory and motor functions.
Torque motors
can be used to apply independent loads at the shoulder and/or elbow
How do we adjust robots to fit the participant's arm?
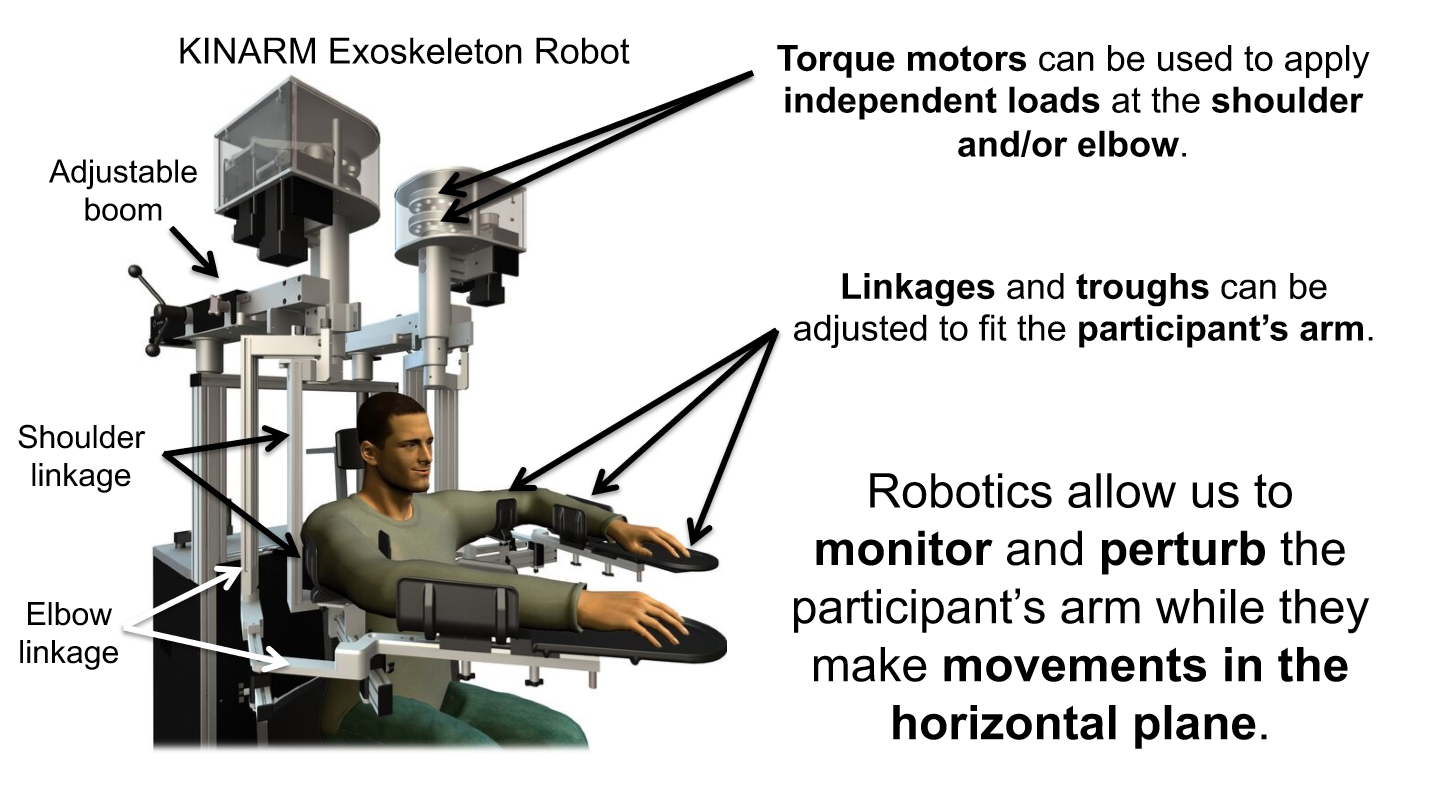
linkages and troughs
What do robotics allow us to do?
to monitor and perturb the participant's arm while they make movements in the horizontal plane
*ONLY reaching in 2D (forward/backwards, left/right)
• Monitor and record arm movements
• Quantify how the nervous system responds to unexpected perturbations
• Quantify sensory and motor deficits in clinical populations
How do robotics monitor and record arm movements? (draw)
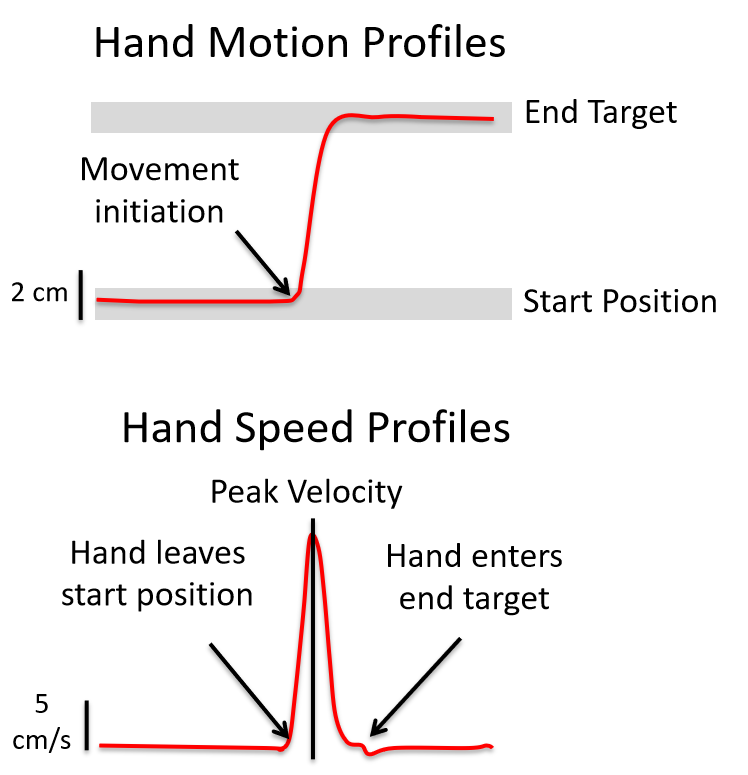
Hand motion profiles and hand speed profiles
*record arm motion while participants perform sensory and motor tasks with their arm
What happens if someone bumps your arm while you are reaching to a door knob vs. a push bar?
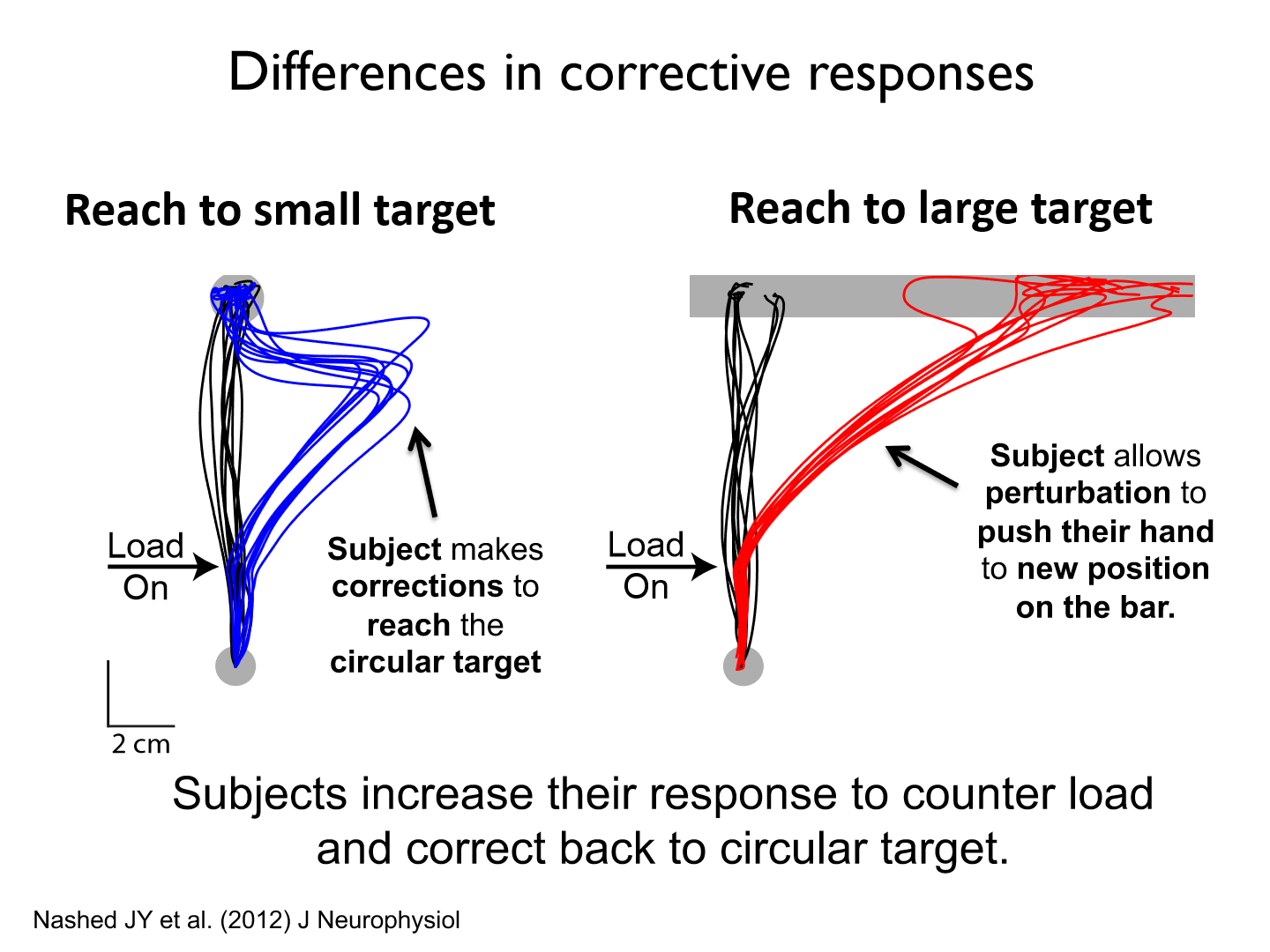
- Reaching to the door knob is much more precise as it is a small target
- The push bar is a much larger target therefore, when it is perturbed participants won't go to the middle of the bar, they will simple go somewhere along the length
*Subjects increase their response to counter load and correct back to circular target
Task description for how target shape influences corrective response
• Subjects instructed to reach the spatial goal.
• no perturbations (loads) applied on most trials.
• perturbations on 20% of trials
• visual-feedback removed at perturbation onset (sensory feedback comes from muscles).
How do we quantify sensory and motor deficits in stroke patients?
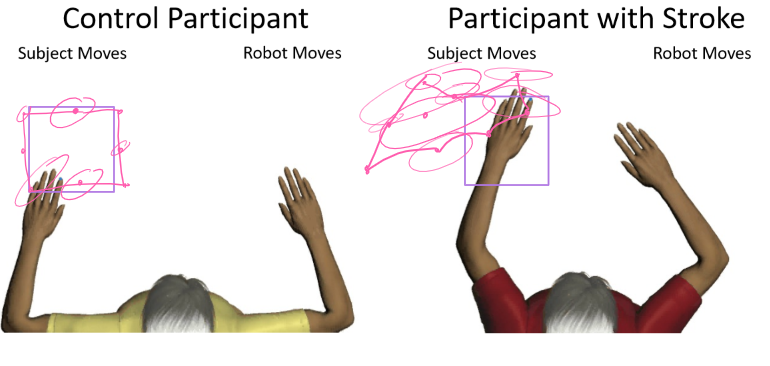
We assess the motor cortex and cerebellum by using position sense (no vision)
*match position that the robot moves their arm to
KINARM Endpoint robot difference
Only controls endpoint/hands
3D Robotic Exoskeletons

devices being used to assist in movement rehabilitation
Pros of robotics
1. Easy to use and non-invasive.
2. Useful for quantifying and perturbing body motion.
3. Easy to integrate with other tools such as EMG.
Cons of robotics
1. Expensive
2. Can require long setup times. (have to calibrate based on different people)
3. Can't replicate many features of how humans move freely in space (unnatural?)
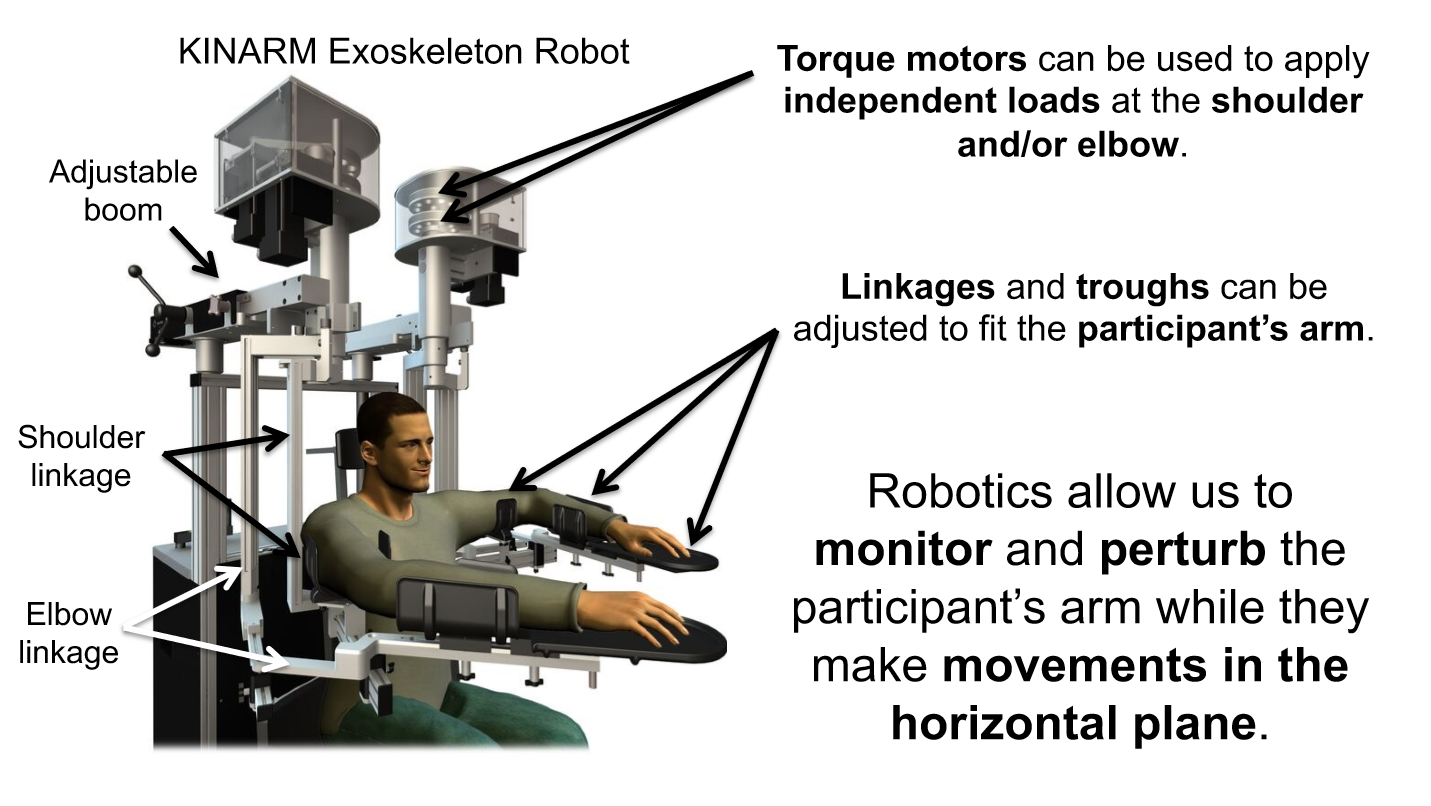
Microneurography
an invasive technique used to record the activity of peripheral neurons
How does microneurography locate and characterize neurons?
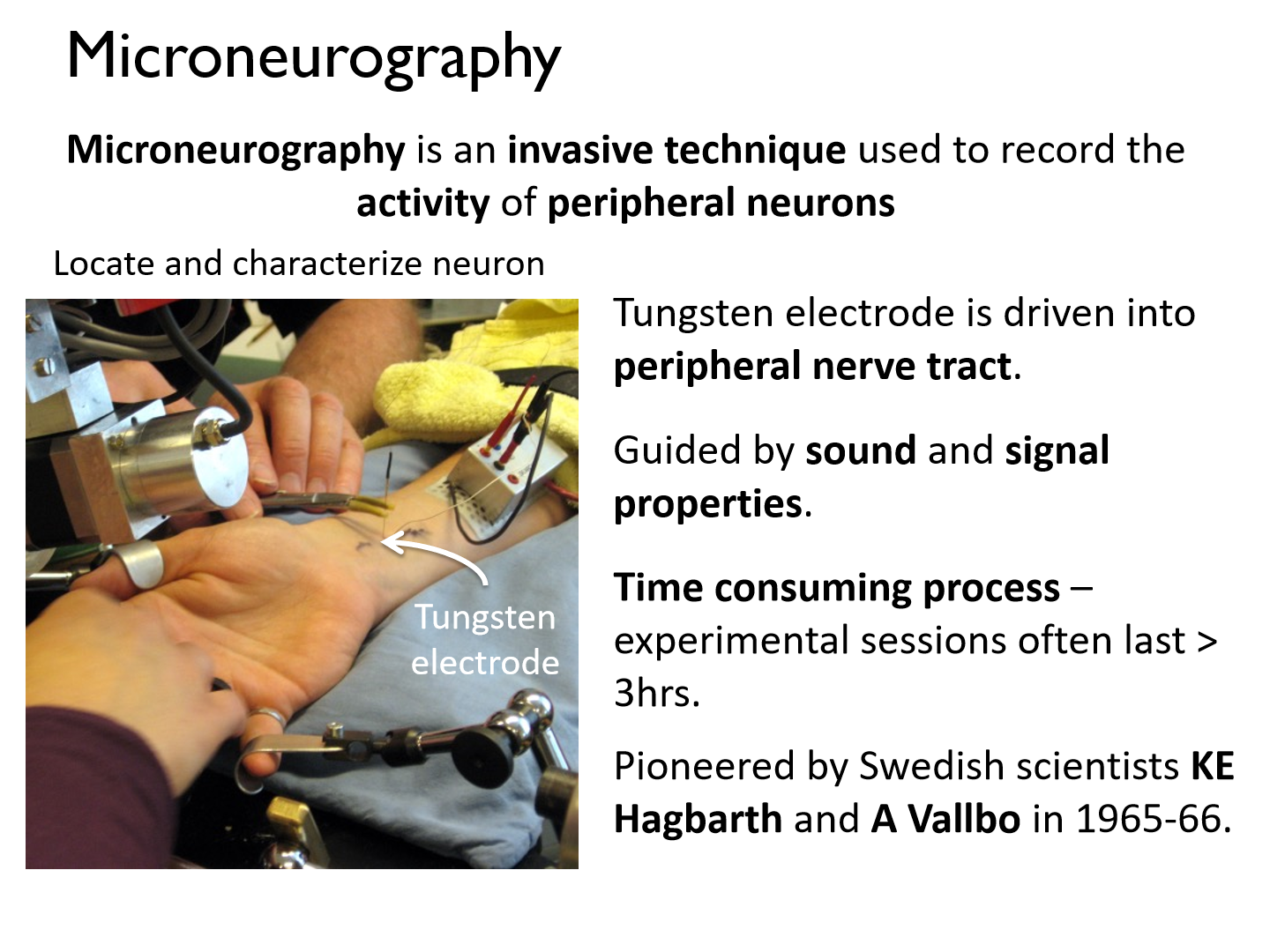
- Tungsten electrode is driven into peripheral nerve tract. (single cell recordings)
- Guided by sound and signal properties.
- Time consuming process – experimental sessions often last > 3hrs.
- Pioneered by Swedish scientists KE Hagbarth and A Vallbo in 1965-66.
Nerve fibre
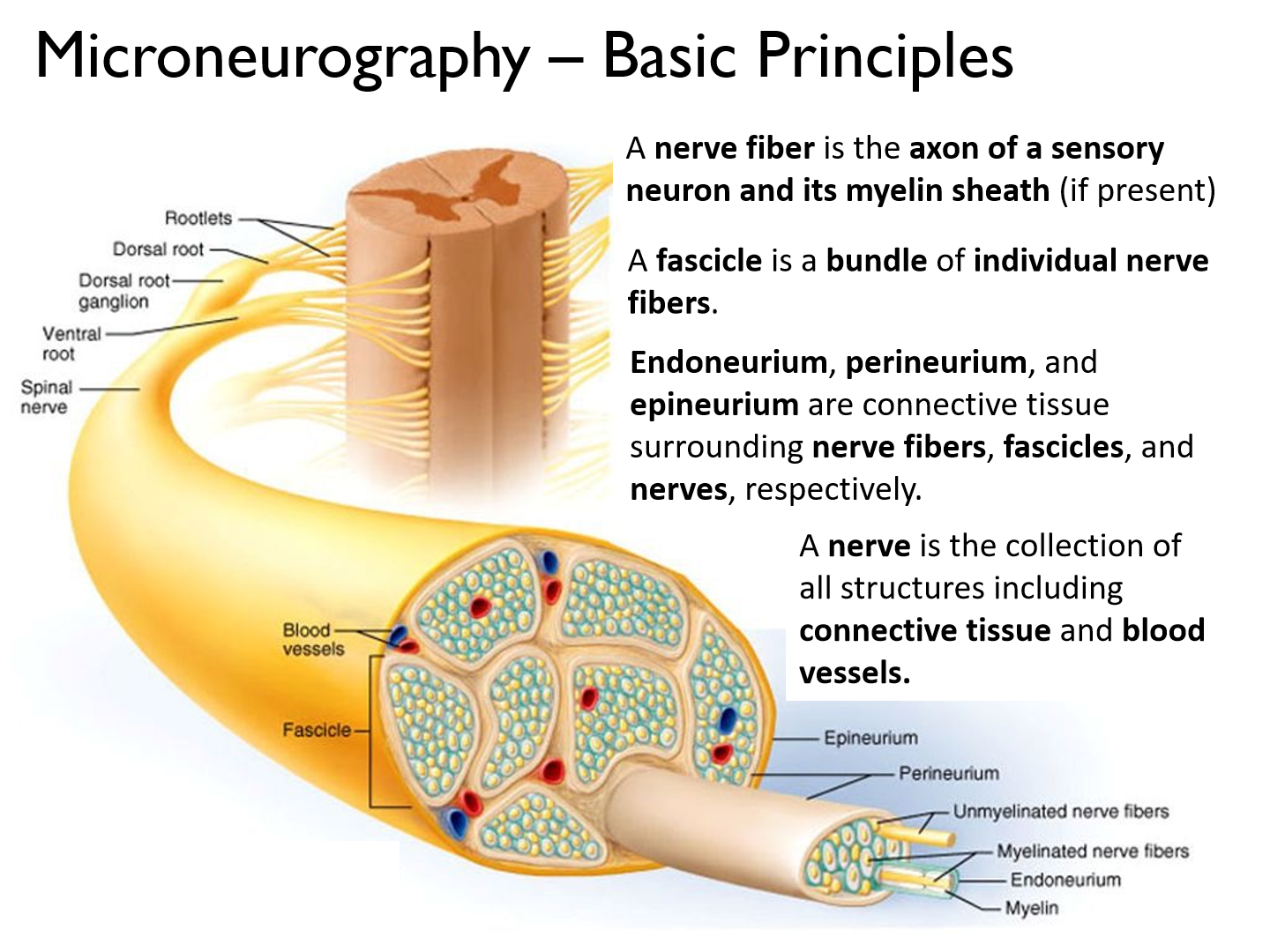
the axon of a sensory neuron and its myelin sheath (if present)
Fascicle
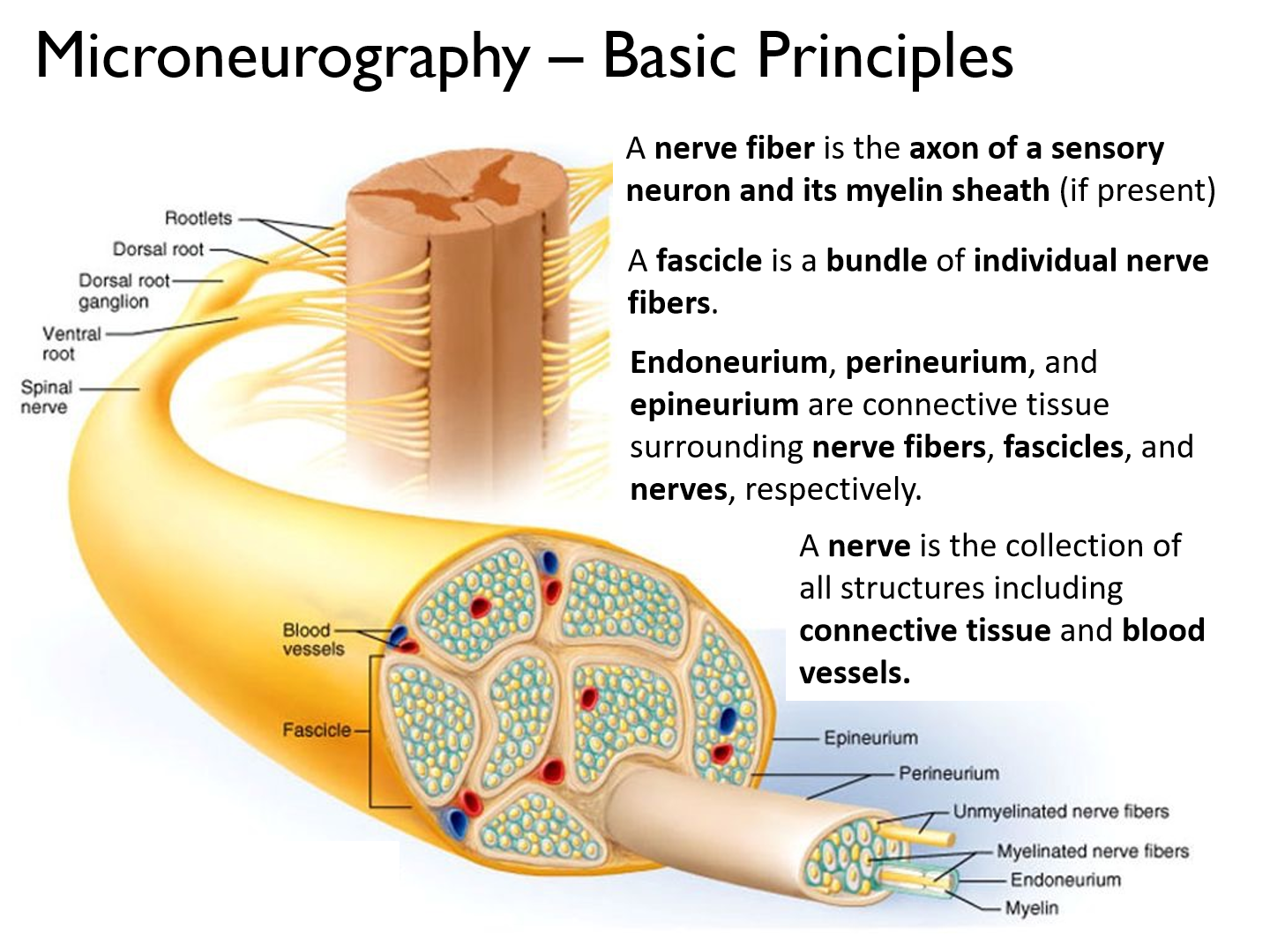
a bundle of individual nerve fibers
Endoneurium, perineurium, and epineurium
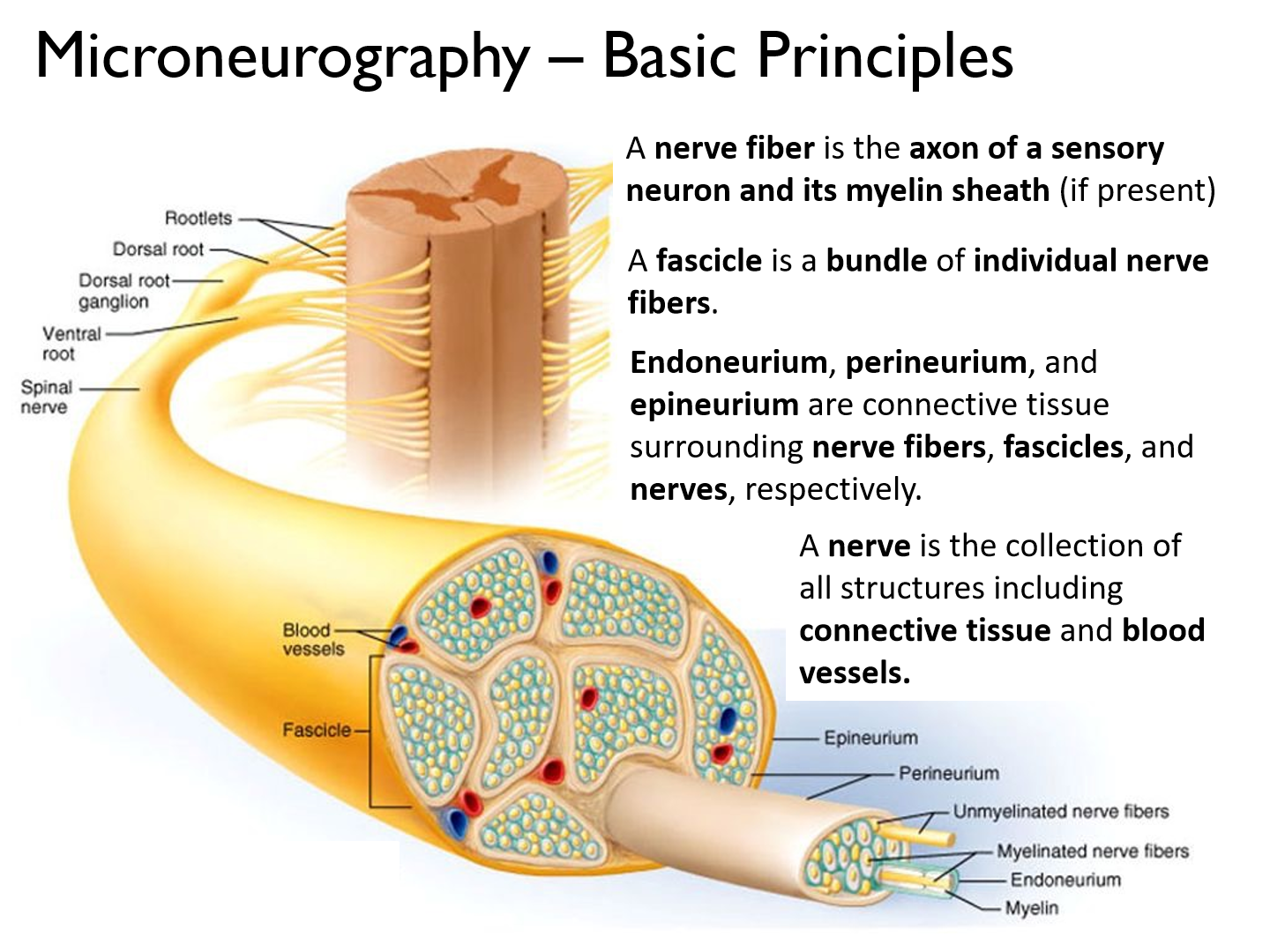
connective tissue surrounding nerve fibers, fascicles, and nerves, respectively.
Nerve
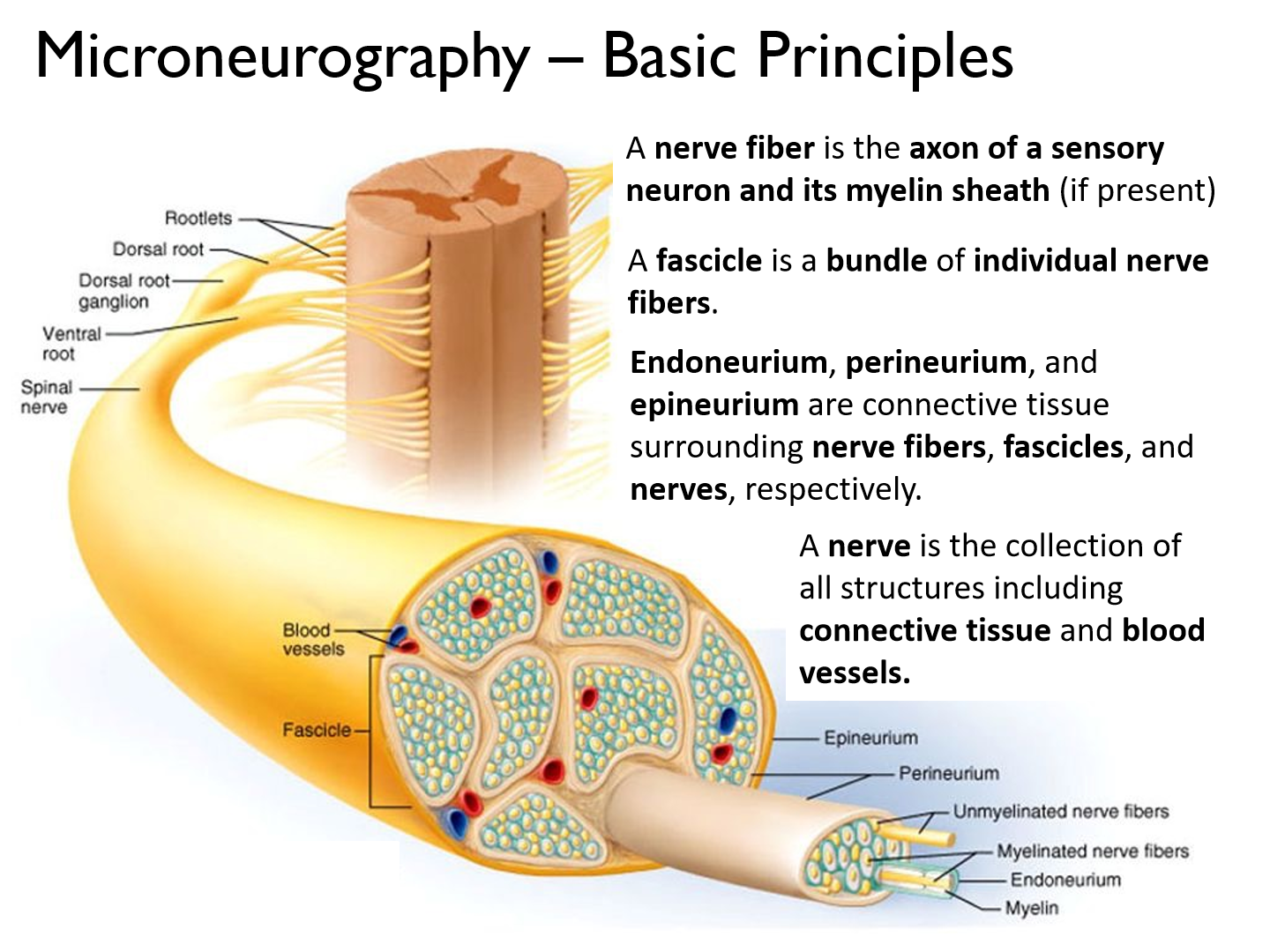
is the collection of all structures including connective tissue and blood vessels.
Microneurography electrode insert
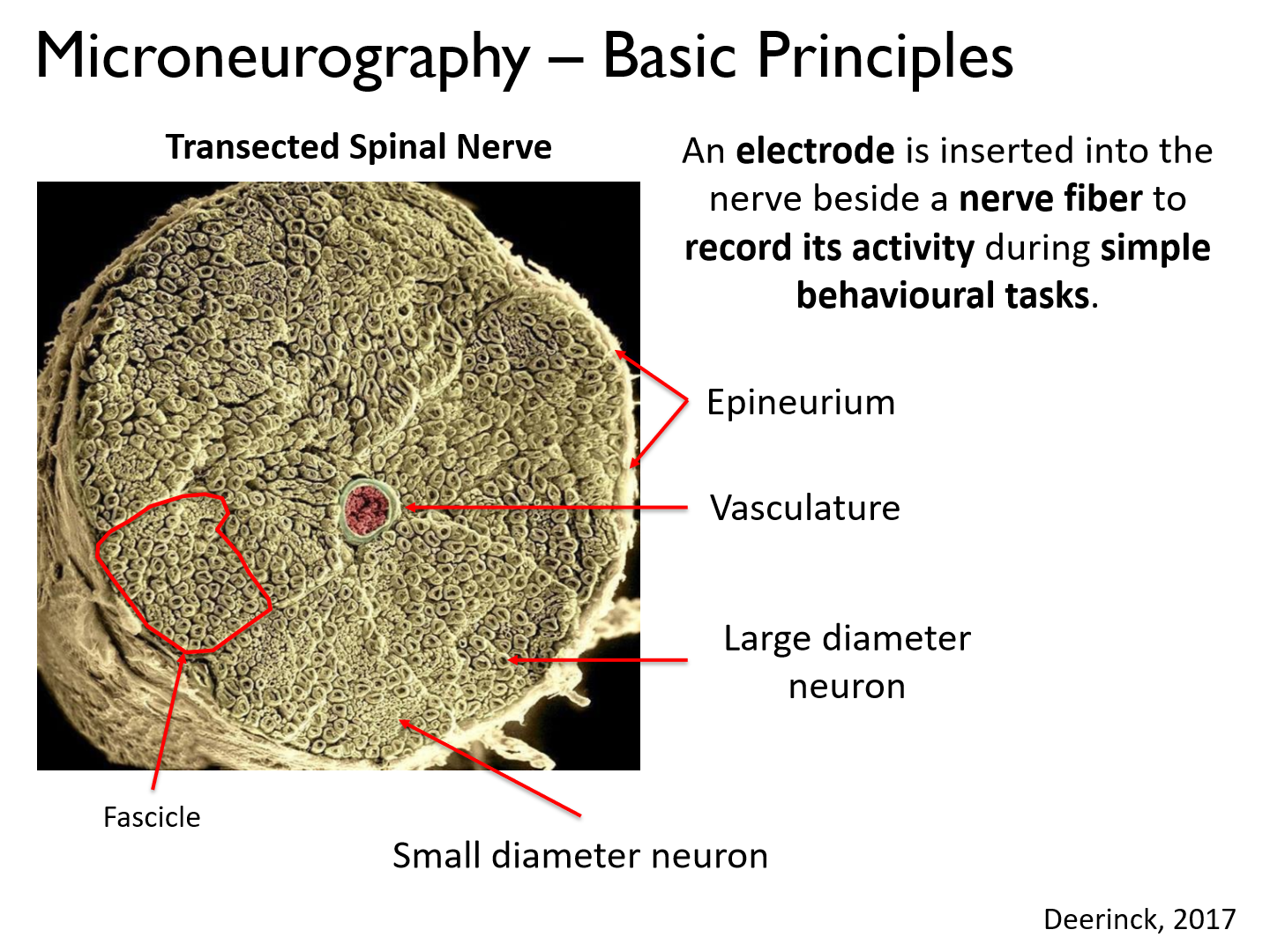
An electrode is inserted into the nerve beside a nerve fiber to record its activity during simple behavioural tasks
Difference between large and small diameter neurons.
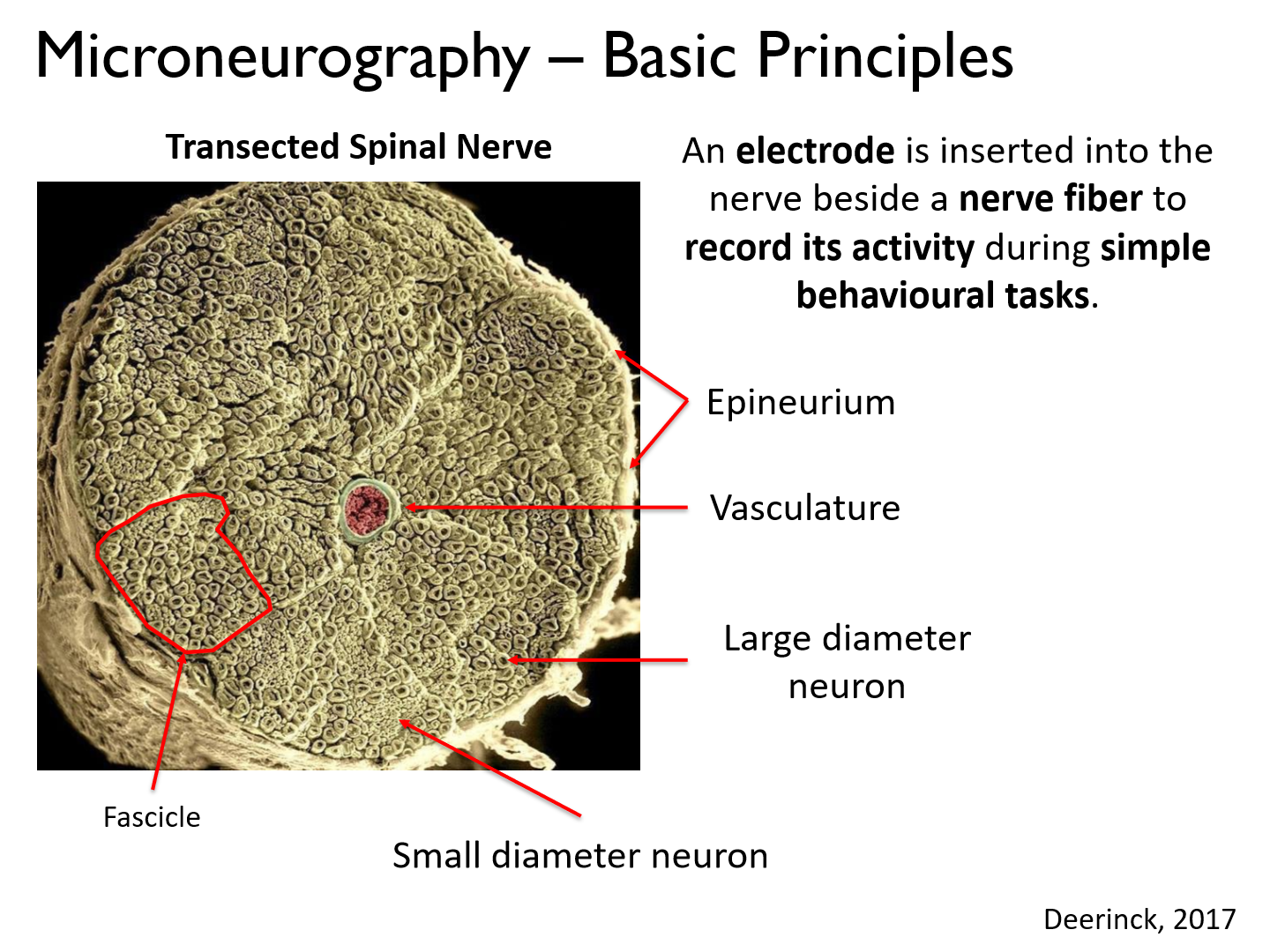
Large diameter:
- large group of muscles controlled
- higher recruitment group (more F produced)
- less precise muscle control
- fast twitch
Small diameter:
- smaller group of muscles controlled
- smaller recruitment group (less F produced)
- more fine movement
- slow twitch
Microneurography recording electrode
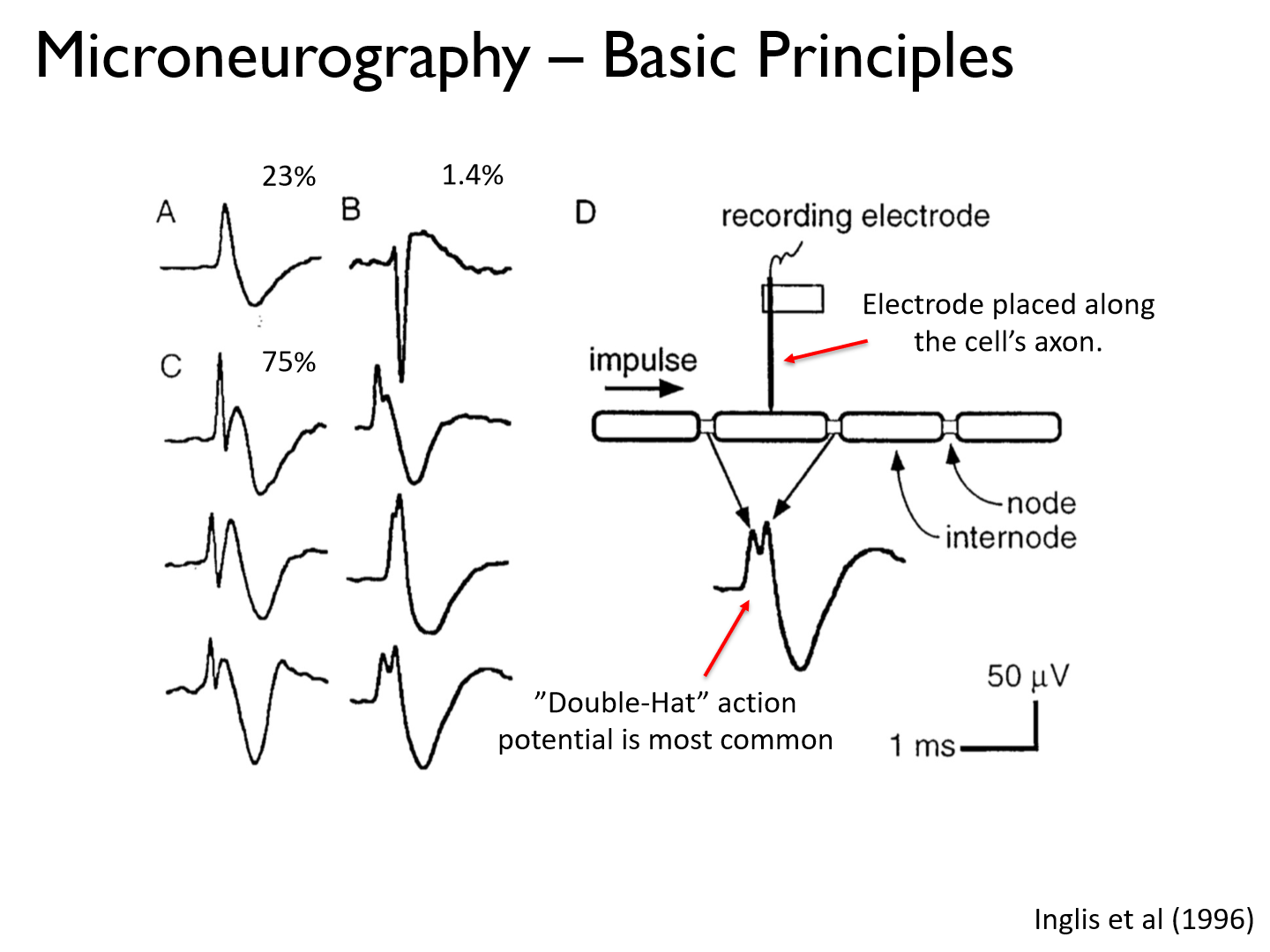
- probably won't hit a node because they are so small
- produce a "double-hat" AP because you are reading the peaks @ both nodes of Ranvier (signals are sent in both directions)
What are the 4 typical steps to a microneurography experiement?
1. Search (find the nerve)
2. Characterize (motor/sensory, what type of receptor, where on skin/muscle)
3. Position
4. Stimulate
Step 1 of microneurography (search for peripheral nerve fiber)

Tungsten electrode is driven into peripheral sensory neuron.
Guided by sound and signal properties.
What are reference/ground electrodes for?
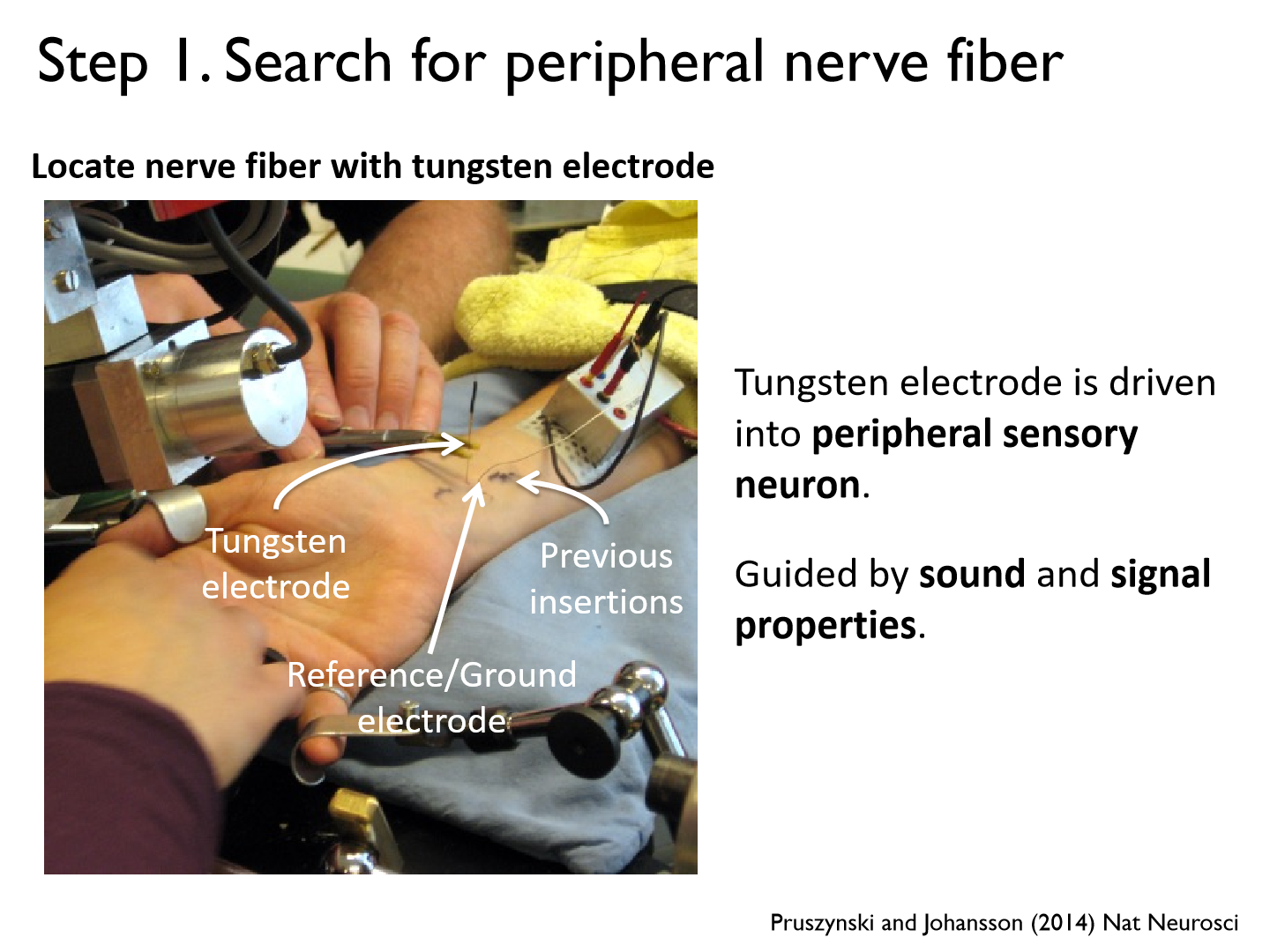
There is a lot of electrical stimuli in the human body, so it takes the average to filter out noise
Step 2 of microneurography (map out the neuron's receptive field)
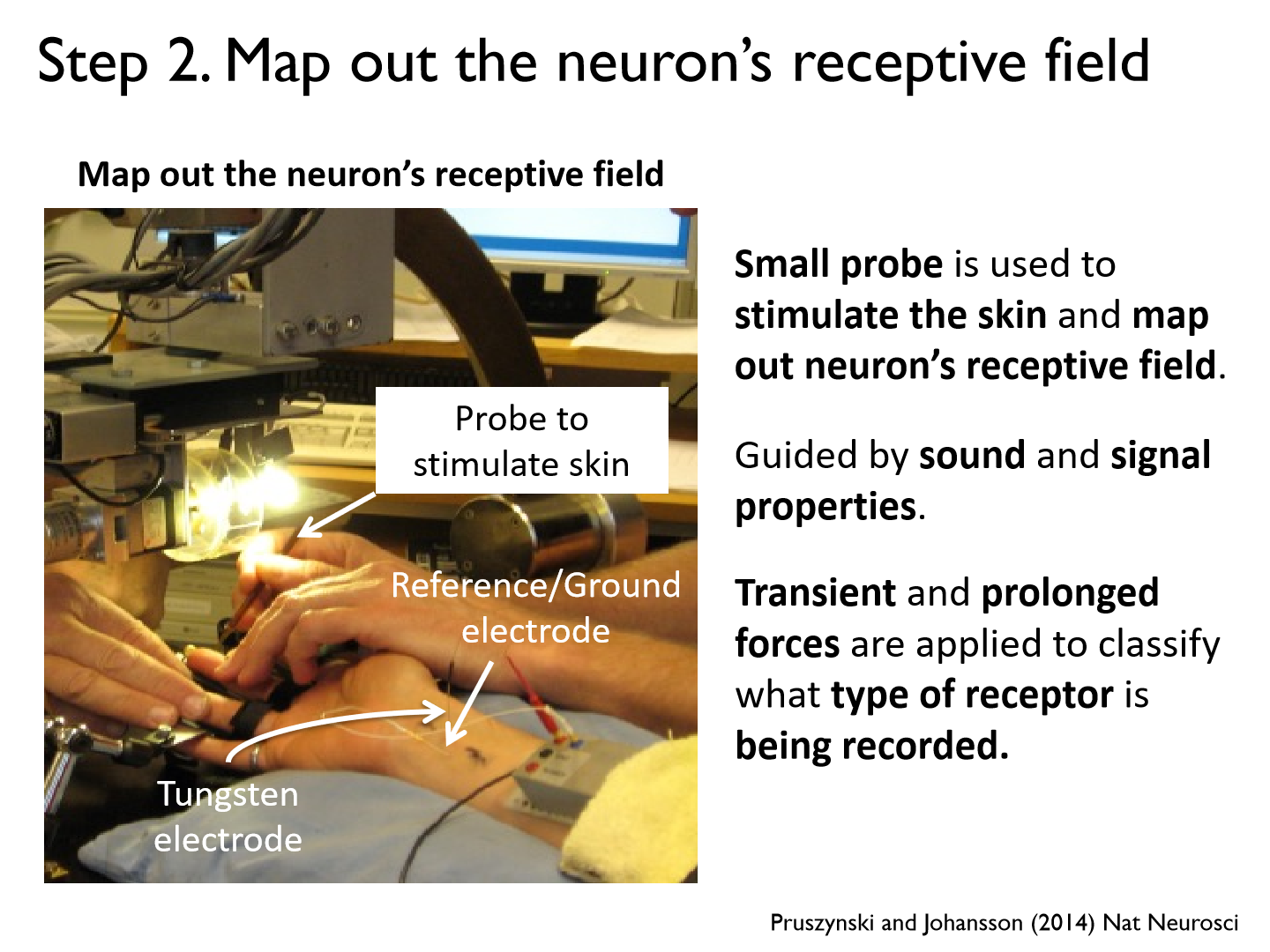
- Small probe is used to stimulate the skin and map out neuron’s receptive field.
- Guided by sound and signal properties.
- Transient and prolonged forces are applied to classify what type of receptor is being recorded.
Electrode is in the nerve and there is a neuron ‘online’. How can we tell what type of neuron it is?
We press around with different stimulus
e.g. skin stroke, deep pressure, heat, etc.
**We want an afferent neuron
Step 3 of microneurography (position and calibrate stimulator rig)
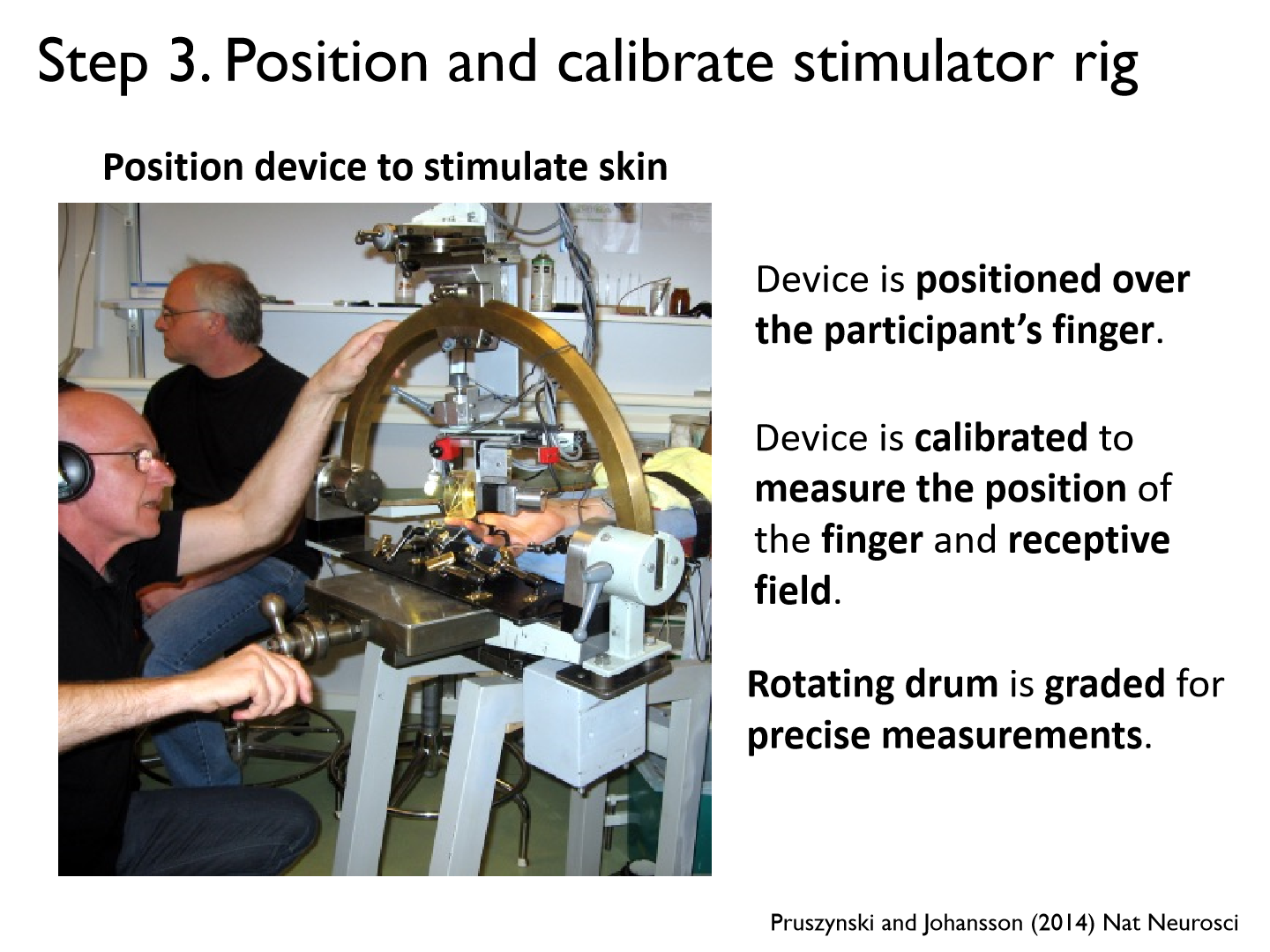
Position device to stimulate skin
- Device is positioned over the participant’s finger.
- Device is calibrated to measure the position of the finger and receptive field.
- Rotating drum is graded for precise measurements.
Step 4 of microneurography (record neuron's response to sensory stimuli)
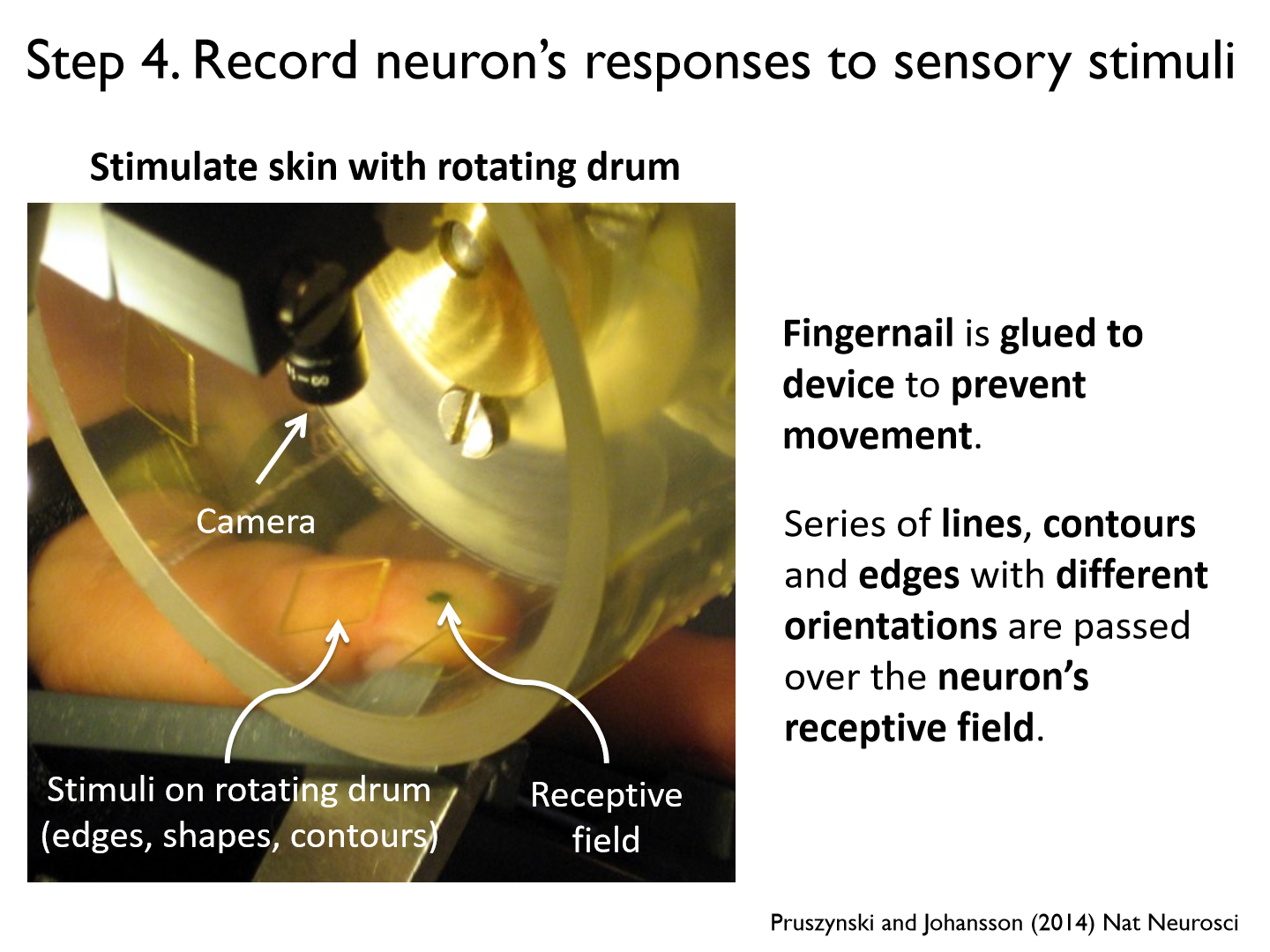
- Stimulate skin with rotating drum
- Fingernail is glued to device to prevent movement.
- Series of lines, contours and edges with different orientations are passed over the neuron’s receptive field.
What is the sound we hear from microneurography?
the action potentials recorded from the peripheral sensory neuron
Microneurography pros
1. Recording from peripheral sensory and motor nerves.
2. Useful for understanding sensory feedback arising from periphery.
3. Can be integrated with other tools such as EMG.
Microneurography cons
1. Time consuming.
2. Highly invasive.
3. Restricted to relatively small movements and simple sensory/motor tasks
Electrophysiological
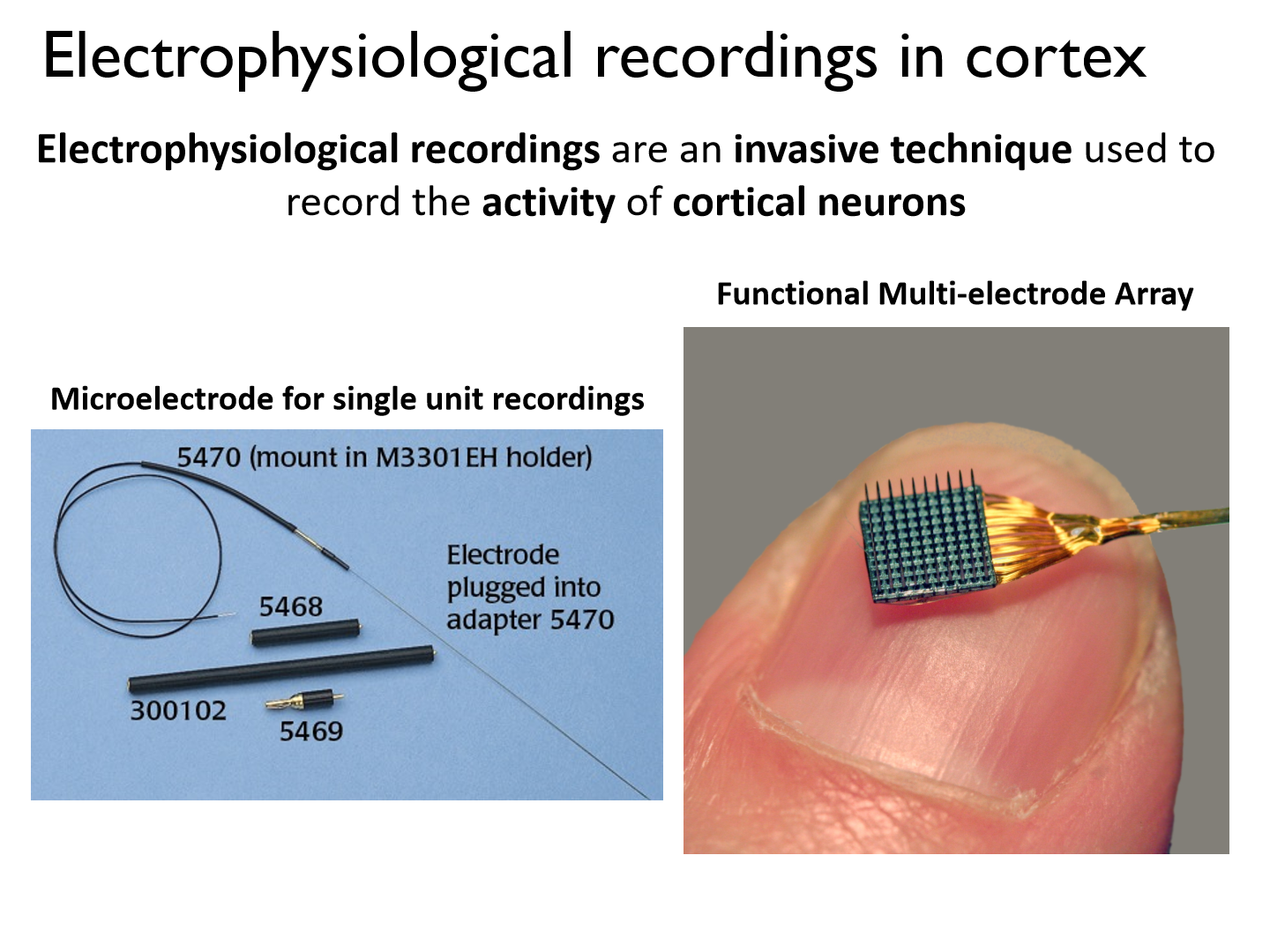
an invasive technique used to record the activity of cortical neurons
Single unit recordings set up
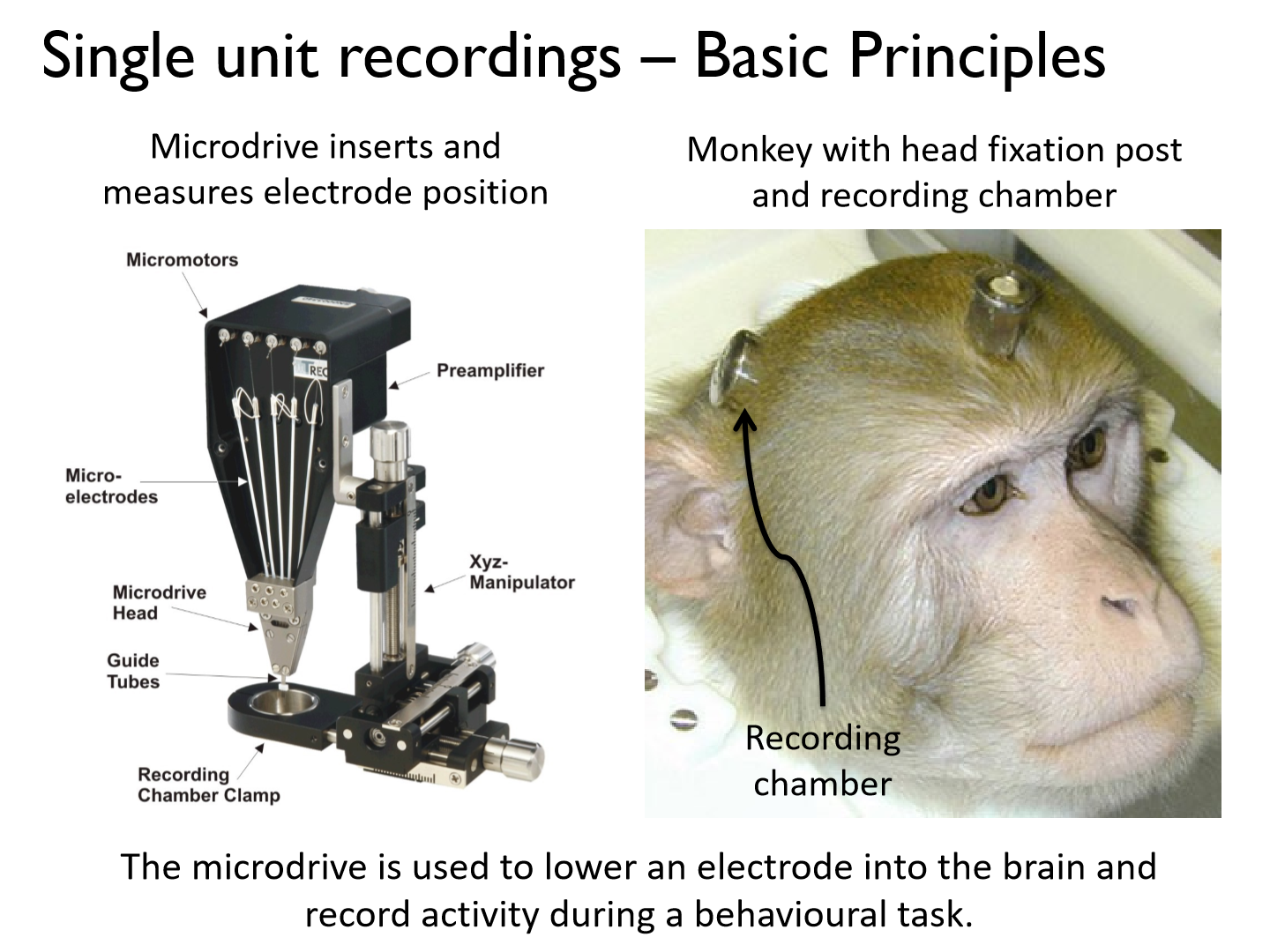
- Microdrive inserts and measures electrode position
- Monkey with head fixation post and recording chamber
- The microdrive is used to lower an electrode into the brain and record activity during a behavioural task.
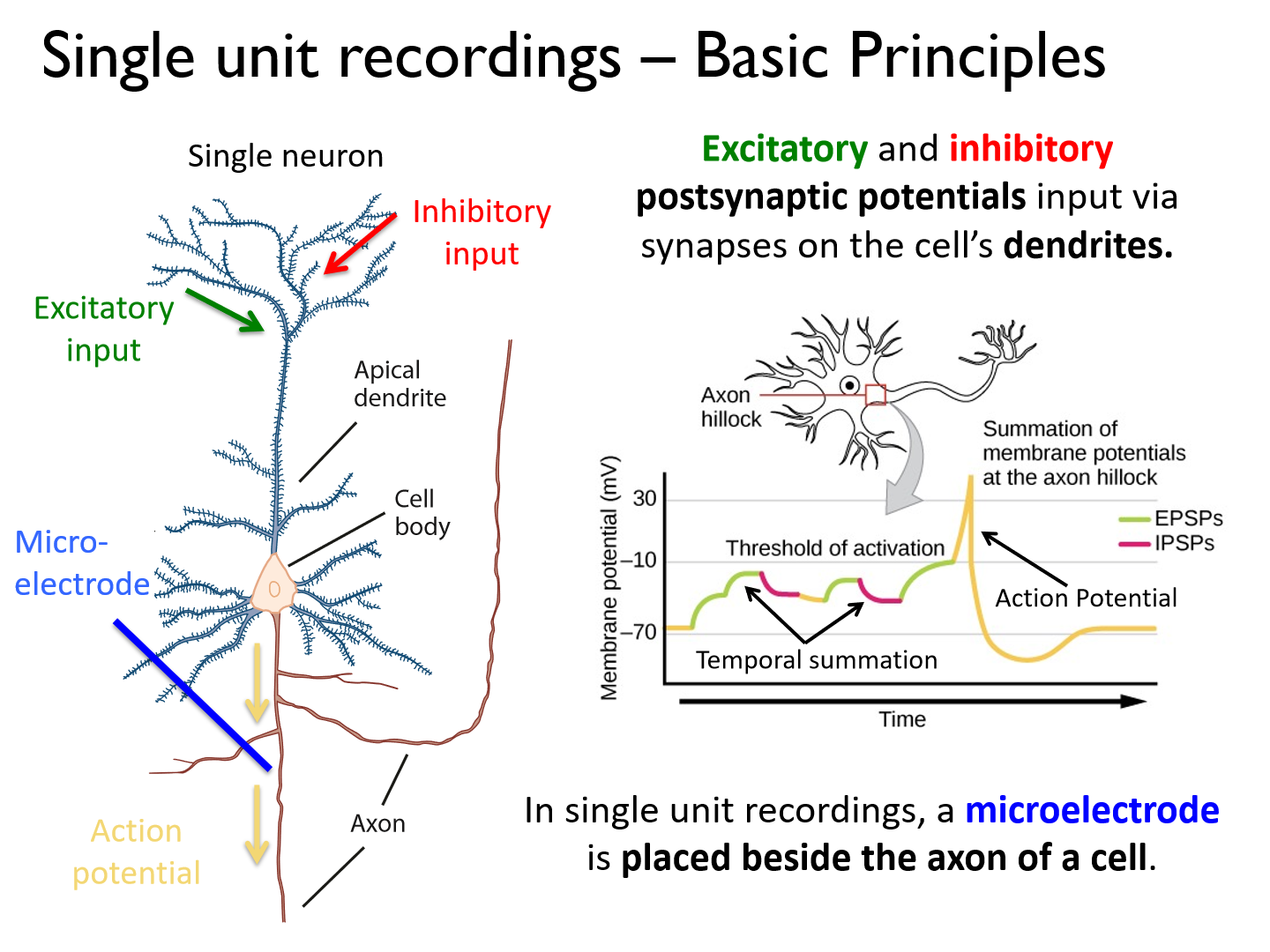
In single unit recordings where is the microelectrode placed?
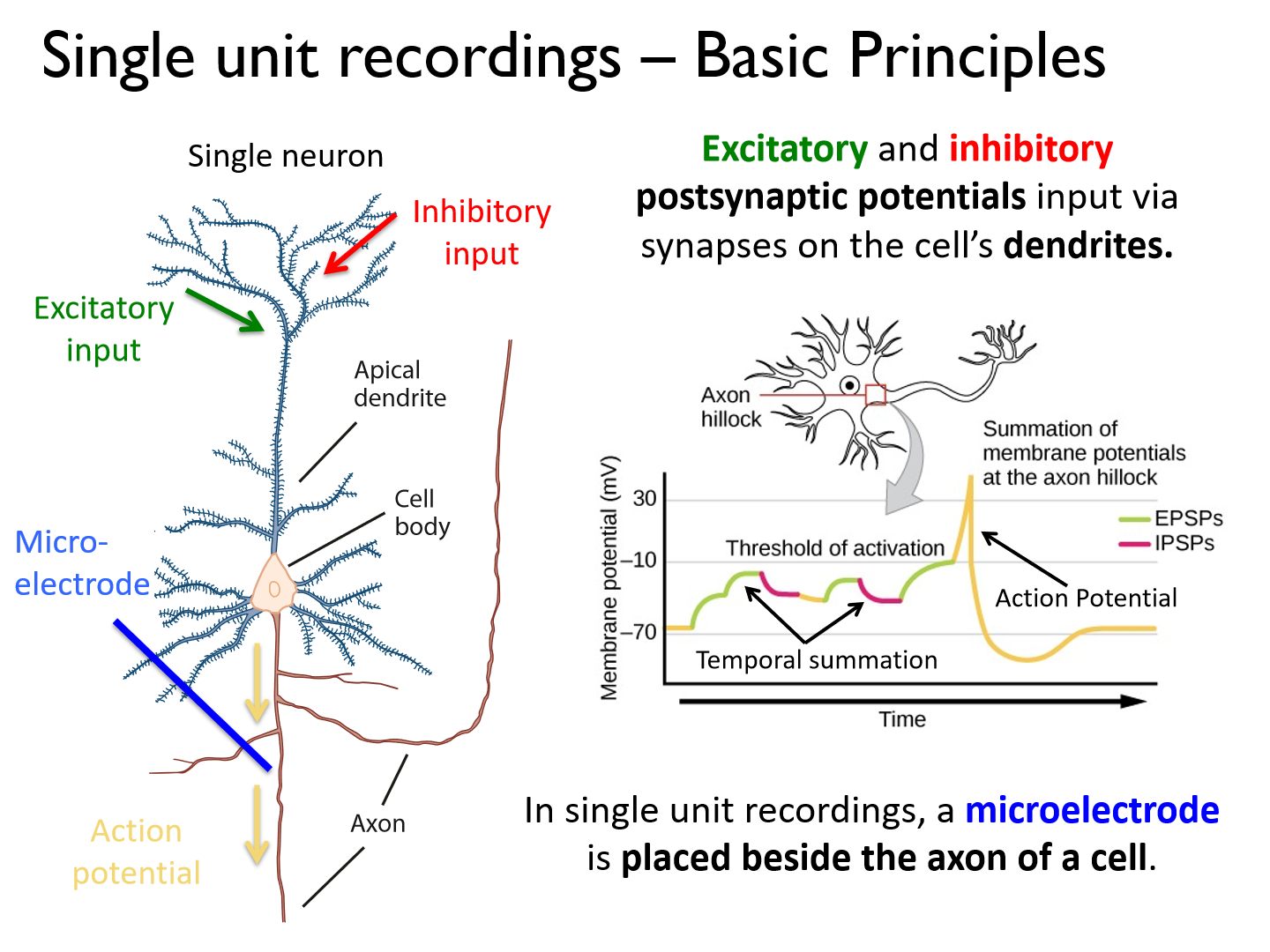
it is placed beside the axon of a cell
*Excitatory and inhibitory postsynaptic potentials input via synapses on the cell's dendrites
In single unit recordings how do we learn about a cell's preference?
The rate at which the cell fires action potentials provides information about the cell’s preference for certain tasks or stimuli.
Single unit recordings to record the membrane potential of individual neurons set up
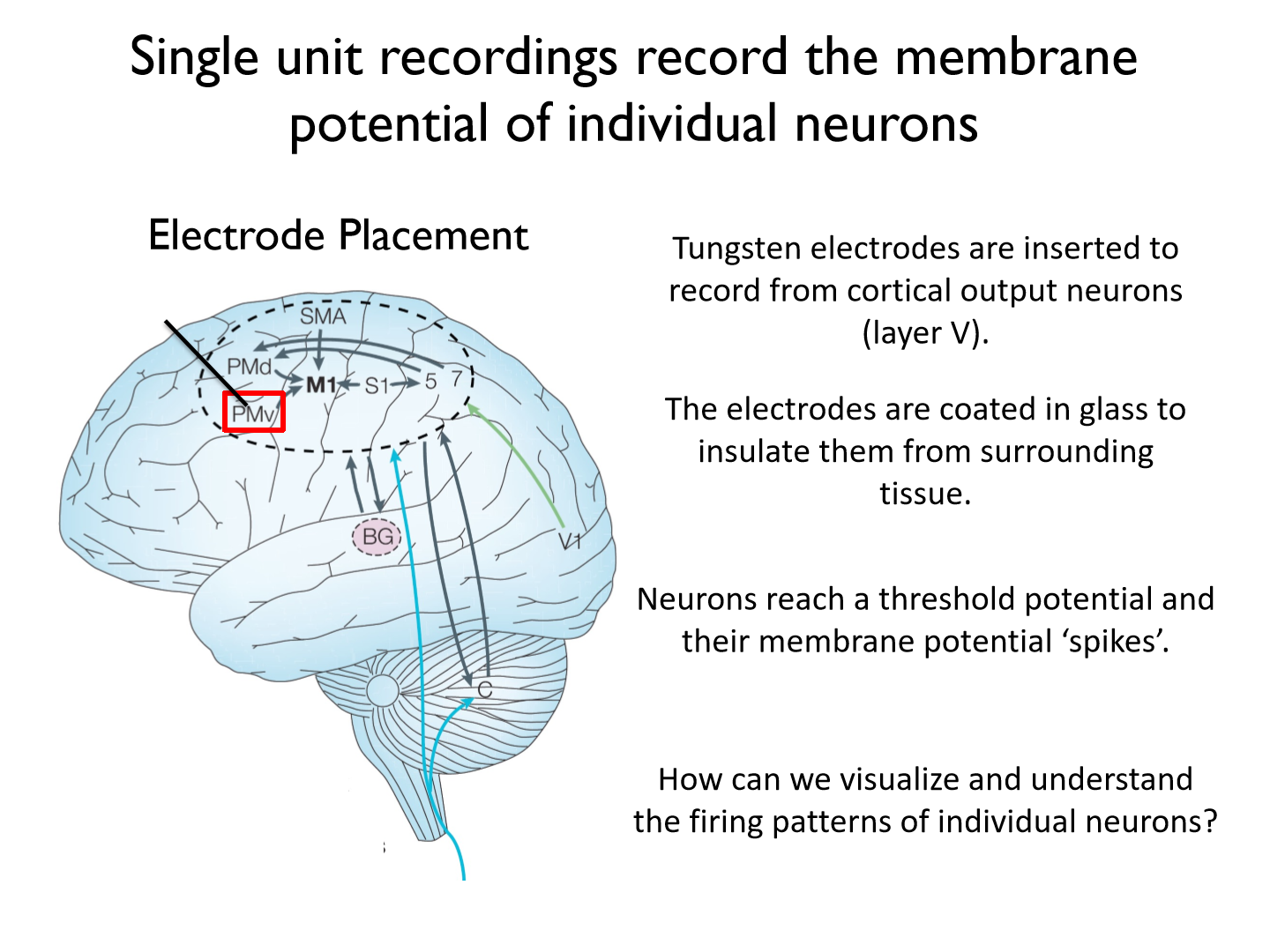
- Tungsten electrodes are inserted to record from cortical output neurons (layer V).
- The electrodes are coated in glass to insulate them from surrounding tissue.
- Neurons reach a threshold potential and their membrane potential ‘spikes’.
How can we visualize and understand the firing patterns of individual neurons?
Raster plots
Raster plots to visualize APs
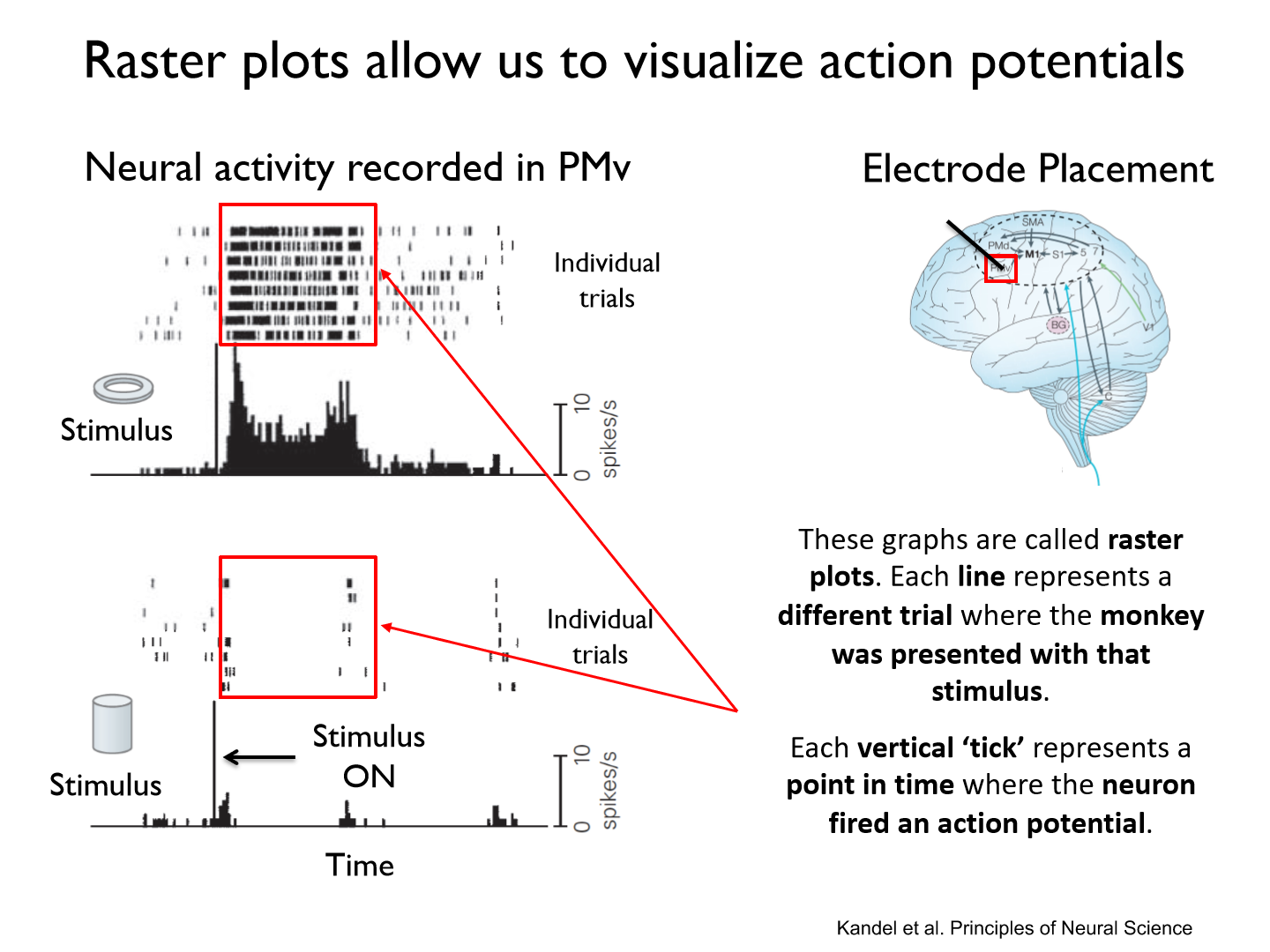
- Each line represents a different trial where the monkey was presented with that stimulus.
- Each vertical ‘tick’ represents a point in time where the neuron fired an action potential.
Poststimulus time histograms (PSTH)
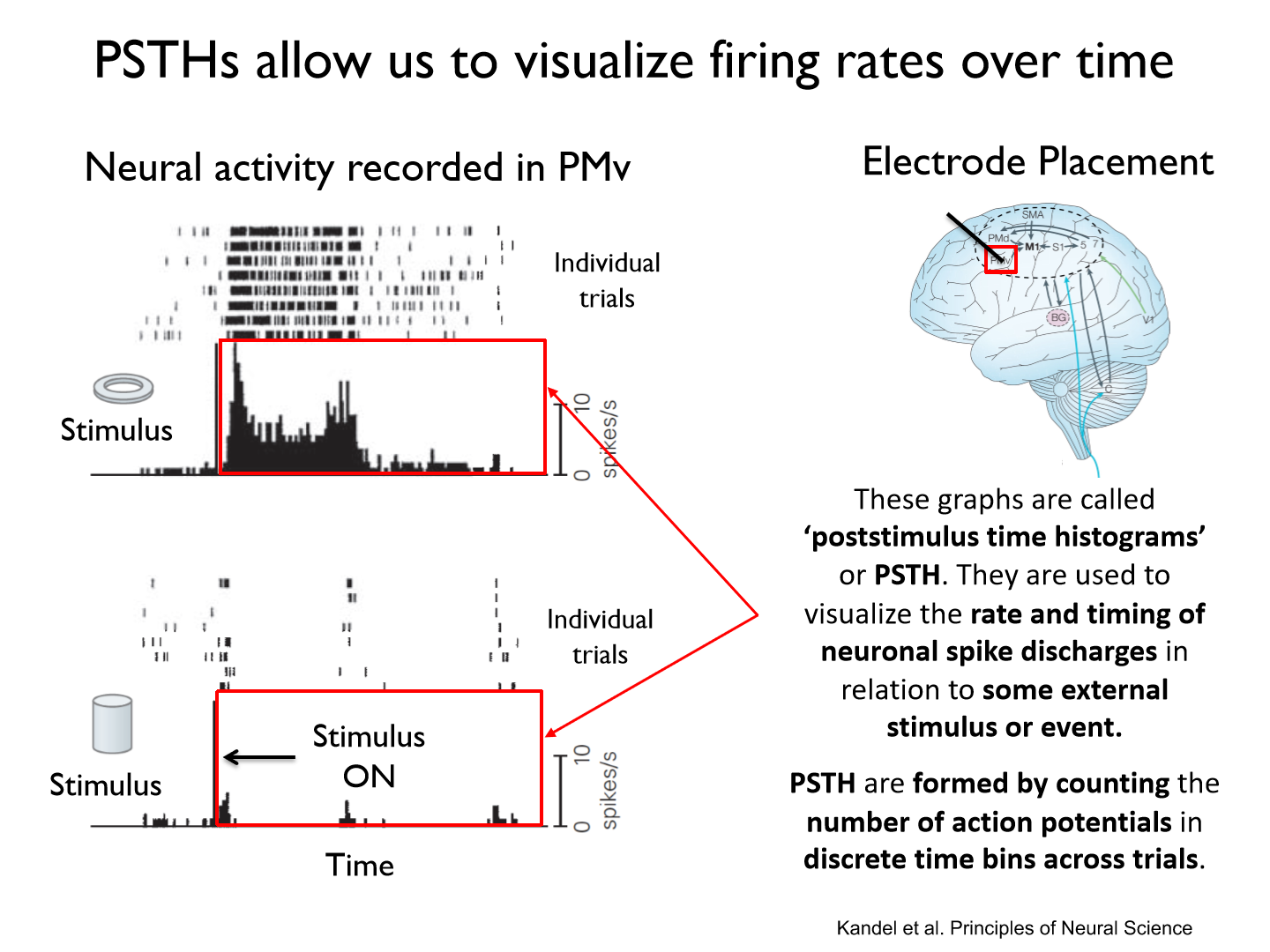
- They are used to visualize the rate and timing of neuronal spike discharges in relation to some external stimulus or event.
- PSTH are formed by counting the number of action potentials in discrete time bins across trials.
Neuron in visual cortex responding to stimuli (bar of light)
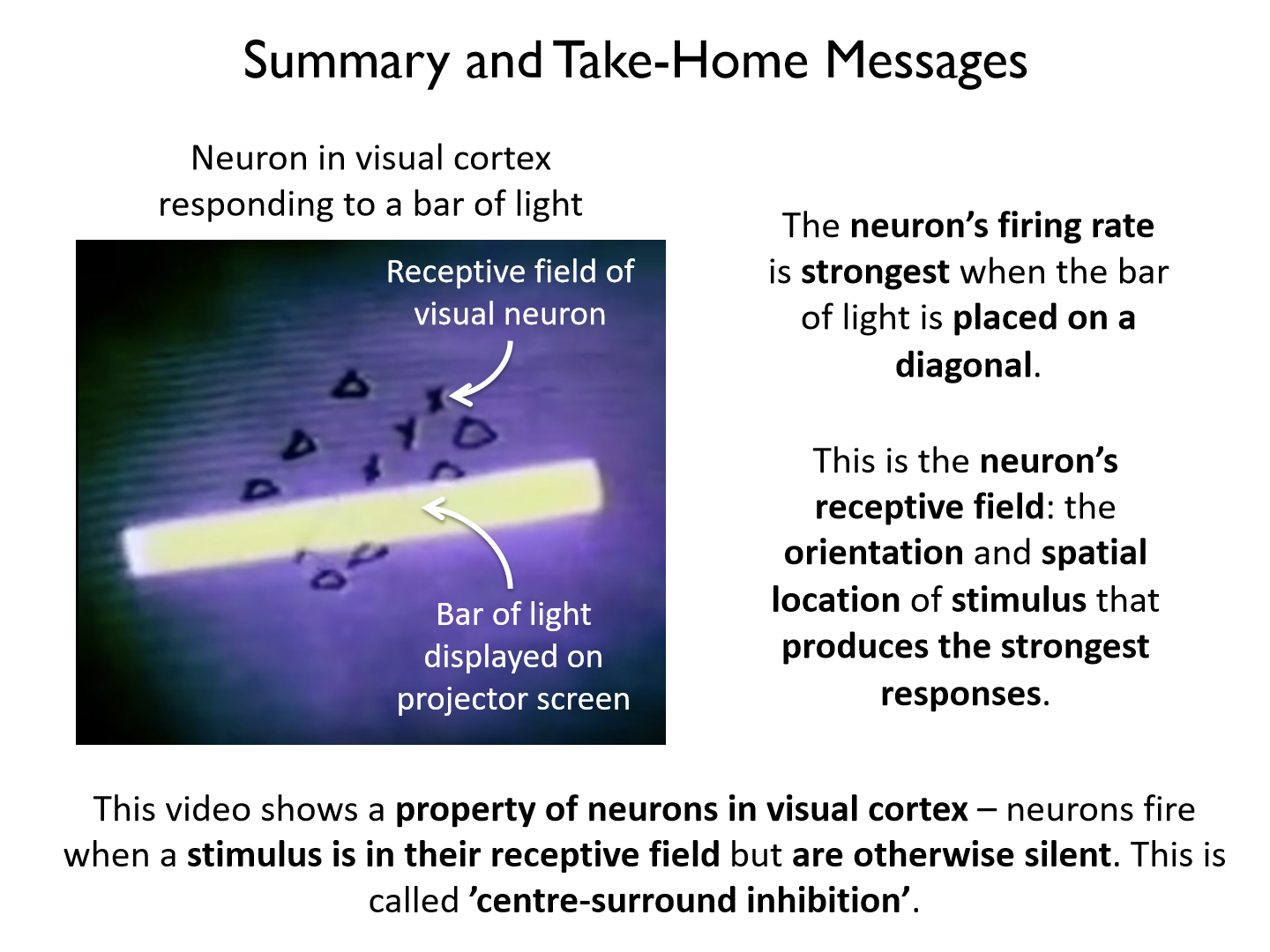
- The neuron’s firing rate is strongest when the bar of light is placed on a diagonal.
- This is the neuron’s receptive field: the orientation and spatial location of stimulus that produces the strongest responses.
Center-surround inhibition
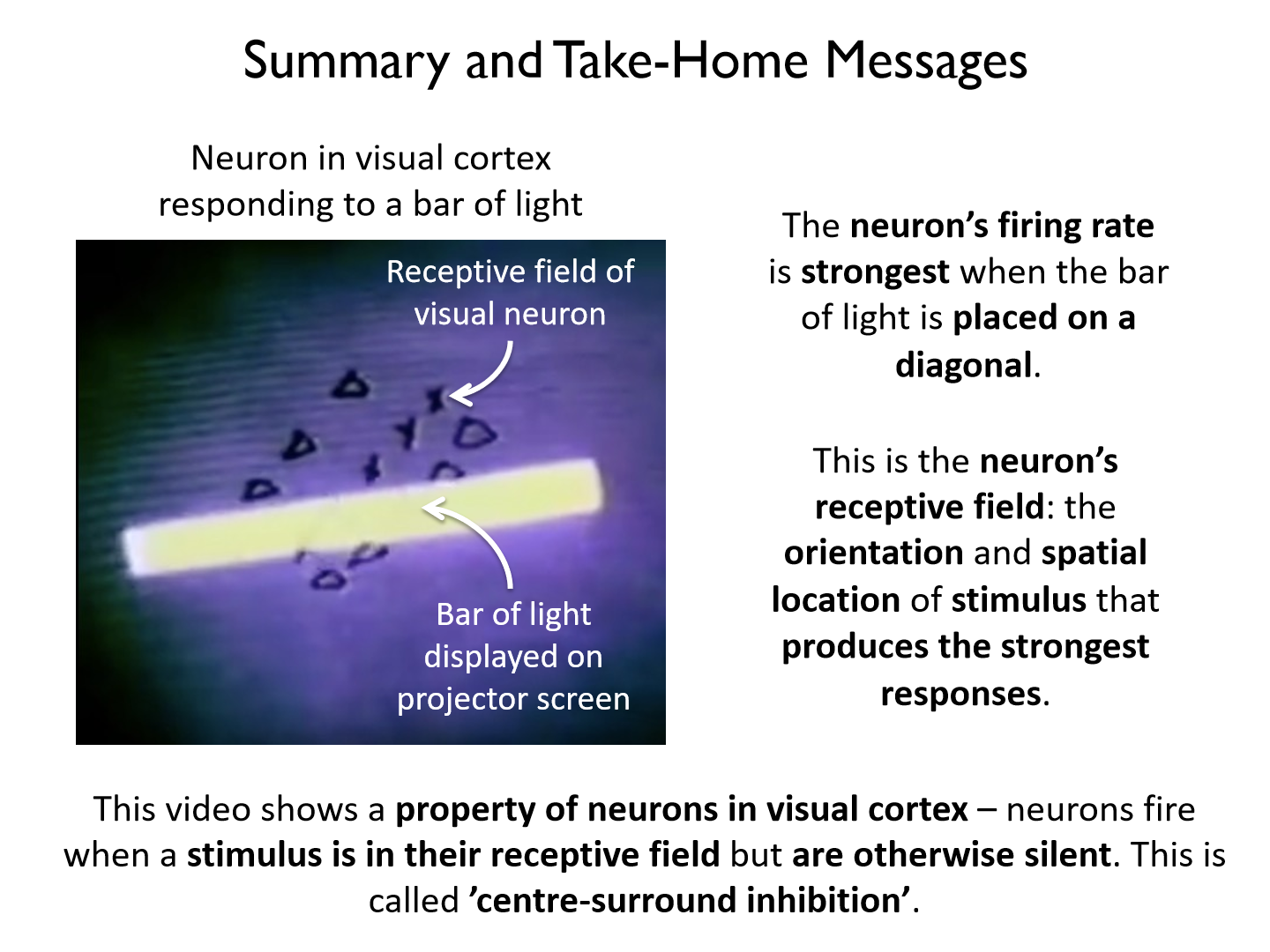
a property of neurons in visual cortex – neurons fire when a stimulus is in their receptive field but are otherwise silent.
Motion Capture
a non-invasive technique used to record body motion during motor tasks
- Cameras are used to record the motion of markers attached to the body.
*infrared camera and retroreflective markers
Basic Principles of Optical-Passive Motion Capture
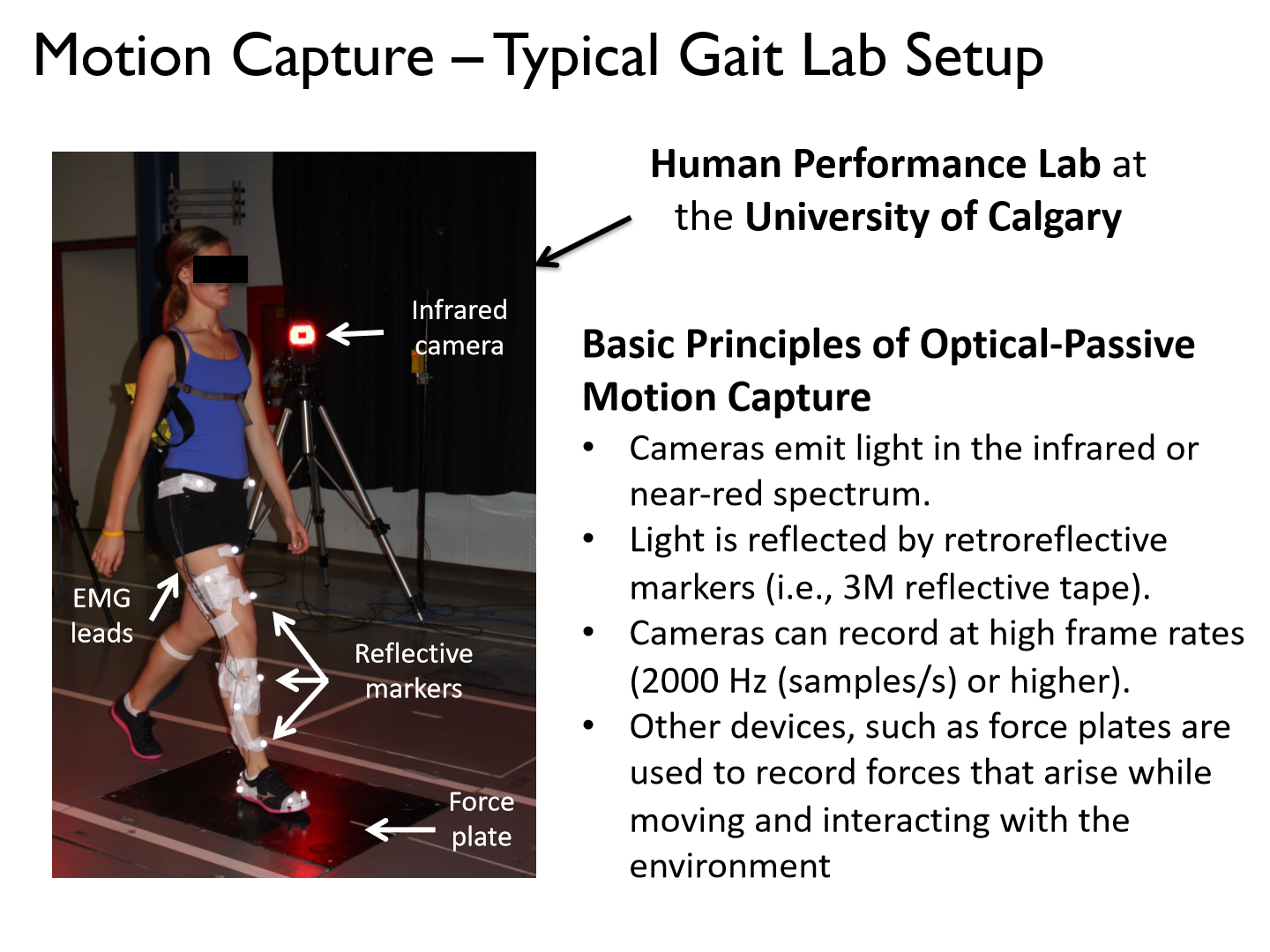
• Cameras emit light in the infrared or near-red spectrum.
• Light is reflected by retroreflective markers (i.e., 3M reflective tape).
• Cameras can record at high frame rates (2000 Hz (samples/s) or higher).
• Other devices, such as force plates are used to record forces that arise while moving and interacting with the environment
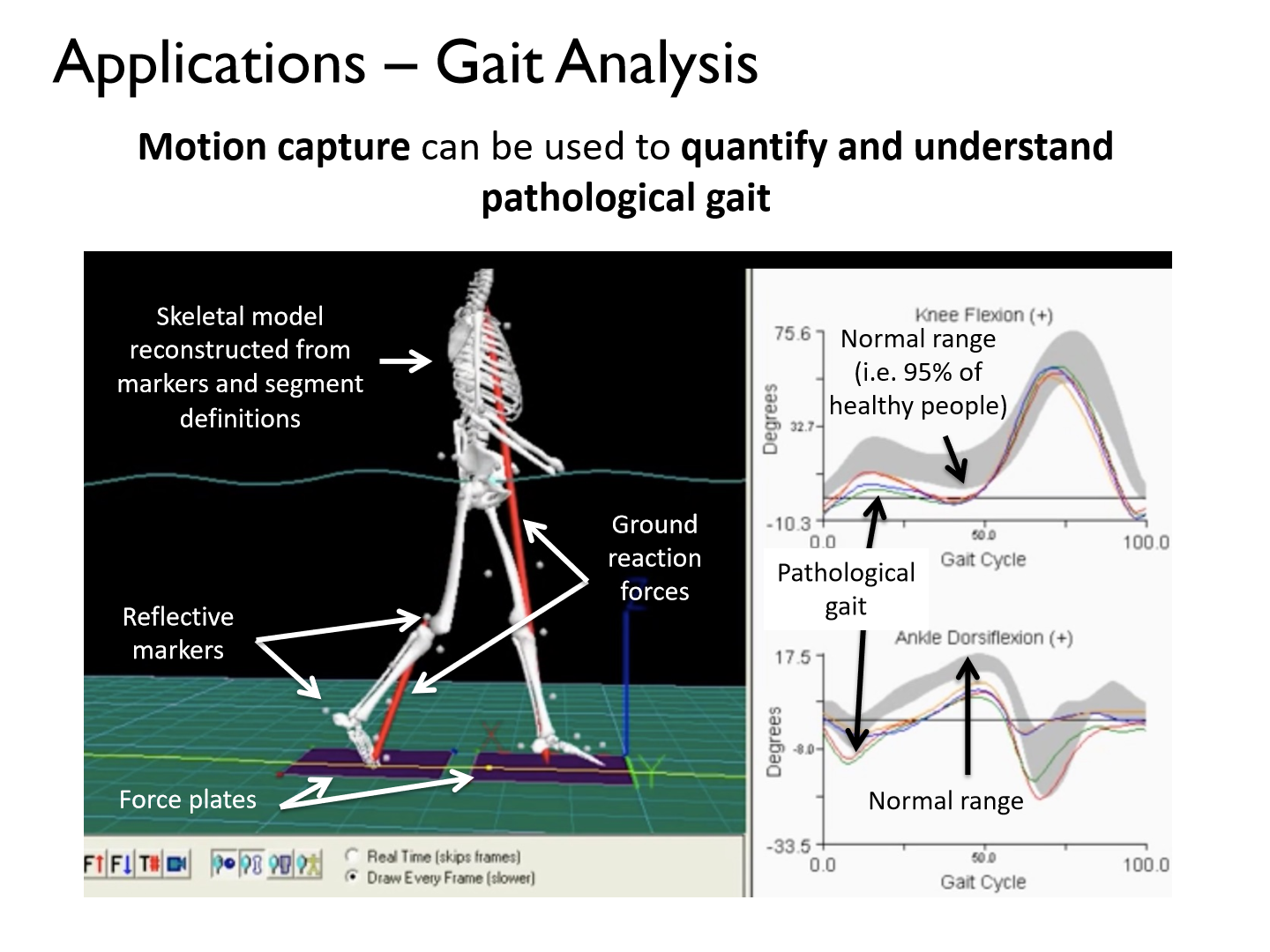
What can we use motion capture for?
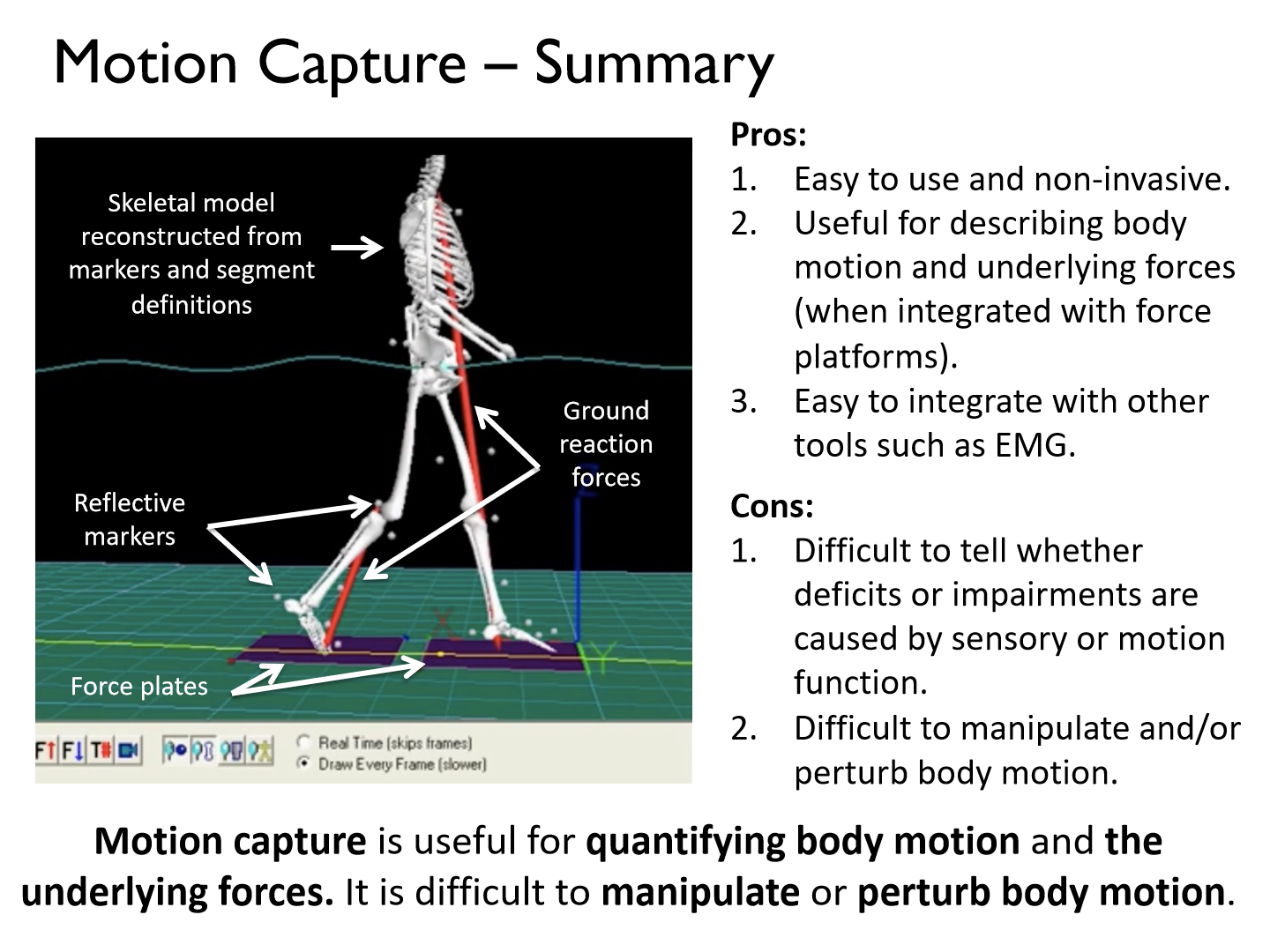
It can be used to quantify and understand pathological gait
- Motion capture is useful for quantifying body motion and the underlying forces. It is difficult to manipulate or perturb body motion.
Pros of motion capture
1. Easy to use and non-invasive.
2. Useful for describing body motion and underlying forces (when integrated with force platforms).
3. Easy to integrate with other tools such as EMG
Cons of motion capture
1. Difficult to tell whether deficits or impairments are caused by sensory or motion function.
2. Difficult to manipulate and/or perturb body motion.
Gait Analysis
What connective tissue surrounds muscle fibers, muscle fascicles, and muscle?
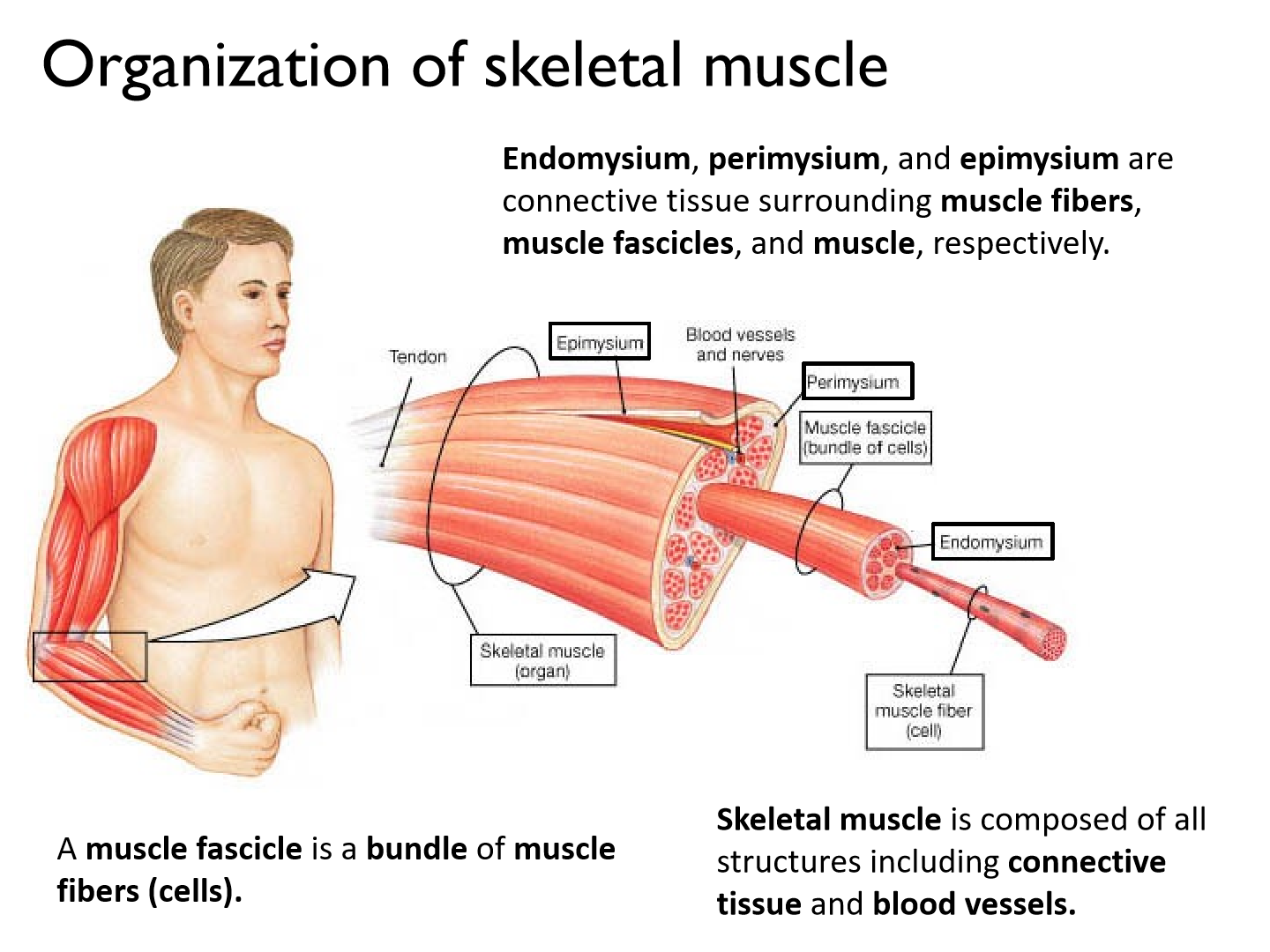
Endomysium, perimysium, and epimysium
Electromyography (EMG) (2 types)
a technique used to record the activity of skeletal muscle during motor tasks
1. surface: lots of crosstalk, superficial muscles, need to be larger muscles
2. indwelling: deep muscles, specific smaller muscles
Surface EMG
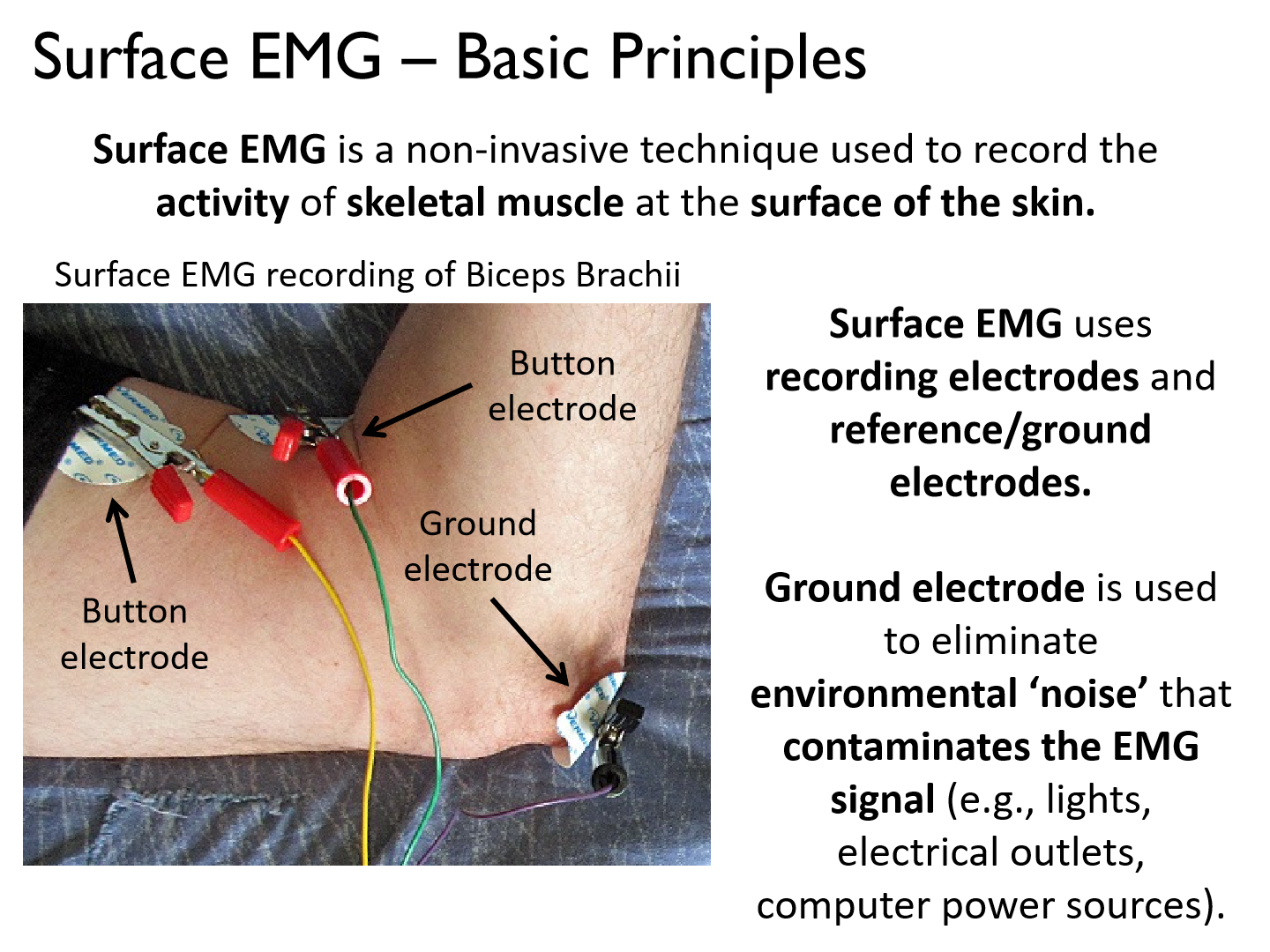
a non-invasive technique used to record the activity of skeletal muscle at the surface of the skin.
*Surface EMG uses recording electrodes and reference/ground electrodes.
*Ground electrode is used to eliminate environmental ‘noise’ that contaminates the EMG signal (e.g., lights, electrical outlets, computer power sources).
Basic principles of EMG
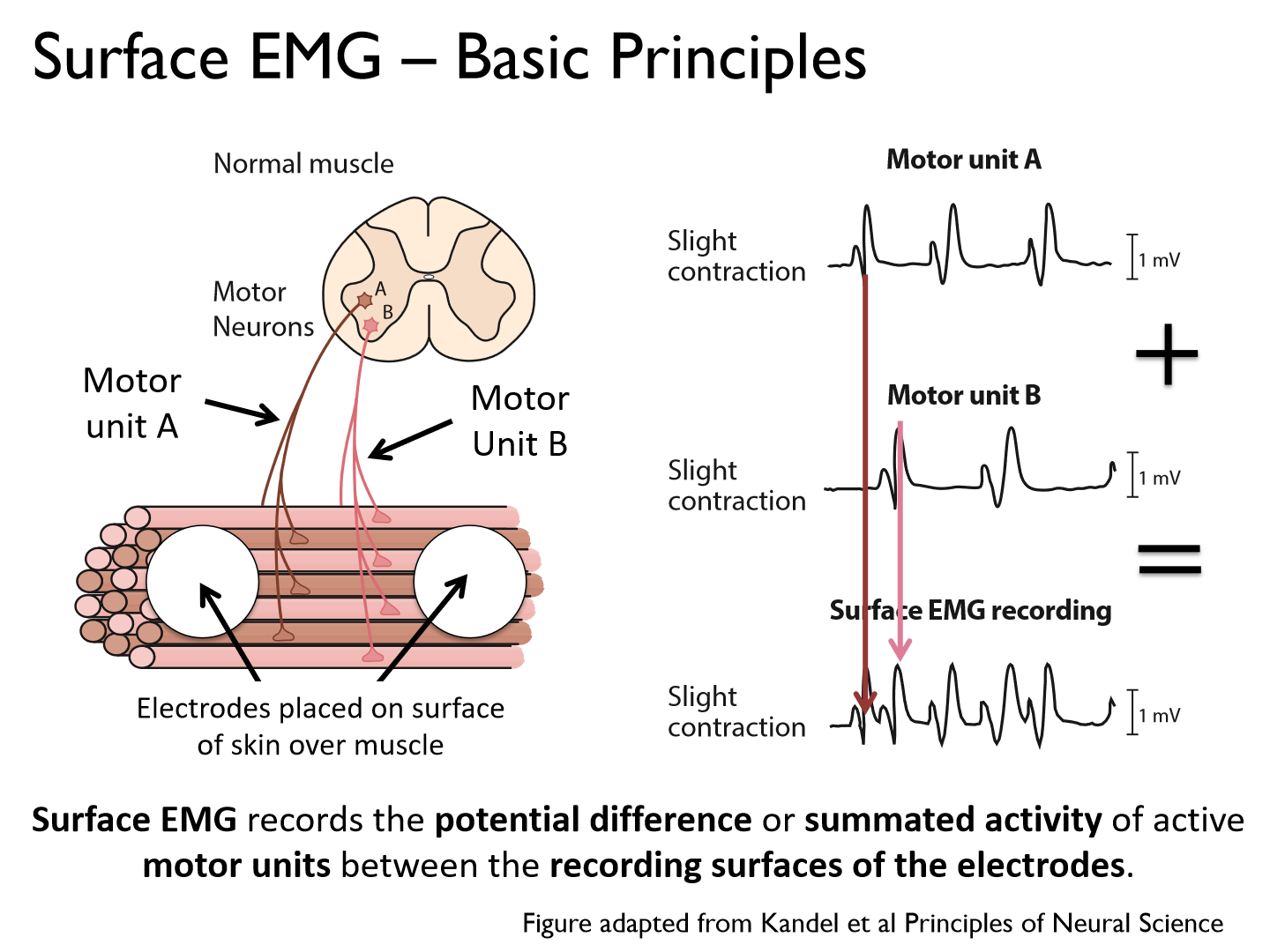
- Electrodes are placed on the surface of the skin over muscle
- Surface electrodes span muscle fibers
- Electrodes will show/pick up firing patterns that differ in amplitude and frequency/timing
What does surface EMG record?
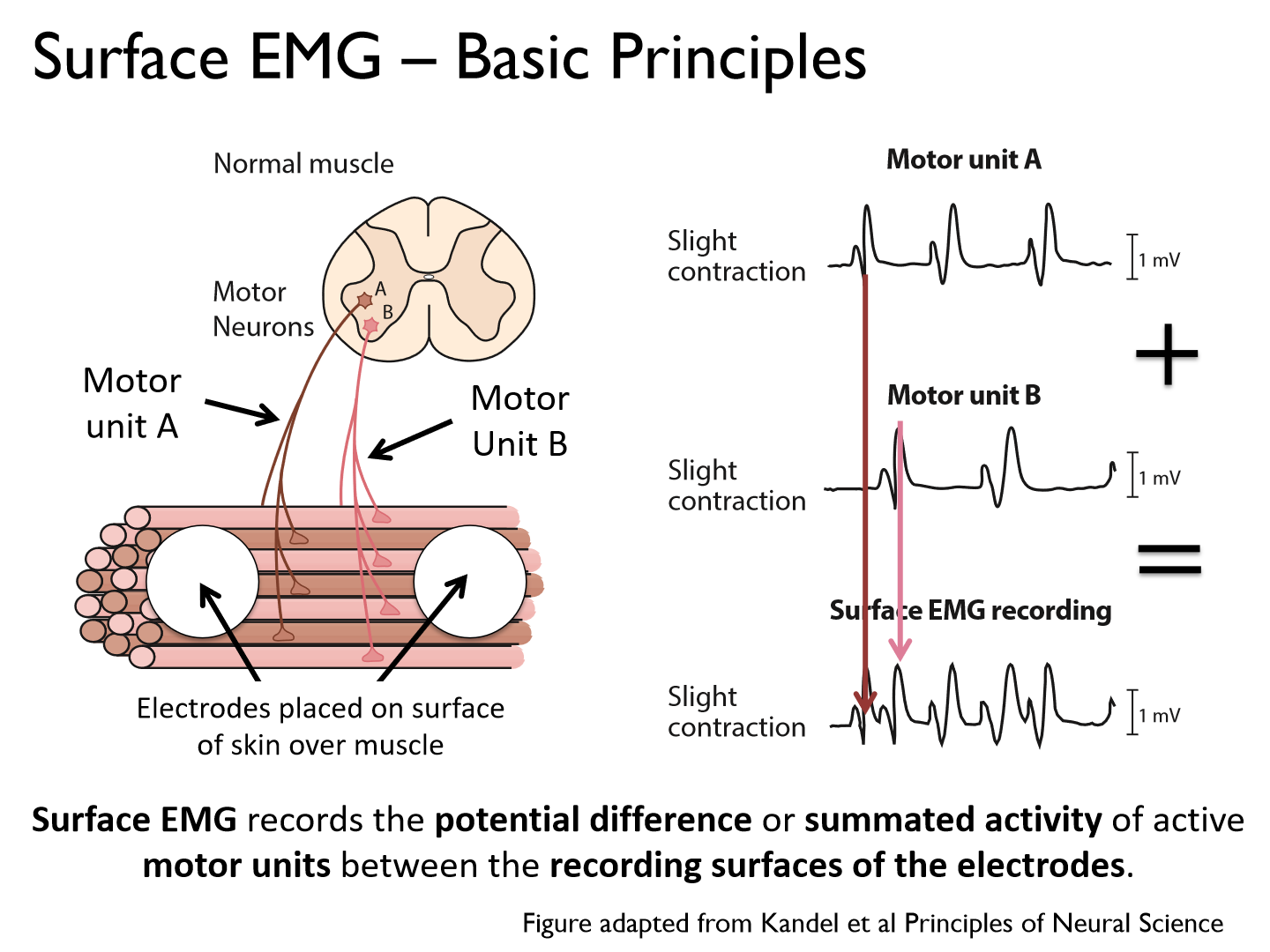
the potential difference or summated activity of active motor units between the recording surfaces of the electrodes.
Types of surface EMG sensors
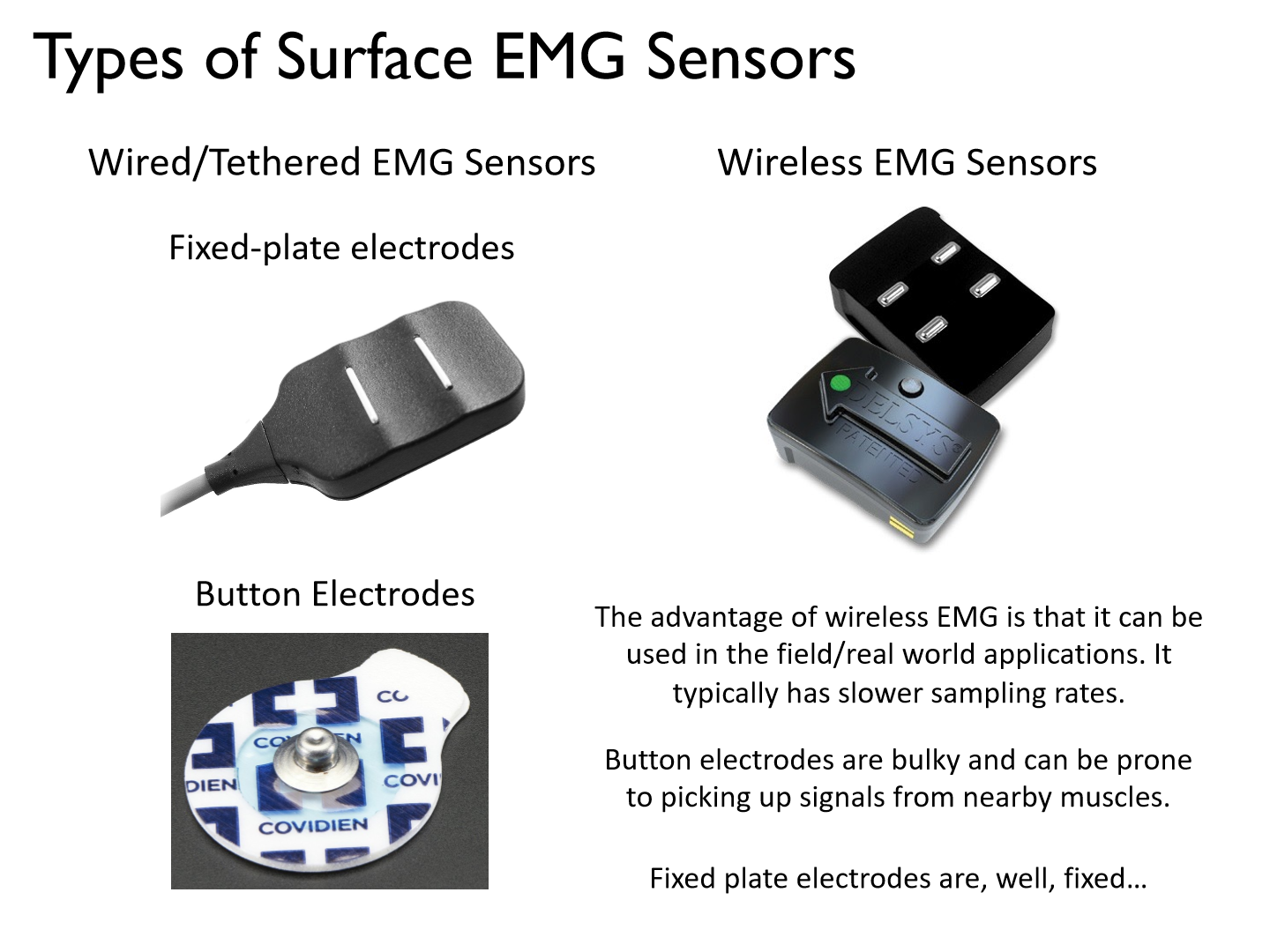
Wired/tethered EMG sensors
1. fixed-plate electrodes
2. button electrodes
Wireless EMG sensors
Pros/cons of different surface EMG sensors
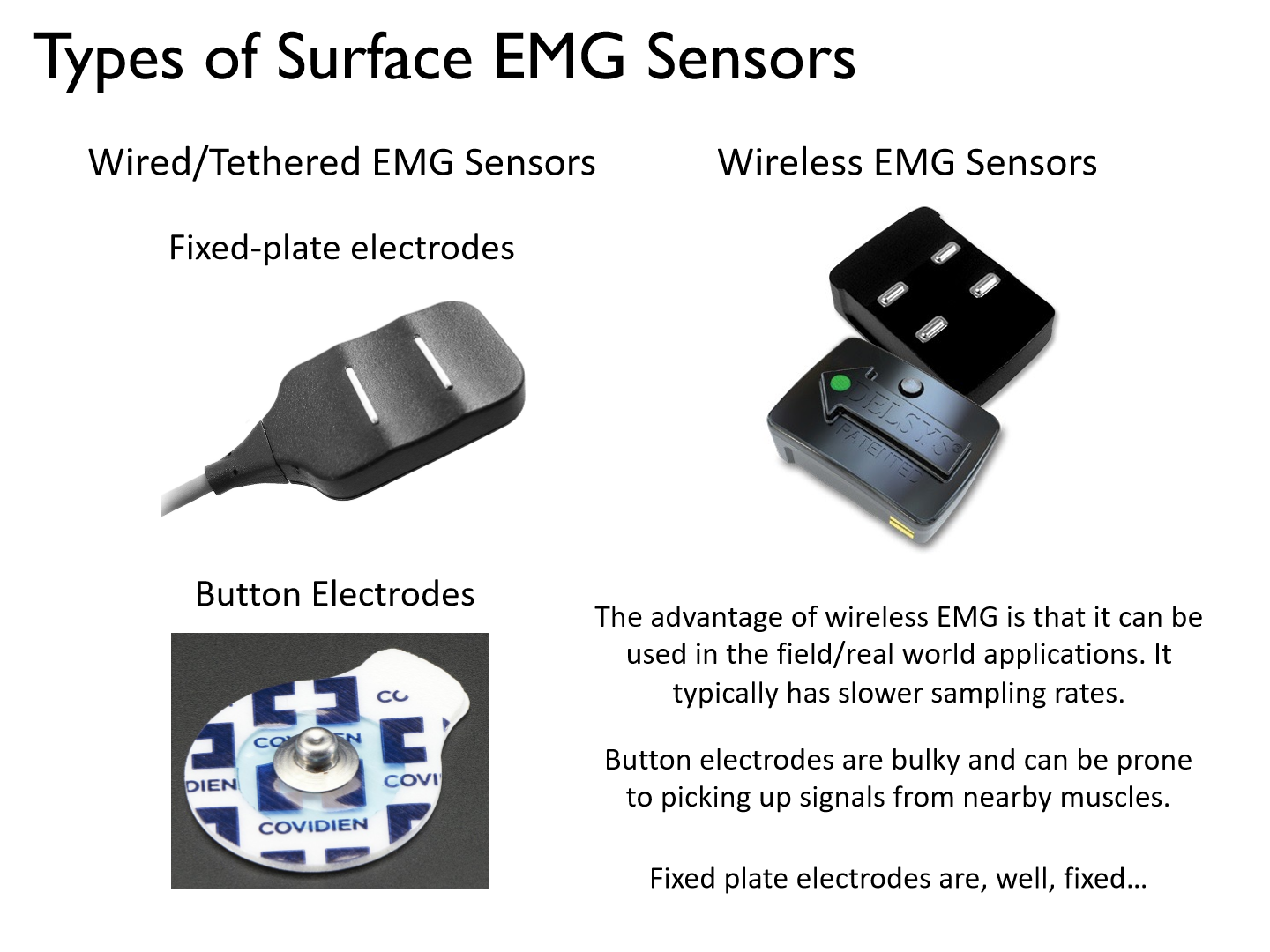
- The advantage of wireless EMG is that it can be used in the field/real world applications.
- Wireless EMG typically has slower sampling rates. It misses data (not as accurate)
- Button electrodes are bulky and can be prone to picking up signals from nearby muscles.
- Fixed plate electrodes are, well, fixed..
Surface EMG Pros:
1) Easy to use.
2) Non-invasive.
Surface EMG Cons:
1) Restricted to superficial muscles
2) Signal quality related to depth of subcutaneous tissue at recording site (e.g., fat).
3) Suitable for large muscles (e.g., crosstalk between adjacent muscles if the muscles are small)
Indwelling EMG (2 types)

an invasive technique used to record the activity of individual motor units in skeletal muscle
1. Concentric needle EMG
2. Fine wire EMG
Needle EMG basic idea
- Needle EMG uses an electrode inserted into skeletal muscle and a reference/ground electrode.
- Ground electrode is used to eliminate environmental ‘noise’ that contaminates the EMG signal (e.g., lights, electrical outlets, computer power sources).
- Typically used in medical diagnostics (e.g., difficult to move with a needle in the arm).
*needle NOT flexible = can't move muscle
Where is needle EMG typically used?
medical diagnostics
What is an advantage of needle EMG?
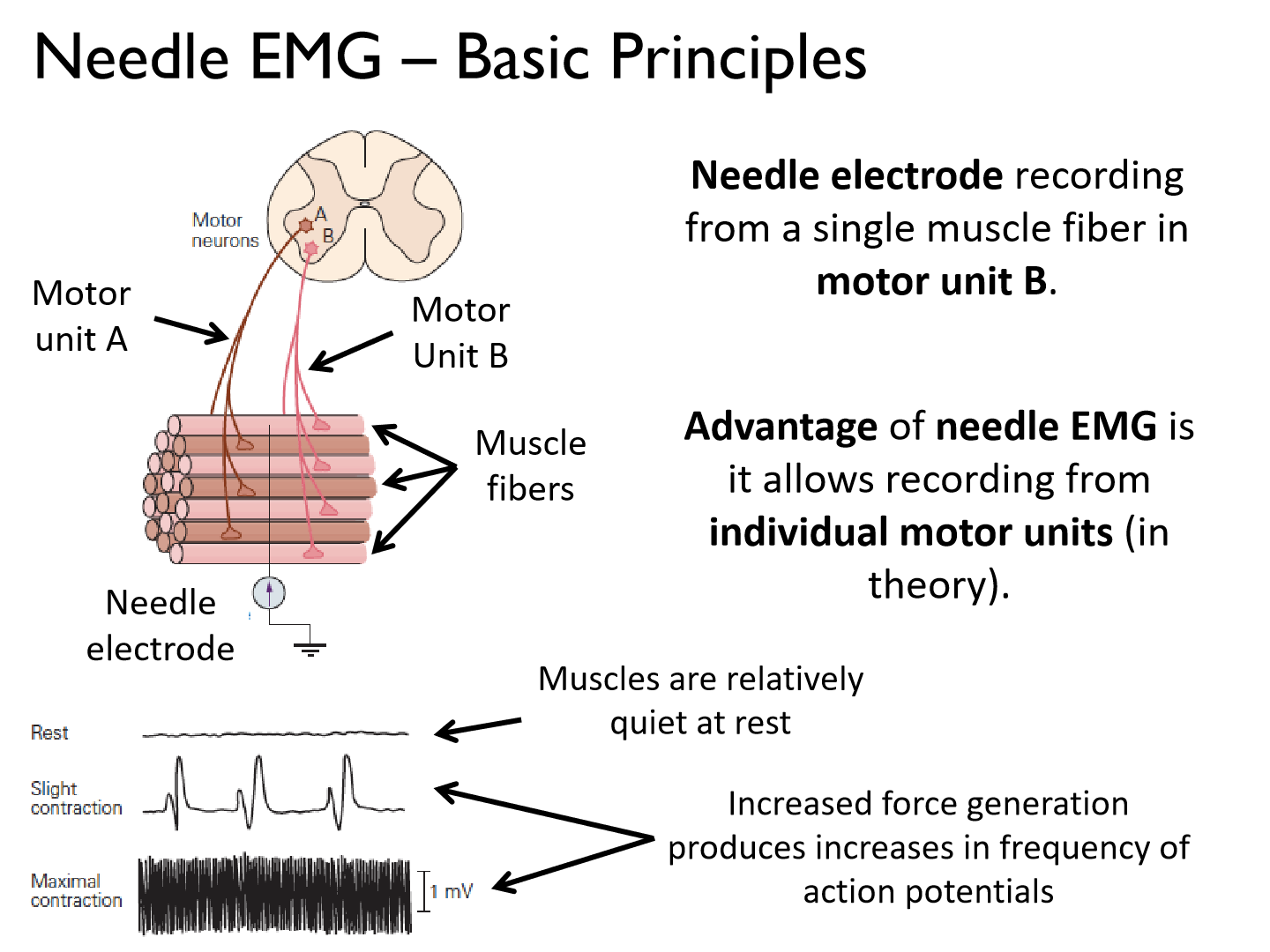
it allows recording from individual motor units (in theory).
Needle EMG Pros:
1) Can be used to record from deep lying muscles
2) Potential to record single motor unit action potentials
3) Useful for medical diagnostics (conduction velocities) and studying basic mechanisms of muscle contraction.
Needle EMG Cons:
1) Amount of movement is restricted.
2) Invasive recording technique.
Fine wire EMG
an invasive technique used to record the activity of individual motor units in skeletal muscle
Fine wire EMG process and purpose
- Fine wire EMG uses a needle inserted into skeletal muscle and a reference/ground electrode. The needle is then retracted, leaving the wires embedded in muscle.
- Typically used to record from deep lying muscles in active motor tasks (i.e., permits more motion than needle EMG).
Fine wire EMG Pros:
1) Can be used to record from deep lying muscles.
2) Smaller recording surface provides better resolution than surface EMG and allows recording from small and/or adjacent muscles.
3) Restricts motion less than needle EMG.
Fine wire EMG Cons:
1) Invasive recording technique.
2) Poorer resolution (larger pickup volume) than needle EMG (but better than surface EMG)
*harder accuracy
Structural Magnetic Resonance Imaging (MRI)
a non-invasive technique that uses magnetic fields to image the anatomy of the brain.
How does a structural MRI work? (when was it invented)
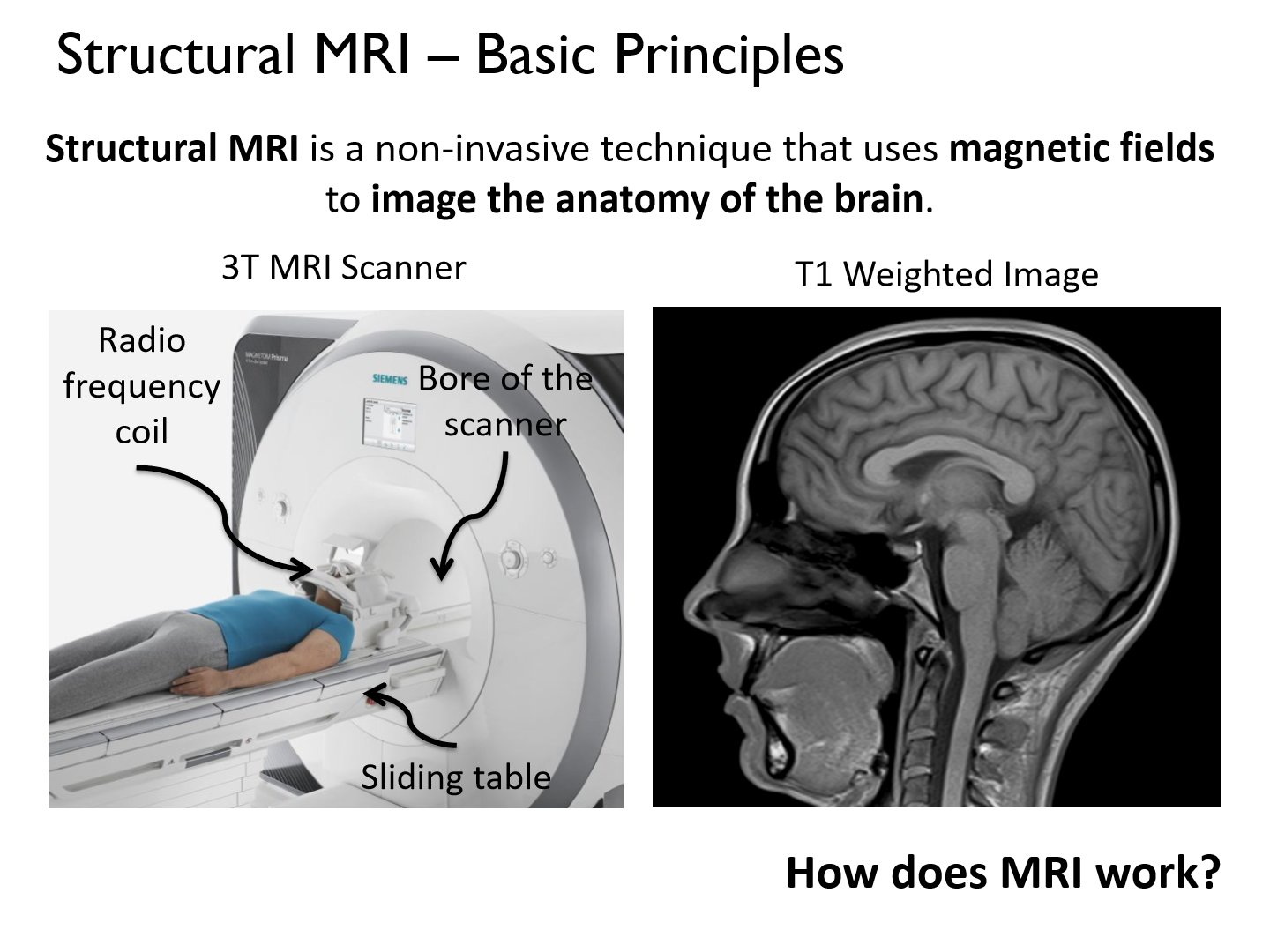
- A tool to safely and routinely image tissue with H2O content (e.g., brain, lungs, heart)
- Structural MRI has a resolution of 1-2 mm 3 (voxel)
- Developed in the early 1970’s by Lauterbur, Mansfield and Damadian.
- Lauterbur and Mansfield won the Nobel Prize in Physics in 2004.
Anatomy of an MRI scanner
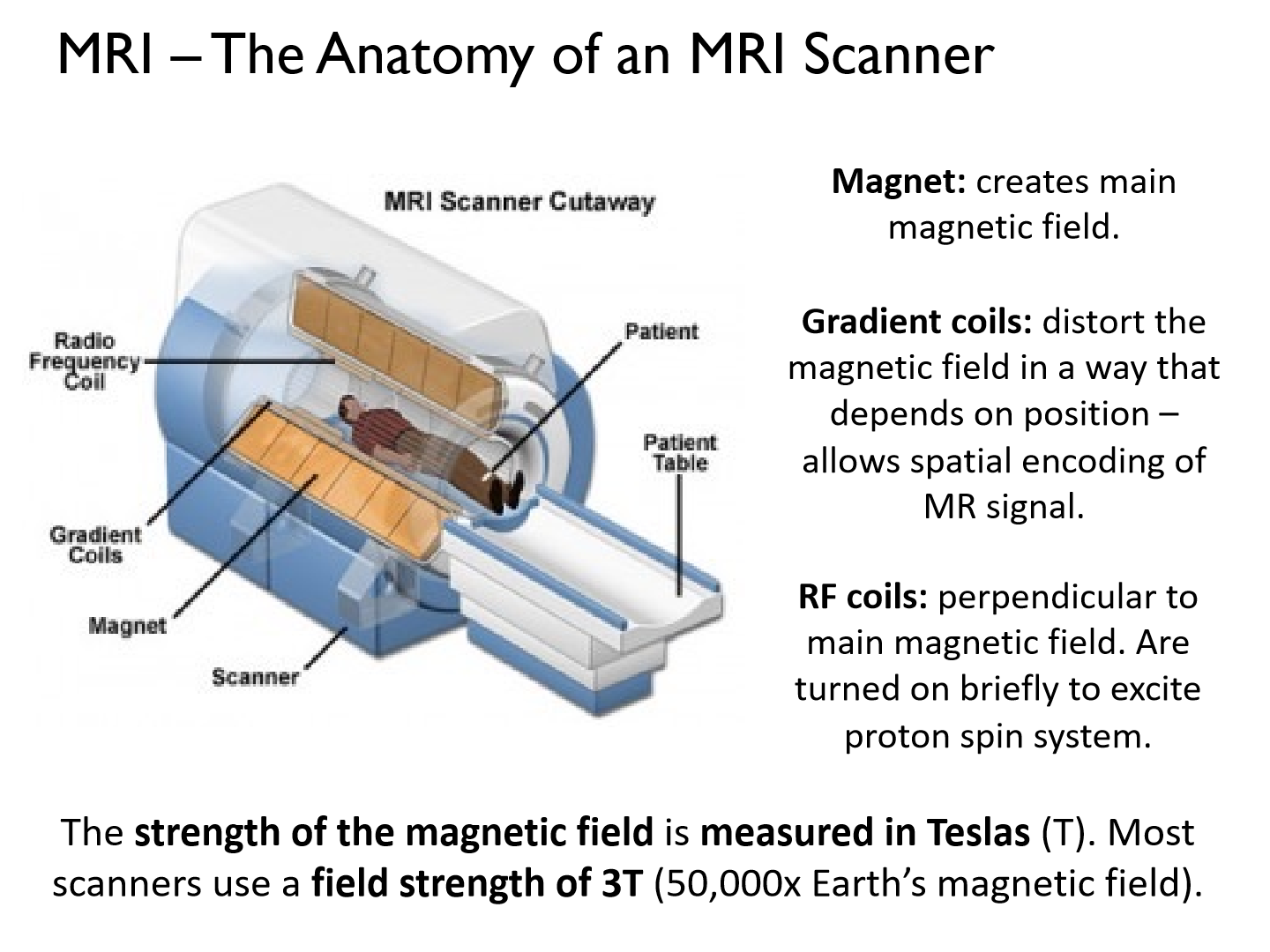
Magnet: creates main magnetic field.
Gradient coils: distort the magnetic field in a way that depends on position – allows spatial encoding of MR signal.
RF coils: perpendicular to main magnetic field. Are turned on briefly to excite proton spin system. (radio frequency)
What is the strength of the magnetic field measured in?
Teslas (T).
Most scanners use a field strength of 3T (50,000x Earth’s magnetic field).
How to MRIs magnetic field work?
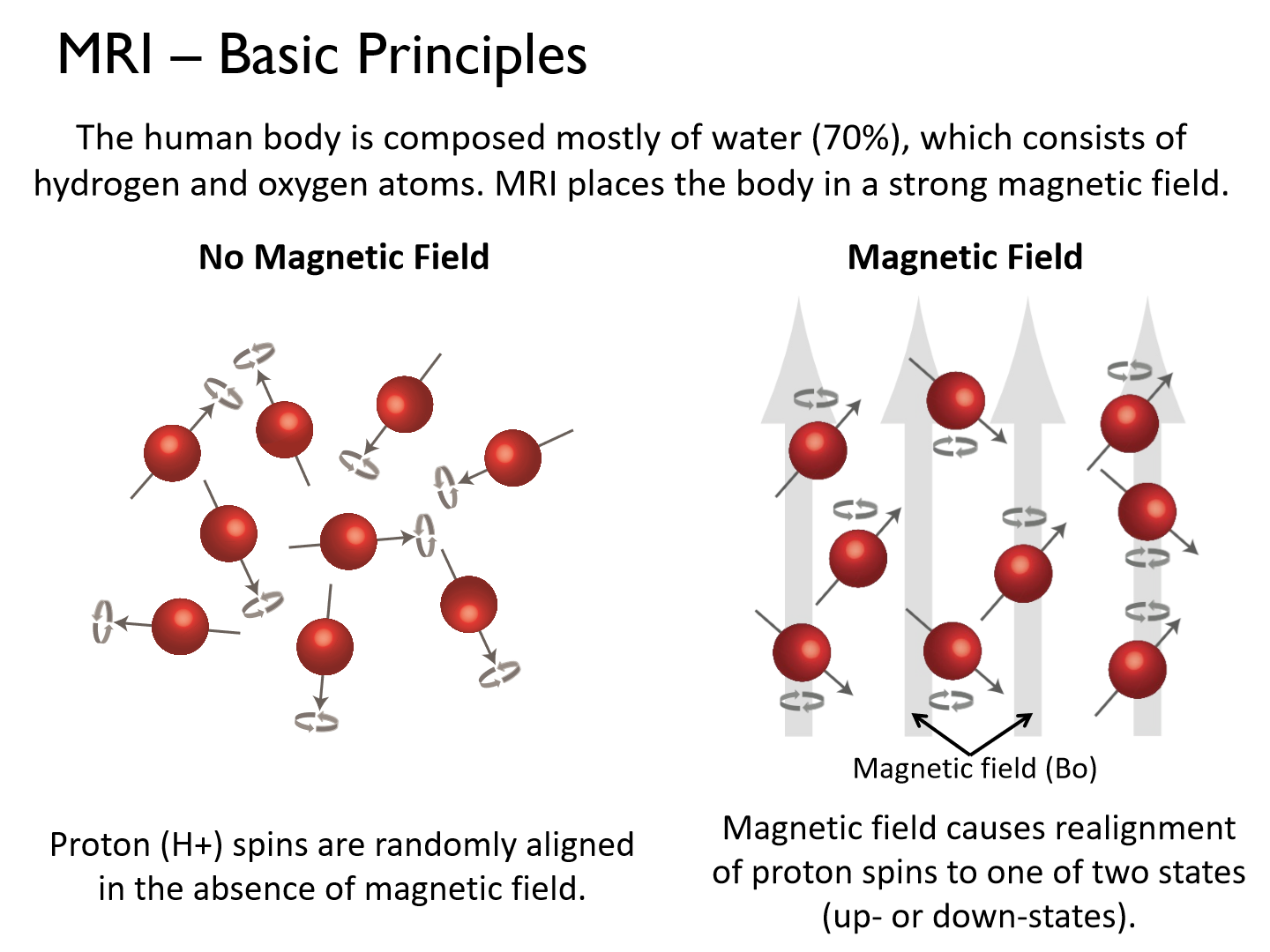
The human body is composed mostly of water (70%), which consists of hydrogen and oxygen atoms. MRI places the body in a strong magnetic field.
*Magnetic field causes realignment of proton spins to one of two states (up- or down-states).
What does the introduction of the magnetic field create?
Introduction of the magnetic field creates a torque that causes the proton to spin on a skew axis around the magnetic field
– precession.
How do MRI's radio waves work?
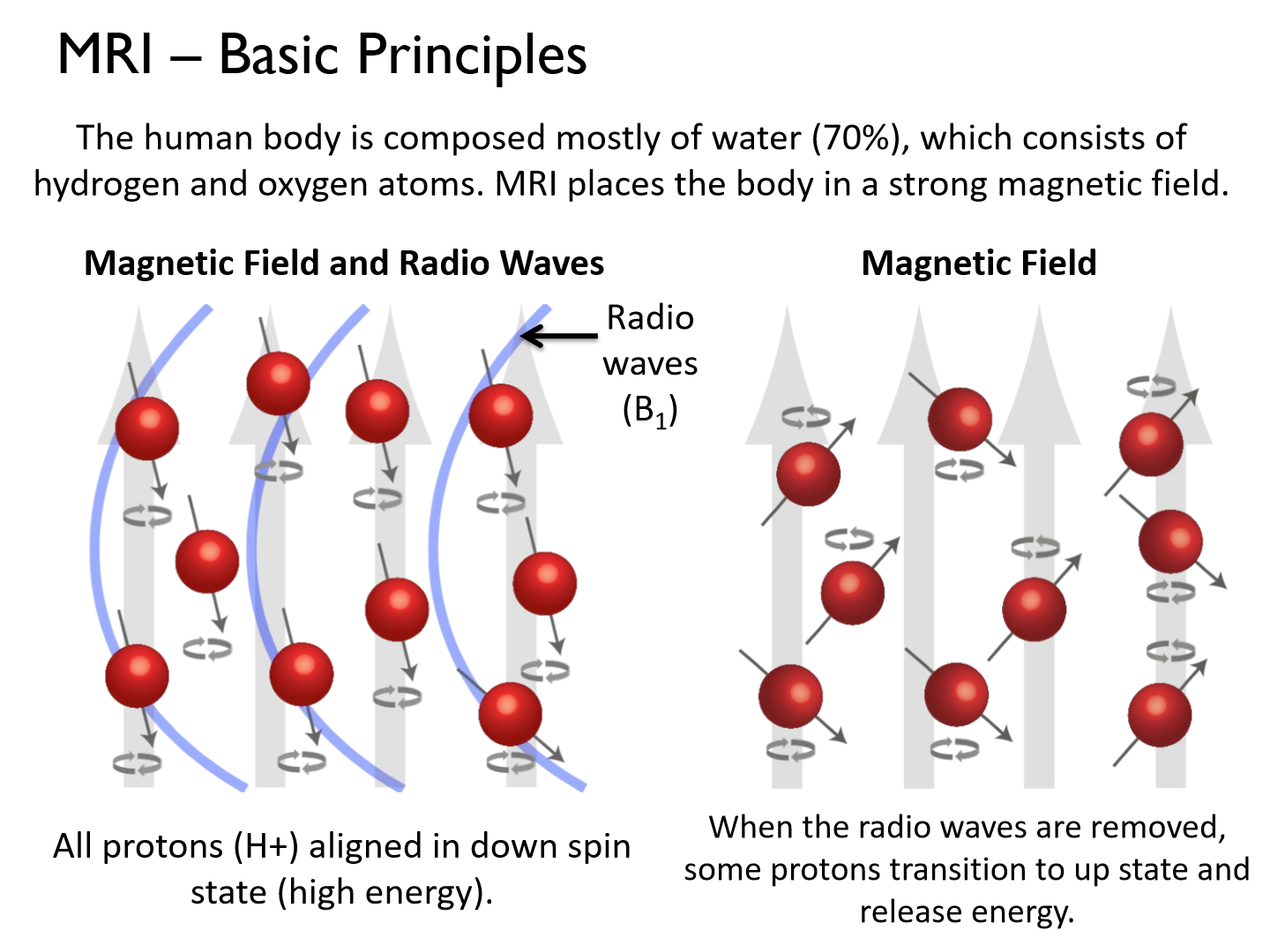
All protons (H+) aligned in down spin state (high energy).
**H2O content varies in different types of tissue (fat, cerebrospinal fluid, bone, etc.). This influences the MR signal/images.
What is the basic unit of measurement in structural MRIs?
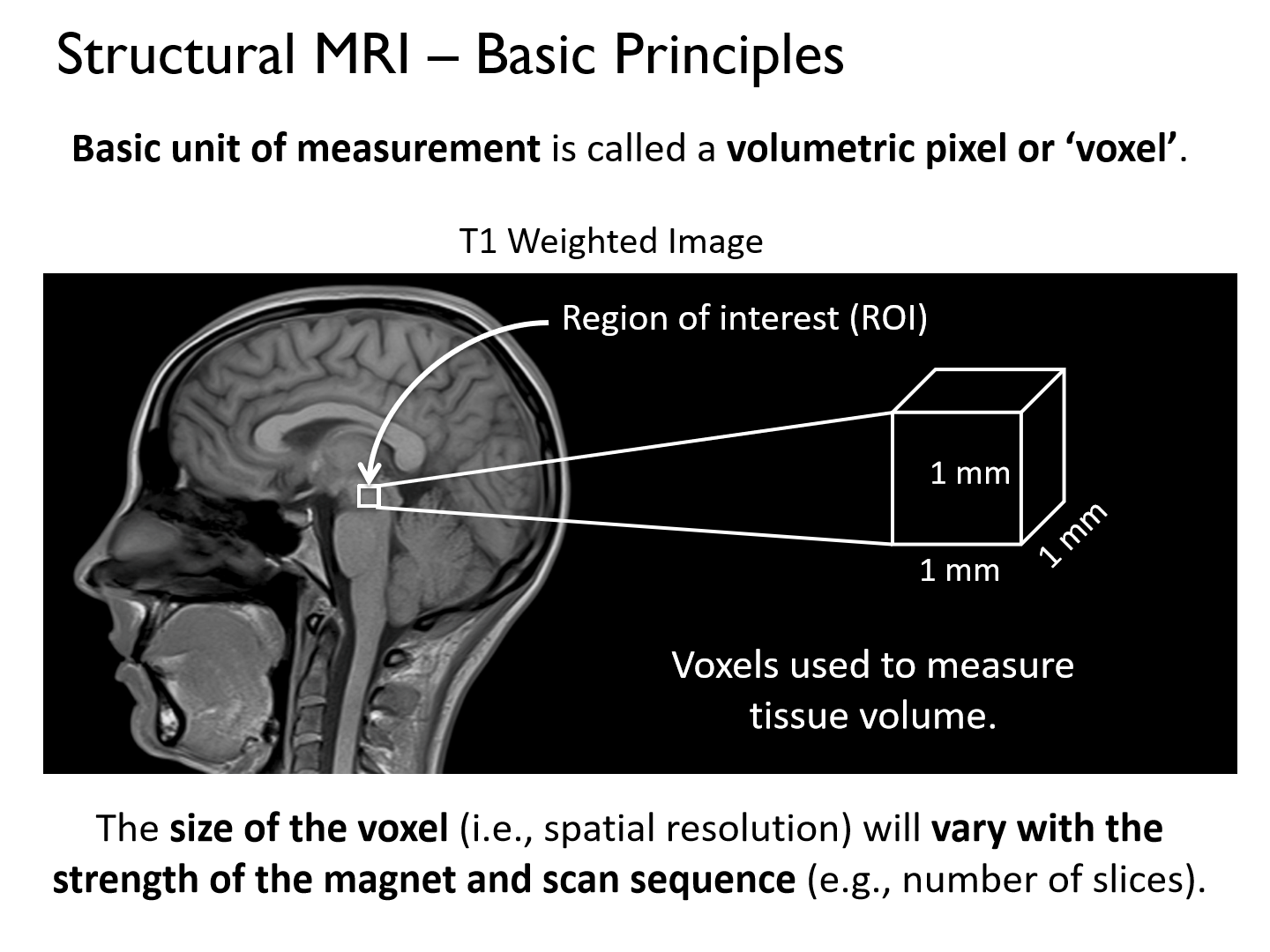
- a volumetric pixel or ‘voxel’.
- The size of the voxel (i.e., spatial resolution) will vary with the strength of the magnet and scan sequence (e.g., number of slices).
Structural MRI Pros:
1. Noninvasive.'
2. Allows visualization of brain structure/anatomy in humans.
3. Good spatial resolution.
4. Understand relationship between brain structure and behavioural function.
Structural MRI Cons:
1. Static snapshots of brain anatomy, but not function.
2. Expensive (~$550/hr research costs)
What is MRI the best tool for?
MRI is the best tool for imaging and quantifying brain structure.
- Structural MRI creates pictures of the brain based on the water content in different types of neural tissue.
Functional Magnetic Resonance Imaging (fMRI)
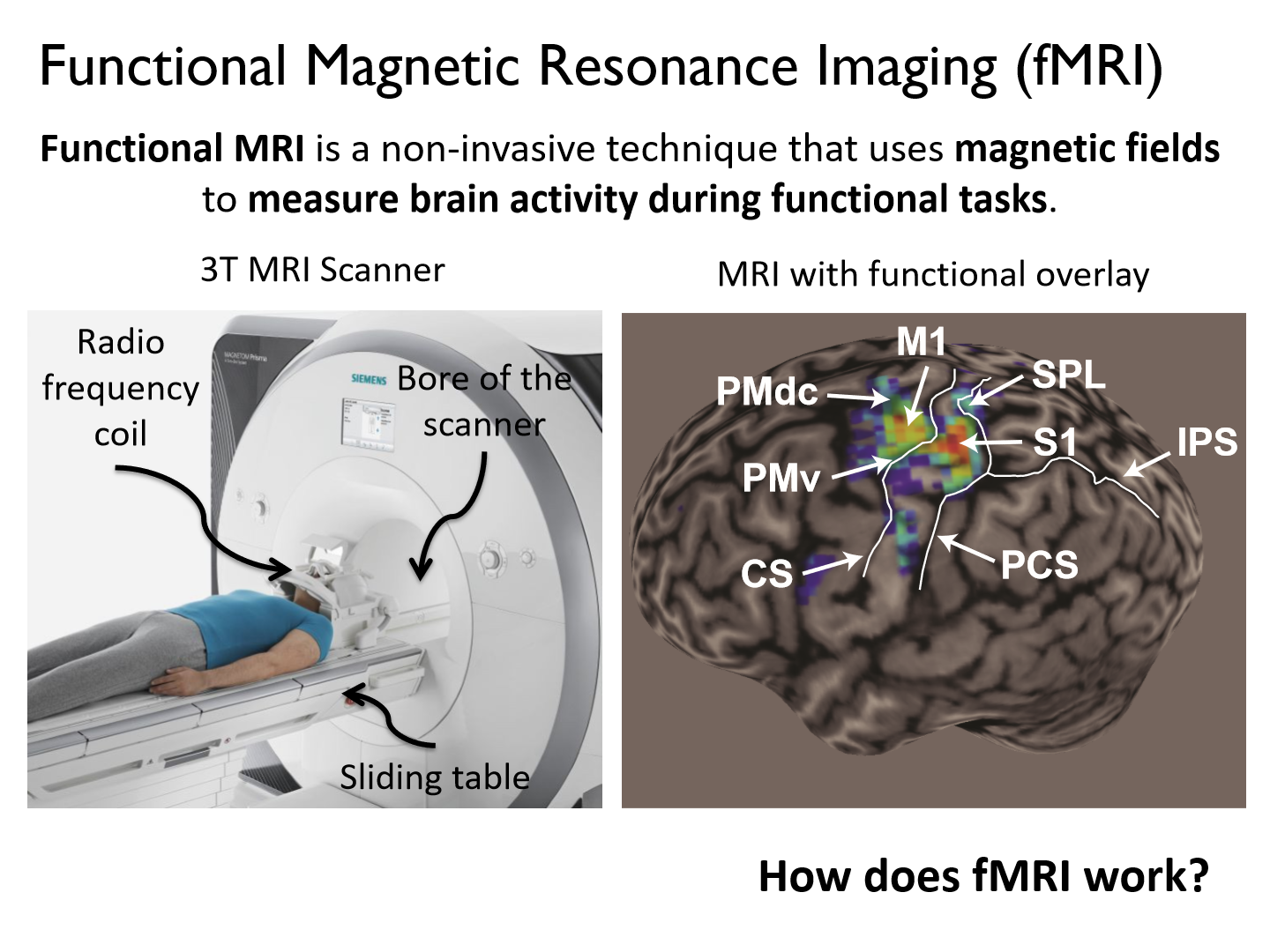
a non-invasive technique that uses magnetic fields to measure brain activity during functional tasks.
*Blood flow
How do fMRIs work?
by measuring blood-oxygenation level dependent signals.
*Increased brain activity leads to increase in regional blood flow. This causes an increase in oxygenated hemoglobin to fuel brain activity.
*Deoxygenated hemoglobin is more magnetic than oxygenated hemoglobin. This leads to different MR signals in active vs. inactive areas of the brain.
What is fMRI a measure of
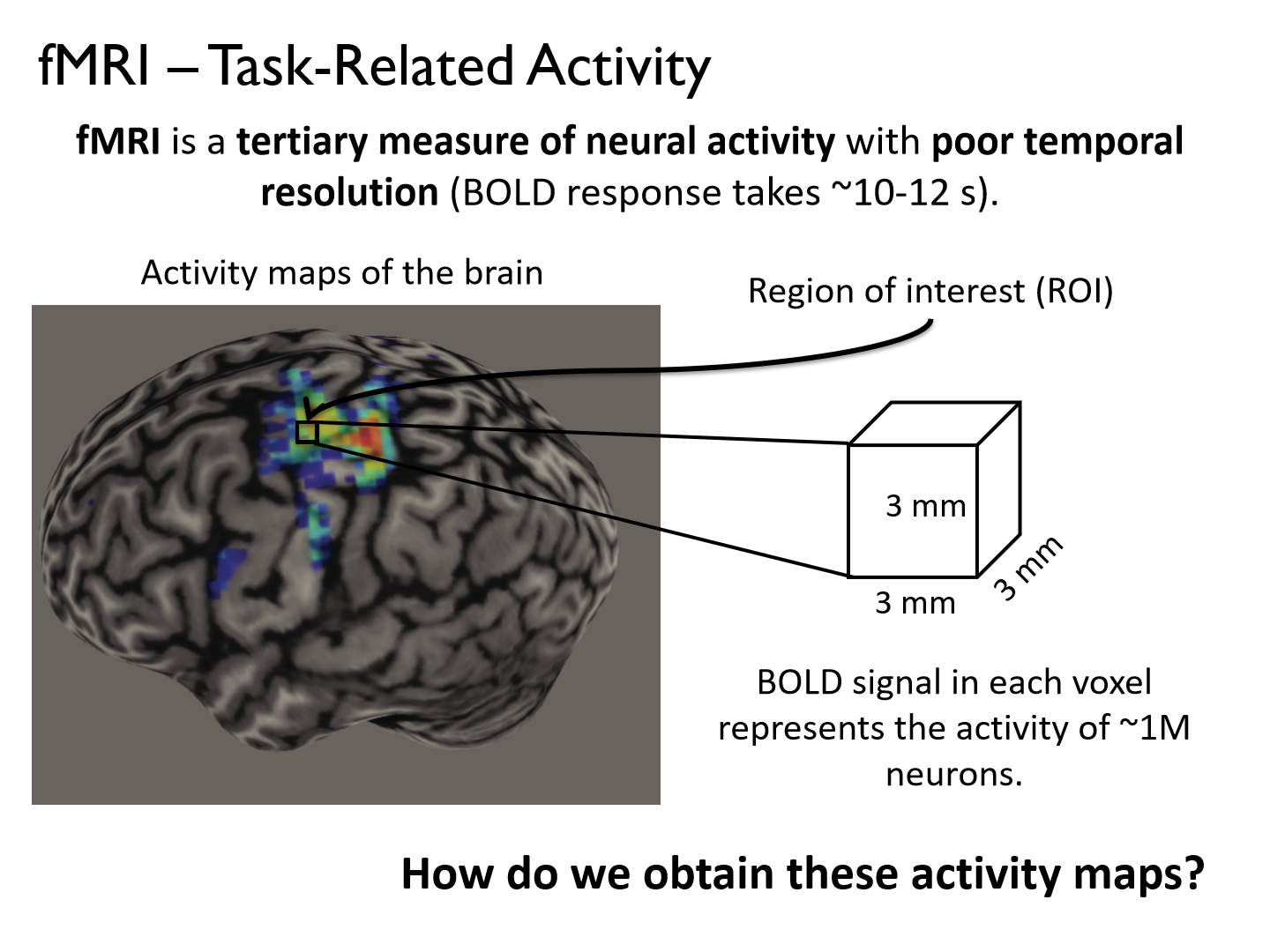
fMRI is a tertiary measure of neural activity with poor temporal resolution (BOLD response takes ~10-12 s).
*delayed measure (NOT most accurate)
What do participants do in a fMRI experiment
participants perform goal-directed actions or cognitive tasks in the MR scanner.
- Participants perform target-directed eye movements or (small) arm movements while the scanner images blood flow in their brain.
*largest change in 02 consumption
What do functional tasks generate in fMRI?
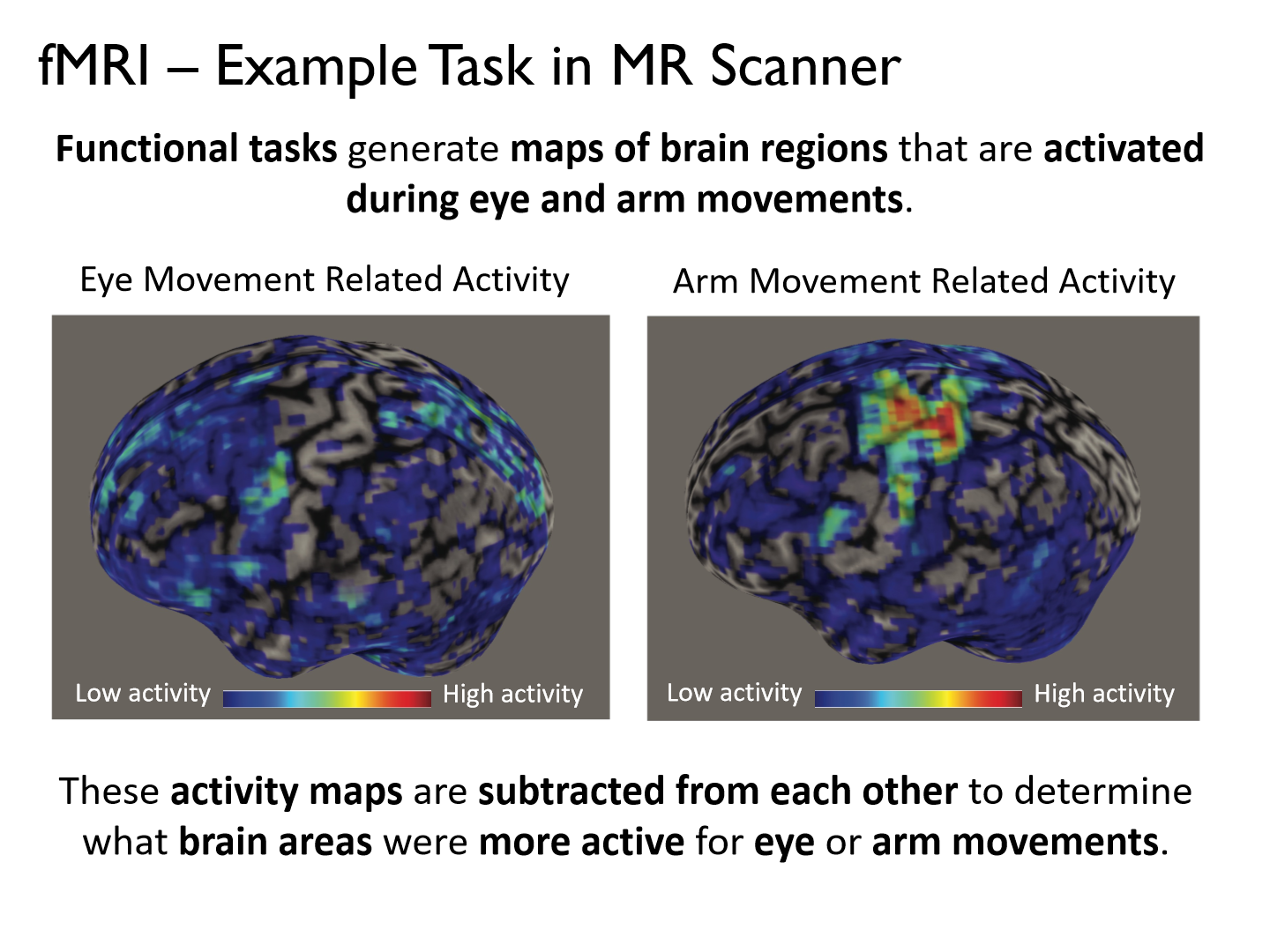
Functional tasks generate maps of brain regions that are activated during eye and arm movements.
*These activity maps are subtracted from each other to determine what brain areas were more active for eye or arm movements.
What does the reaching network look like
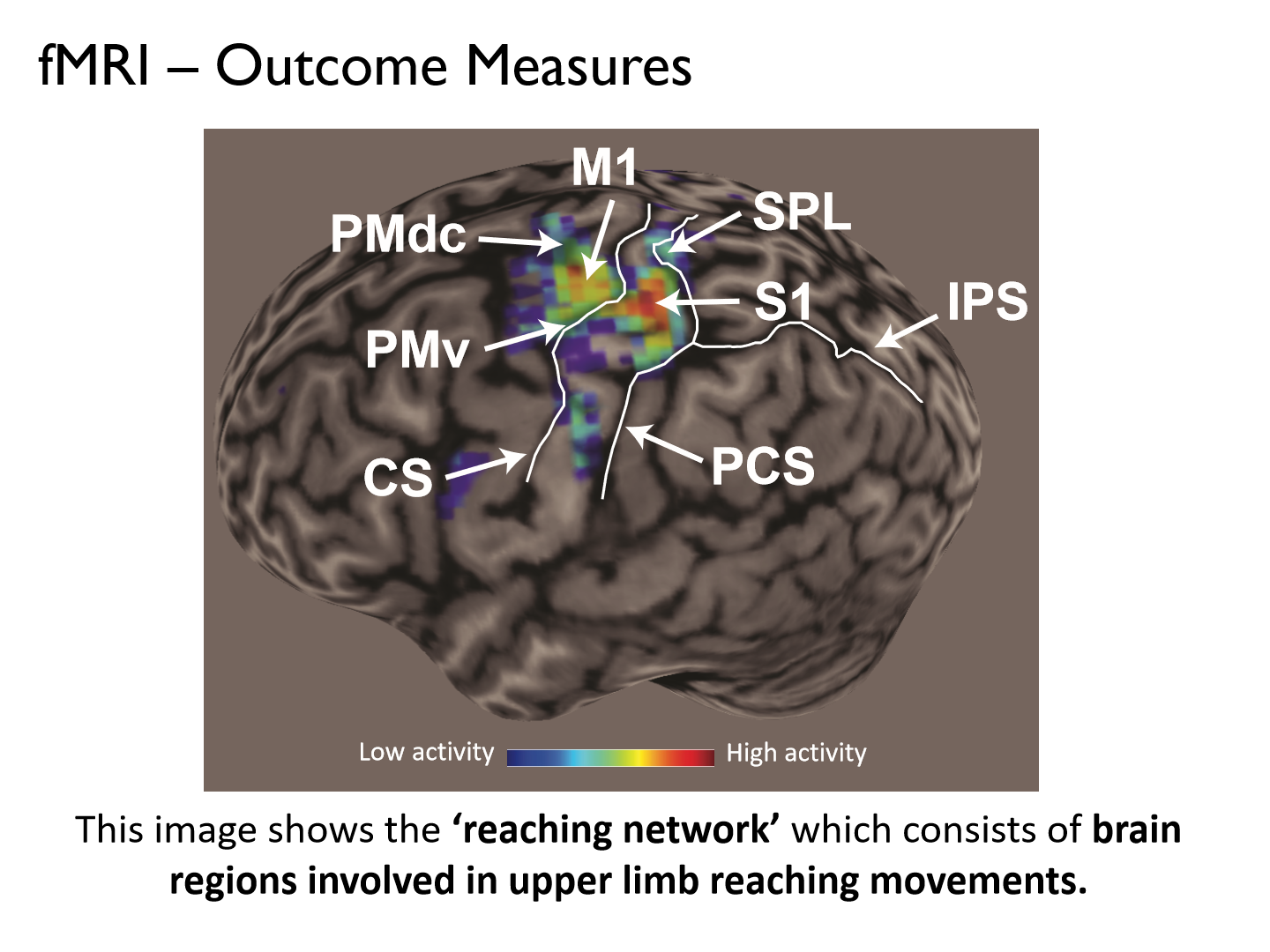
the ‘reaching network’ which consists of brain regions involved in upper limb reaching movements.
*M1: primary motor cortex
S1: primary sensorimotor cortex
What is fMRI the best tool for?
the best tool for imaging and quantifying brain function.
fMRI Pros:
1) Noninvasive.
2) Allows quantification of brain activity in awake and behaving humans.
3) Good spatial resolution.
fMRI Cons:
1) Poor temporal resolution (10-20s, looks at average activity)
2) Permits only small movements. Large movements distort the magnetic field or move the head (motion artifact).
3) Expensive (~$550/hr research costs)
*We are measuring non-instantaneous actions
What does the nervous system use sensory feedback from our body and surrounding world for?
to adjust ongoing actions
Tactile inputs from the motor periphery are _______ for voluntary motor actions
critical
What happens to movement when a participant's fingers are anesthetized?
finger movements become uncoordinated
*sensory feedback from cutaneous receptors is critical for normal motor function
Cutaneous mechanoreceptor
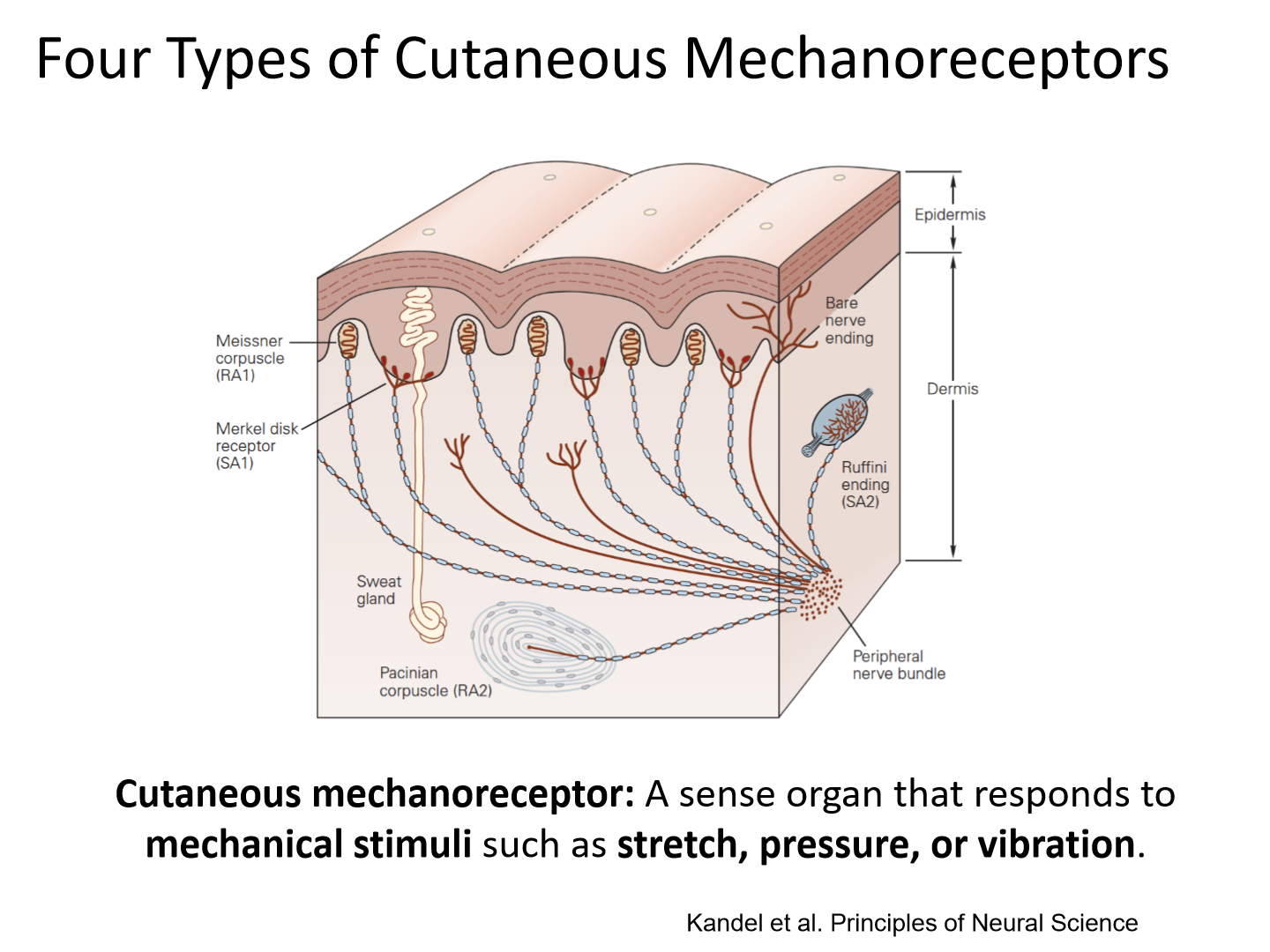
A sense organ that responds to mechanical stimuli such as stretch, pressure, or vibration
What are the 4 types of mechanoreceptors in glabrous skin?
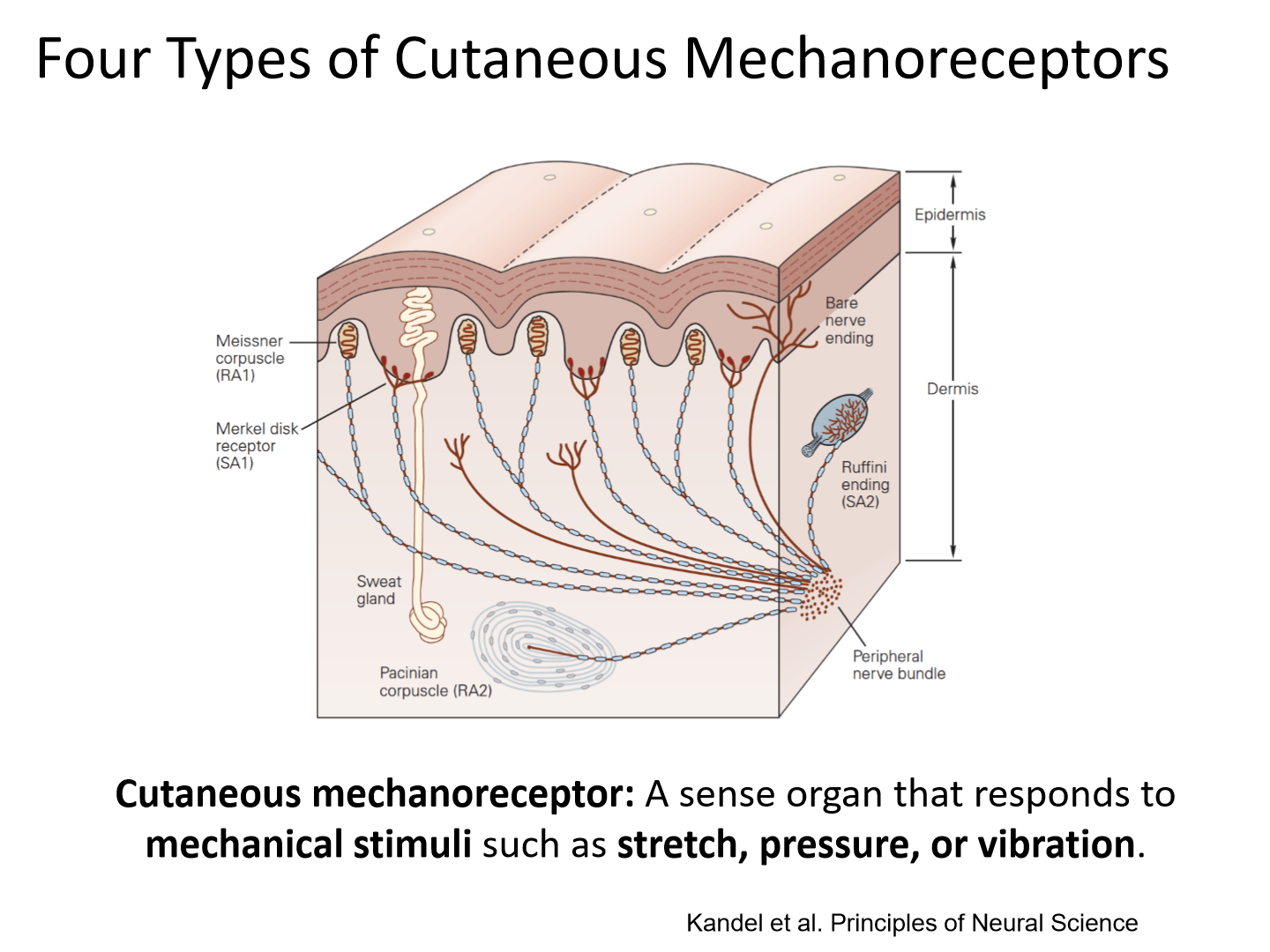
Meissner corpuscles, Merkle disks, Ruffini endings, Pacinian corpuscles
Glabrous skin
Hairless skin (e.g. palm of hand, sole of foot)
How do the 4 mechanoreceptors in glabrous skin differ?
These receptors differ in terms of their:
1) innervation patterns, (sup.=more, deep=1)
2) location in the skin,
3) size of receptive fields, (Type 1=small, Type 2=large)
4) how they respond to touch.
How does hairy skin differ in mechanoreceptors?
Hairy skin includes the same receptors, with the exception of Meissner’s corpuscles. In hairy skin, hair follicle receptors provide similar information to Meissner’s corpuscles.
Surface receptors (Type 1) Innervation and Location in the skin
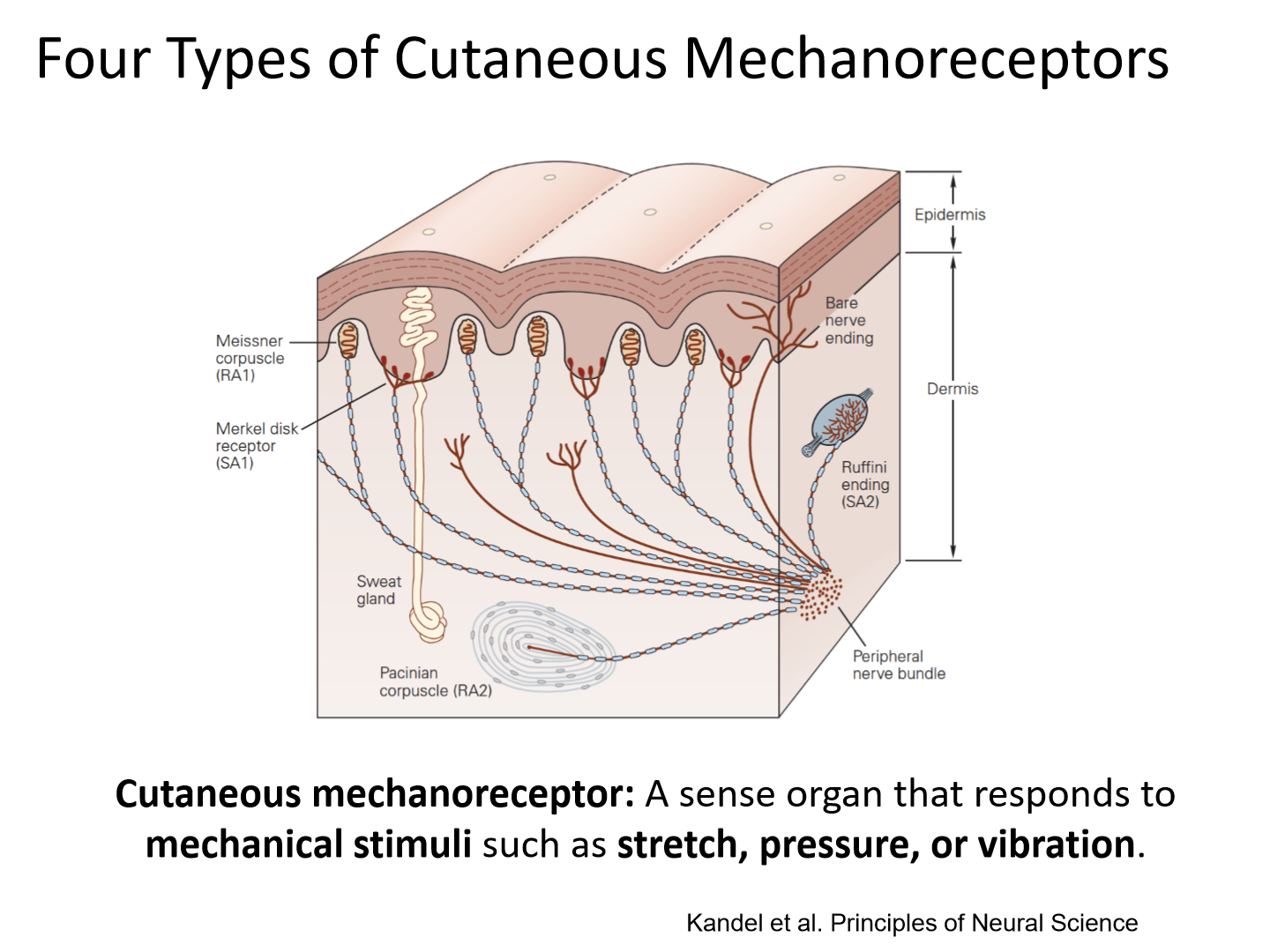
- Meissner Corpuscles, Merkel Disks.
- The nerve fibers innervating these small receptors have branching terminals.
- Each nerve fiber can innervate as many as 90-100 Merkel discs and 10-50 Meissner corpuscles.
- Low vibration frequency
Deep receptors (Type 2) Innervation and Location in the skin
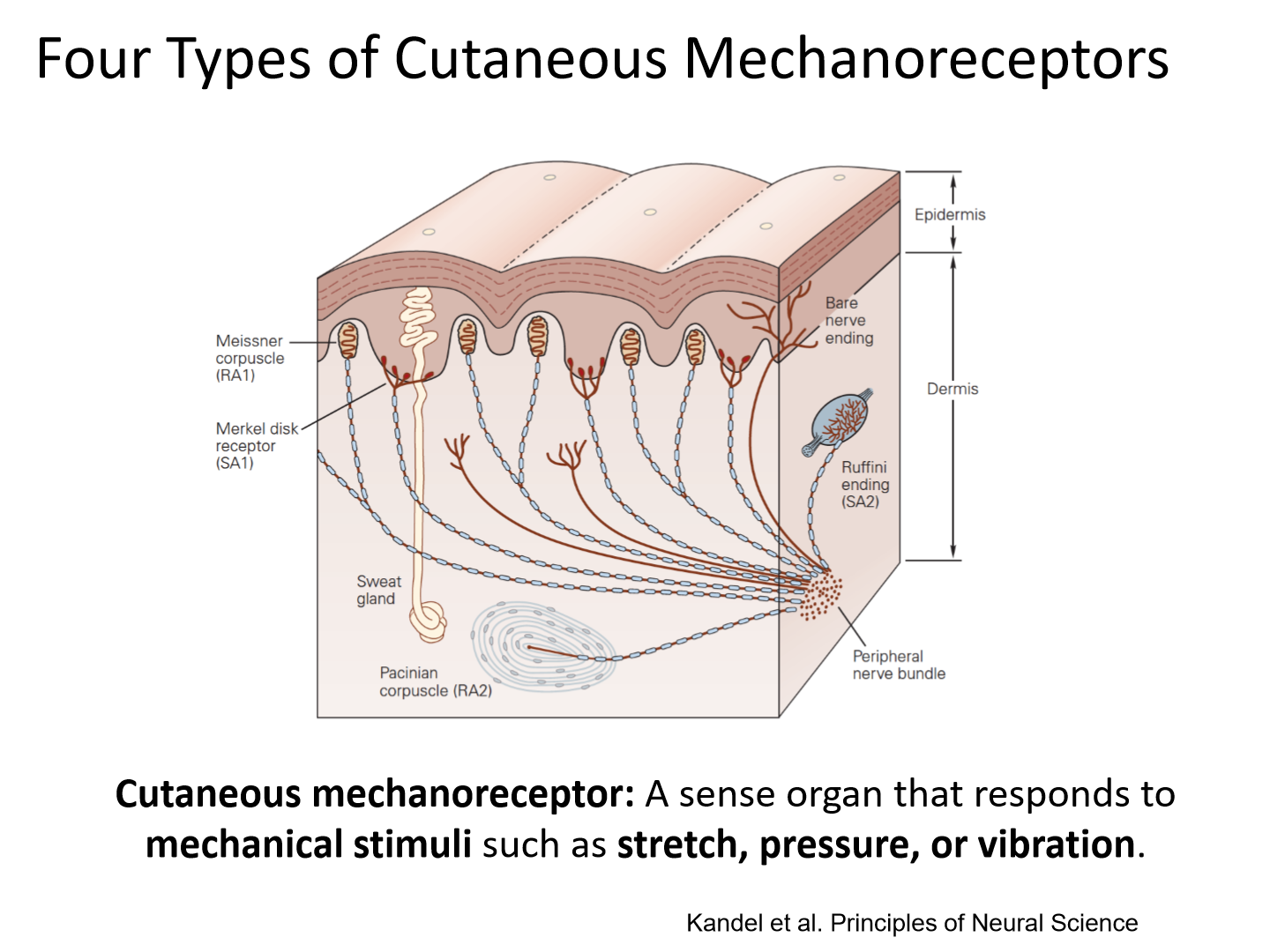
- Pacinian Corpuscles, Ruffini Endings.
- The nerve fibers innervating these large receptors innervate only one receptor.
- High vibration frequency
Slow adapting vs. rapid adapting
Slow Adapting (SA): Fire when a stimulus is applied (sustained).
Rapid Adapting (RA): Fire at stimulus onset and offset (transients).
Which mechanoreceptors are SA vs RA and different vibration frequencies
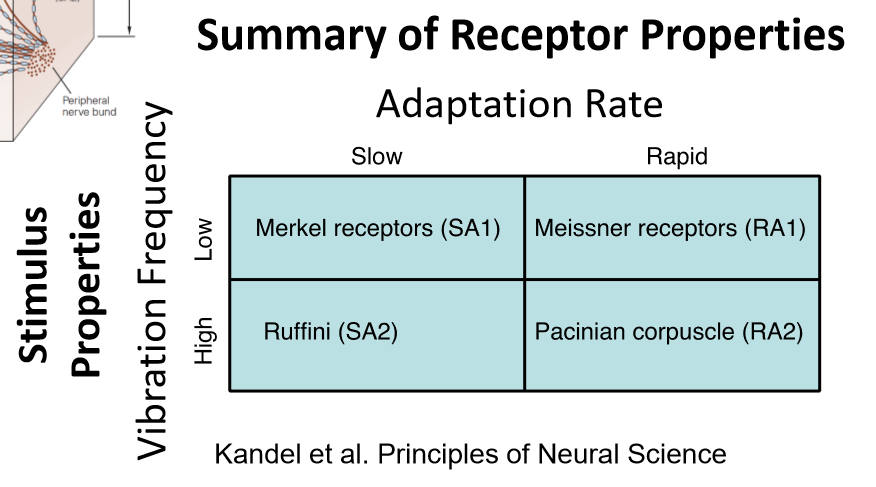
Slow: Merkle and Ruffini
Rapid: Meissner and Pacinian
Merkle discs
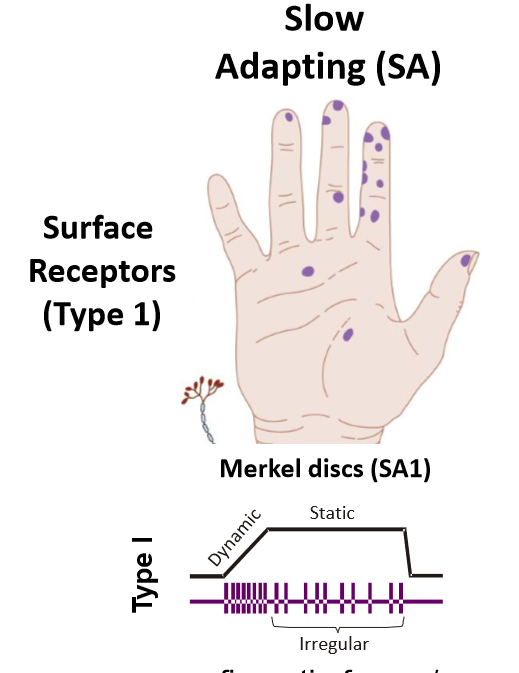
SA1
• fingertip forces/pressures
• fine forms
• Edges, points & contours
• Texture
• Reading Braille
Phone
*Signal pressure applied to the skin and are sensitive to edges, points and contours. They distinguish textures and stimuli with high spatial resolution and are important for reading Braille
Meissner corpuscles
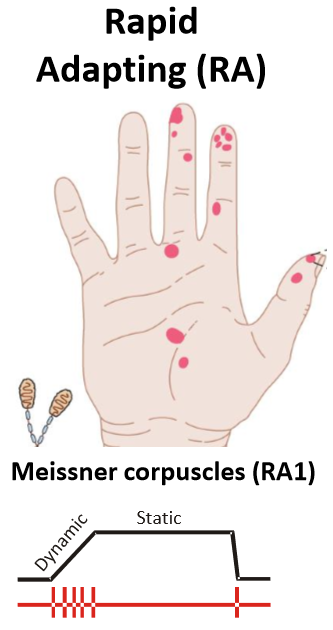
RA1
• ∆ fingertip forces
• fine forms
• moving stimuli
• friction
Beer
*They detect initial contact of the hand with objects, slippage of objects in the hand, low frequency vibrations. Respond to changes in applied stimulus- stroking, fluttering, friction, fine forms.
Properties of Surface Receptors
1. Small, complex receptive field with several hotspots
2. Nerve endings branch and innervate many receptors
3. Receptive fields are smallest on the fingertips (11mm2 for SA1 and 25mm2 for RA1)
Ruffini endings
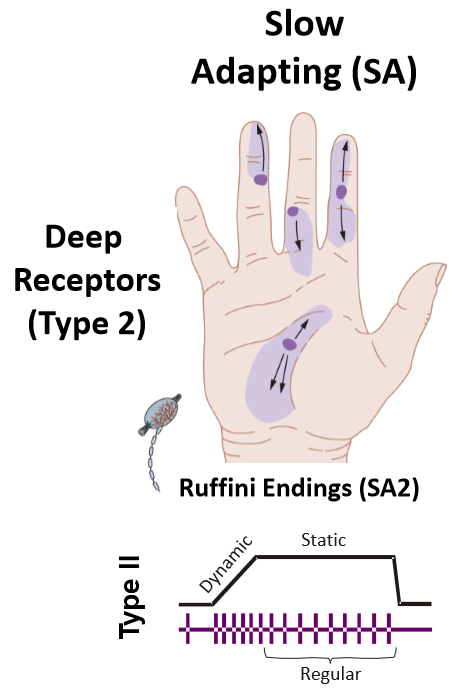
SA2
• tissue strain
• Skin indentation
• Finger movements that stretch skin
Walking
*Responds to tissue strain and skin indentation. Active during movements that stretch the skin.
Pacinian corpuscles
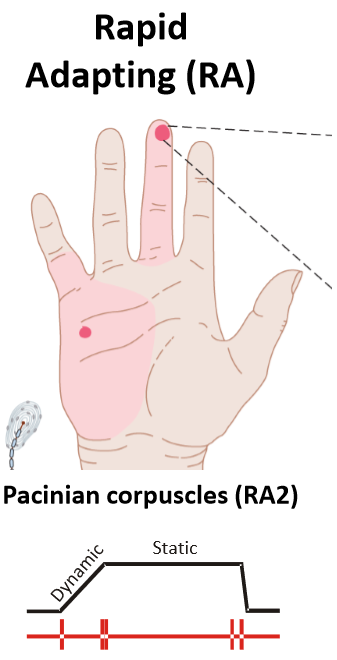
RA2
• transient events
• High-frequency vibration (500 Hz)
• Motion in nanometer range
Blind cane
*Responds to motion in the nanometer range, transient events and high frequency vibrations. High temporal resolution with 1 ms precision is important for detecting vibrations in hand-held tools or objects.
Properties of deep receptors
1. Large receptive field with single ’hot spot’ located directly above the receptor
2. Nerve endings innervate single, large receptors
Cutaneous mechanoreceptors summary
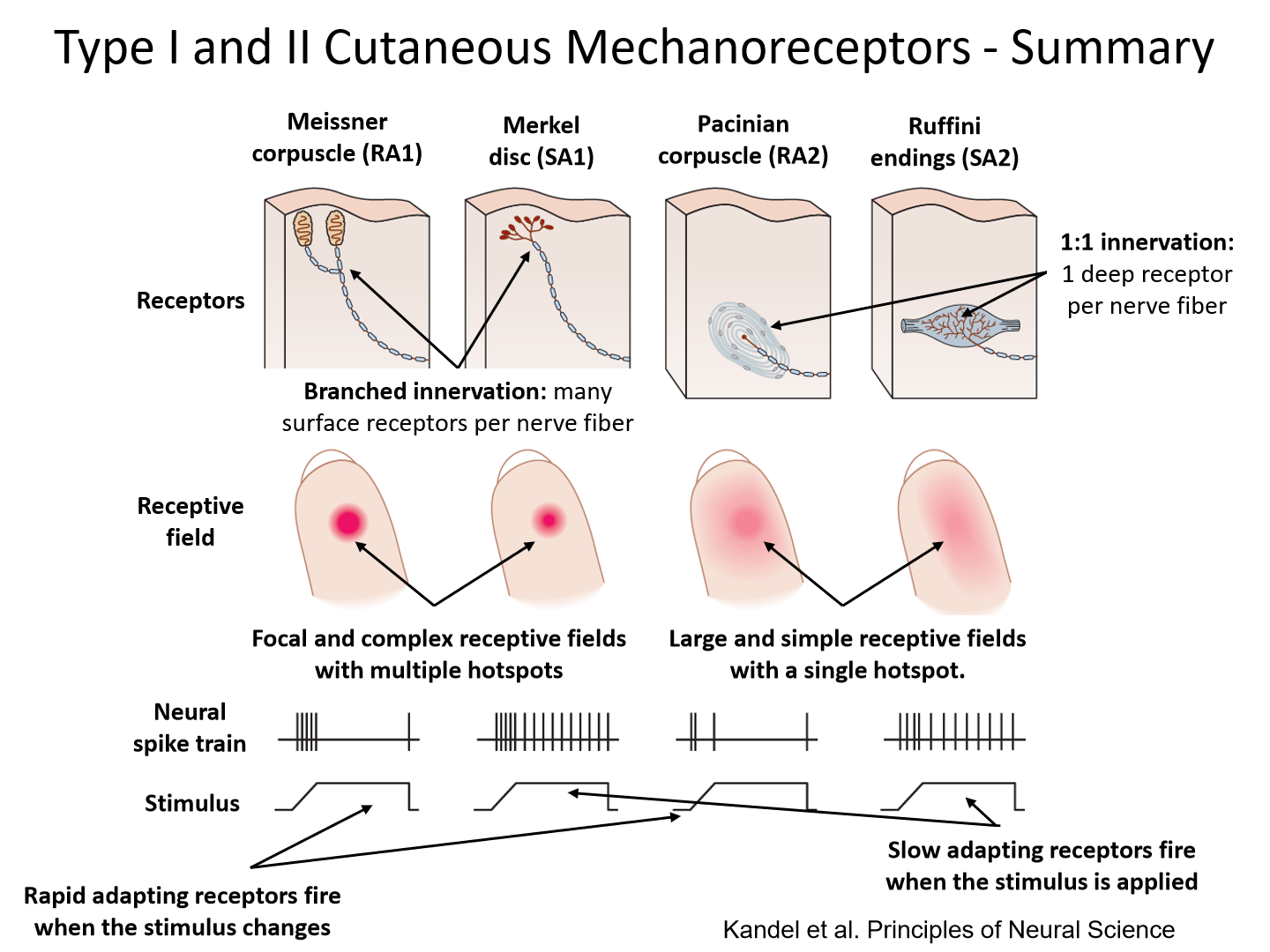
Threshold for rapid indentation/vibration of each mechanoreceptor
SA1: 8um
RA1: 2um
SA2: 40um
RA2: 0.01um
Stretch sensitive ion channel meissner corpuscle)
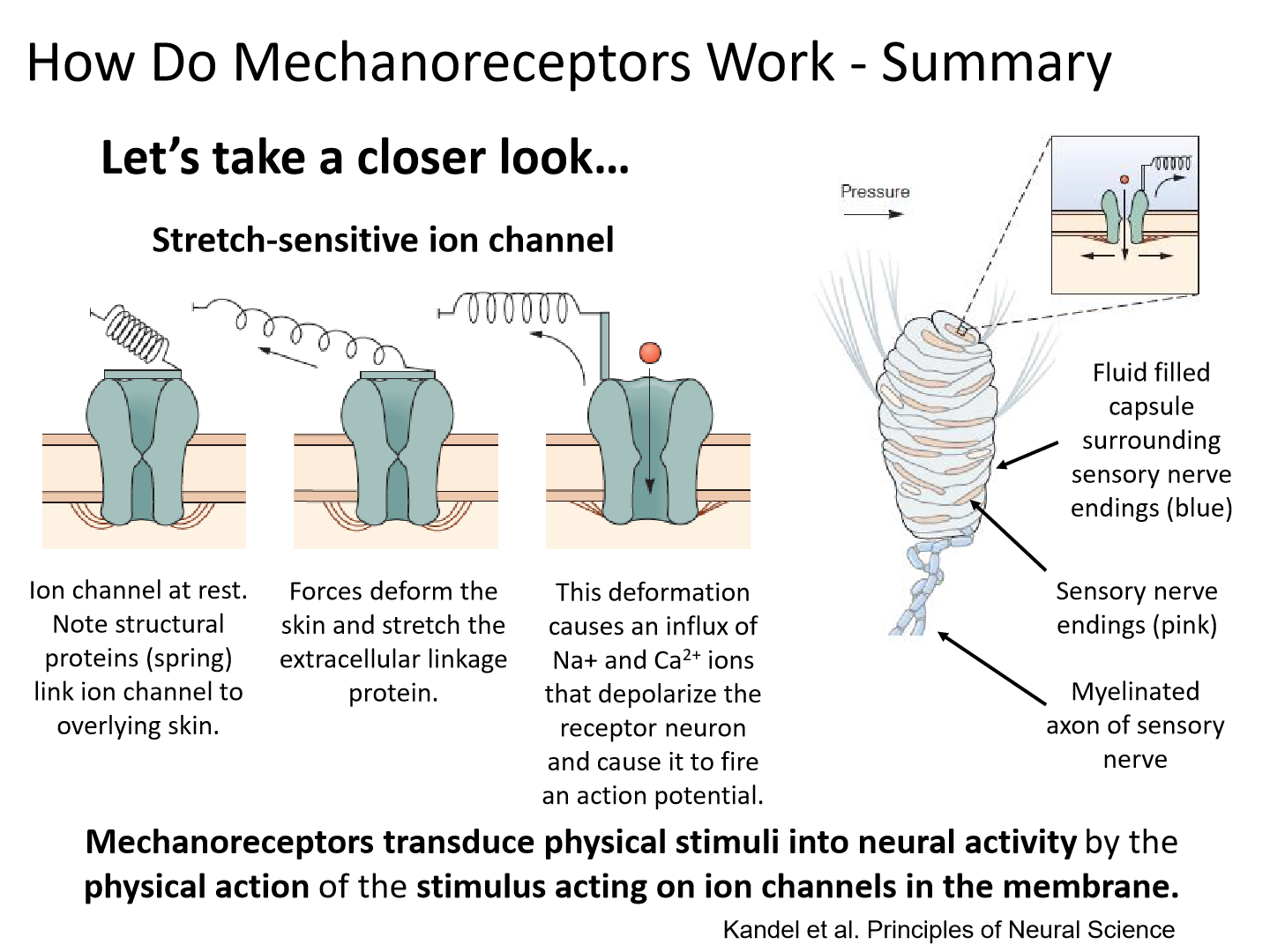
1. ion channel is at rest
2. forces deform the skin and stretch the extracellular linkage protein
3. this deformation causes an influx of Na+ and Ca2+ ions that depolarize the receptor neuron and cause it to fire an action potential
Which mechanoreceptor has the highest temporall resolution?
Pacinian corpuscles
- very small movements stimulate
- most sensitive
What is temporal sensitivity?
the speed of stimulus when it is applied or removed
Merkle discs (SA1) in braille experiment
they are the smallest receptors with the most branched innervation. They provide the most precise spatial information
What mechanoreceptor has the most precise spatial information?
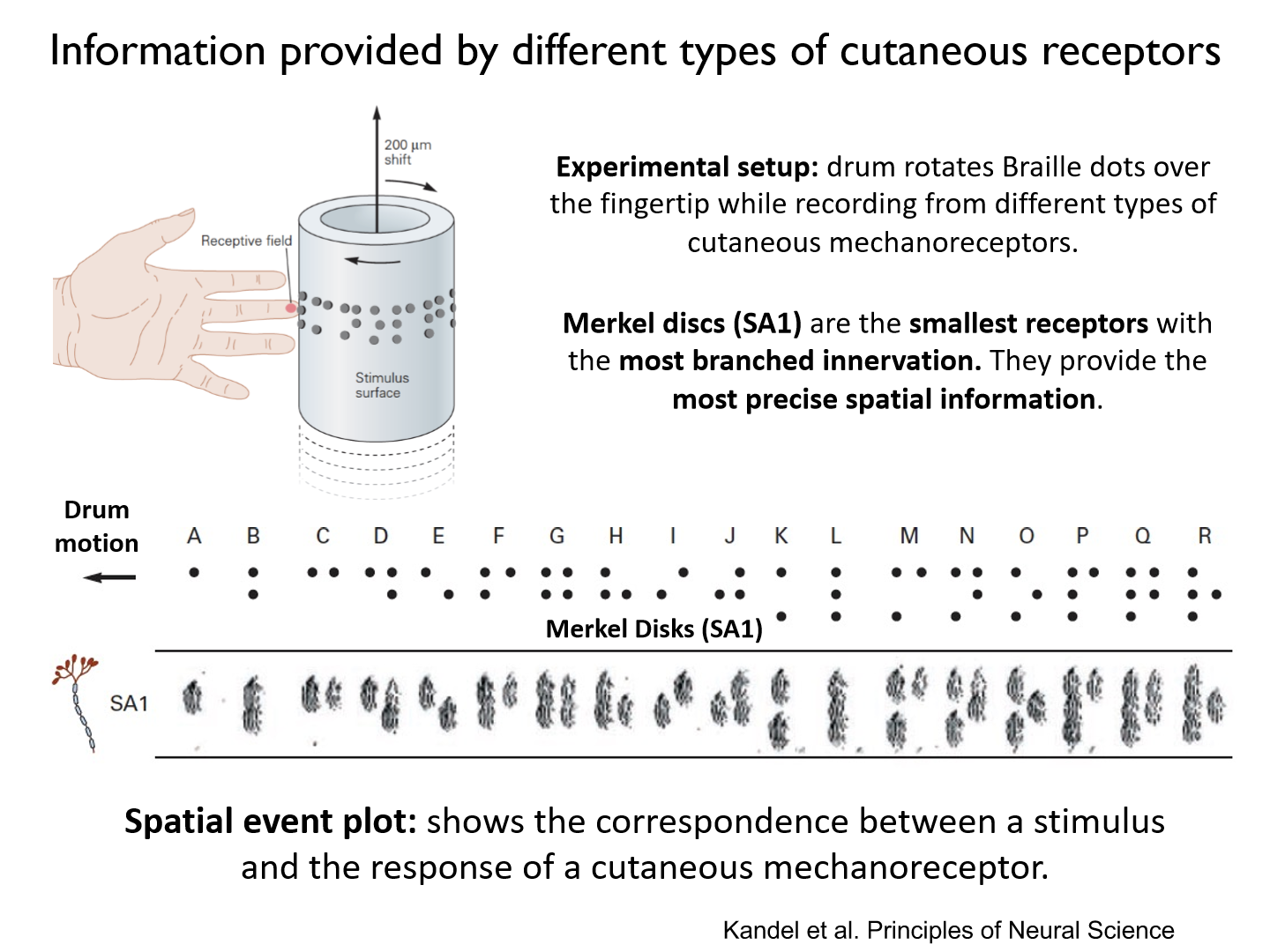
Merkel discs (SA1)
- discern between points
Spatial event plot
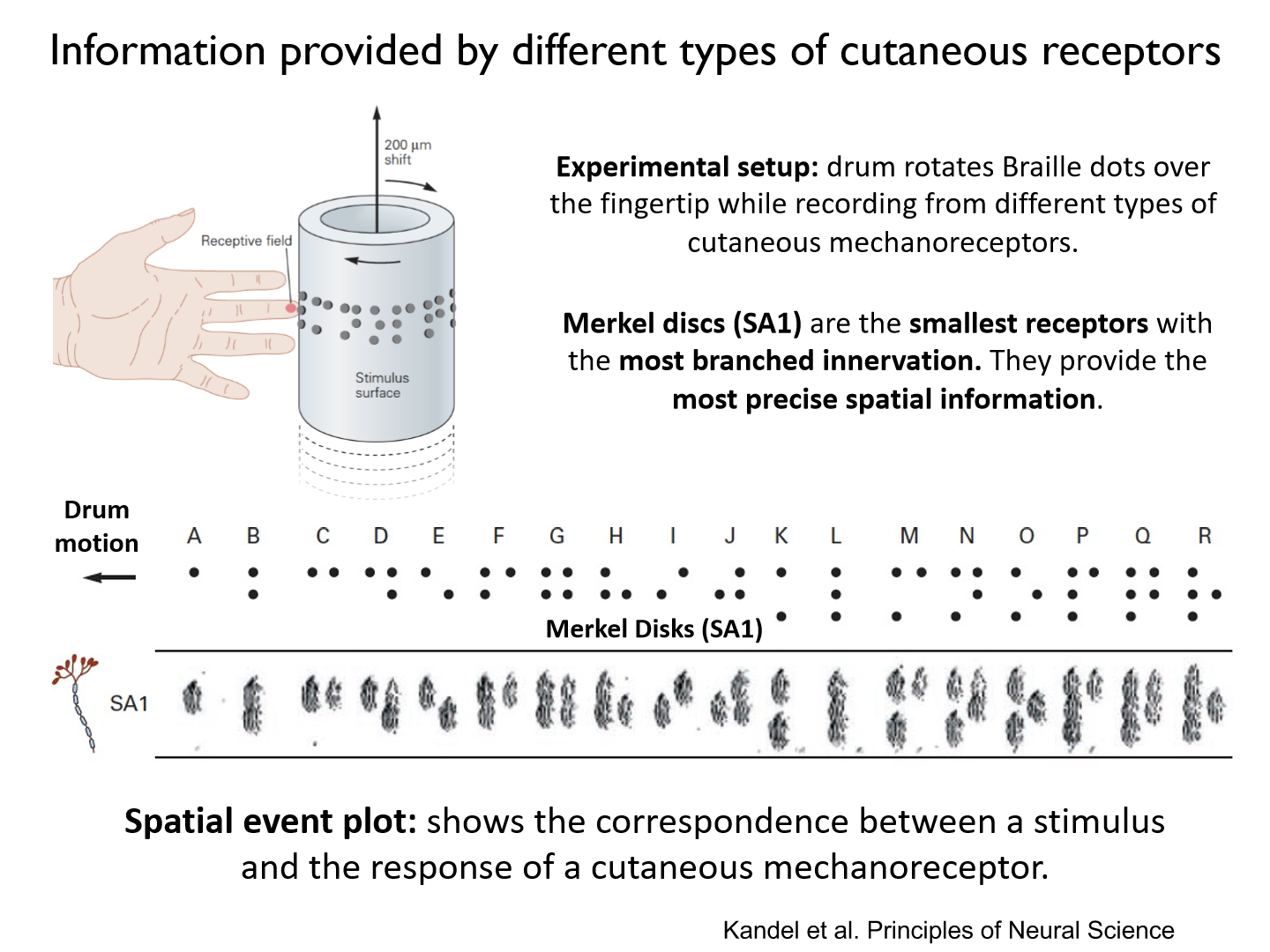
shows the correspondence between a stimulus and the response of a cutaneous mechanoreceptor
Meissner corpuscles (RA1) in braille experiment
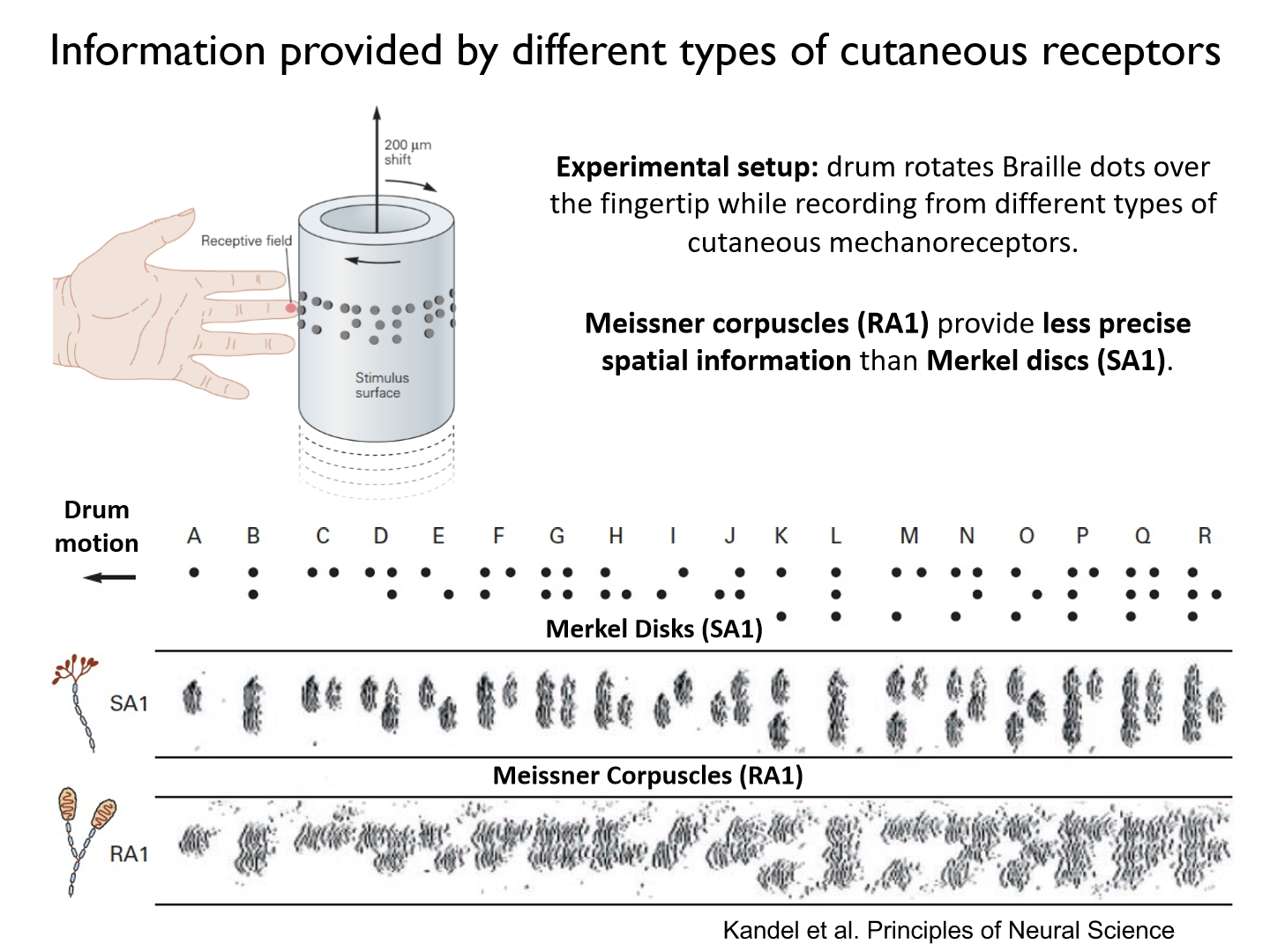
provide less precise spatial information than Merkel discs (SA1)
Ruffini and pacinian mechanoreceptors in braille experiment
the receptive fields of deep receptors are too large to provide precise spatial information
How do sensory neurons travel?
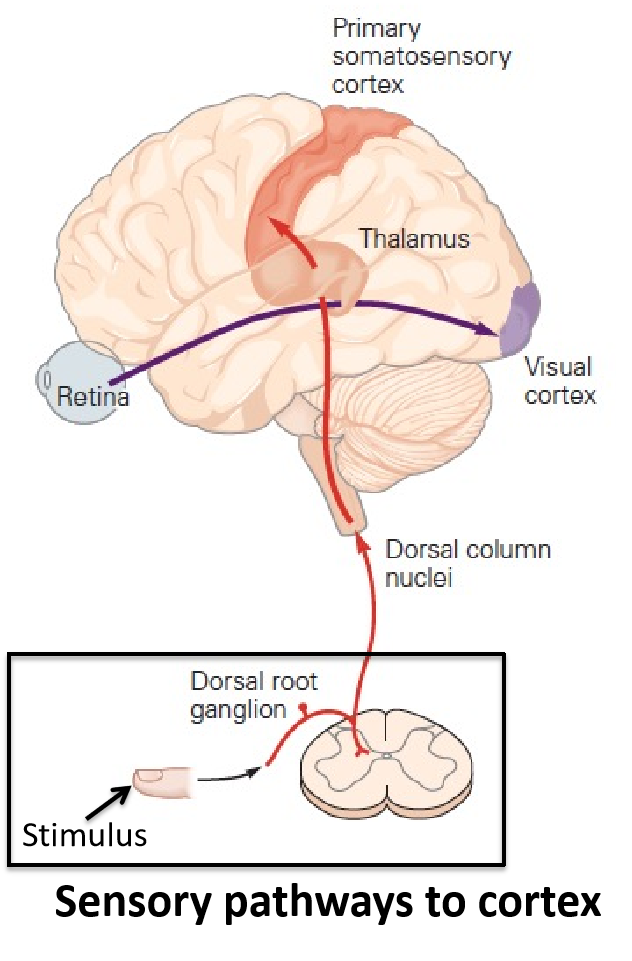
In bundles (peripheral nerves) to the horn of the spinal cord.
Where is sensory feedback from cutaneous mechanoreceptors processsed?
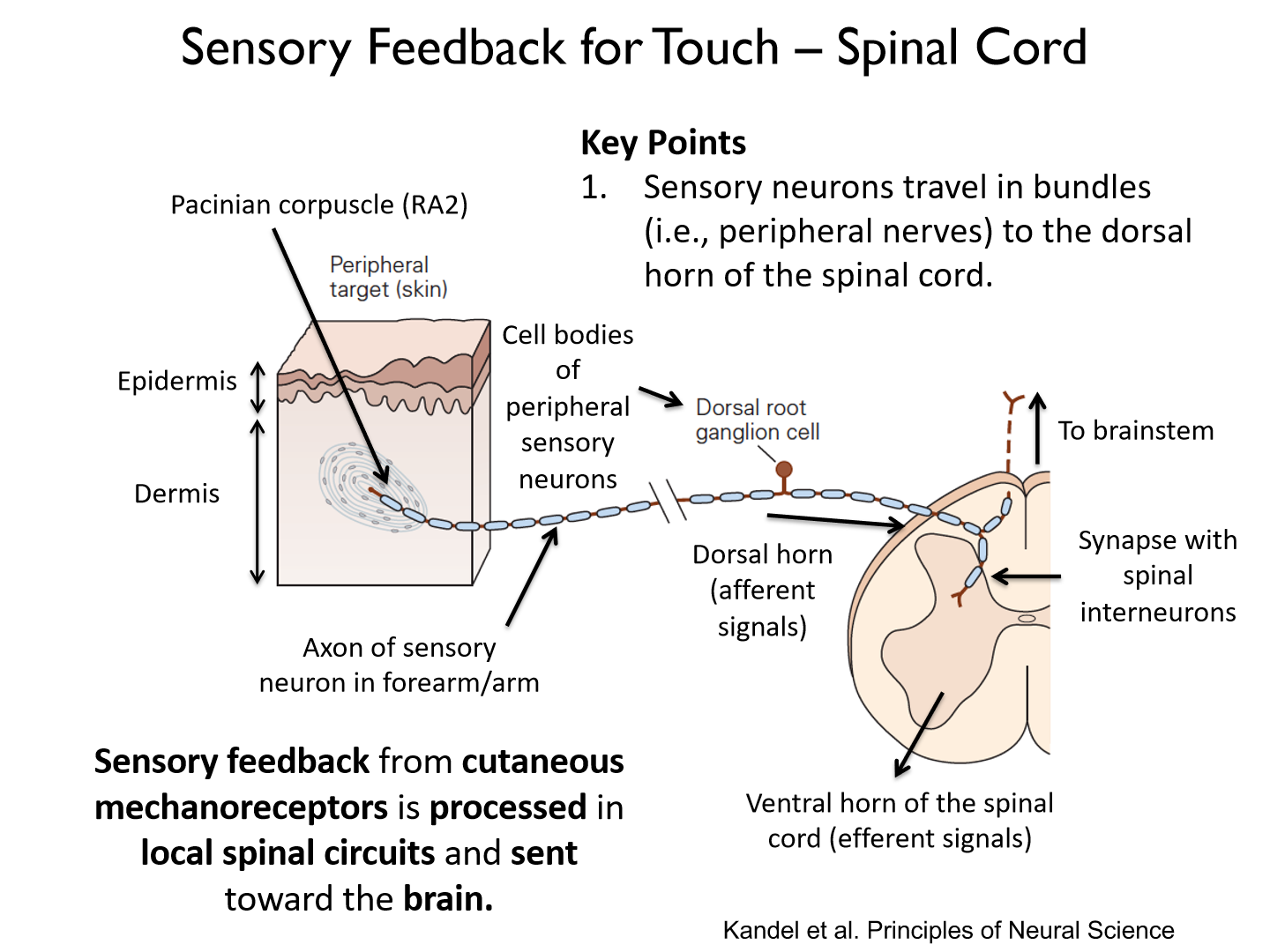
It is processed in local spinal circuits and sent toward the brain
- uses the DCML tract (dorsal column-medial lemniscus pathway)
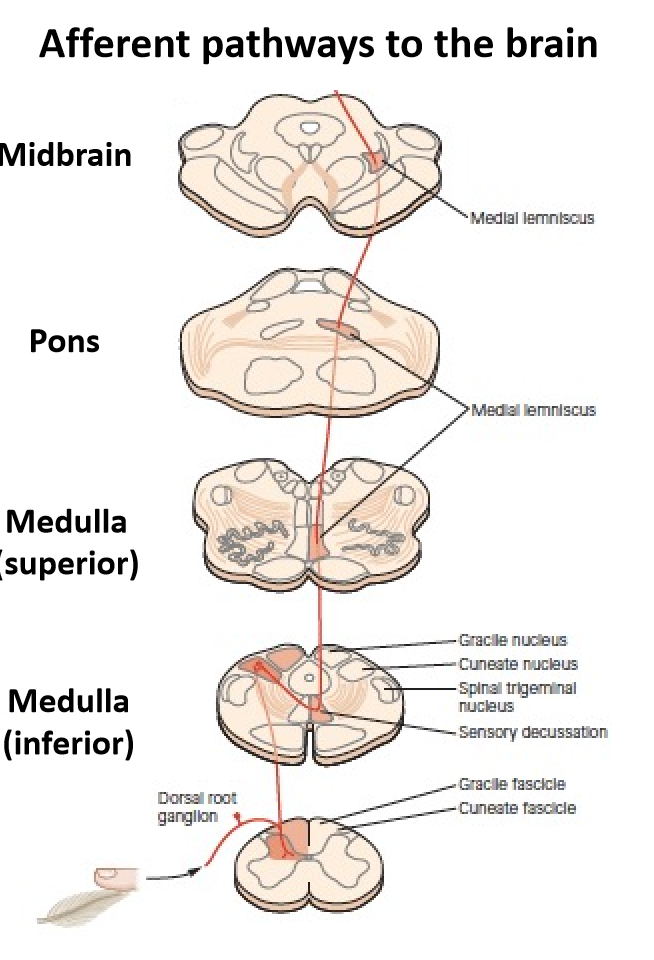
What are 2 ascending axons of the dorsal columns?
- Gracile fascicle
- Cuneate fascicle
Cuneate fascicle
carries sensory information from the upper body and trunk
Gracile fascicle
carries sensory information from the lower limbs and trunk
- what's touching grass
Where are motor neurons found?
in the ventral horn of the spinal cord
How does sensory information travel?
from the periphery to the brain in orderly tracts. (organized by structure)
Somatotopic organization of ascending tracts
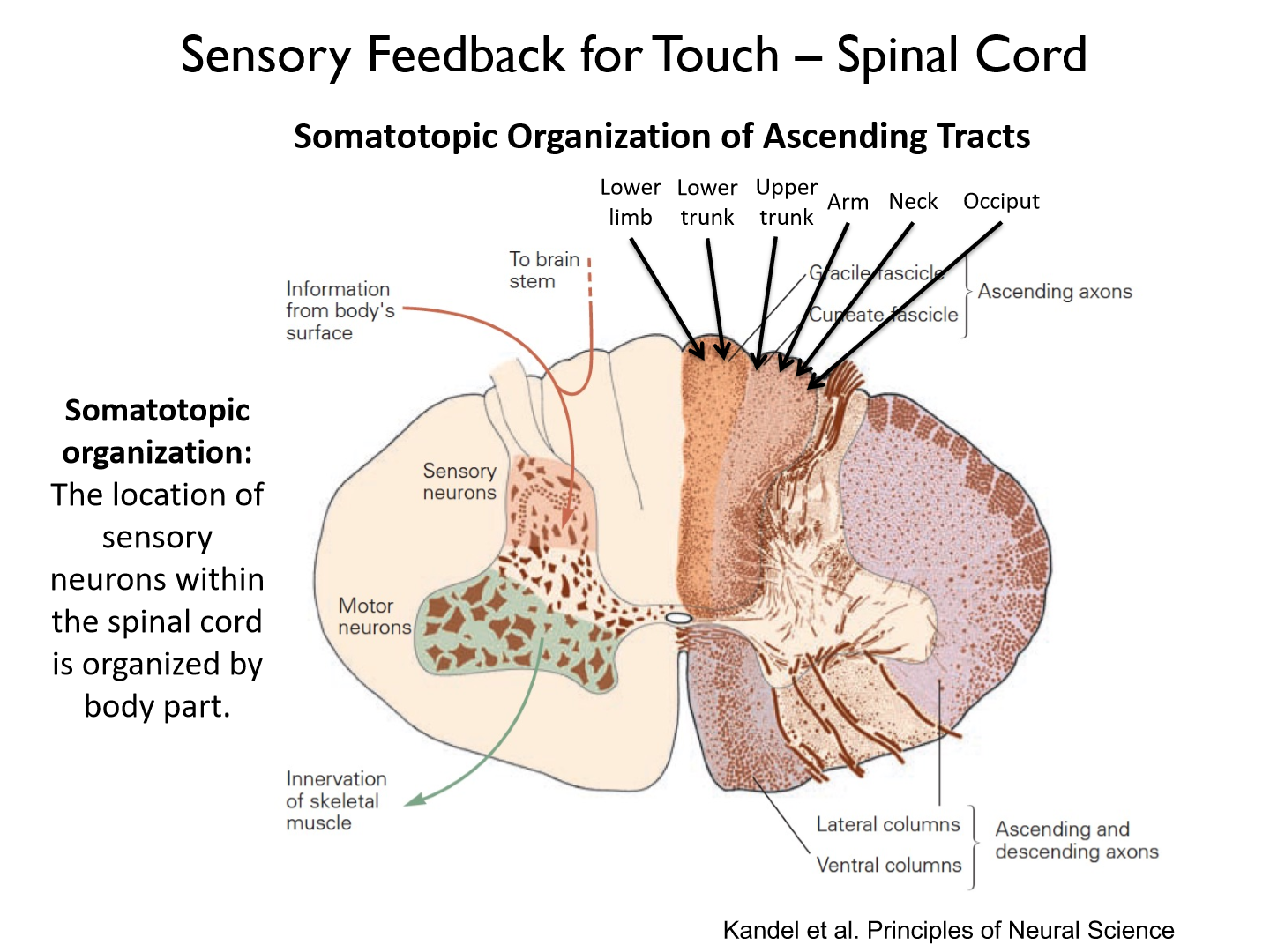
Medial
1. lower limb (G)
2. lower trunk (G)
3. upper trunk (C)
4. arm (C)
5. neck (C)
6. occiput (back of skull)
somatotopic organization
the location of sensory neurons within the spinal cord is organized by body part
What does the dorsal column consist of?
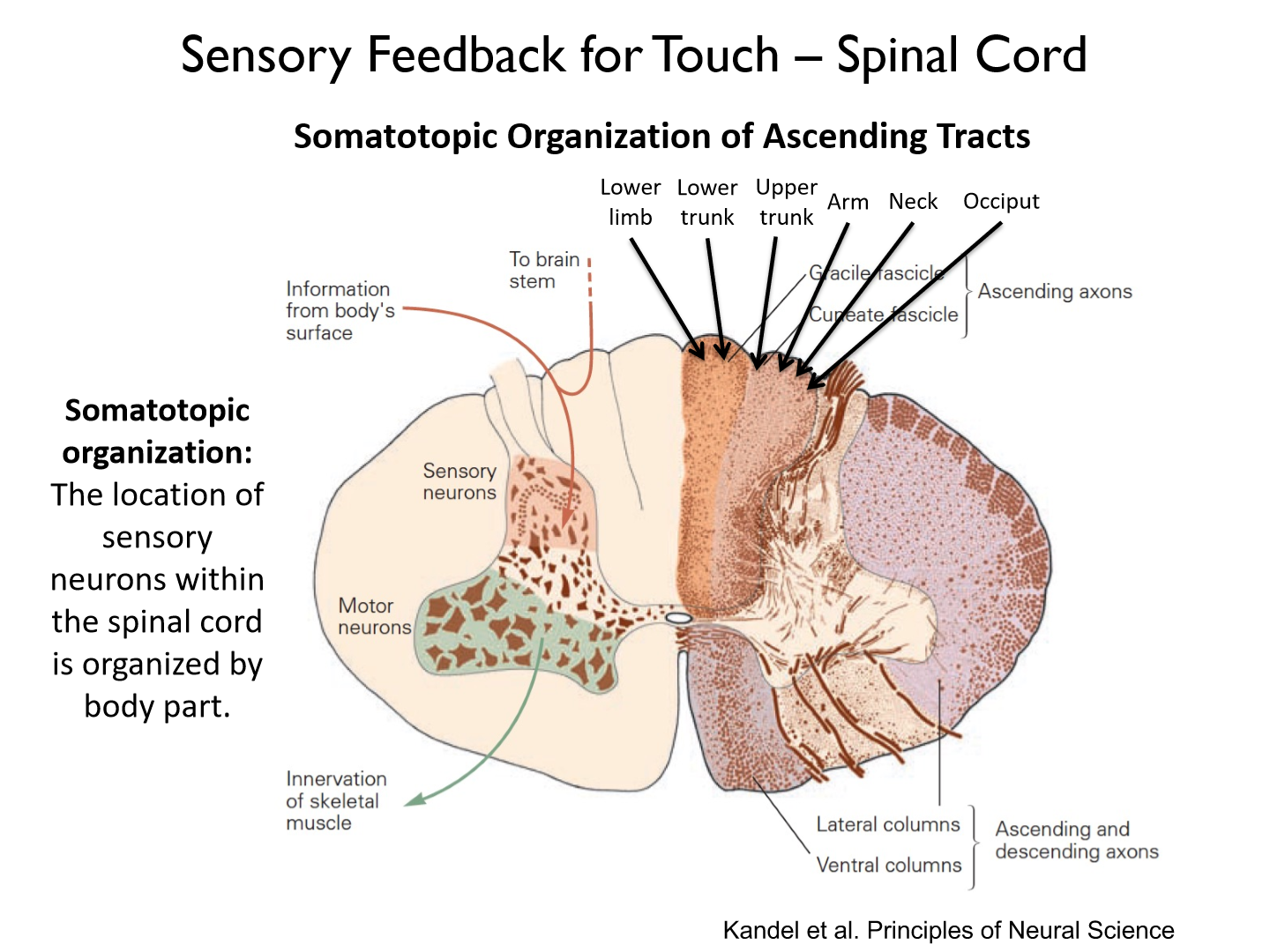
axons of sensory neurons that carry touch and proprioceptive information
Where does somatosensory information decussates?
the somatosensory information switches (decussates) from the ipsi-(same) to contralateral (opposite) side of the body in the medulla.
Where does sensory feedback travel up?
the medial lemniscus
What are the 3 key points of sensory feedback?
1. Somatosensory information travels up the dorsal columns in the gracile (lower limbs +trunk) or cuneate fascicle (upper limbs + trunk).
2. Somatosensory information switches (decussates) from the ipsi- (same) to contralateral (opposite) side of the body in the medulla.
3. Information travels up the medial lemniscus, synapsing in the thalamus and pass information to primary somatosensory cortex.
What are the 3 key points of sensory feedback for touch?
1. Sensory neurons travel in bundles (peripheral nerves) to the dorsal horn of the spinal cord.2. Dorsal column consists of the axons of sensory neurons that carry touch and proprioceptive information.3. Neurons in the medial lemniscus synapse onto neurons in the thalamus.
4. Thalamic neurons relay sensory information to primary somatosensory cortex via the posterior limb of the internal capsule.
What is the thalamus' role in sensory feedback?
it is a 'relay center' for somatosensory information from the periphery
What are the two portions of the thalamus in charge of somatosensory information?
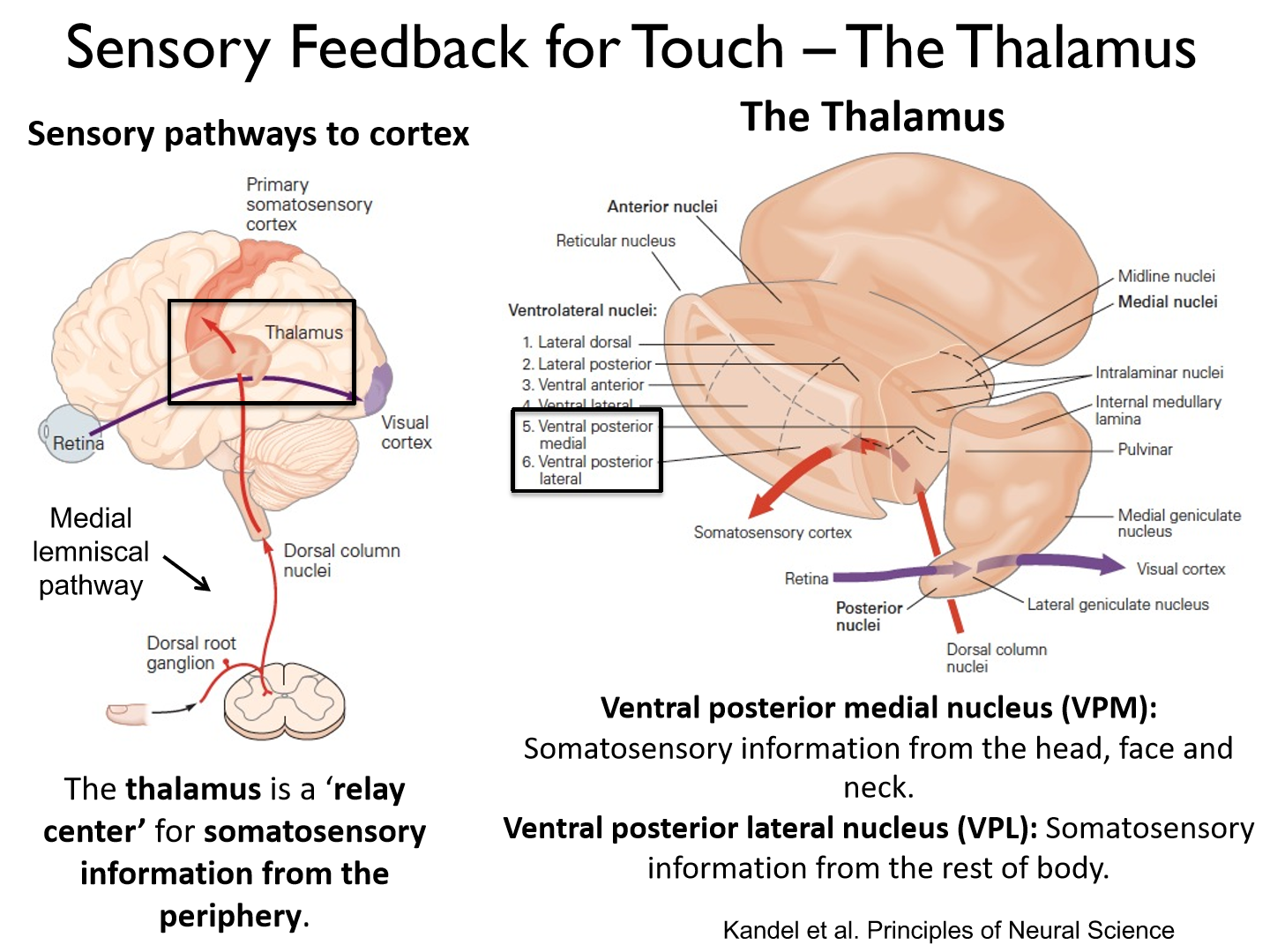
1. Ventral posterior medial nucleus (VPM): somatosensory information from the head, face and neck
2. Ventral posterior lateral nucleus (VPL): somatosensory information from the rest of the body
How do thalamic neurons relay sensory information to the primary somatosensory cortex?
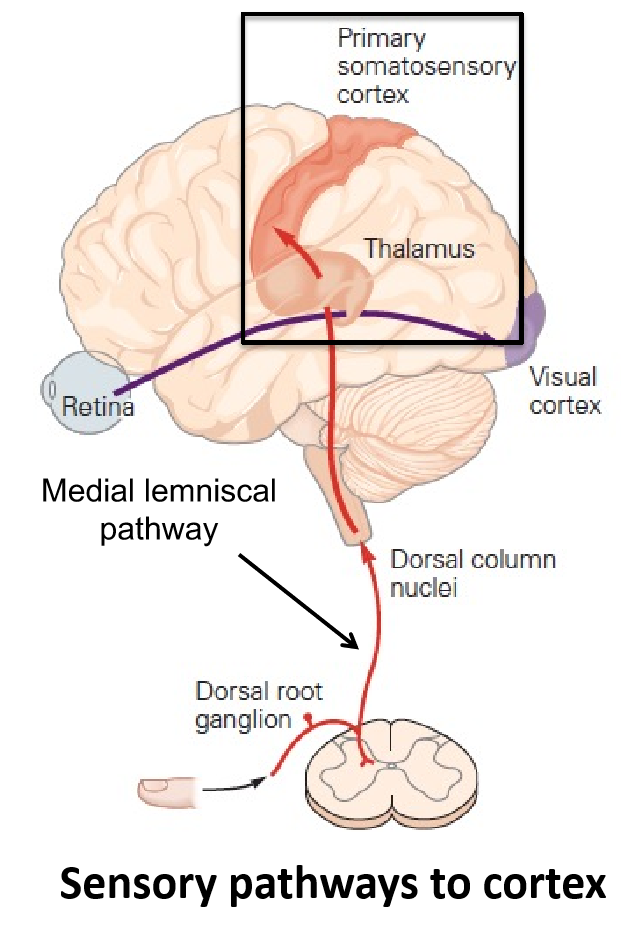
The posterior limb of the internal capsule.
*white matter
What is the internal capsule?
a white matter tract that carries information from the thalamus to primary sensory cortex
What are the 3 neurons between the periphery and cortex?
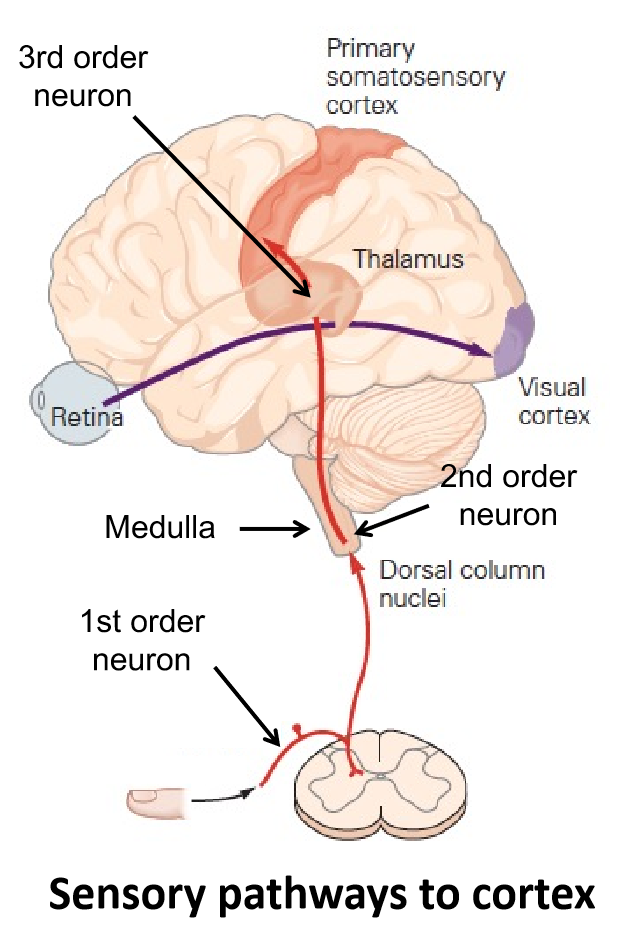
1. Somatosensory information travels up the posterior column in the gracile and cuneate fascicles.2. Somatosensory information switches from the ipsi- to contralateral side of the body (decussates) in the medulla.3. Neurons in the medial lemniscus synapse in the thalamus and pass information to primary somatosensory cortex.
The pathway from the periphery to primary somatosensory cortex is called the:
dorsal column-medial lemniscal pathway (DCML)
How is the primary somatosensory cortex organized?
its is organized (roughly) by body part (homunculus or map)
- larger representation of areas that are more sensitive to sensory stimuli (hands, feet, face, lips)
4 main divisions of primary somatosensory cortex (S1)
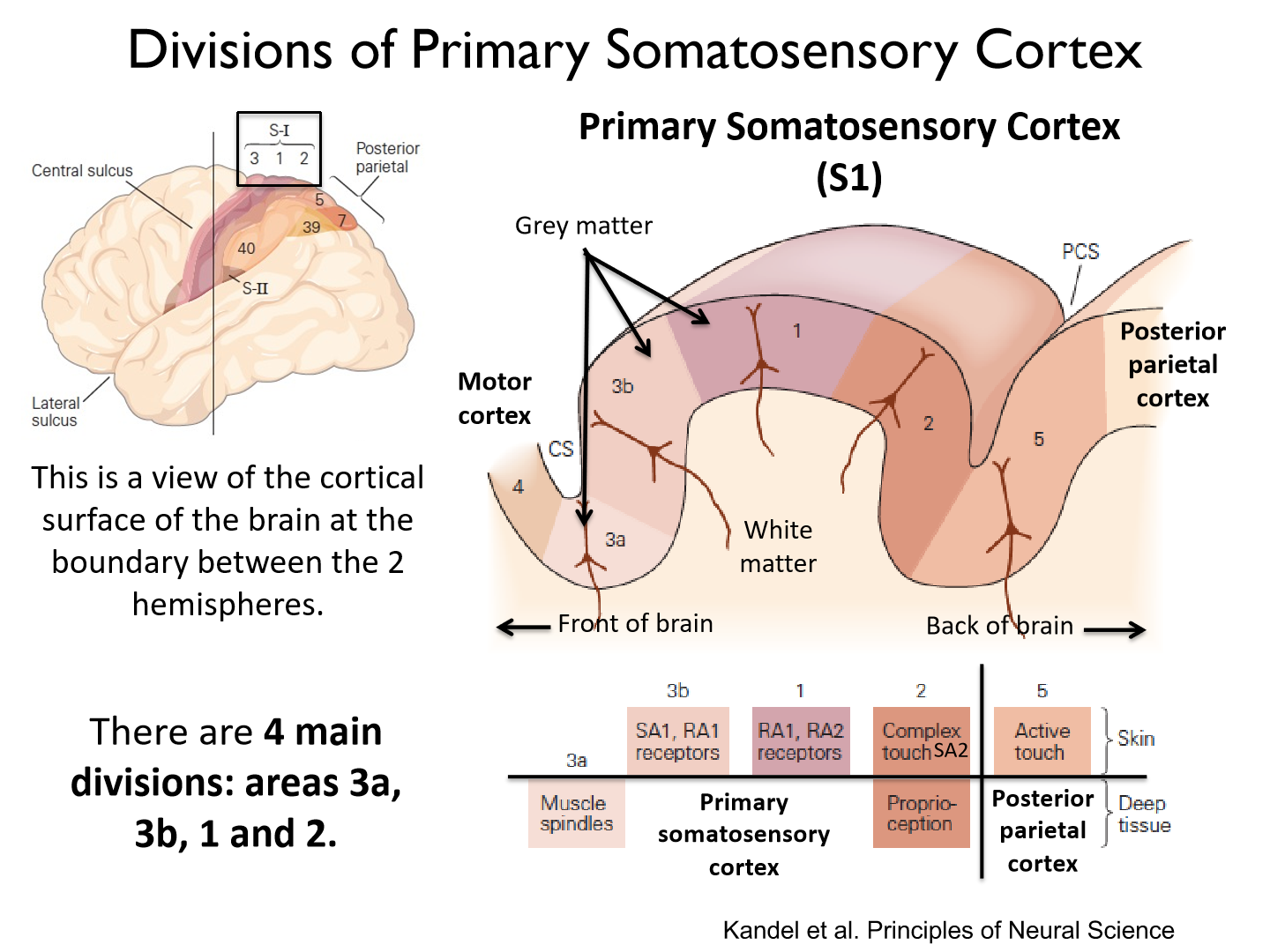
3a, 3b, 1 and 2
*each area receives different types of somatosensory feedback from the periphery
What somatosensory feedback does each division receive?
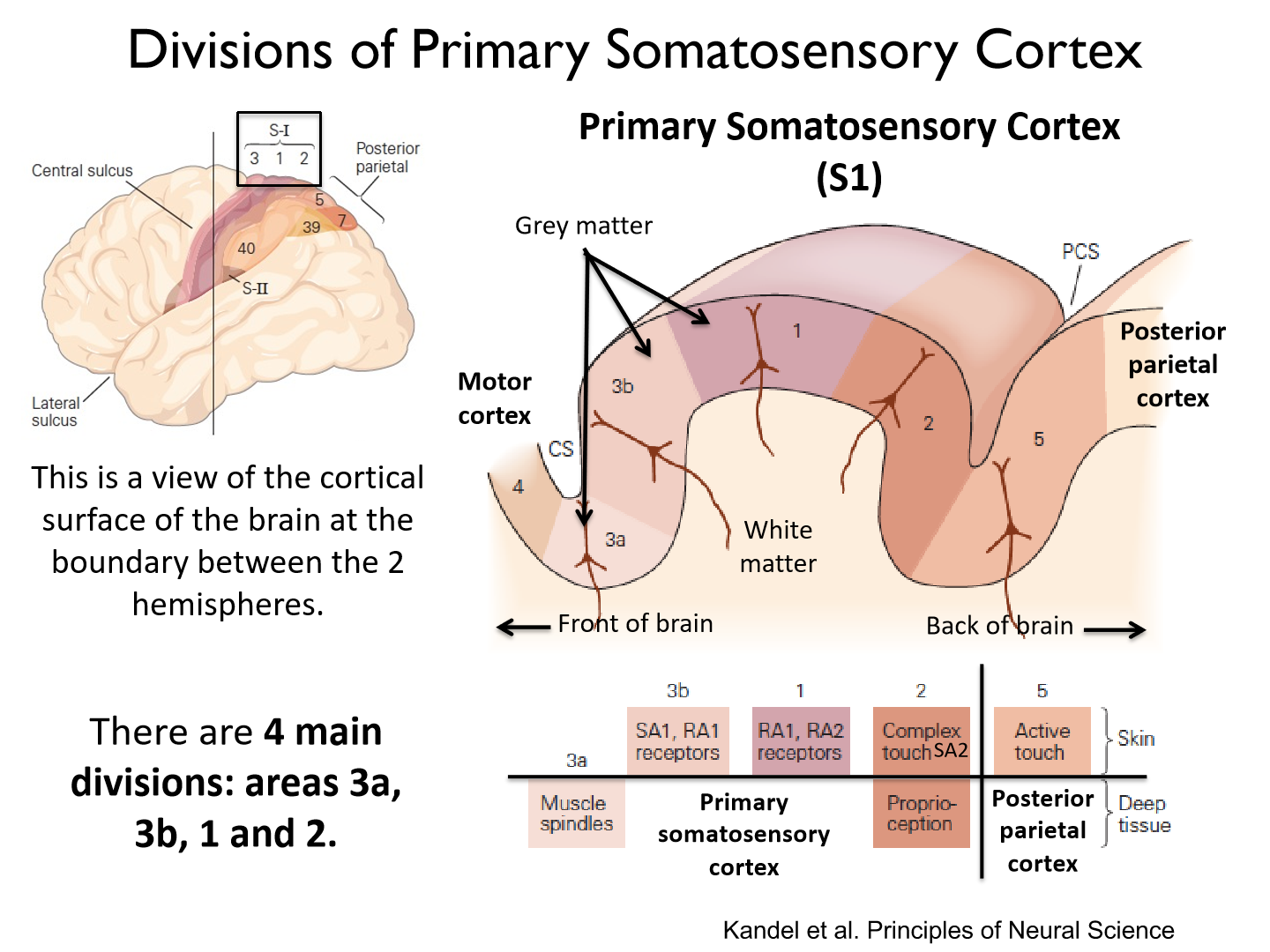
3a: muscle spindles (deep tissue)
3b: SA1, RA1 (skin)
1: RA1, RA2 (skin)
2: Complex touch SA2 (skin), Proprioception (deep tissue)
Posterior parietal cortex:
5: Active touch (skin)
Draw the box diagram showing flow of tactile feedback in S1
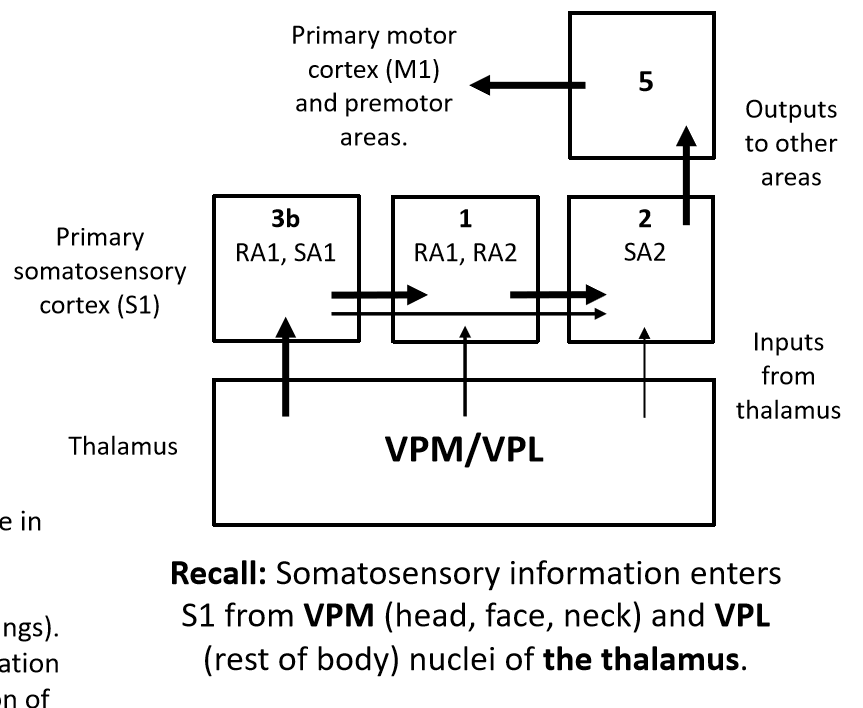
*internal capsule to relay from VPM/VPL to 3b
*arrow thickness=extent of connections
Area 3b
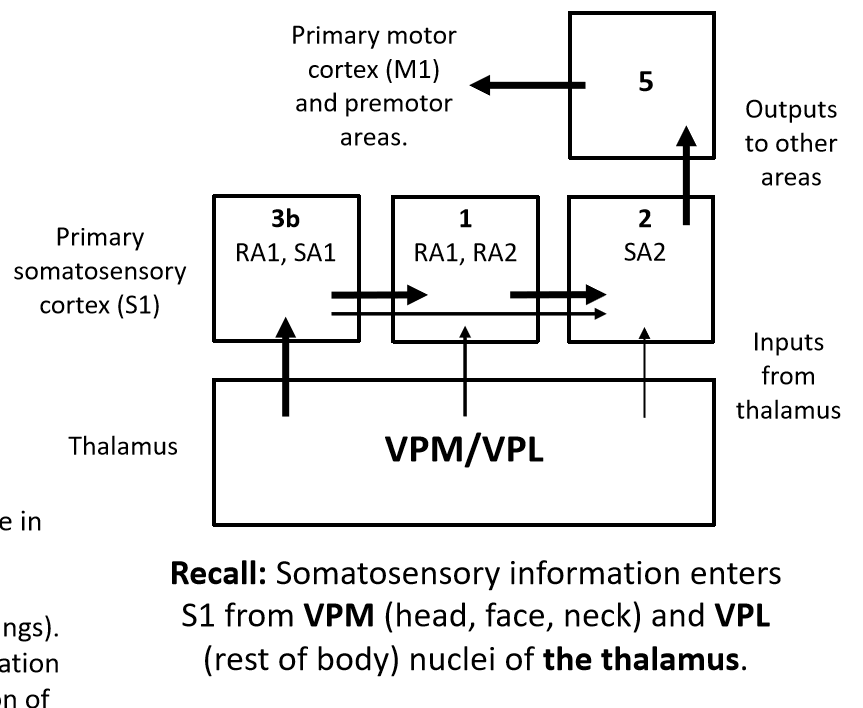
Receives input from SA (Merkel disc) and RA1 (Meissner corpuscle). Detects force (SA1), location of stimulus (SA1 & RA1) and change in force (RA1).
*force, location, change in force
Area 1
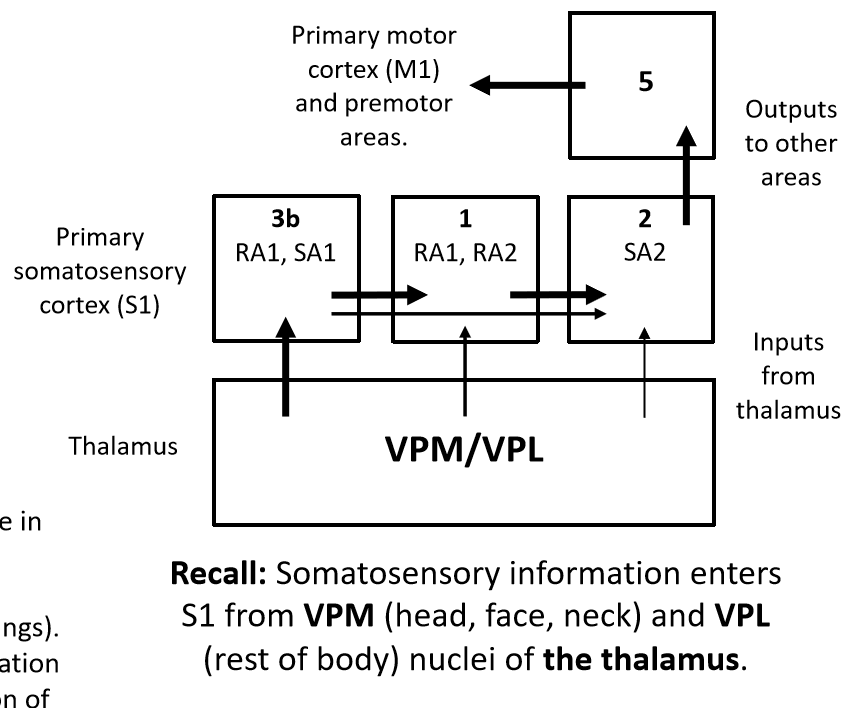
Receives input from RA1 and RA2 (Pacinian corpuscle) receptors. Detects change in force (RA1) and stimulus motion (RA2).
Area 2
Receives input from SA2 (Ruffini endings). Detects stretch caused by self motion. Integration with info from areas 3b & 1 allows separation of self vs. stimulus motion.
Tactile Acuity Experiment
- Small forces are applied to the fingertip with one or two small, rounded stimuli.
- The accuracy of the participant’s responses (i.e., % correct) at each inter- stimulus distance provides information about the tactile acuity of different regions of the body
Summary of Experiment1. Vary the distance between stimuli or orientation of stimuli.2. Ask subjects to make perceptual judgments – one point or two (horizontal or vertical in orientation version)
Results of the tactile acuity experiment and merkel discs (SA1)
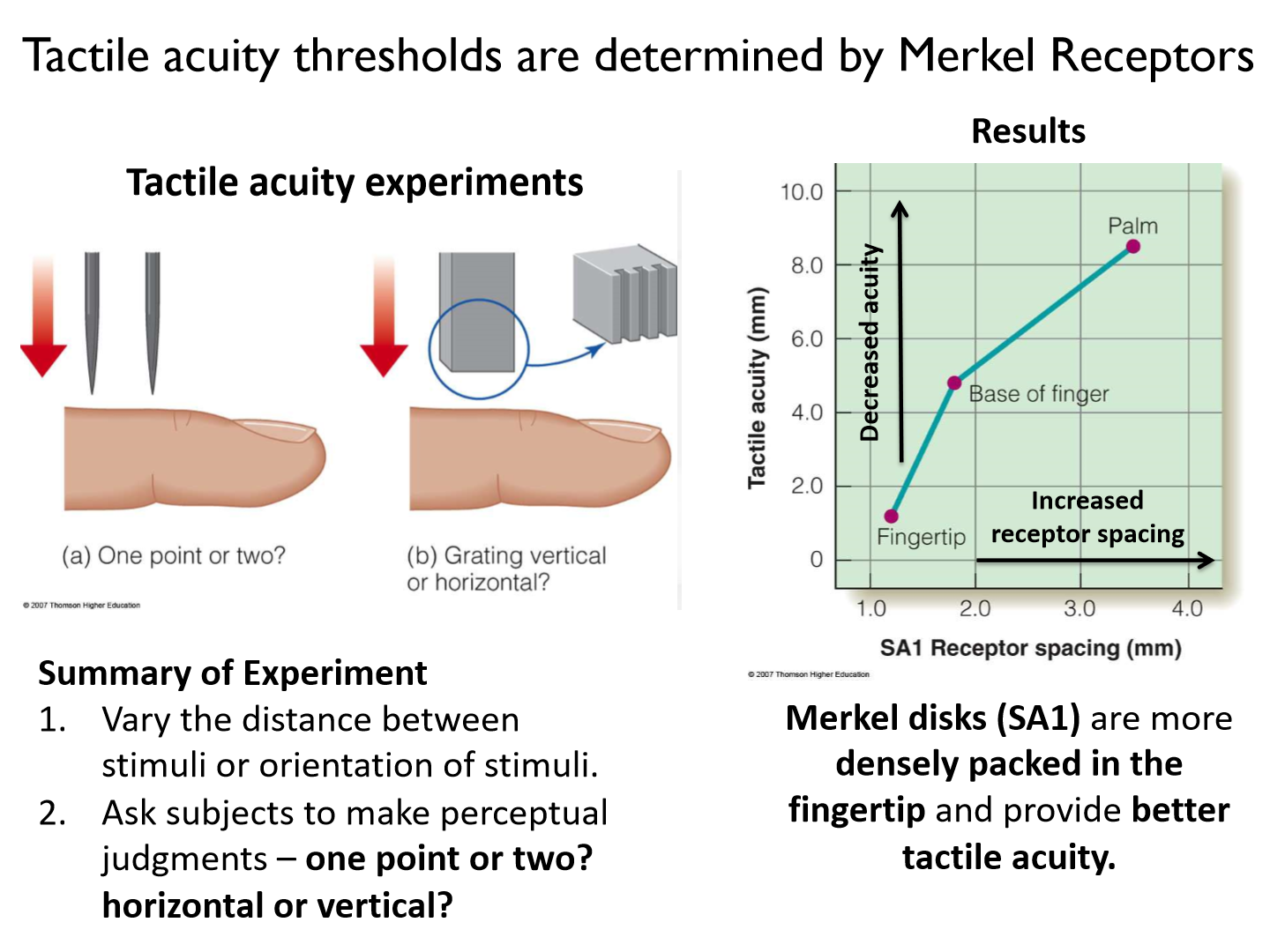
SA1s are more densely packed in the fingertip and provide better tactile acuity
Is there a different amount of Merkel receptors across fingers?

No! Tactile acuity decreases from the tip of the index to pinky fingers, but the density of Merkel receptors is roughly constant across fingers.
Why does tactile acuity decrease from the tip of the index to pinky fingers, but the density of Merkel receptors is roughly constant across fingers?
- Larger representation of the index finger in S1, suggesting that in addition to the density of Merkel discs, the representation of the fingers in S1 is a limiting factor in tactile acuity.- But there is a larger representation of the index finger in S1. S1, not the Merkel receptors, seem to be the limiting factor in tactile acuity.
Corticosensory
Brain and physical receptor
Is tactile acuity similar between hands?
yes!
Central plasticity
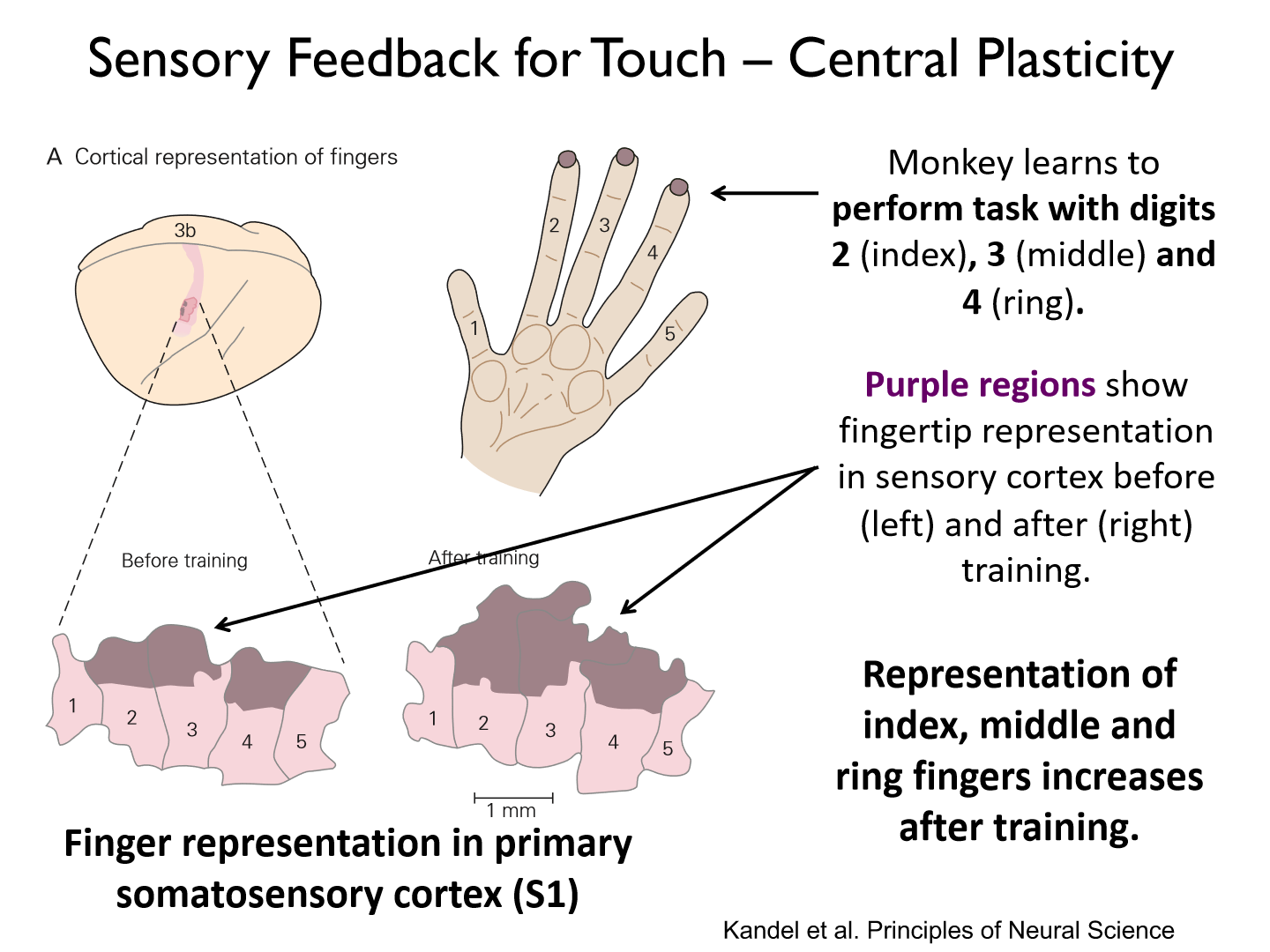
You can perform task to increase representation of digits in the somatosensory cortex
When does tactile acuity peak?
It peaks in early adulthood (1mm) and declines in older adults (>2mm by 60-70yrs old)
What part of the hand has the highest spatial acuity?
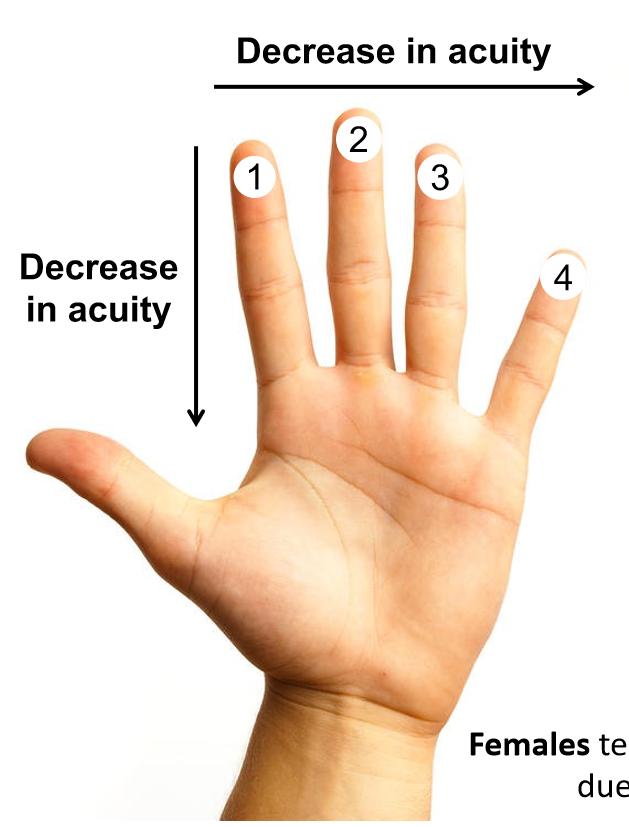
The distal pad of index finger
Where does spatial acuity decline across the hand?
• Spatial acuity declines progressively from the index topinky finger (50% reduction)• Spatial acuity declines rapidly from distal to proximal finger pads (60-80% reduction in palm)
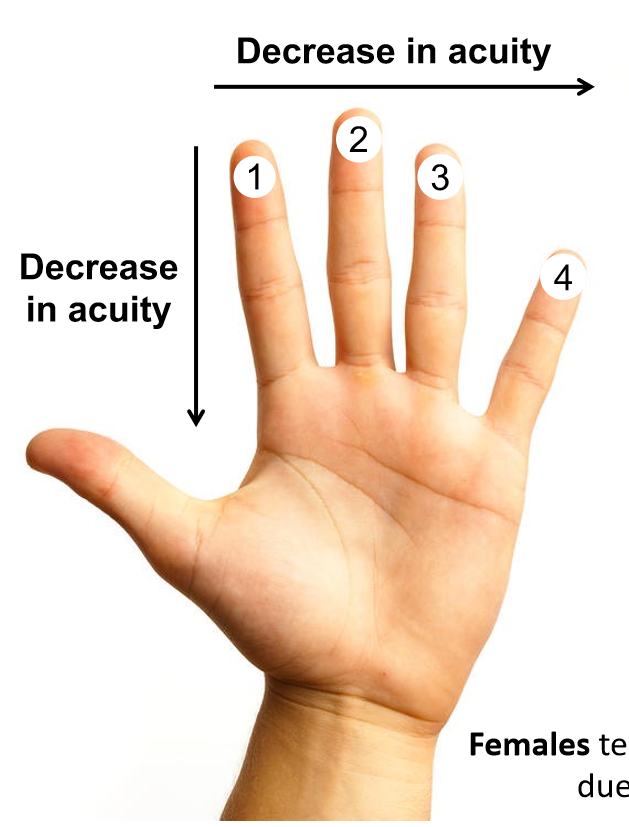
Do males or females tend to have better tactile acuity?
- Females tend to have better tactile acuity than males due to smaller finger size (on average).- The number of Merkel discs is ~constant across people, so smaller fingers tend to have a higher density of Merkel discs (better acuity).
How is proprioception carried?
dorsal route --> caudal medulla --> thalamus
*from GTO, vestibular, cutaneous, muscle spindles (MOST important)
Guillain-Barré Syndrome
an autoimmune disorder that attacks healthy peripheral nerves – typically after a virus or bacterial infection (note – deafferentation is uncommon).
Patient GL: Deafferentation (what we observe)
- caused by demyelination of large diameter peripheral nerves responsible for touch and proprioception.
- Diagnostic tests using needle EMG indicate motor neurons were unaffected (i.e., muscle function is normal)
Most common cause of deafferentation
Most common form is acute inflammatory demyelinating polyneuropathy (AIDP). It affects 1 in 100,000/year in North America.
Problems that arise from deafferentation
- Damage to myelin sheath causes improper transmission of sensory (and/or motor) signals.- Reduction in density of myelinated fibers (<1/2 normal values), particularly large diameter fibers (0.31% vs. 18% in healthy).
**No cutaneous, muscle or deep tendon reflexes. No cortical response following electrical stimulation of peripheral nerves.
Intact vs. destroyed proprioceptive system with reaching task
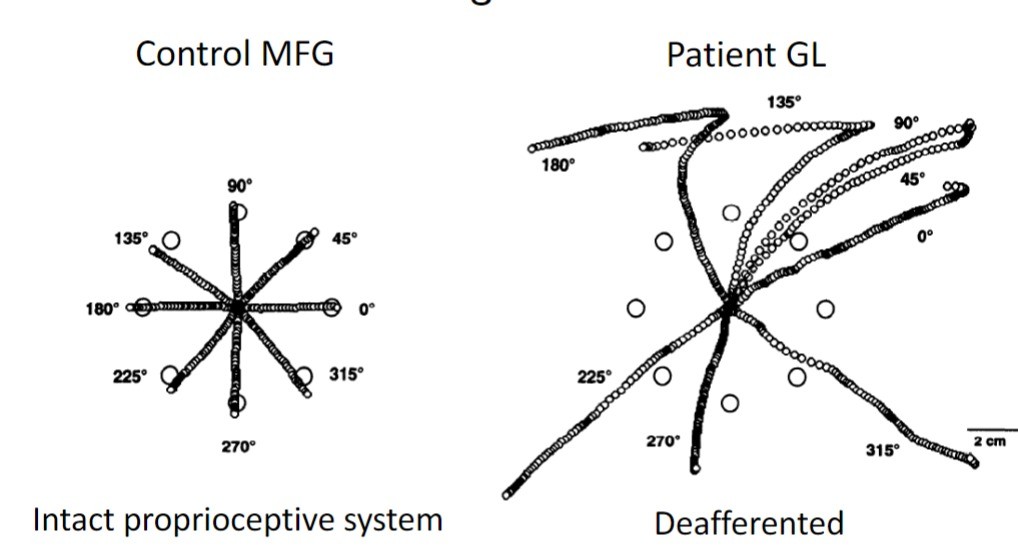
- Healthy people tend to make smooth, accurate and roughly straight reaching movements.
- Without vision, Patient GL makes inaccurate, jerky movements with large errors. (miss targets, slower)
Ian Waterman
Ian Waterman: had a sudden and complete deafferentation (loss of sensation) from the neck down at 19 years old.
1. Without skin, muscle and joint afferents, Waterman loses all sense of position and motion of body segments (i.e., proprioception) below the level of his neck (cranial nerves unaffected).2. In the absence of visual feedback, he could not sit upright for longer than 2s without falling over.3. He developed compensatory strategies to overcome proprioceptive loss. The strategies rely heavily on vision and ’freezing’ muscles (i.e., maintaining contraction) to maintain body postures when visual information is not available.
*use more energy for daily activity
*jerky gait (changes in EMG)
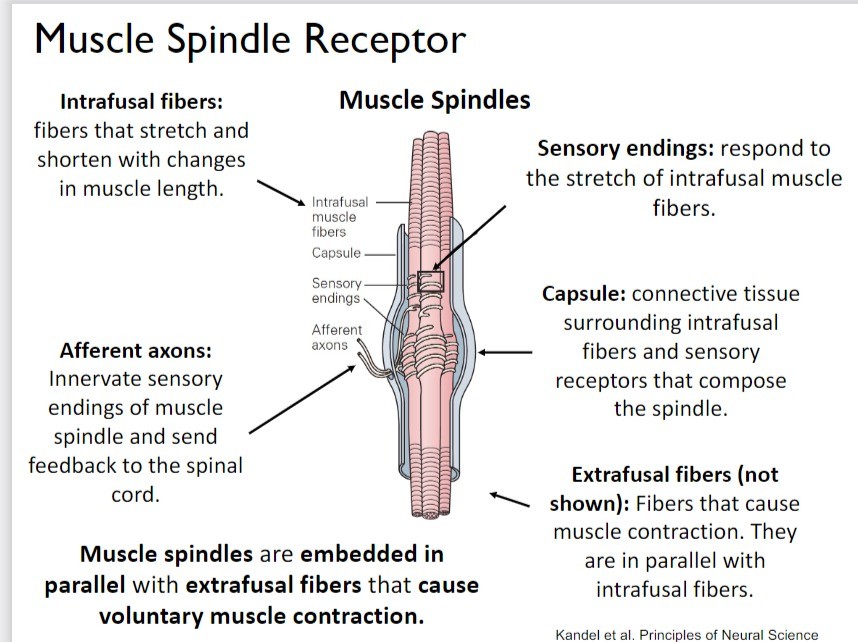
Muscle spindle sensitivity
Muscle spindles are sensitive to the amount and rate of muscle stretch.
1. Bag: rate of change in muscle length
2. Chain: sustained/length of muscle
*imbedded in intrafusal fibres
Intrafusal fibres
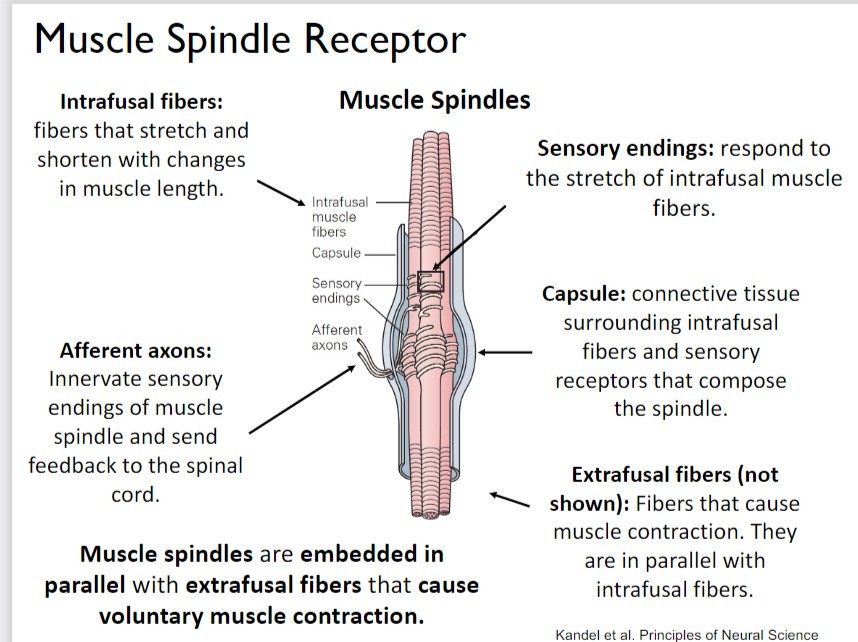
fibers that stretch and shorten with changes in muscle length. (contain muscle spindles)
*produce NO force
Afferent axons
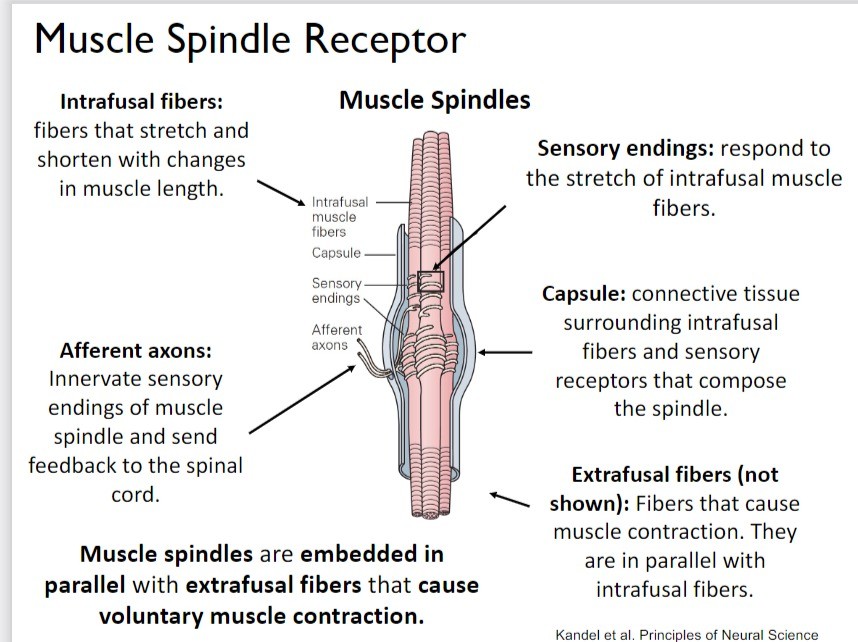
Innervate sensory endings of muscle spindle and send feedback to the spinal cord.
- primary = annulo spiral = everything
- secondary = flower spray = chain fibers
Sensory endings
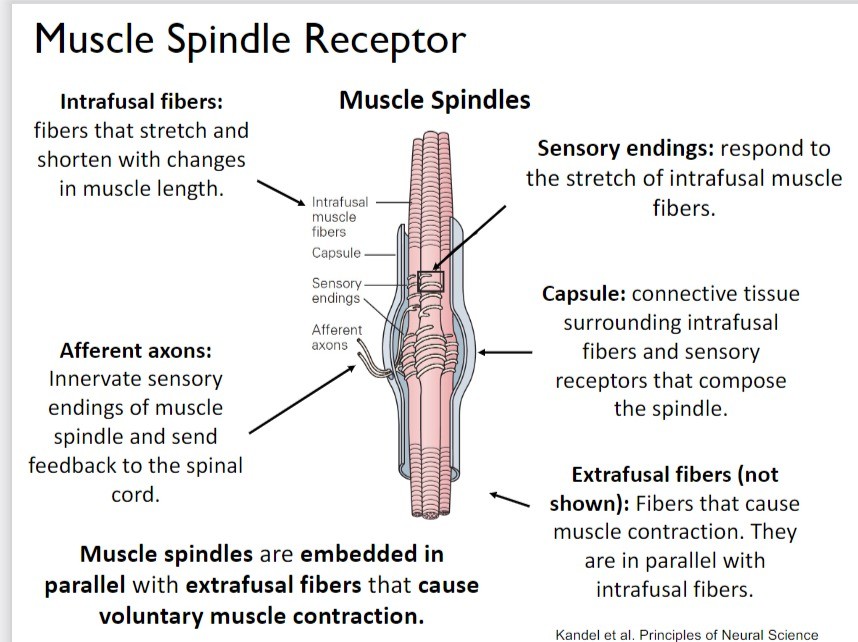
respond to the stretch of intrafusal muscle fibers.
Capsule
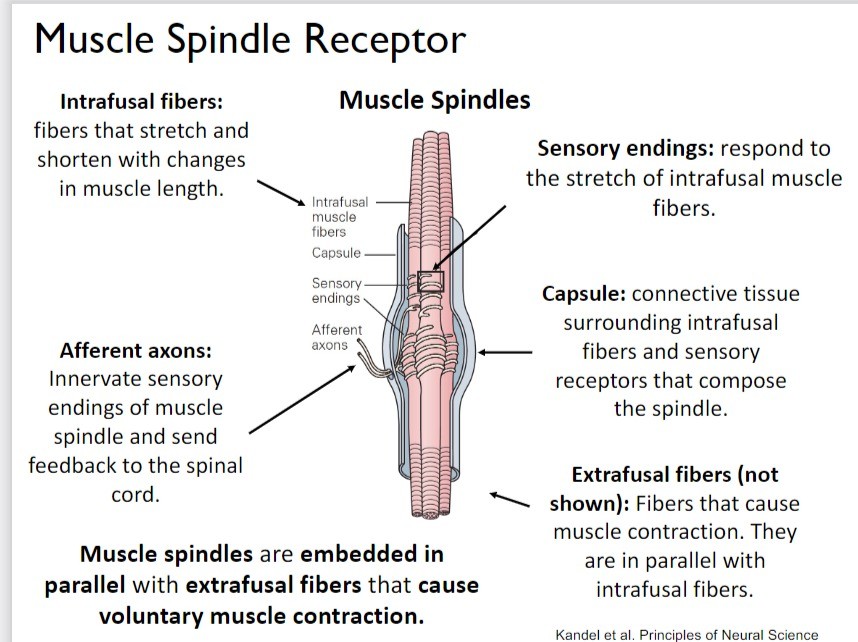
connective tissue surrounding intrafusal fibers and sensory receptors that compose the spindle.
Extrafusal fibers (not shown)
Fibers that cause muscle contraction. They are in parallel with intrafusal fibers.
*produce force!
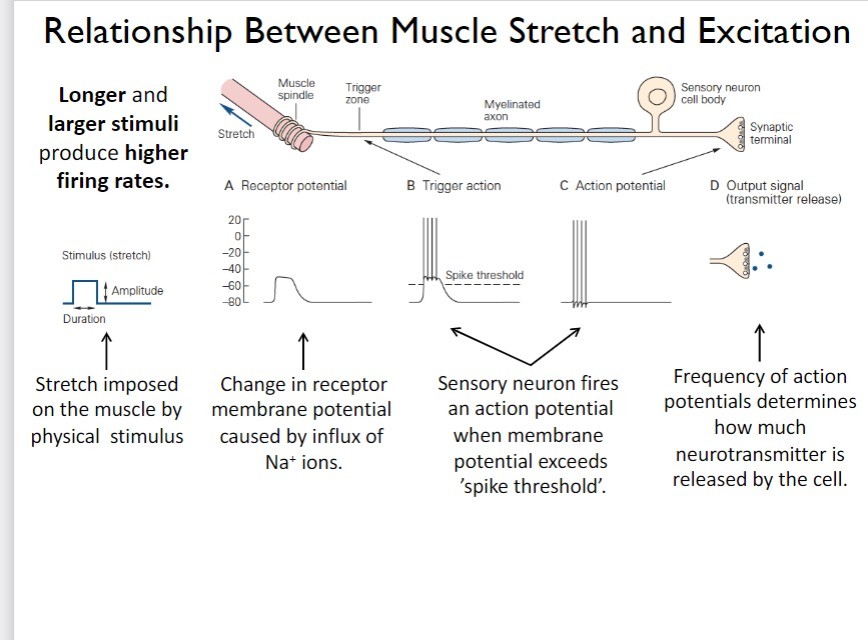
What happens when a muscle stretches?
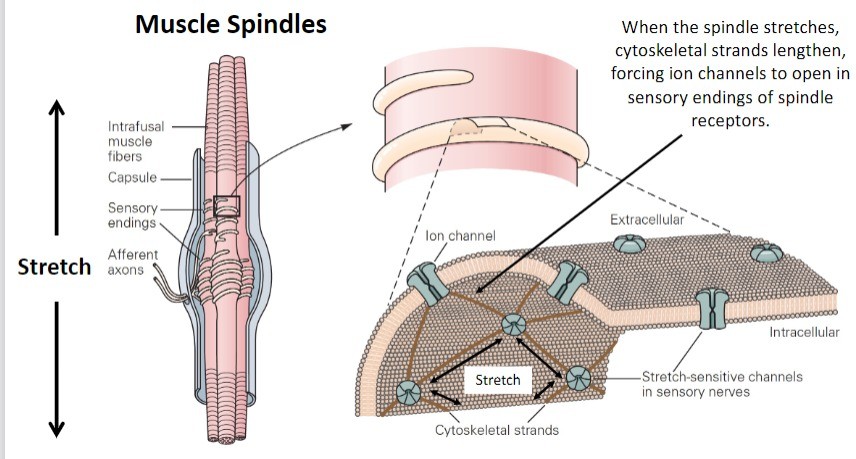
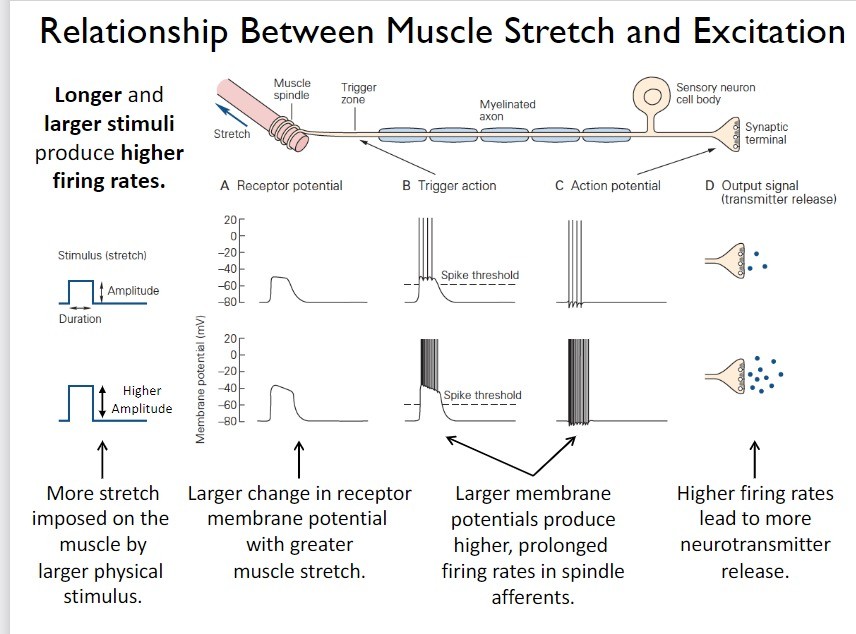
Muscle stretch deforms and opens stretch-sensitive ion channels. The influx of ions depolarizes the spindle receptor and causes it to fire action potentials.
**When the spindle stretches, cytoskeletal strands lengthen, forcing ion channels to open in sensory endings of spindle receptors.
*Na+
What portion of the muscle contracts?
The ends of the muscle
- middle portion is stationary
Do muscle spindles stop firing APs when relaxed?
No!
When the muscle is relaxed (i.e., rest/not contracted), muscle spindles maintain a low baseline (i.e., tonic) firing rate.
What do muscle spindle firing patterns look like at rest?
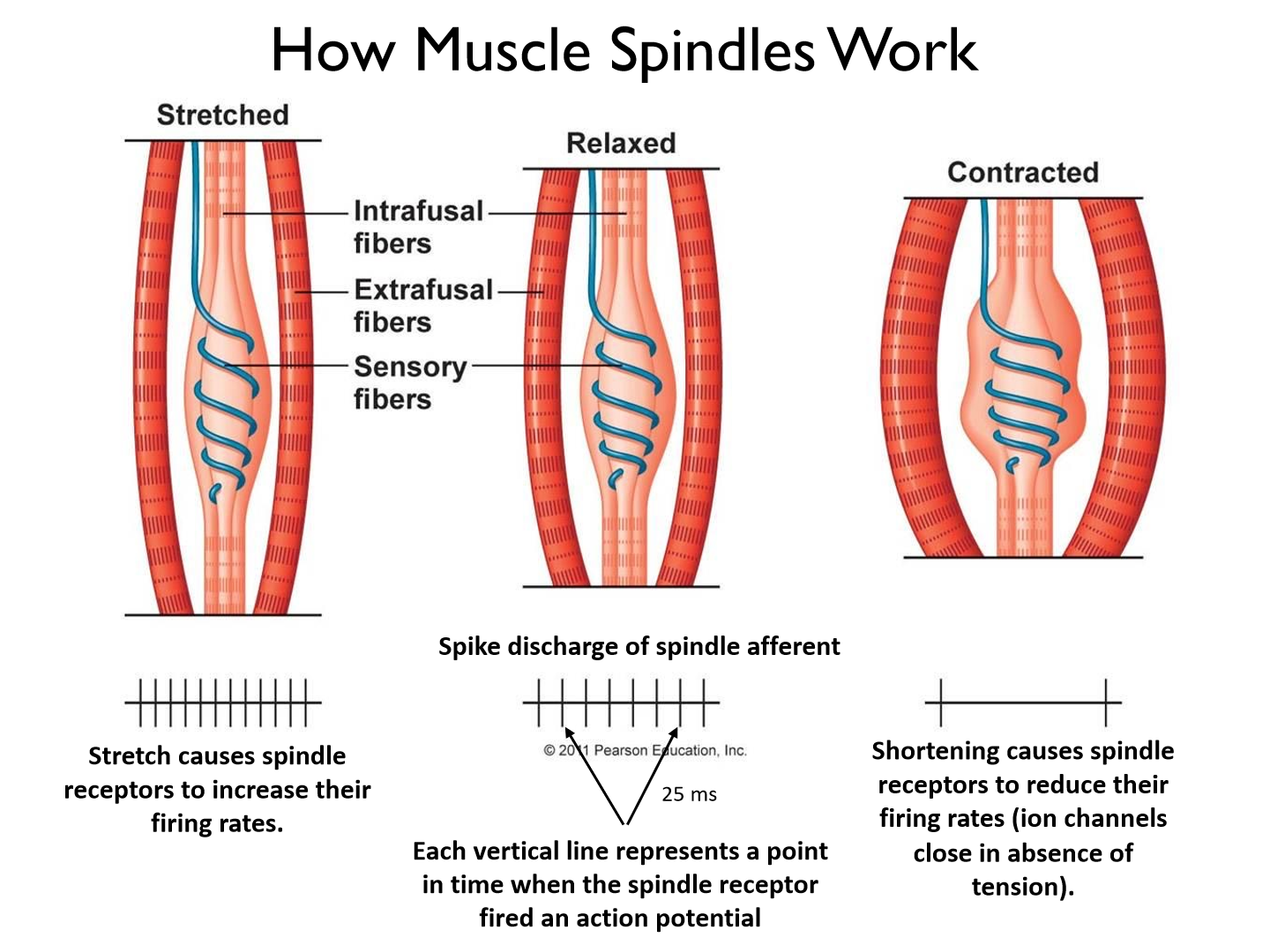
Muscle spindles have regular firing patterns
– the amount of time between action potentials is relatively constant.
*1a, type 2 = flower spray
What happens to the muscle spindle firing when the muscle stretches?
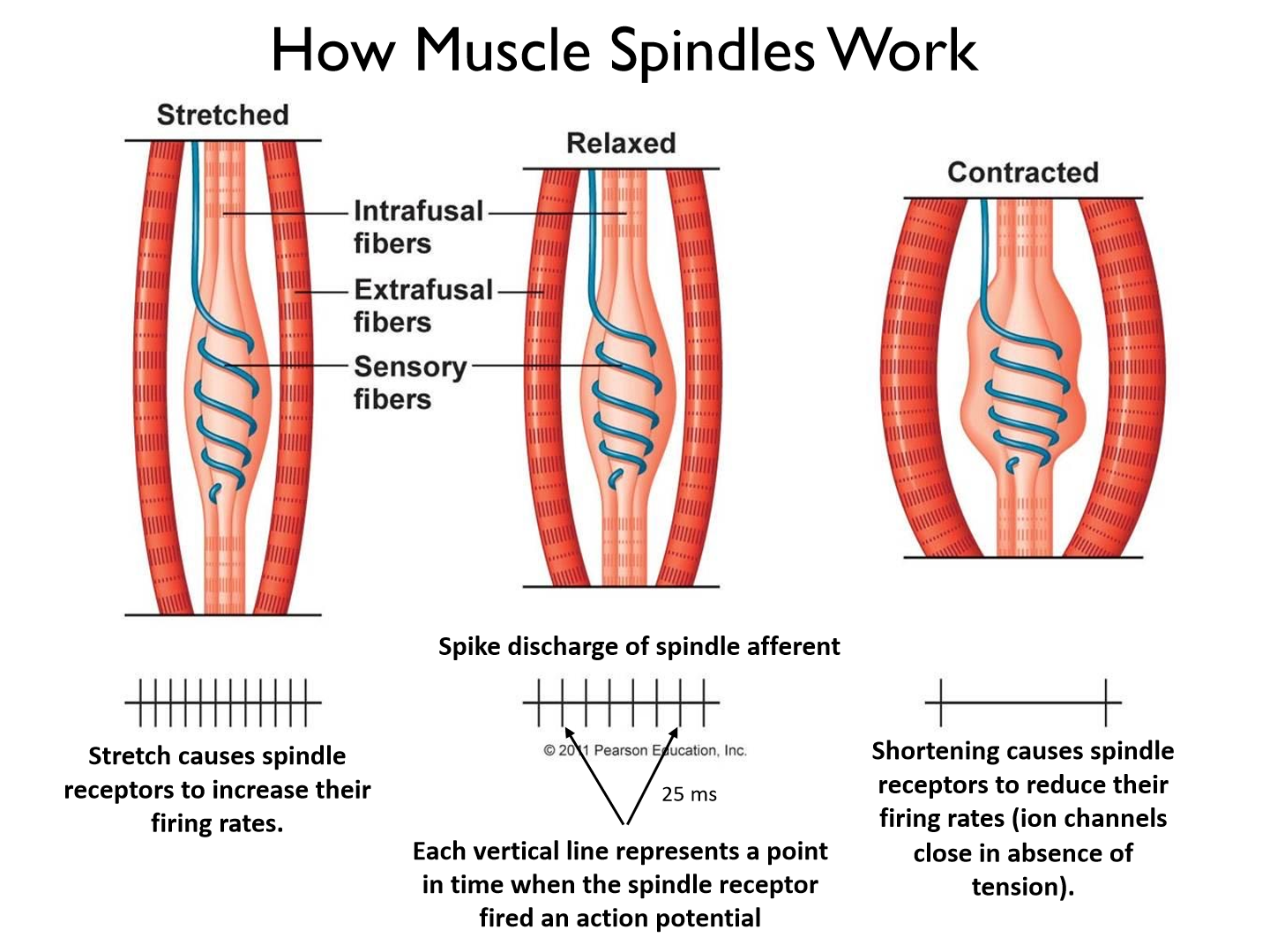
Muscle stretch causes spindle receptors to increase their firing rates.
What happens to the muscle spindle firing when the muscle contracts??
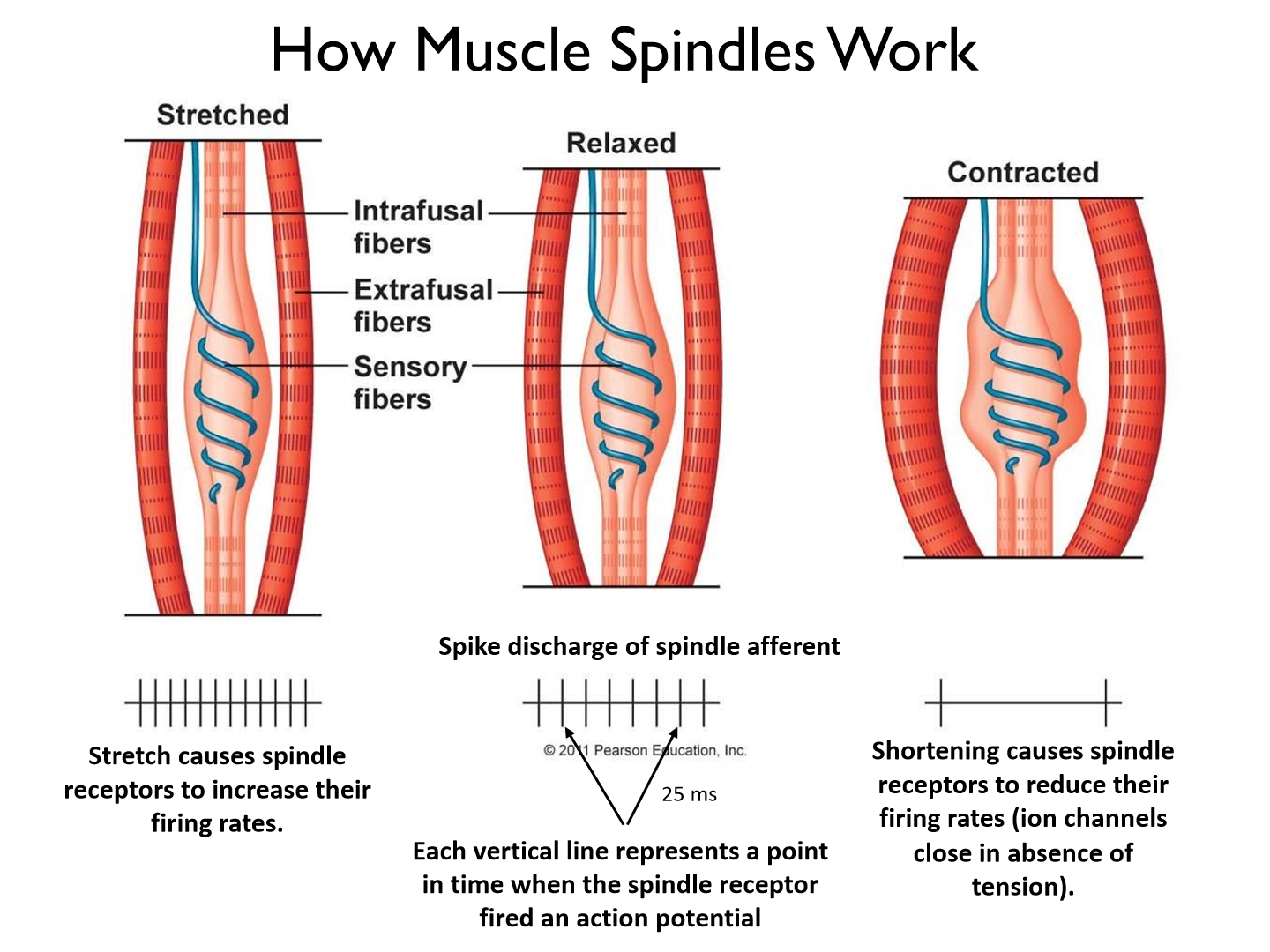
Muscle shortening causes spindle receptors to reduce their firing rates (ion channels close in absence of tension)
Membrane potential is proportional to:
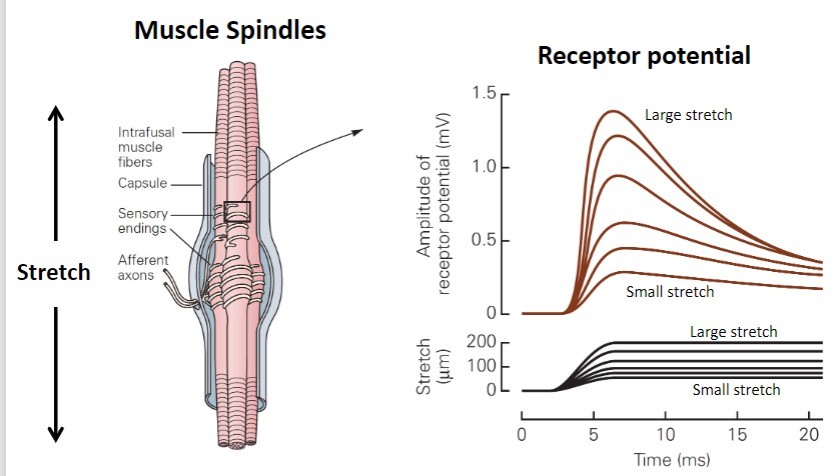
the amount and rate of muscle stretch.
Relationship Between Muscle Stretch and Excitation
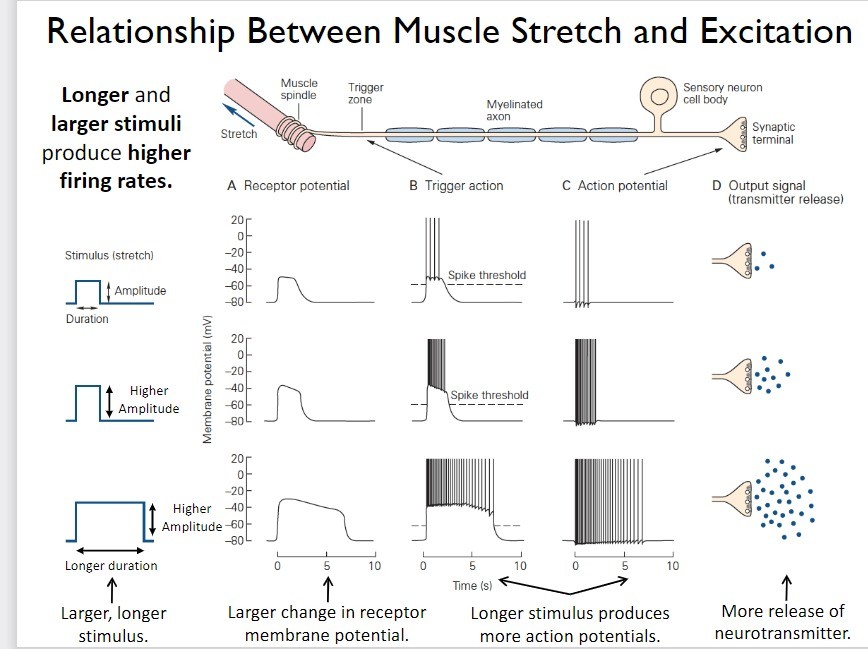
Longer and larger stimuli produce higher firing rates.
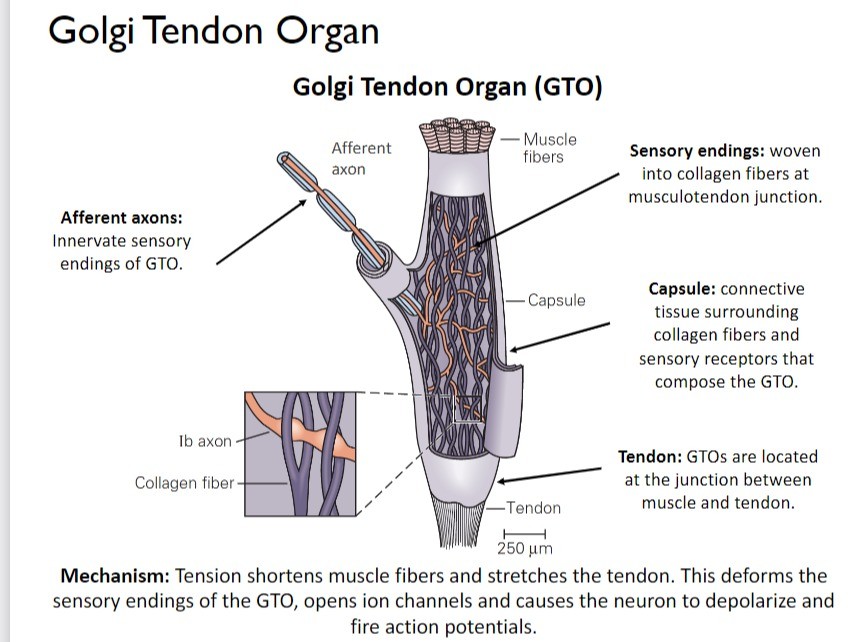
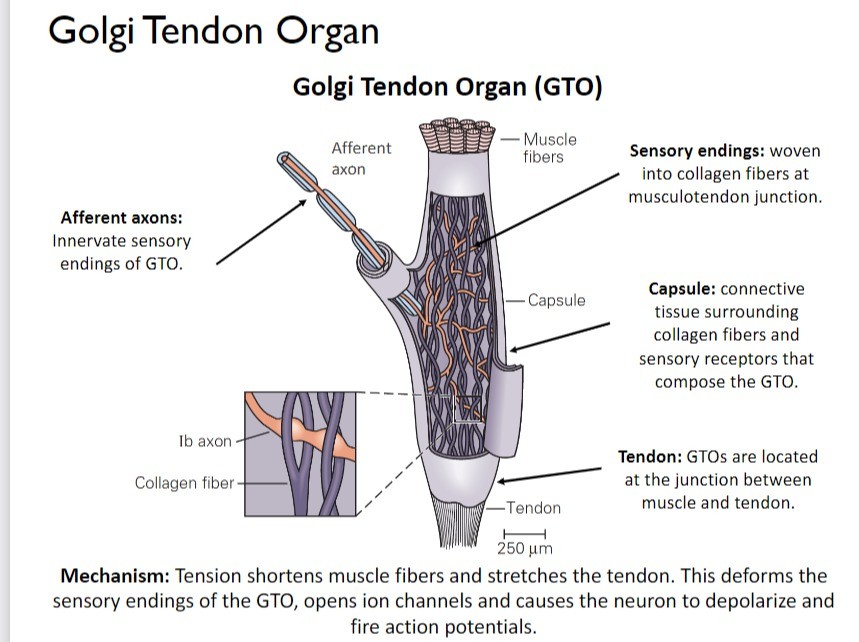
Golgi tendon organ sensitivity
Golgi tendon organs are sensitive to muscle tension (force).
Afferent axons of the GTO
Innervate sensory endings of GTO.
Sensory ending in GTO
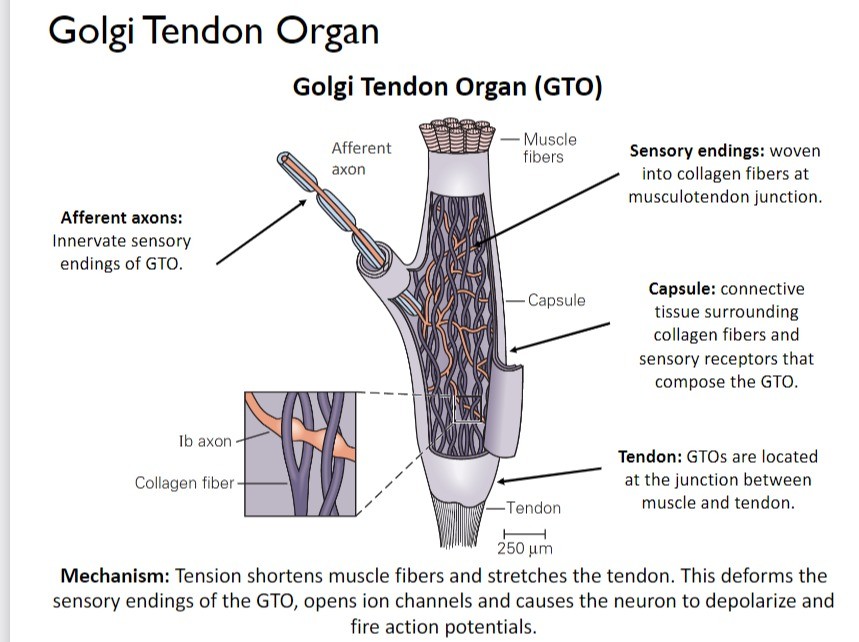
woven into collagen fibers at musculotendon junction
Capsule of GTO
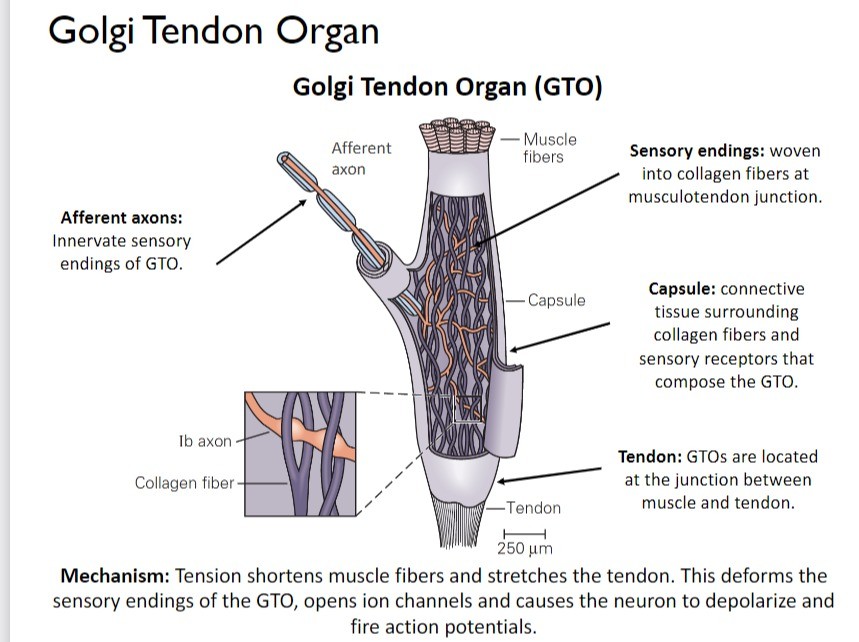
connective tissue surrounding collagen fibers and sensory receptors that compose the GTO.
Where are GTOs located?
GTOs are located at the junction between muscle and tendon.
Mechanism of golgi tendon organs
Tension shortens muscle fibers and stretches the tendon. This deforms the sensory endings of the GTO, opens ion channels and causes the neuron to depolarize and fire action potentials.
*collagen fibres crush the dendrites causing a measure of the force from muscle spindles
What are the 'blue' strands of GTOs?
collagen fibres
*NOT rate of contraction (muscle spindles)
What is GTO discharge proportional to?
GTO discharge is proportional to muscle tension. Thus, GTOs provide information about the force of contraction.
Do GTOs measure passive stretch of muscles?
NO! When stretching the muscle is loose = no tendon pulling
- even if you were going to rip your muscle = no
- joint receptors would detect ripping (hyperextension/flexion)
Type Ia afferents
- are the largest diameter afferents.
- They innervate all types of intrafusal fibers.
*faster conduction
*measure velocity of stretch
Type II afferents
Medium diameter afferents (smaller than type Ia, lower conduction velocities) that innervate static nuclear bag and nuclear chain fibers.
Muscle spindles are composed of 3 types of intrafusal fibers:
static nuclear bag fibers, dynamic nuclear bag fibers, static nuclear chain fibers.
What do muscle spindles typically have?
they typically have 2-3 bag fibers and a variable number of chain fibers (3-5).
Dynamic nuclear bag fibers
are sensitive to the velocity of muscle stretch. They fire when motion lengthens intrafusal fibers.
*pure bag type = dynamic phase
Static nuclear bag fibers
are sensitive to the amount of muscle stretch. They fire when motion lengthens intrafusal fibers.
*also innervated by static gamma neurosn
*both dynamic and length
What determines whether a spindle is more sensitive to the rate or amount of stretch?
The ratio of dynamic nuclear bag fibers to static nuclear bag and nuclear chain fibers
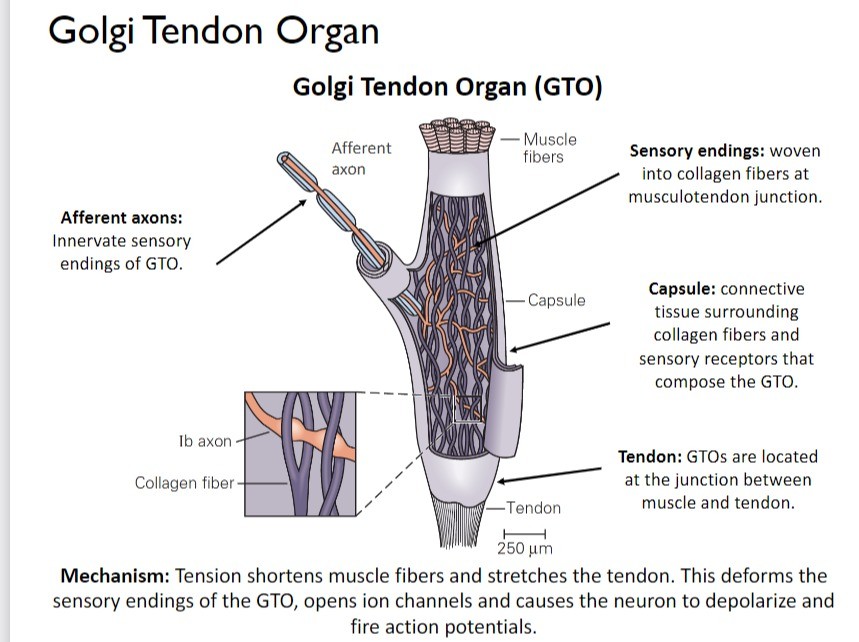
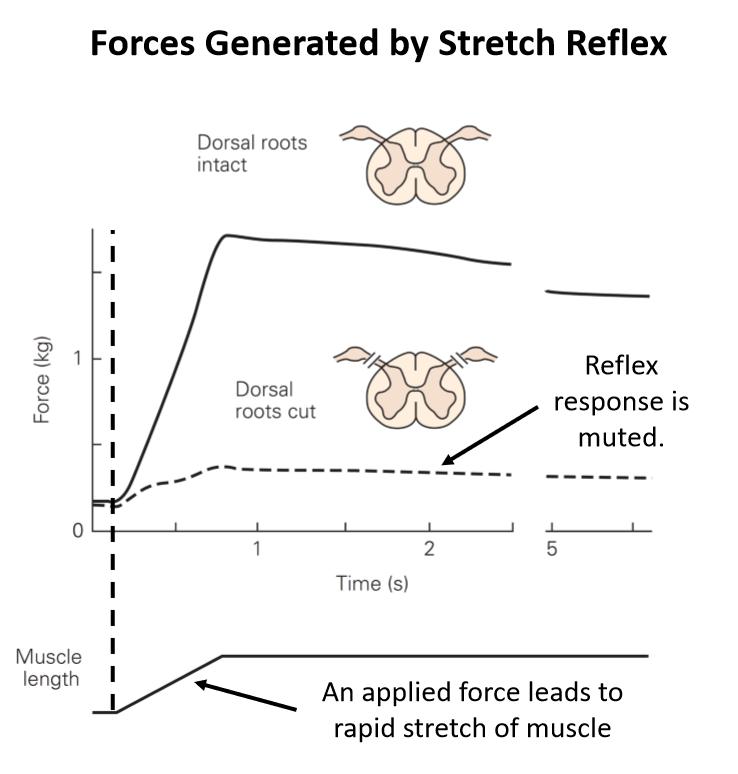
Knee jerk reflex (stretch reflex) process
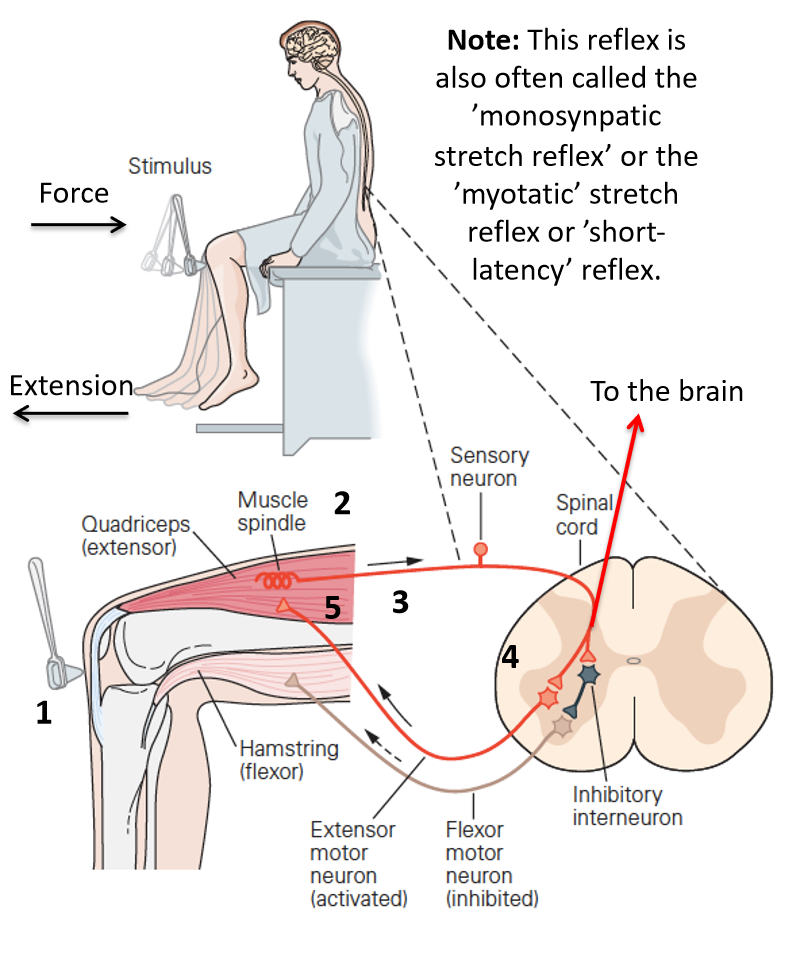
1. Tendon tap rapidly lengthens the quadriceps muscle.2. Stretch of quadriceps muscle lengthens intrafusal fibers, causing spindle to fire action potentials.3. Spindle afferents enter the spinal cord via the dorsal horn.4. Sensory neuron synapses on and excites alpha motor neuron (AMN).5. Excitation of AMN causes reflex contraction of quadriceps.6. Sensory neuron also synapses on inhibitory interneuron, which inhibits AMN of antagonist muscle (reciprocal inhibition).7. Hamstring (antagonist) is inhibited.8. Throughout steps 1-7, information is also being sent to the brain.
How long does the knee jerk reflex (stretch reflex)
The entire process from when a force is applied and reflexive muscle activity takes only 20-25 ms!
Why doesn't rapid contraction of the quadriceps cause a stretch reflex in the hamstrings?
Reciprocal inhibition!
6. Sensory neuron also synapses on inhibitory interneuron, which inhibits AMN of antagonist muscle (reciprocal inhibition).7. Hamstring (antagonist) is inhibited.8. Throughout steps 1-7, information is also being sent to the brain.
How does reciprocal inhibition work?
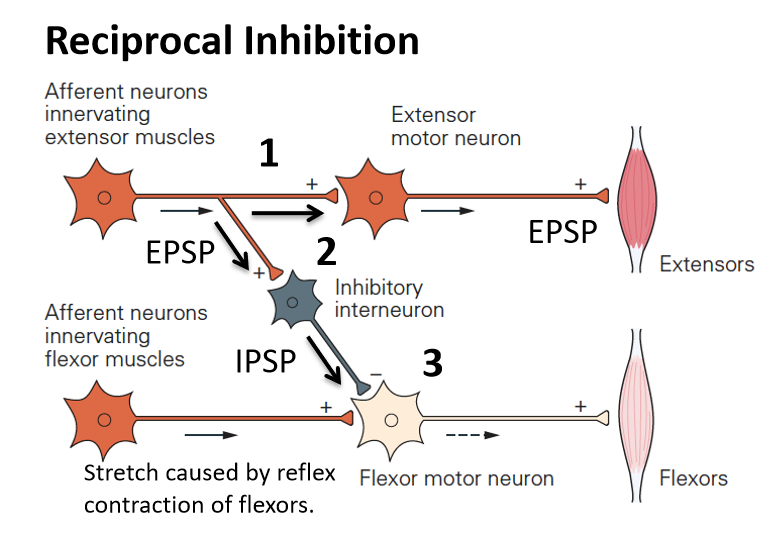
1. Muscle spindle inputs excite AMN and contracts the extensors.2. Muscle spindle inputs synapse on and excite inhibitory interneurons in the spinal cord.3. Graded summation of IPSP (inhibitory post-synaptic potential) and EPSPs at AMN of flexor muscles (typically causes inhibition).
Stretch reflex - activation of the synergists
Stretch of agonist muscle produces reflex contraction of agonist (homonymous; biceps brachii) and synergist muscles (e.g., brachialis), and inhibition of its antagonist(s)
Homonymous muscle
means ‘in the same muscle stretched by the stimulus’
How does deafferentation affect the amplitude of spinal reflexes?
Basic reflex function is impaired when their is no sensory information from the periphery
Central/Non-contractile region: of muscle spindle
middle doesn't contract = no stretch response (must have same tension to still respond)
What is the point of gamma-motor neurons?
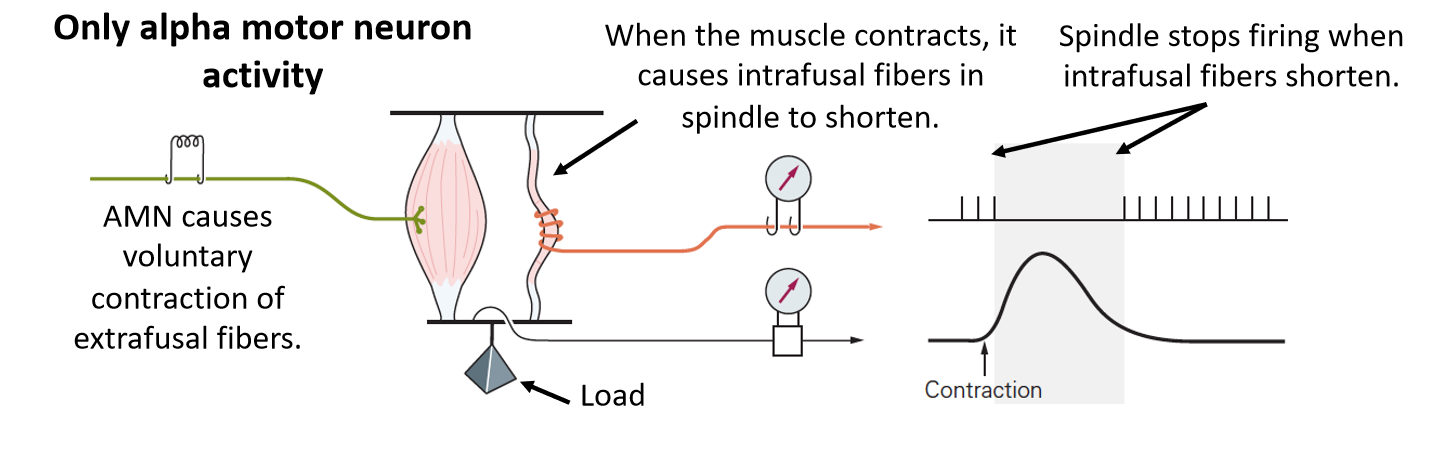
If there was only alpha motor neuron activity, muscle spindles would lose their sensitivity during voluntary movements.
How do gamma motor neurons help maintain spindle sensitivity to measure unexpected changes in muscle length during voluntary movements?
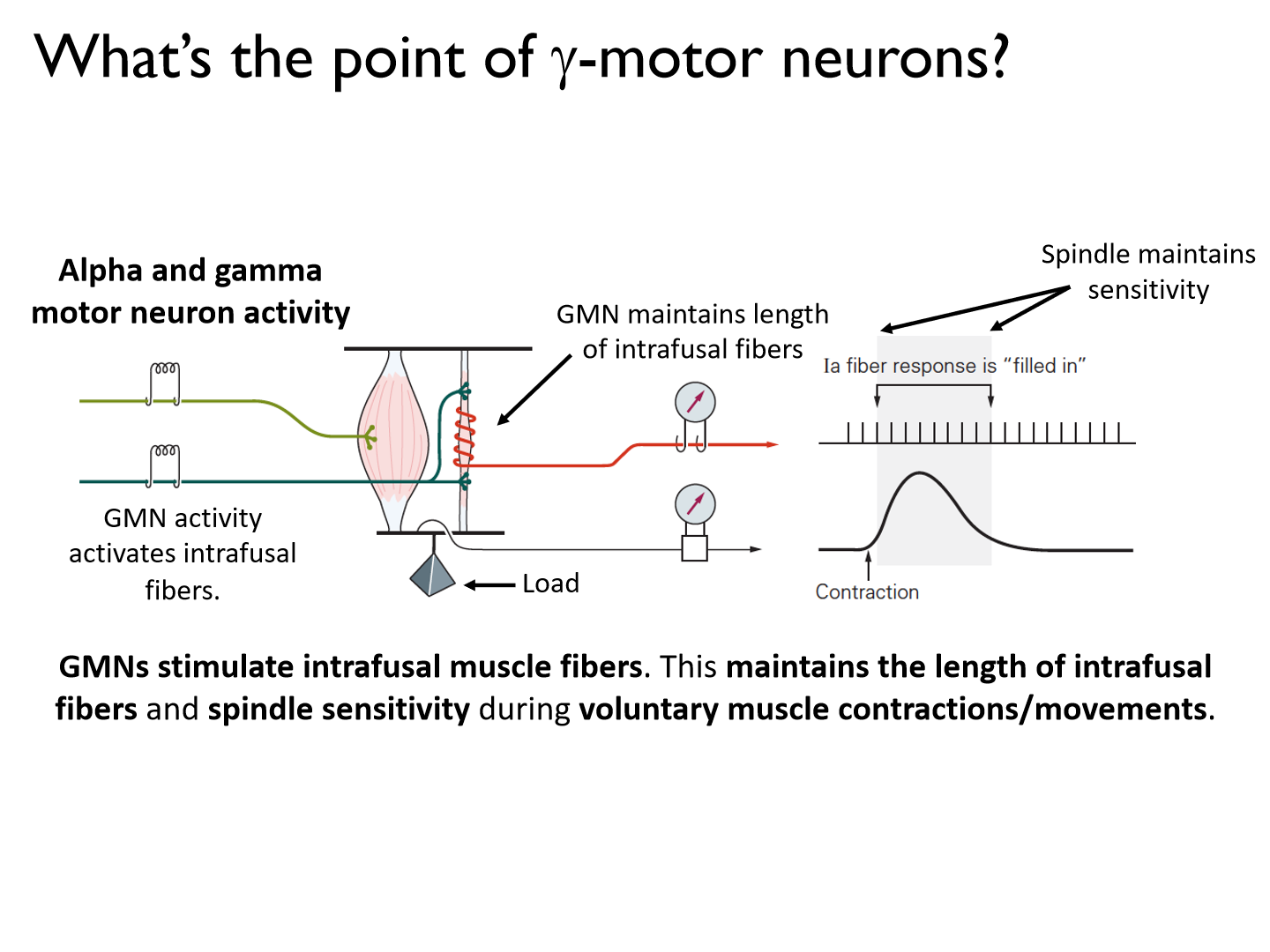
GMNs stimulate intrafusal muscle fibers. This maintains the length of intrafusal fibers and spindle sensitivity during voluntary muscle contractions/movements.
What the gamma mechanism called?
alpha-gamma coactivation
*NO independent
alpha-gamma coactivation during voluntary movements
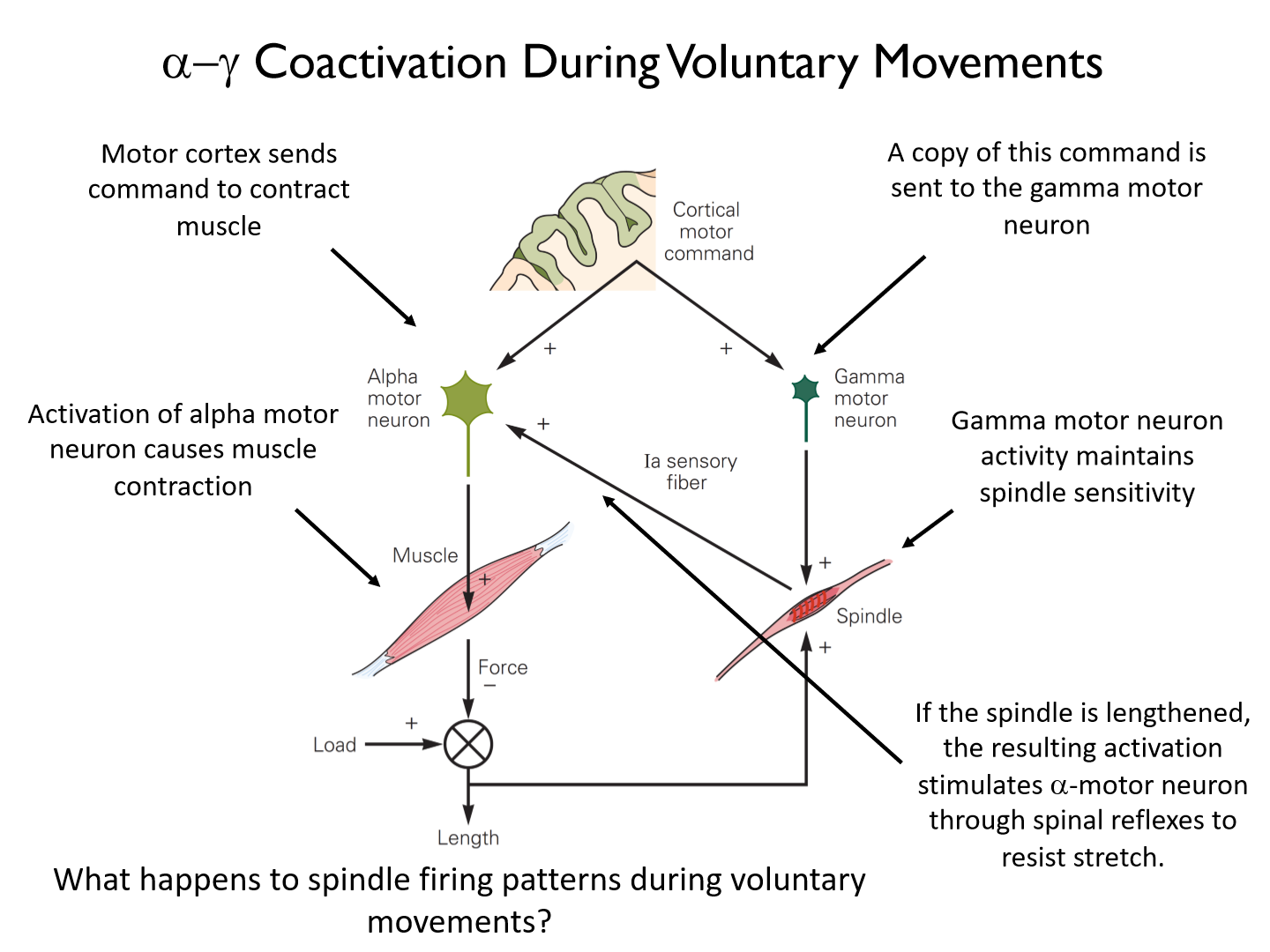
*Ia sensory fiber (muscle spindle) discharge rate increases during voluntary contraction
What happens to spindle firing patterns during voluntary movements?
*Ia sensory fiber (muscle spindle) discharge rate increases during voluntary contraction
*During active contractions, a-g coactivation maintains (at the very least) or can even increase spindle firing rates and sensitivity to changes in muscle length (sensory feedback).
- says there is a stretch going on
Static vs. dynamic gamma motor neurons
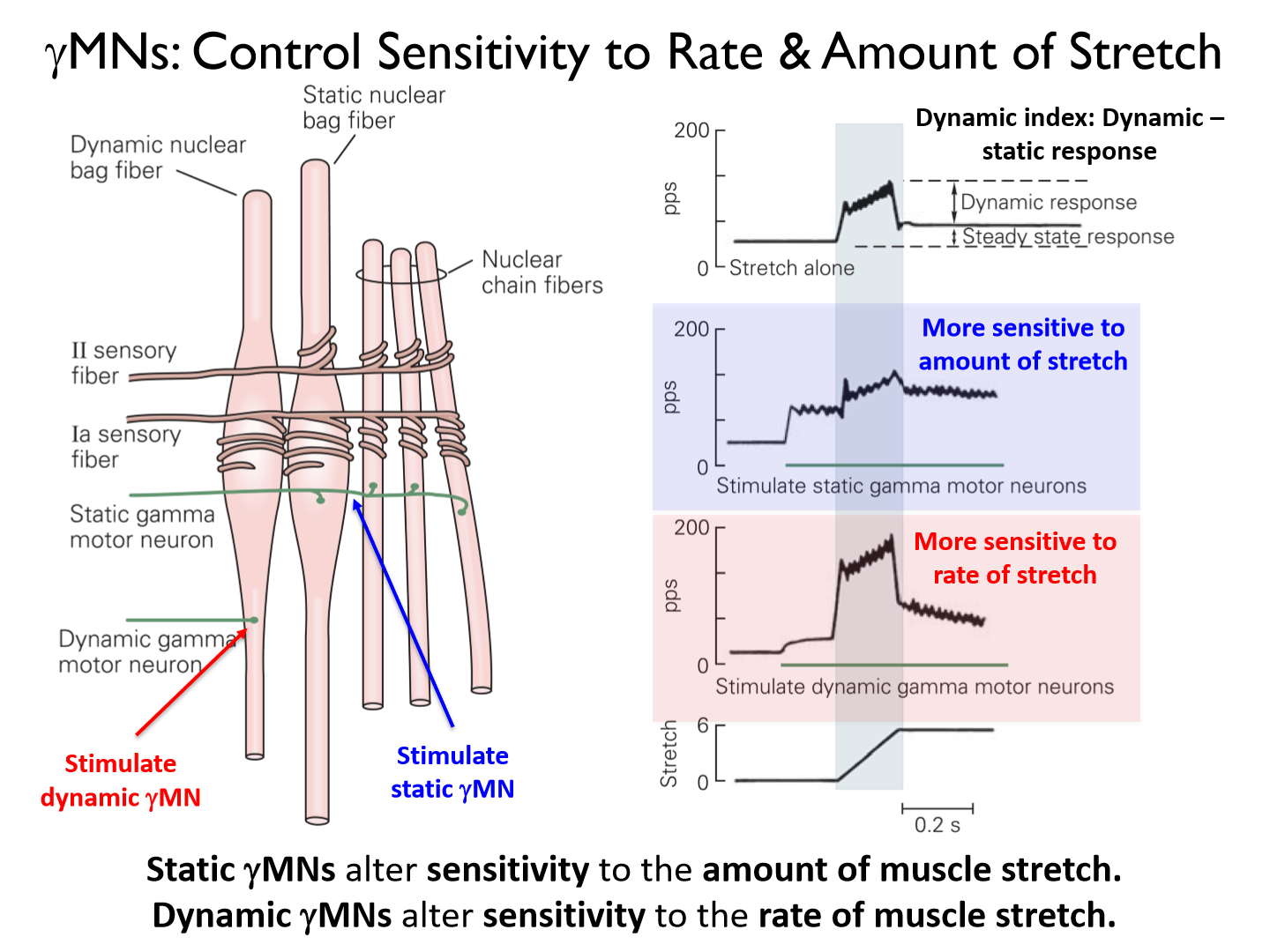
- Static gMNs alter sensitivity to the amount of muscle stretch.- Dynamic gMNs alter sensitivity to the rate of muscle stretch.
Golgi tendon organ reflex
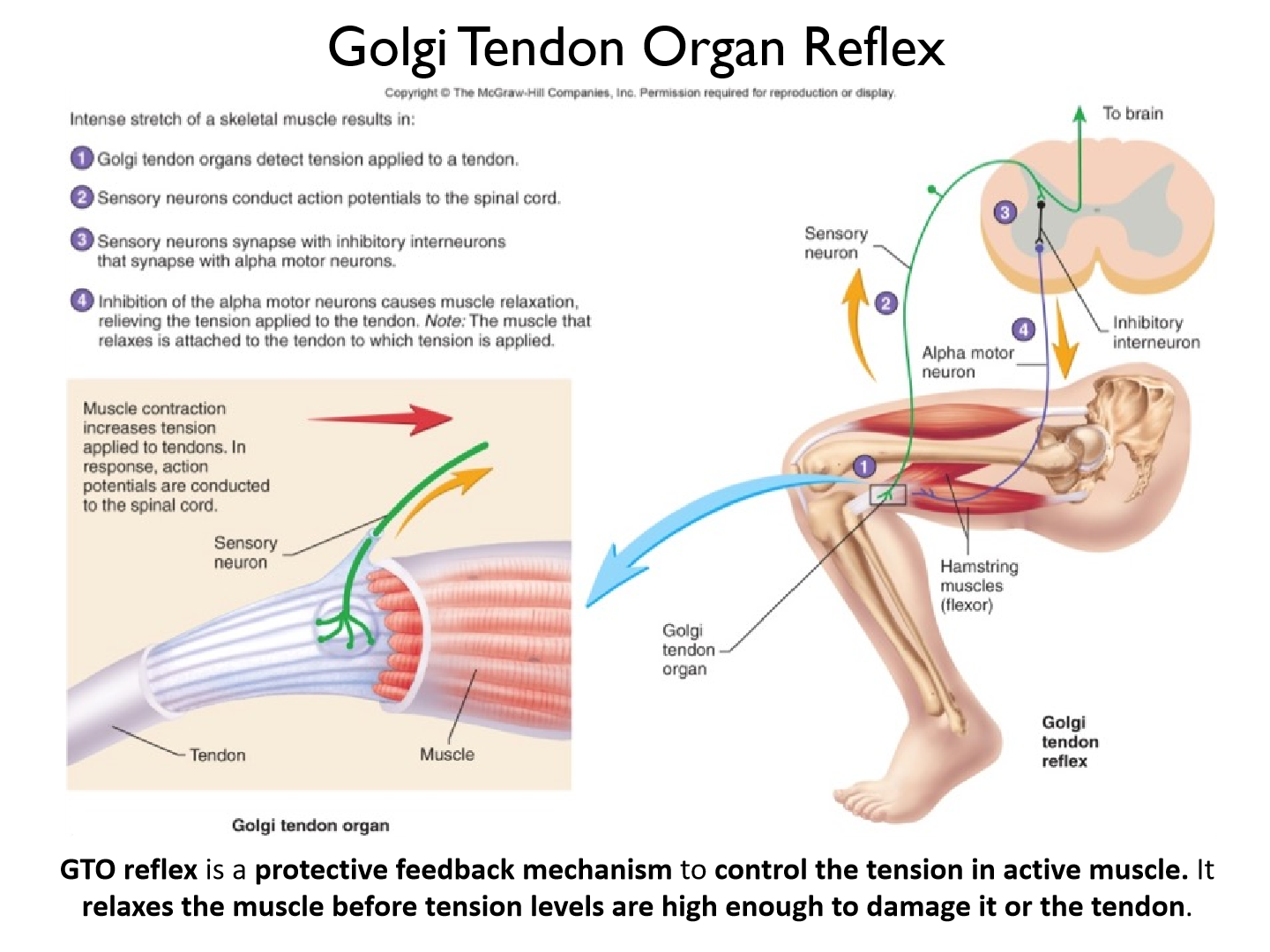
GTO reflex is a protective feedback mechanism to control the tension in active muscle. It relaxes the muscle before tension levels are high enough to damage it or the tendon.
*autogenic inhibition (turn off homogenous muscle)
Why do steroids increase tendon tears?
- GTO organ = more stimulus = responds less to force
- steroids increase muscle activity and growth quickly = does NOT strengthen tendon growth (need to stimulate as well)
What muscle spindle intrafusal fibers respond to the knee jerk reflex
primarily bag type (dynamic)
Reflective vs. voluntary movement
Reflective: Most Automatic Start within 20 ms of the onset of a perturbation that stretches muscle
Voluntary: Least Automatic Take ~120 ms to launch a voluntary movement following a visual or mechanical stimulus. (more synapses = slow)
Reflexes
Traditional view of reflexes is that they involve automatic, stereotyped, involuntary and rapidresponses to a sensory stimulus.
e.g. knee jerk
Short-Latency Stretch Reflex (SLR)

The short-latency stretch reflex involves spinal processing and occurs 20-50ms after a muscle is stretched by a physical stimulus. It is also often called the ‘myotatic reflex’ or ‘monosynaptic stretch reflex’.
- can be controlled with topdown inhibition
- increases with increased background activity
Long-Latency Stretch Response (LLR)
Is a polysynaptic reflex that involves cortical processing. It happens 50-105ms after a muscle is stretched by a physical stimulus. It is often called the ‘long-loop’ response or ‘transcortical’ response.
Why does LLR have such a long response speed?
- age (demylination)
- arm = faster
- leg = slower
How do we measure stretch responses in the lab?
We pply loads to the body (e.g. wrist) for 100ms or more and observe how subjects respond.
Speed and input of each feedback/response mechanism
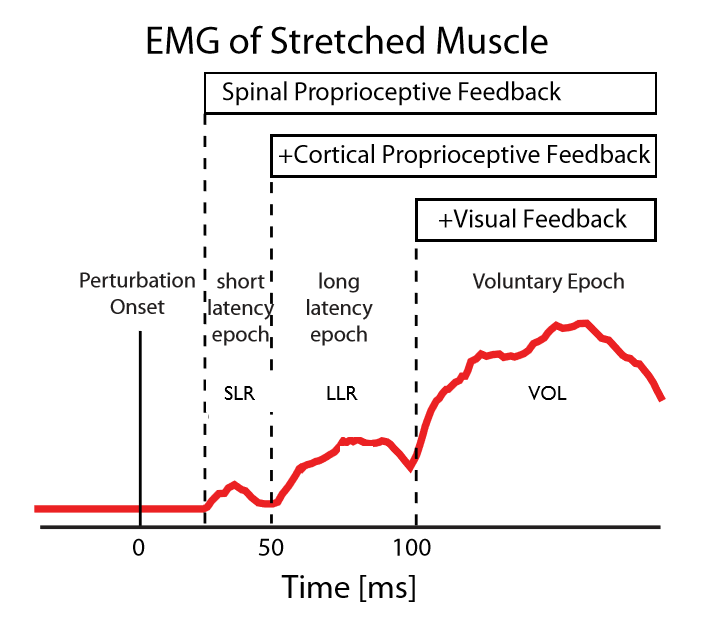
Short-latency response (SLR: 20-50ms): spinal feedback.Long-latency response (LLR: 50-105ms): spinal and cortical feedback.Voluntary response (VOL: 100+ ms): spinal, cortical, and visual feedback
Properties of SLR
SLR recruit only spinal circuits and have simple processing capabilities
Processing capabilities of SLR (what are they affected by)
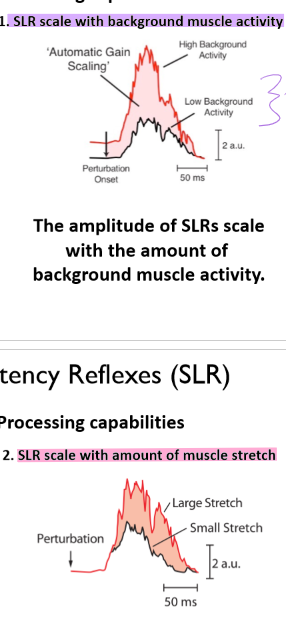
1. The amplitude of SLRs scale with the amount of background muscle activity.
2. For a given amount of background activity, the amplitude of SLRs scale with the amount and rate of muscle stretch.
LLR vs. voluntary actions
Voluntary actions and LLRs recruit the same sensory and motor areas of the brain
- Voluntary: includes visual!
LLR properties
LLRs (50-105ms post perturbation) recruit sensory and motor circuits in the brain and show flexible, goal-directed processing.
Processing capabilities of LLR (M2)
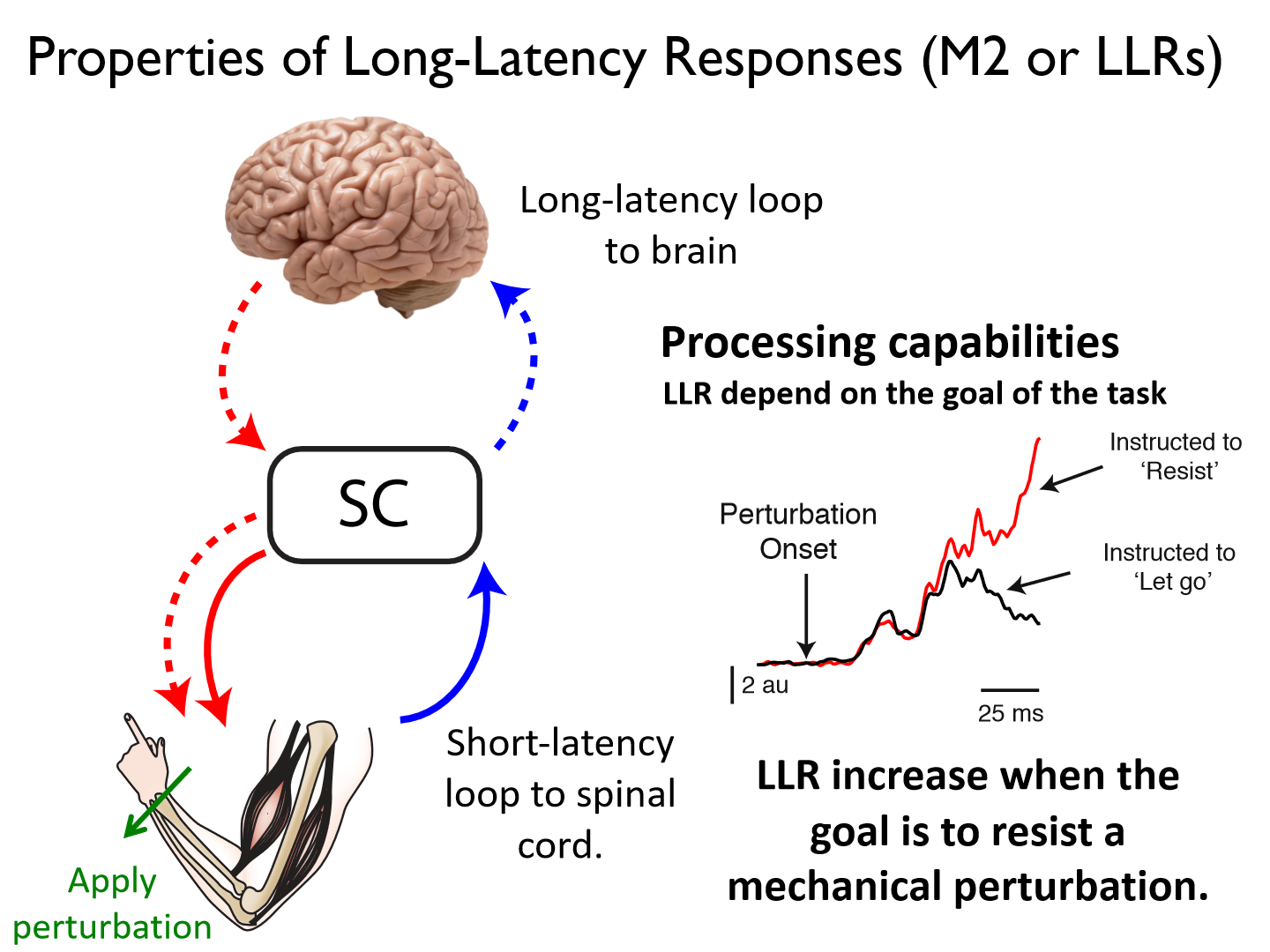
LLR increase when the goal is to resist a mechanical perturbation.
*trying to maintain a single goal (less adaptation) increases LLR activity
Where are goal-directed feedback responses generated?
the primary motor cortex (M1)
Goal-directed responses in hand kinematics.
Goal-directed responses begin in ~50ms in M1. M1 responses are larger when the hand is pushed away from target (OUT) and must make a correction to get to target on time.
Voluntary response (VOL)
The voluntary response (reaction time) happens with latency of 120-180 ms.
What processes the goal-directed abilities of voluntary actions?
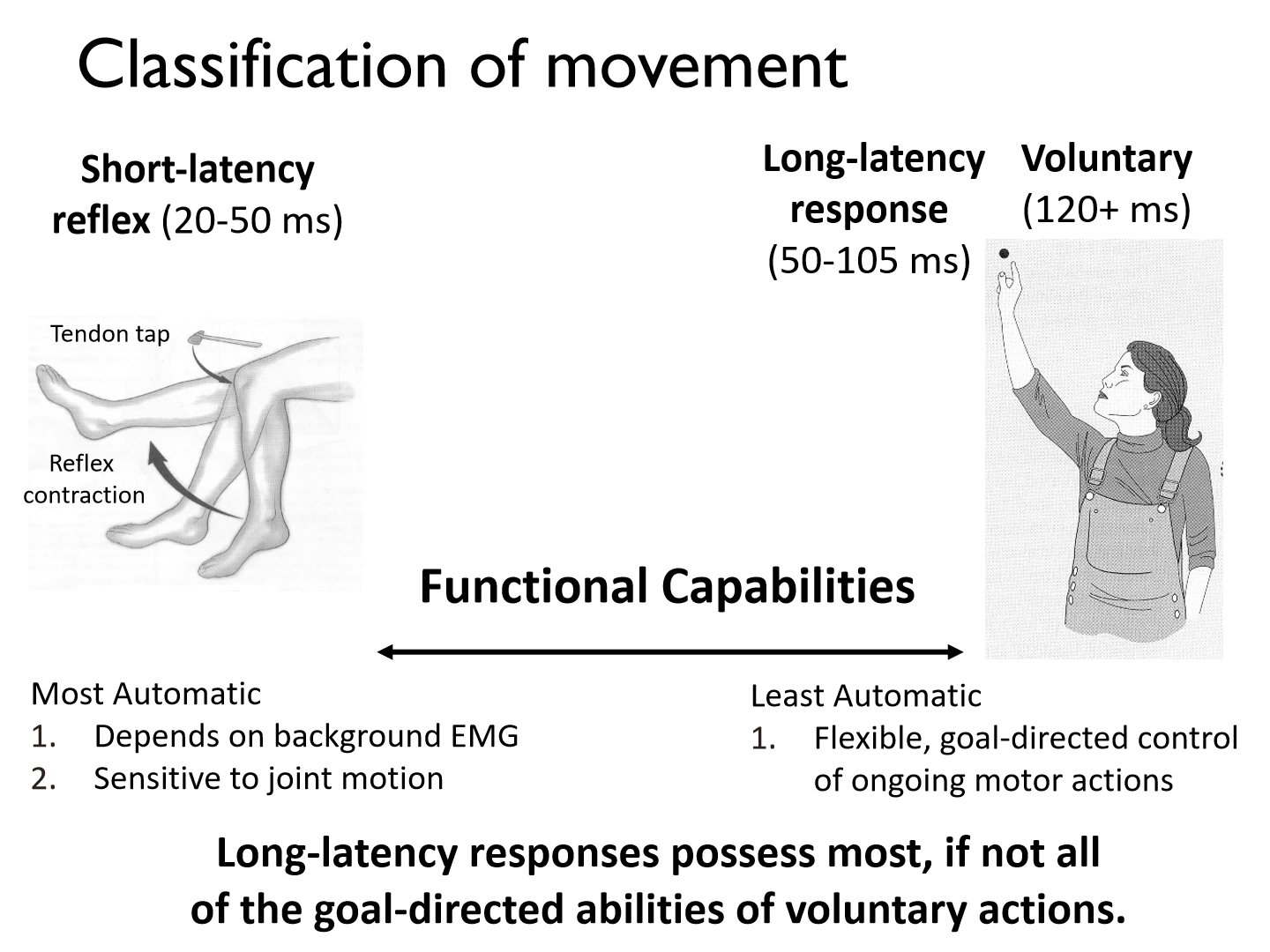
Long-latency responses possess most, if not all of the goal-directed abilities of voluntary actions.
Sensory Feedback for Proprioception key points
1. Sensory neurons travel in bundles (peripheral nerves) to the dorsal horn of the spinal cord.2. Dorsal column consists of axons of sensory neurons that carry touch and proprioceptive information.
Sensory Feedback for Proprioception – Dorsal Column- Medial Lemniscus Pathway (DCML Pathway)
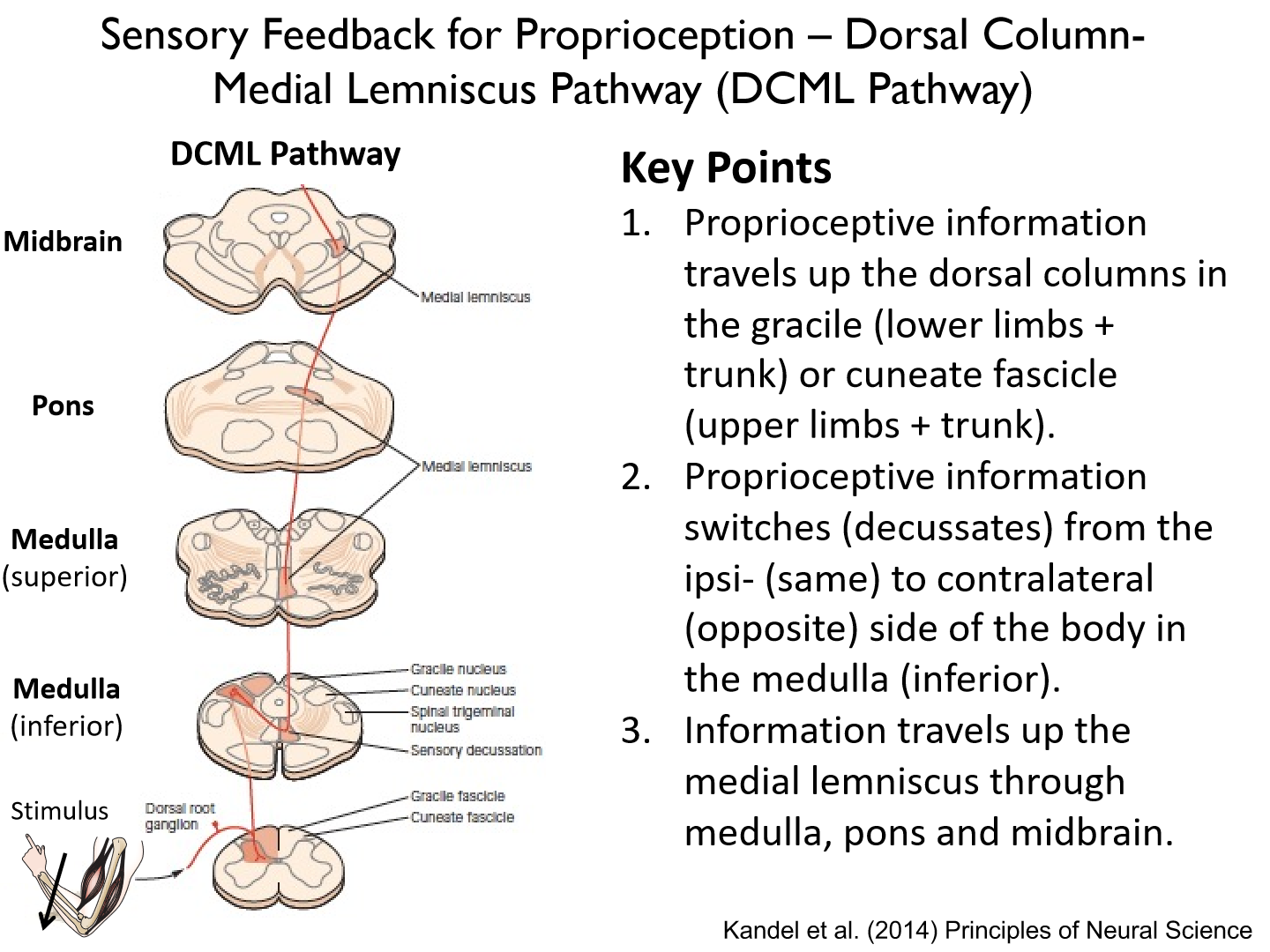
1. Proprioceptive information travels up the dorsal columns in the gracile (lower limbs + trunk) or cuneate fascicle (upper limbs + trunk).2. Proprioceptive information switches (decussates) from the ipsi- (same) to contralateral (opposite) side of the body in the medulla (inferior).3. Information travels up the medial lemniscus through medulla, pons and midbrain.
4. Sensory neurons travel in bundles (peripheral nerves) to the dorsal horn of the spinal cord.5. Dorsal column consists of the axons of sensory neurons that carry touch and proprioceptive information. These neurons synapse with neurons in medial lemniscus (located in the medulla).6. Neurons in the medial lemniscus synapse onto neurons in the thalamus.
7. Thalamic neurons relay proprioceptive information to primary somatosensory cortex via the posterior limb of the internal capsule
What are the 1st and 2nd synapses of the DCML pathway?
1st synapse: caudal medulla
2nd: thalamus
What is the internal capsule?

a white matter tract that carries information from the thalamus to primary sensory cortex.
Box diagram showing flow of proprioceptive feedback in S1
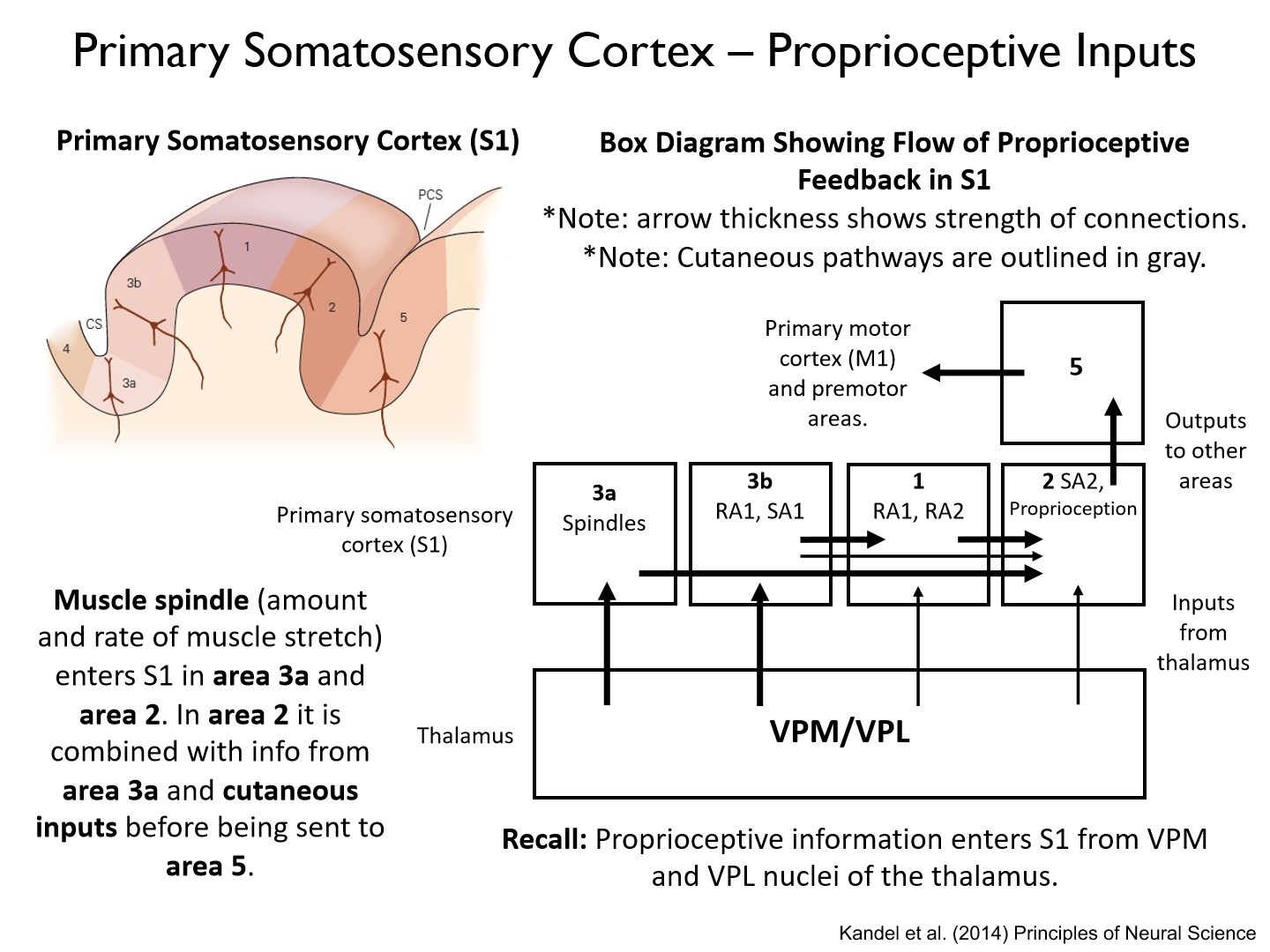
Primary somatosensory cortex 3a and 2
Muscle spindle (amount and rate of muscle stretch) enters S1 in area 3a and area 2. In area 2 it is combined with info from area 3a and cutaneous inputs before being sent to area 5.
Dorsal Spinocerebellar Pathway – Lower Limbs to Cerebellum
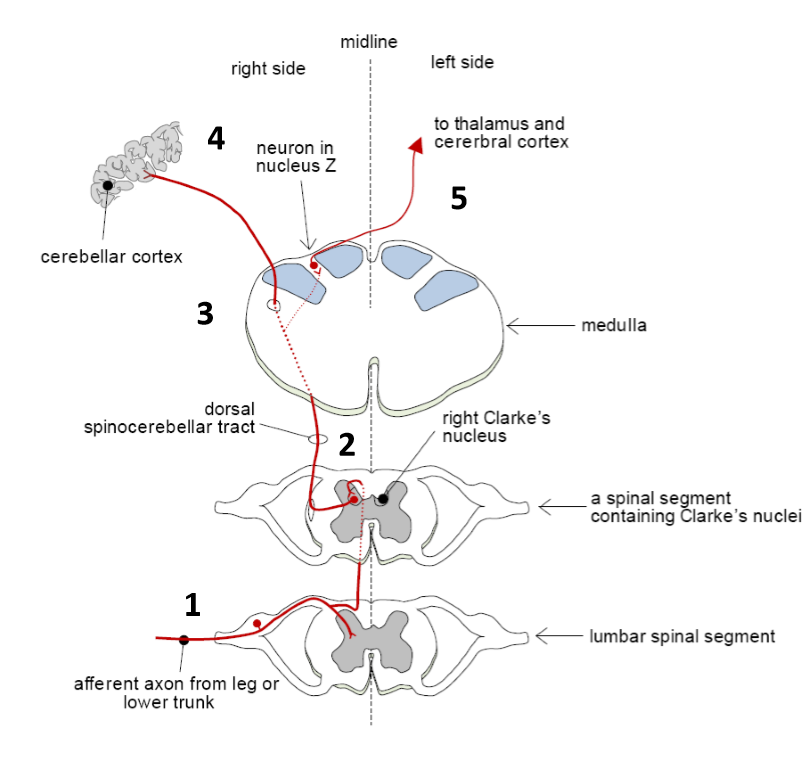
1. Somatosensory information carried by axons of sensory neurons of GTOs and spindles enter the dorsal horns of the spinal cord.
2. Somatosensory information travels up the ipsilateral dorsal horn of the spinal cord until it synapses onto 2nd order neuron in Clarke’s nucleus.
3. 2nd order neuron travels up dorsal spinocerebellar tract until it reaches the junction between the medulla and pons.
4. Information enters the cerebellum via the inferior cerebellar peduncle.
5. Some information decussates and travels to contralateral S1 via the thalamus.
Note: Information from the right side of the body enters the right side of the cerebellum
Clarke's nucleus
- Clarke’s nucleus is composed of neurons in the dorsal horn of the spinal cord.- Axonal projections from Clarke’s nucleus give rise to the dorsal spinocerebellarpathway.- Its projections enter the ipsilateral cerebellum via the inferior cerebellar peduncle.
**Clarke’s nucleus is a major spinal relay center involved in unconscious proprioception (perception for action).
Anterior Spinocerebellar Pathway – Lower Limbs to Cerebellum
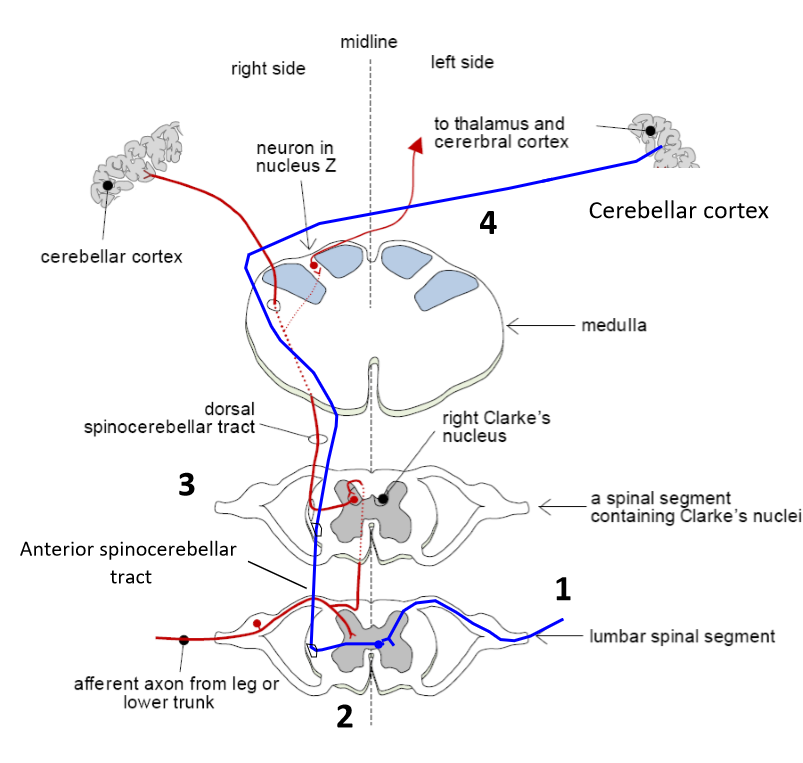
1. Somatosensory information carried by axons of sensory neurons of GTOs enter the dorsal horns of the spinal cord.
2. Some somatosensory information decussates to anterior spinocerebellar tract.
3. 2nd order neuron travels up anterior spinocerebellar tract until it reaches the junction between the medulla and pons.
4. Somatosensory information decussates again and enters ipsilateral cerebellum via the superior cerebellar peduncle
**Note: Information from the right side of the body enters the right side of the cerebellum.
What is the reason for the 'double cross'?
survival of spinal cord injuries
Cuneocerebellar tract
is upper limb homolog of dorsal spinocerebellar tract
Rostral spinocerebellar tract
is upper limb homolog of anterior spinocerebellar tract.
Spinocerebellar Tracts - Cerebellum overview
- Neurons in the dorsal and anterior (ventral) spinocerebellar tracts target the ipsilateral cerebellar cortex, and eventually, the deep cerebellar nuclei.
- The cerebellum is important for detecting and correcting errors during ongoing movements.
- After being processed in the cerebellum, proprioceptive feedback travels to the contralateral sensory and motor areas via the thalamus. This pathway is important for unconscious proprioception (proprioception for action).
*DCML --> SI
DSC --> SI (slower = more synapses)
Cerebellar once processed goes to SI (much slower = double processing)
Where LLR and voluntary epoc come in
What is the difference between the dorsal and anterior spinocerebellar pathway
SAME information
- difference is contralateral vs. ipsilateral
There are 4 main regions in S1:
1) Area 3a: Spindle and (muscle length).
2) Area 3b: input from SA1 & RA1 receptors (location, force and change in force applied to skin).
3) Area 1: input from RA1 & RA2 receptors (motion of stimulus or object relative to skin).
4) Area 2: Proprioception – sense of relative position and motion of body parts, self vs. externally generated motion (combines info from areas 3a, 3b, and 1).
Each separate region of S1 has its own:
somatosensory organization
- homunculous
Summary of S1
Location:
• Rostral parietal lobe
• Caudal to the central sulcus
Inputs:
• Somatosensory feedback from thalamus
- VPL: upper limb, lower limb, trunk.
- VPM: head, neck, face.
Homunculus (somatotopic map):
• Amount of space is proportional to number of receptors (also loosely related to dexterity of body part).
S1 Outputs:
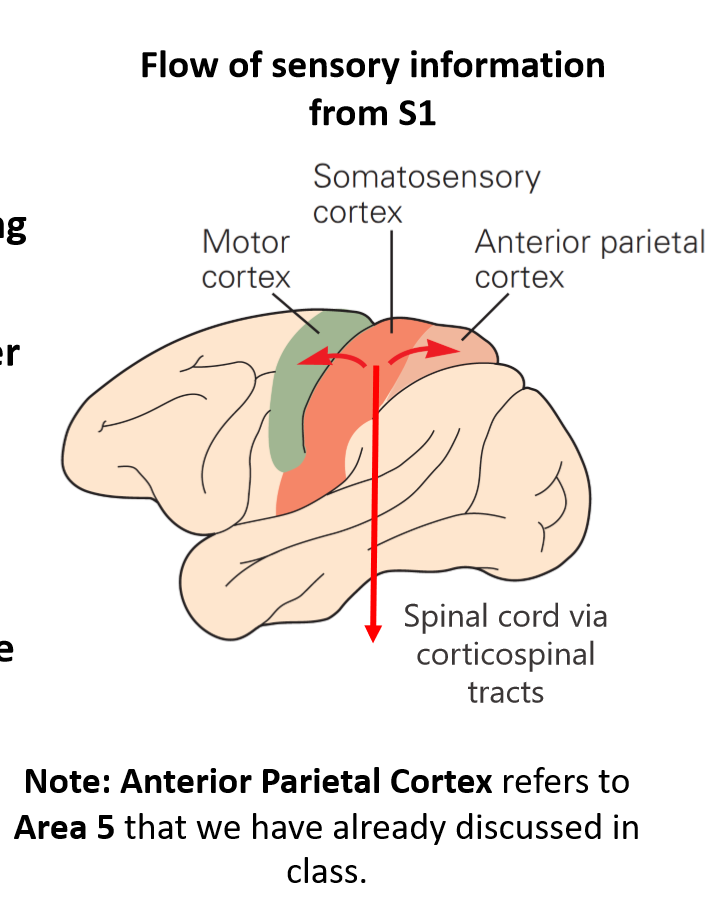
• Primary motor cortex (M1) in frontal lobe to influence ongoing motor actions.
• Area 5 in parietal lobe for higher level sensory processing and integration of somatosensory information with visual feedback (we’ll touch more on this later).
• Corticospinal tracts (lateral and ventral) to influence ongoing sensory and motor processing in the spinal cord
Descending Pathways – S1
Internal capsule is a white matter tract that carries information from primary sensory cortex to the spinal cord.
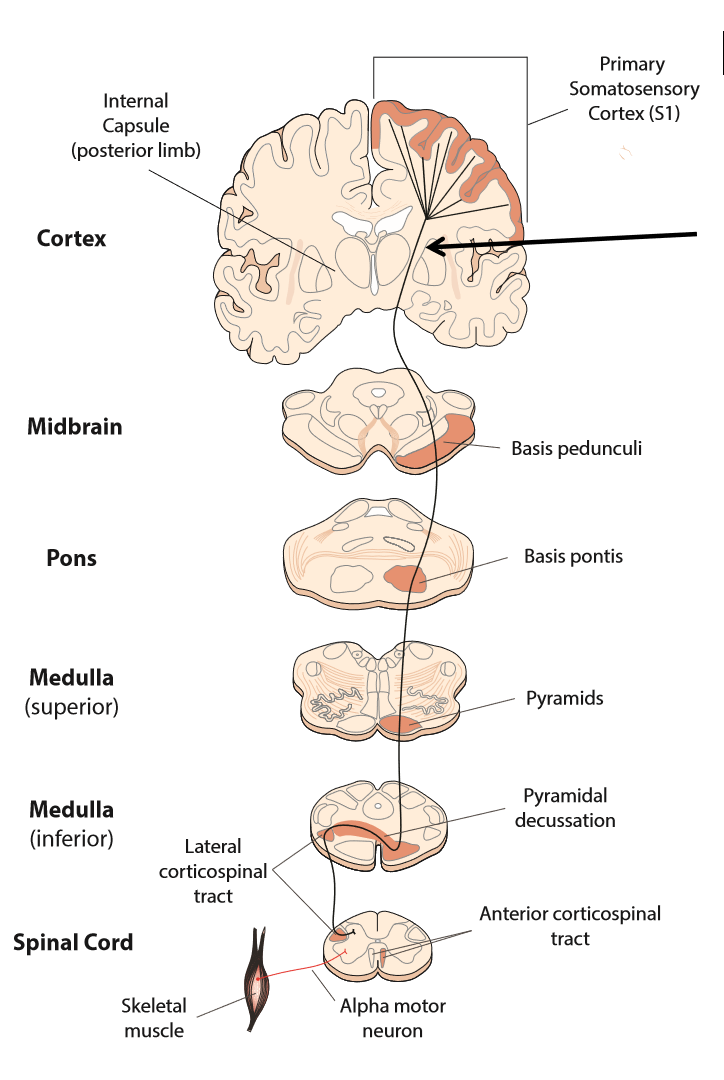
Key points of descending pathways - S1
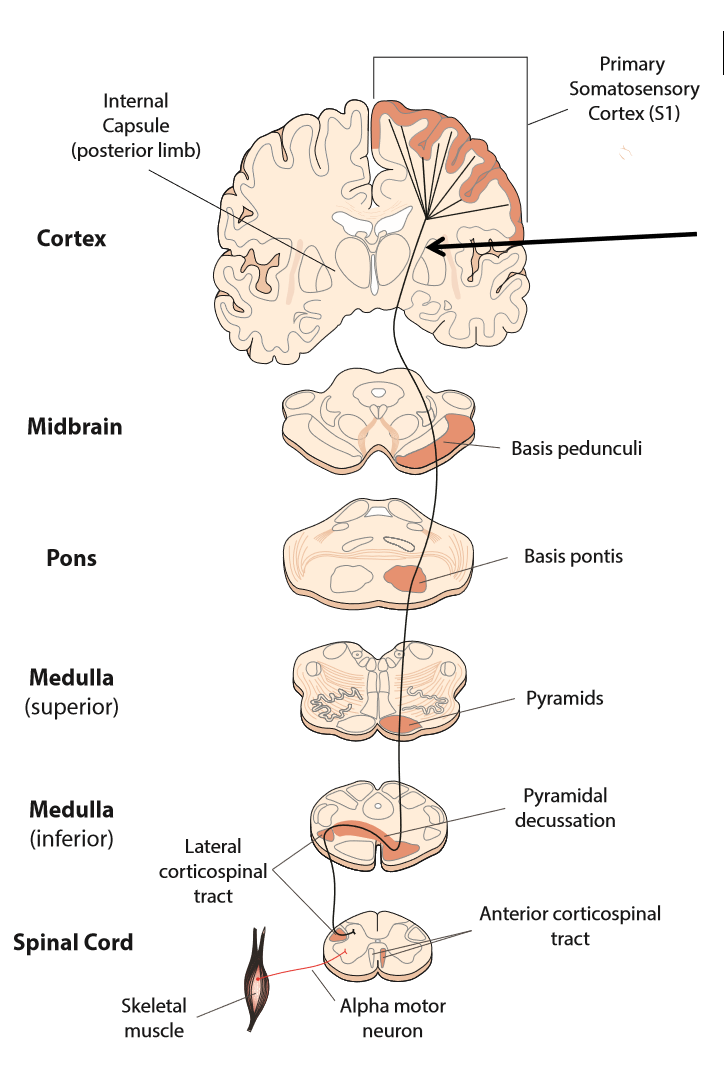
1. Output neurons leave S1 and travel via the internal capsule (posterior limb) to the midbrain, pons and medulla.
2. In the medulla, these neurons enter the pyramids – a protuberance of descending neurons arising from different areas of cerebral cortex.
3. Most neurons (90%) decussate (switch sides) from ipsi- (same) to contralateral side (opposite). This switch happens at pyramidal decussation to the lateral corticospinal tract (CST).
4. Neurons travel down lateral CST until they synapse on sensory neurons in dorsal horn or interneurons in intermediate zones of the spinal cord.
*10% are from the ventral (anterior) cortical spinal track (ipsilateral and bilaterally)
S1 projects axons down the lateral corticospinal tract to:
influence the ongoing processing of sensory information in local spinal circuits (or activity in motor neurons via interneurons).~30% of CST (corticospinal tract) neurons arise from S1.
*increase or decrease peripheral firing rate through S1
Damage to descending S1 pathways
Damage to descending neuron above pyramidal decussation affects contralateral side of the body.Damage to descending neuron below pyramidal decussation affects ipsilateral side of the body
Amputees often report:
• Vivid sensory representation of their missing limb.• Phantom movements of the missing limb.• Feel phantom limb with stimulation of other body parts (reference fields).
Phantom Limb Syndrome
• Patients often report feeling ’phantom pain’ in amputated body parts.• Phantom pain is caused by reorganization of S1 following the loss of a limb.
Why does phantom pain occur?
- These ’referred sensations’ are caused by the remapping andreorganization of cortical circuits in S1.- Recall: Arm and face areas are adjacent to the hand area in S1.- As hand afferents wither in S1, adjacent areas may take over
Prosthetics and Phantom Limbs
• Describes how prosthetics can be used to alleviate phantom pain• Talks about abnormal phantom limbs – changes in size, perceived deformities, pain.
Phantom Limbs and Mirror Box Therapy
Mirror boxes can be used to alleviate painful postures of the phantom limb. Proven efficacy via clinical trials and now used in clinical practice.
1) How does mirror box therapy influence cortical remapping associated withphantom limbs (does it prevent extensive remapping)?2) Is there a dose-response relationship (more therapy = less remapping)?3) Is early mirror box therapy more effective (less reorganization/plasticity)?
1) Yes
2) Yes
3) early = more effective
Phantom Limbs and Cortical Reorganization
• Motor areas of the brain are active when individual with phantom hand is asked to move their fingers – there is a representation of the hand preserved in the brain (not so for individual without phantom hand).• More cortical reorganization is associated with more phantom pain (i.e., plasticity isn’t a good thing).
1) Do the individuals with no phantom limb (presumably complete reorganization) experience more phantom pain?2) Is phantom pain caused by incomplete remapping of cortex?3) Are there other areas in the brain (e.g., cerebellum) that show a representation of the phantom limb?4) Is there a relationship between sensory and motor reorganization?
1) sometimes, sometimes not
2) Maybe
3) We think so
4) Yes
What is the anterior parietal cortex?
Area 5 (technically separate from the somatosensory cortex)
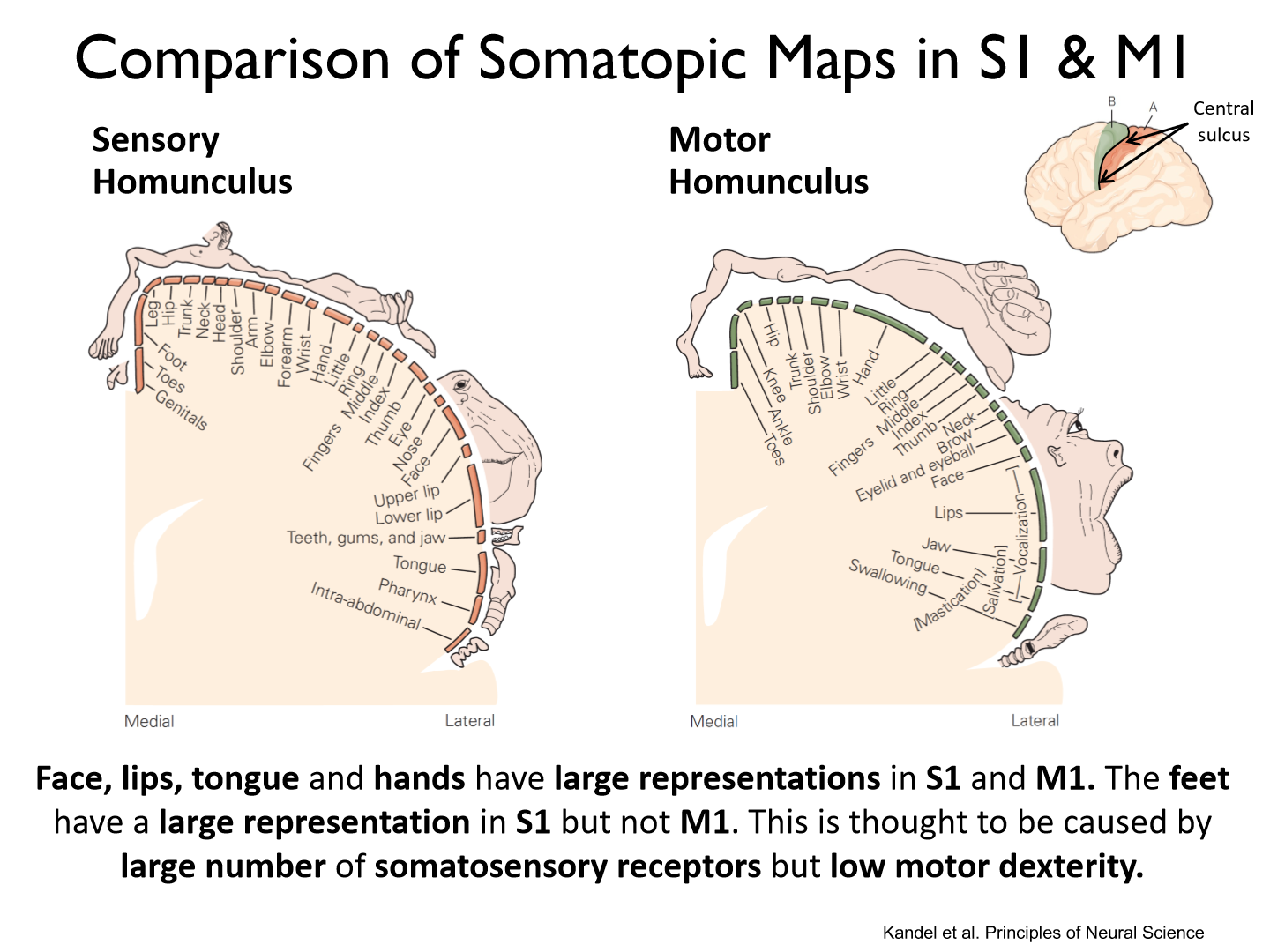
How is the primary motor cortex organized?
- organized by body part (homunculus or somatotopic map).- Larger representation for areas requiring fine, dextrous control (hands, face, lips, tongue).
S1 somatotopic map vs. M1 somatotopic map
- S1’s somatotopic map has larger representations for regions with larger numbers of receptors (feet, hands, face, lips, tongue)
- M1’s somatotopic map has larger representations for regions that require more dextrous/fine control (hands, face, lips, tongue)
**NO FEET
Do we see a the same regions larger in S1 and M1?
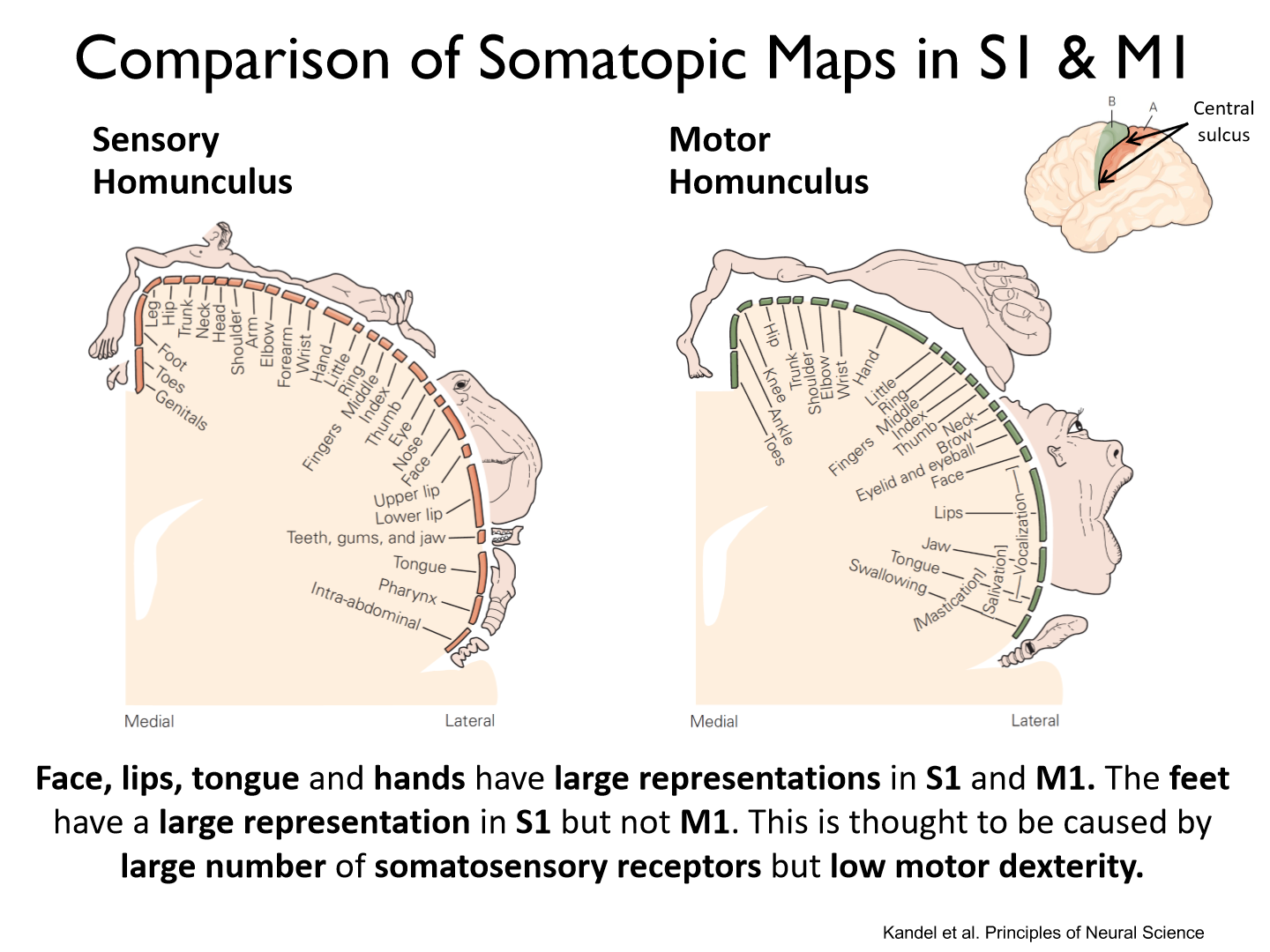
Face, lips, tongue and hands have large representations in S1 and M1. The feet have a large representation in S1 but NOT M1. This is thought to be caused by large number of somatosensory receptors but low motor dexterity.
Anatomy of M1 (area 4)
• Caudal portion of frontal lobe• Rostral to central sulcus
Inputs to M1
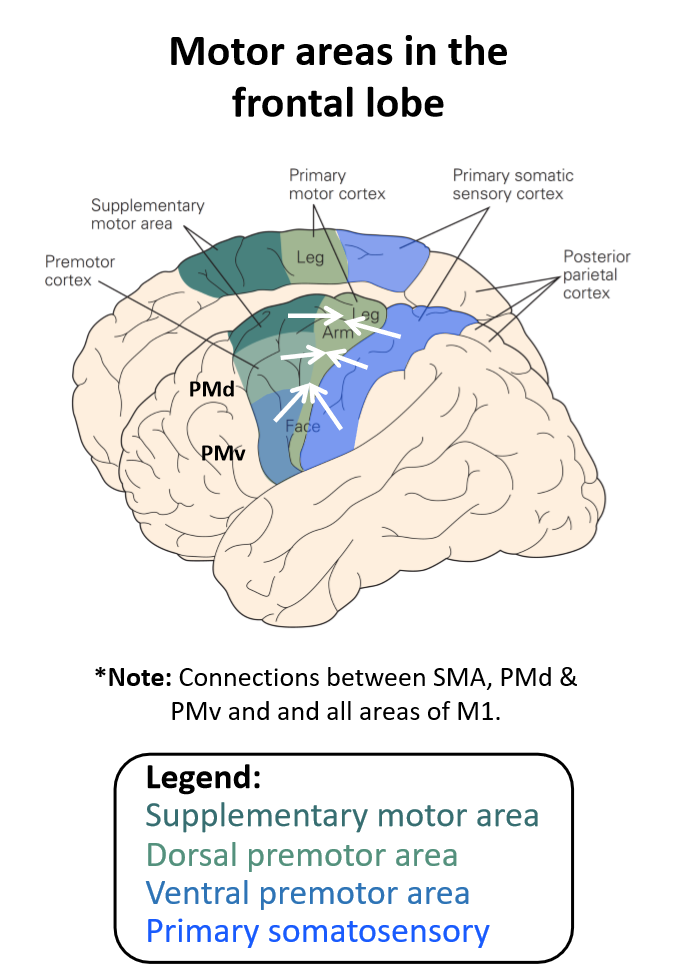
Cortical Structures• Receives somatosensory feedback from primary somatosensory cortex (S1)• Planning-related activity from supplementary motor areas (SMA)• Planning-related activity from premotor areas- Dorsal Premotor Area (PMd)- Ventral Premotor Area (PMv)
*M1 includes all 3
Homunculus map of M1
Amount of space is proportional to dexterity/precision of movements made by that body part/effector.
M1 outputs
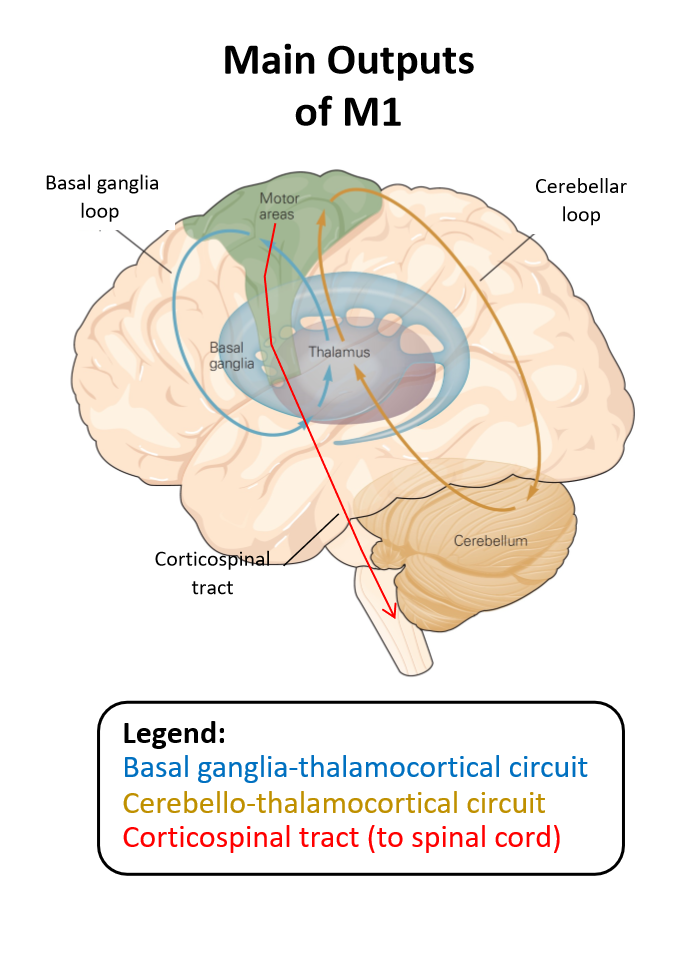
• Outputs to descending motor tracts to initiate and control voluntary motor actions (corticospinal tract). • Connections with the cerebellum provide efference copy (corollary discharge) of motor signals during ongoing actions (cortico-ponto-cerebellar circuit). (copy of motor command)• Recurrent connections with nuclei within the basal ganglia influence ongoing processing in M1 (basal ganglia-thalamocortical circuits). (thalamus and bellow processing)
Lesion Models
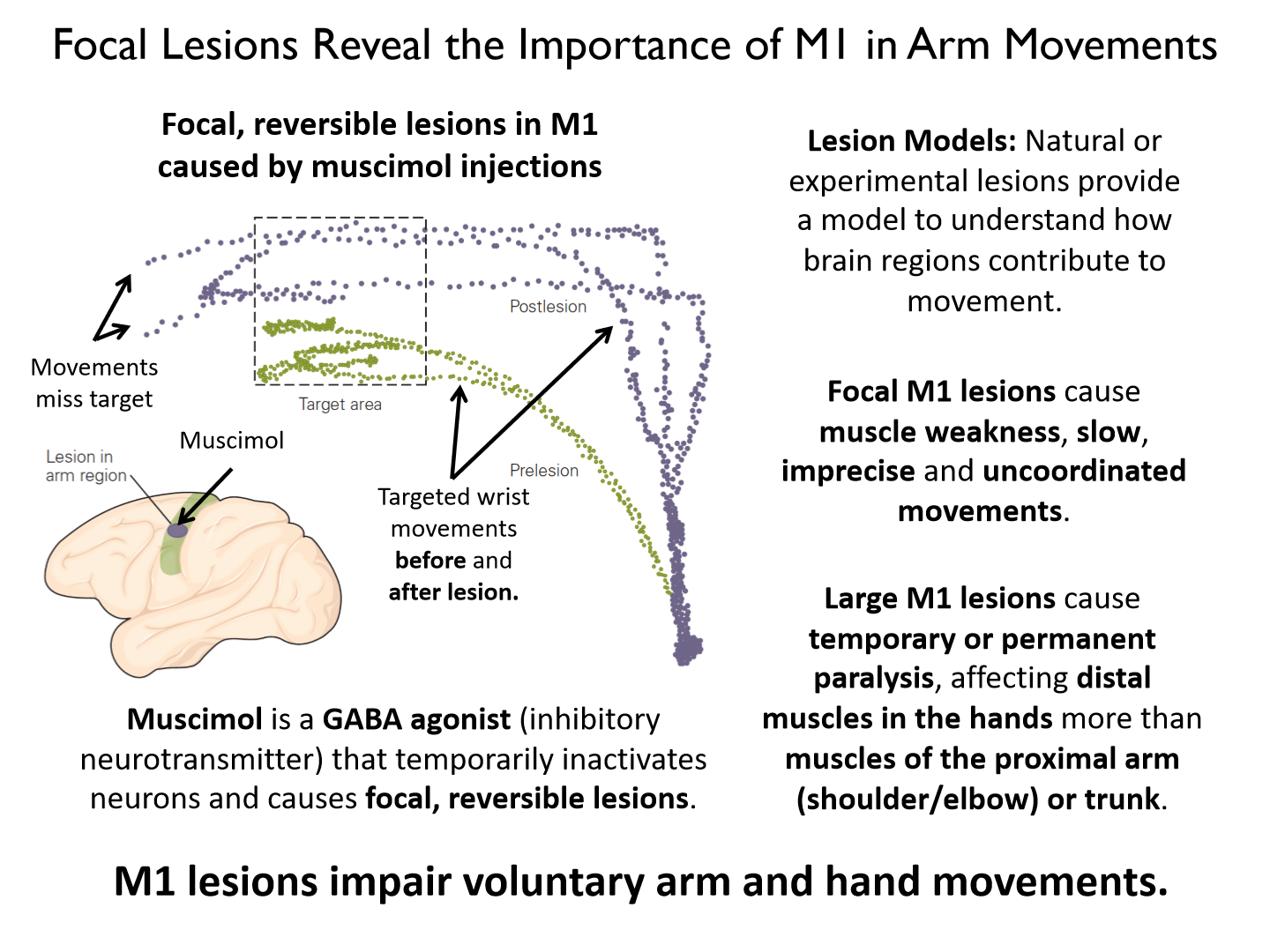
Natural or experimental lesions provide a model to understand how brain regions contribute to movement.
Focal M1 lesions cause:
muscle weakness, slow, imprecise and uncoordinated movements
Large M1 lesions cause:
temporary or permanent paralysis, affecting distal muscles in the hands more than muscles of the proximal arm (shoulder/elbow) or trunk.
Why do large M1 lesions affect distal muscles in the hands more?
Distal has more overlap & more representation in the brain
- information from both sides = hard to fully turn off area
Muscimol
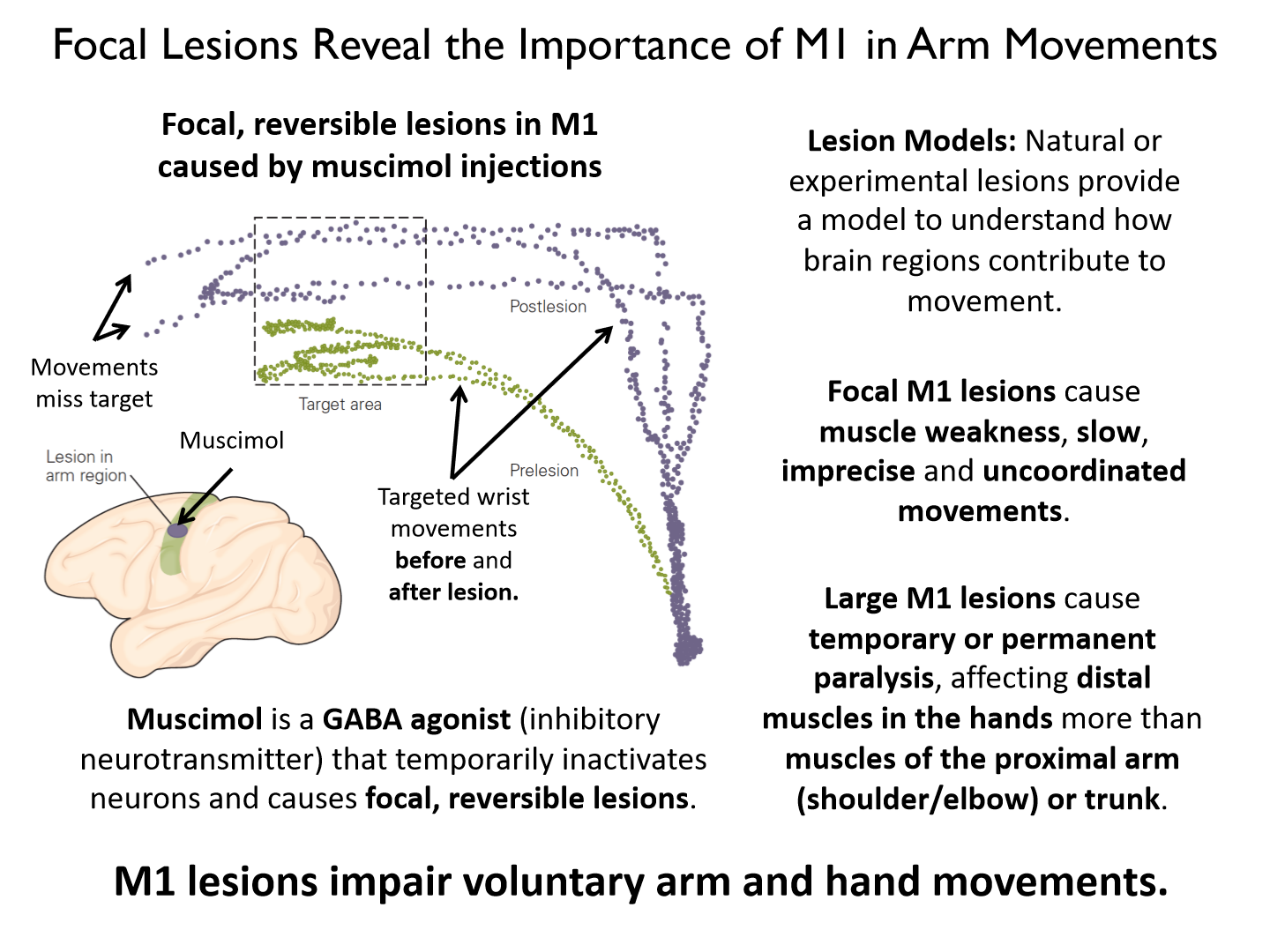
is a GABA agonist (inhibitory neurotransmitter) that temporarily inactivates neurons and causes focal, reversible lesions.
Overall what do M1 lesions impair?
voluntary arm and hand movements
Descending M1 pathway
Lateral Corticospinal tract
Descending M1 pathway key points
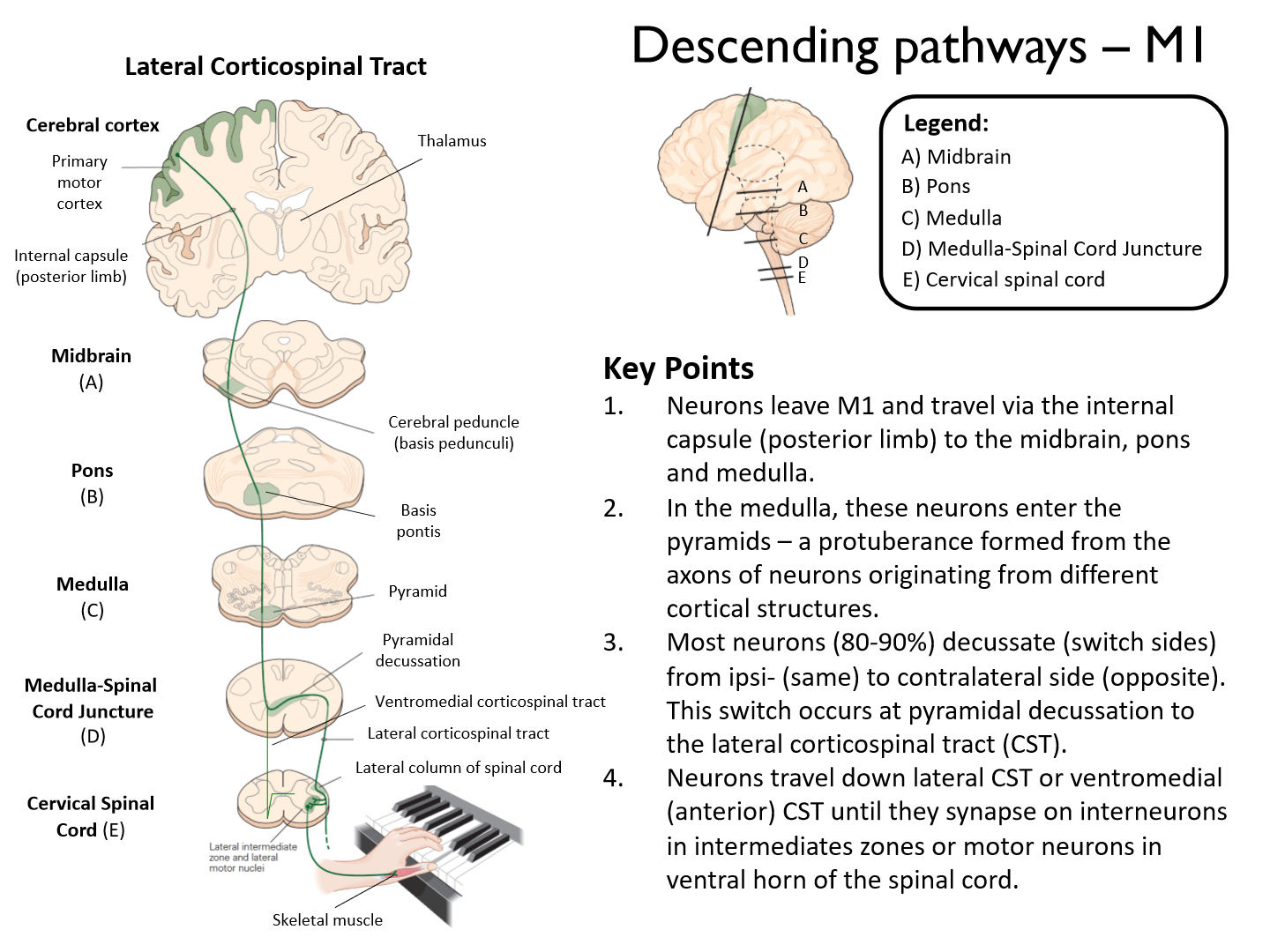
1. Neurons leave M1 and travel via the internal capsule (posterior limb) to the midbrain, pons and medulla.2. In the medulla, these neurons enter the pyramids – a protuberance formed from the axons of neurons originating from different cortical structures.3. Most neurons (80-90%) decussate (switch sides) from ipsi- (same) to contralateral side (opposite). This switch occurs at pyramidal decussation tothe lateral corticospinal tract (CST).4. Neurons travel down lateral CST or ventromedial (anterior) CST until they synapse on interneurons in intermediates zones or motor neurons in ventral horn of the spinal cord
What is the largest contributor to the descending motor tracts?
the corticospinal tracts (CST)
• Lateral CST: account for 80-90% of CST neurons. Control muscles of the appendicular skeleton (muscles of the upper and lower limbs).• Anterior or Ventromedial CST: 10- 20% of CST neurons. Control muscles of the axial skeleton (muscles of the trunk). - proximal
What is the single largest contributor to the CSTs?
*M1 is the single largest contributor to the CSTs. ~36% of CST neurons originate in M1. (30% S1)
- M1 projects axons down the lateral CST to influence generate muscle activity during ongoing motor actions.
Damage to descending neuron above pyramidal decussation affects:
contralateral side of the body.
Damage to lateral CST neuron below pyramidal decussation affects
ipsilateral side of the body
Damage to ventromedial CST neuron below pyramidal decussation affects
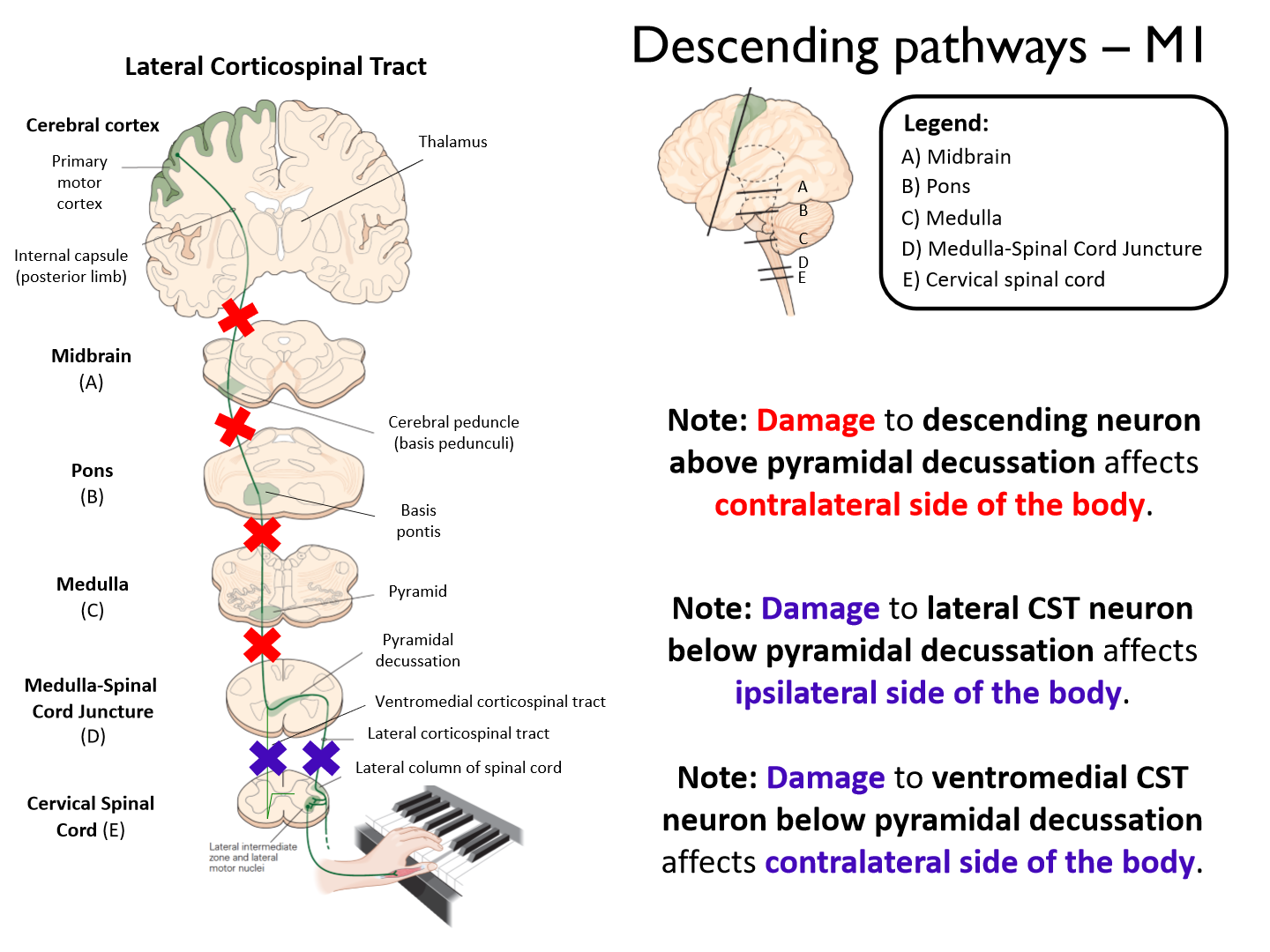
contralateral side of the body.
Diffusion tensor imaging (DTI)
showing strengthening of the corticospinal tracts with music experience.
Stroke in DTI
- Reduction in the density and thickness of CSTs after stroke impacting M1 or descending fibers.
- Clinical symptoms may arise from damage to M1 or the white matter tracts that connect it to the spinal cord.
- Diffusion tensor imaging (DTI) showing degradation of the corticospinal tracts (Wallerian degeneration) post-stroke.
**stop having inputs = die off = NOT useful
UE-FM
is the Upper Extremity Fugl- Meyr assessment score. Large numbers = low impairment.
*larger legion = affect CST more = more impairment
*Overlap between lesion and CST is a significant predictor of functional impairment (also seems to be related to recovery)
Lateral corticospinal tract
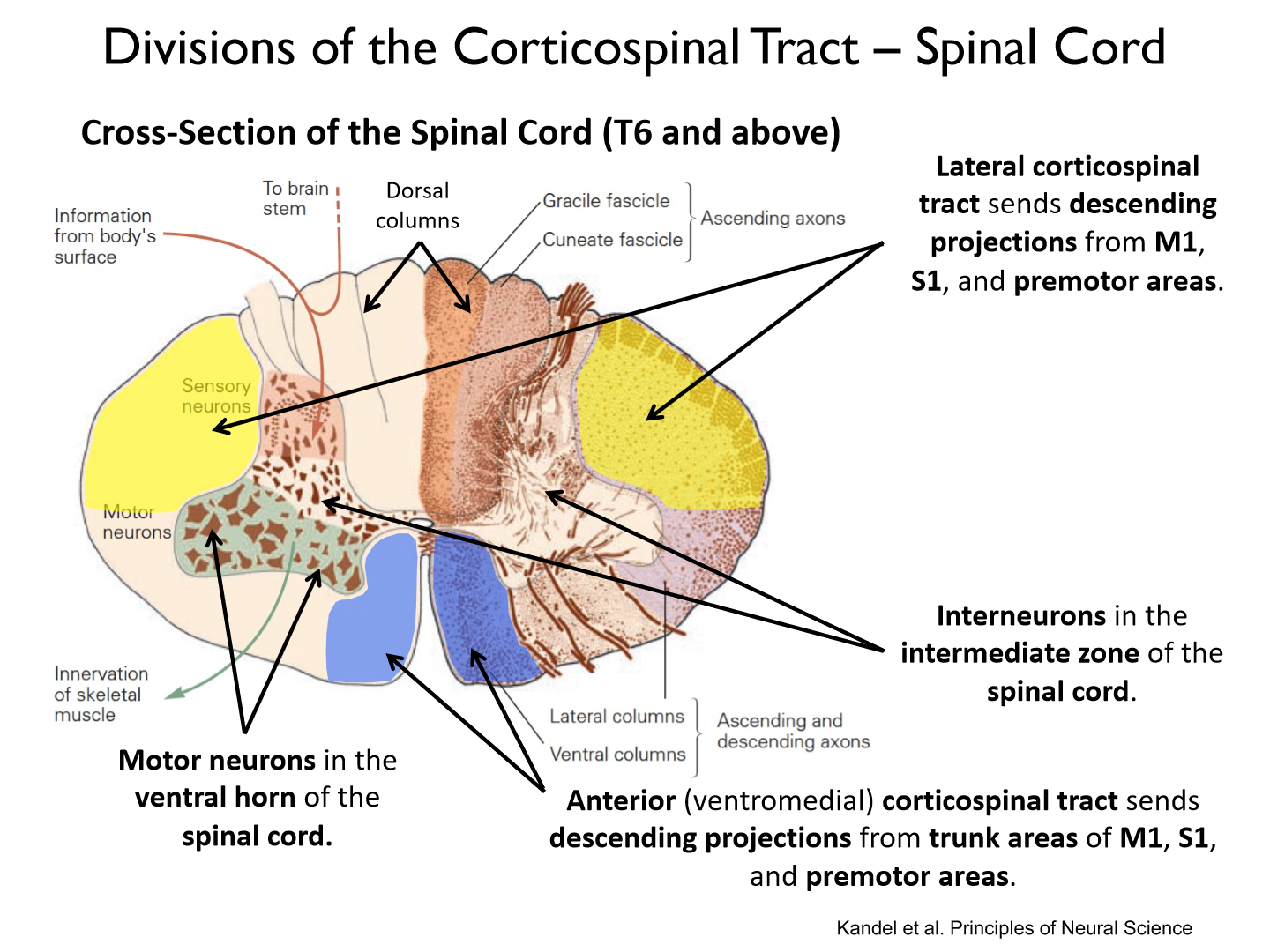
sends descending projections from M1, S1, and premotor areas.
Anterior (ventromedial) corticospinal tract
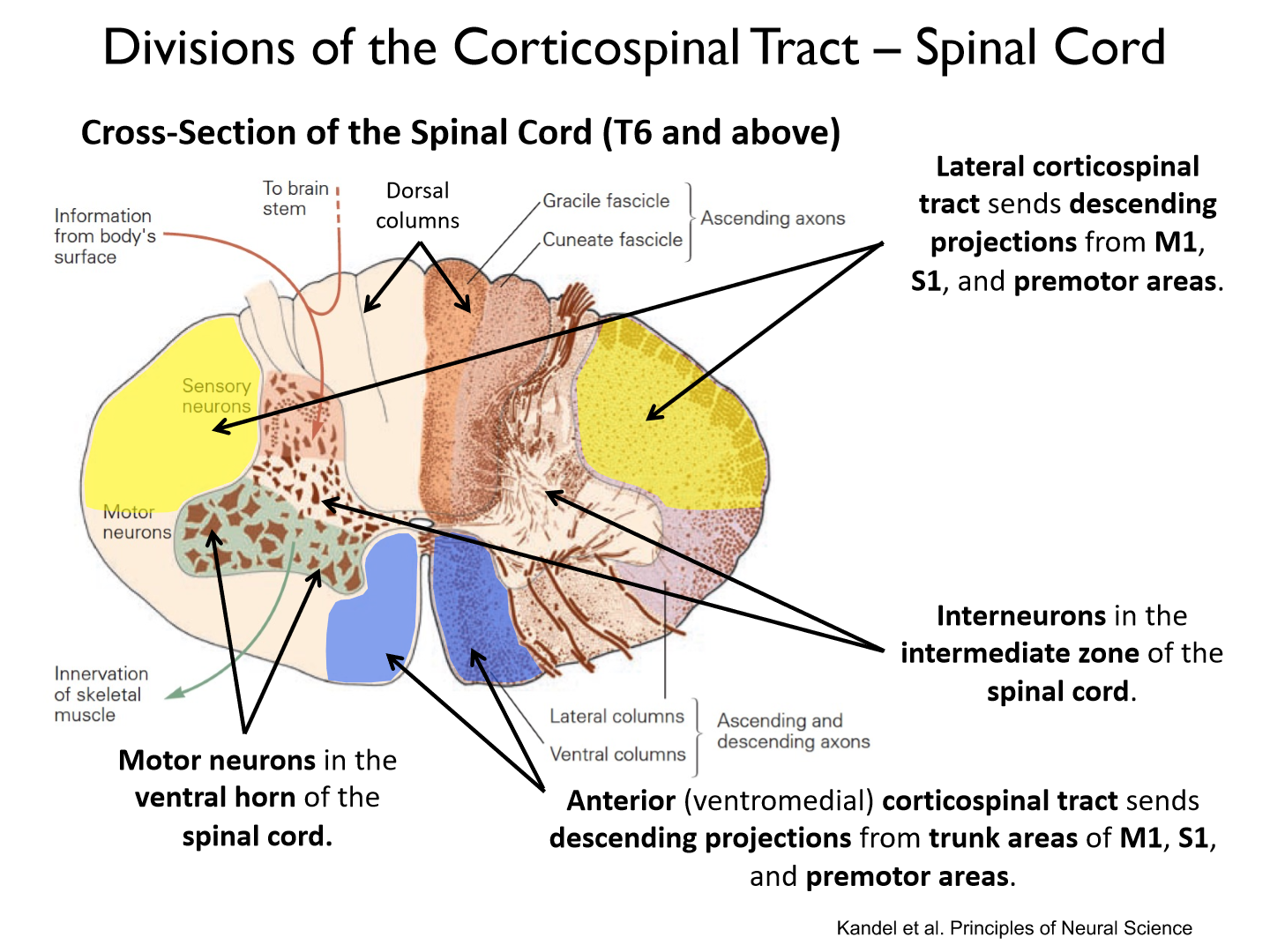
sends descending projections from trunk areas of M1, S1, and premotor areas.
Most lateral corticospinal tract neurons synapse on ___________ in the _______________ of the spinal cord.
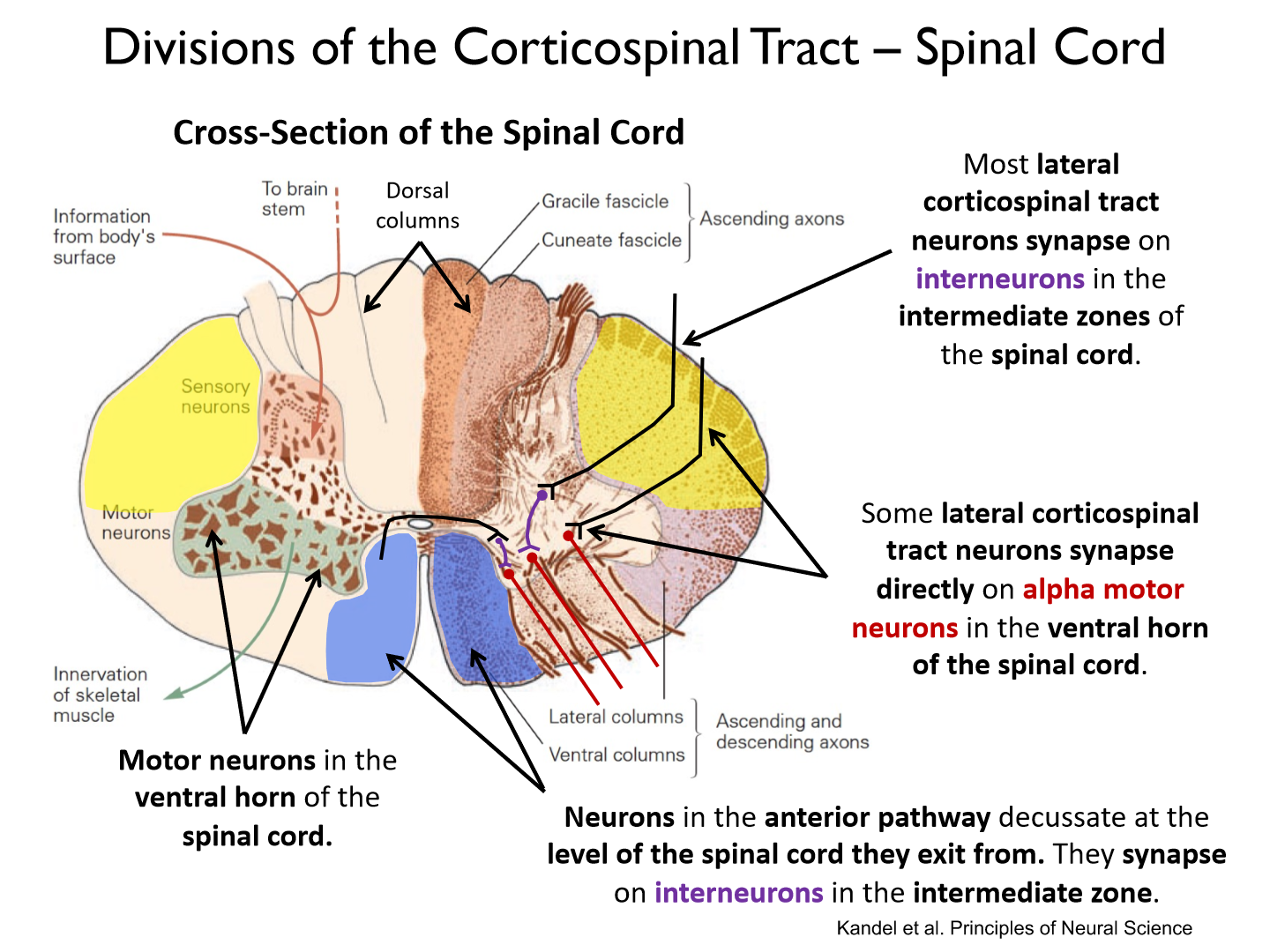
interneurons; intermediate zones
Some lateral corticospinal tract neurons synapse directly on _______________ in the _____________ of the spinal cord.
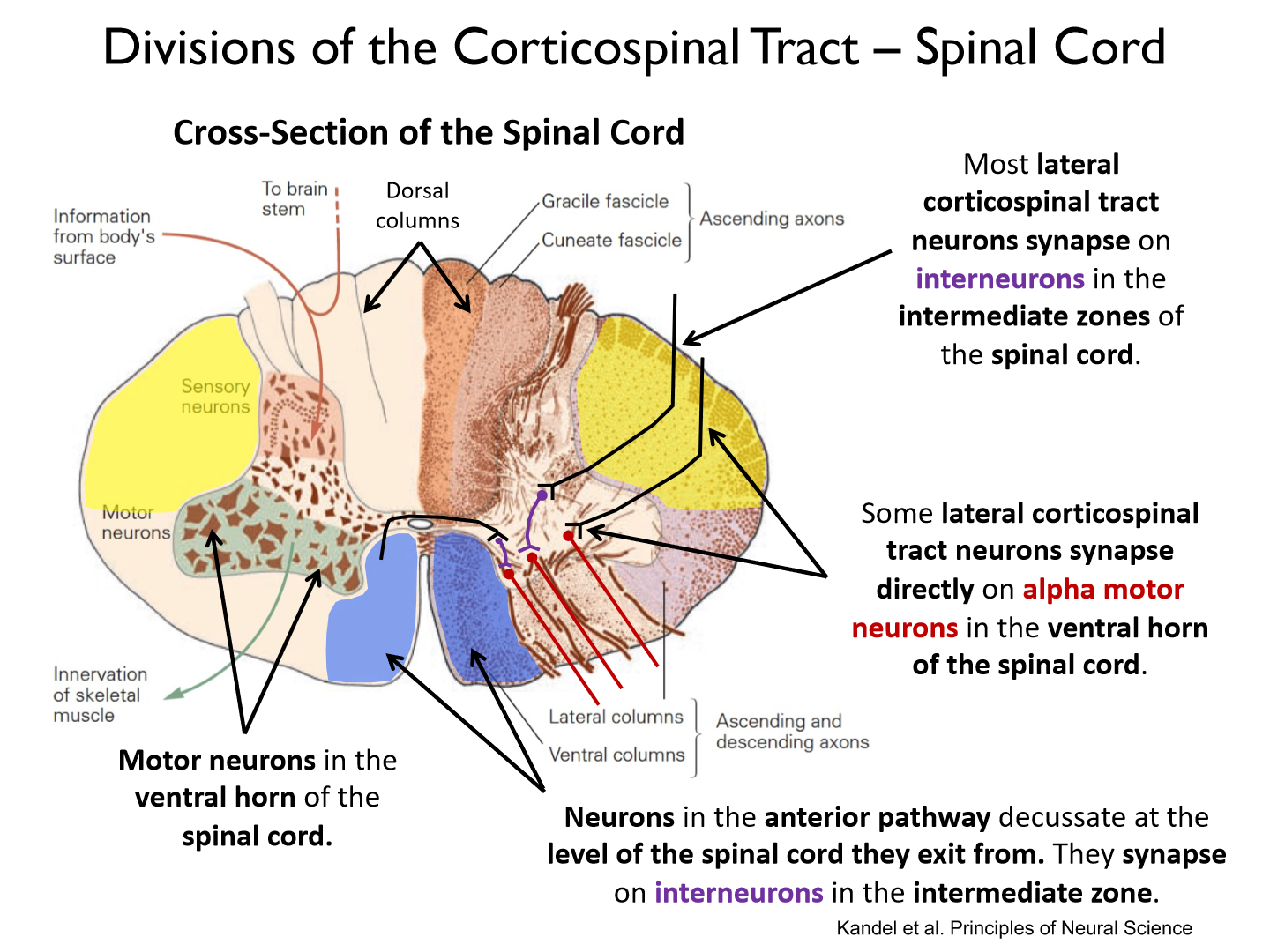
alpha motor neurons; ventral horn
Neurons in the anterior pathway decussate at the _____________________________. They synapse on ______________ in the intermediate zone.
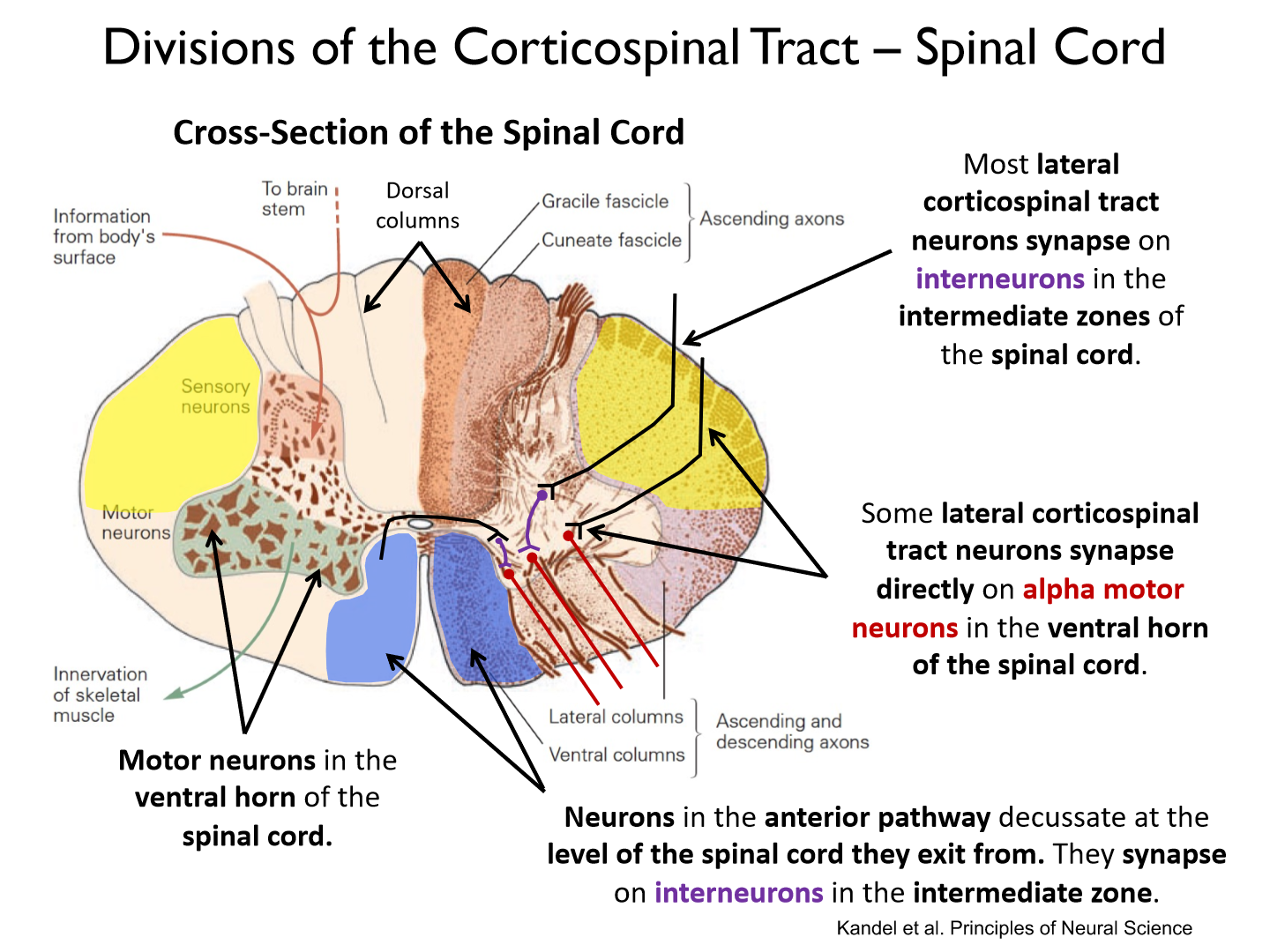
level of the spinal cord they exit from; interneurons
Two types of corticospinal tract (CST) neurons:
1) CST neurons: synapse with interneuron in spinal cord before synapsing with spinal motor neurons.
2) Corticomotoneuronal cells (CM): synapse directly onto spinal (i.e., alpha) motor neurons.
*Travel on the SAME paths
How do we map out neural contributions to the CST?
- Images generated by labelling neurons with viruses and proteins and viewingslices of cortical tissue under a powerful microscope.
- Images show that M1 is the largest contributor to the CSTs of the frontal motor areas.
Overview of viral tracing:
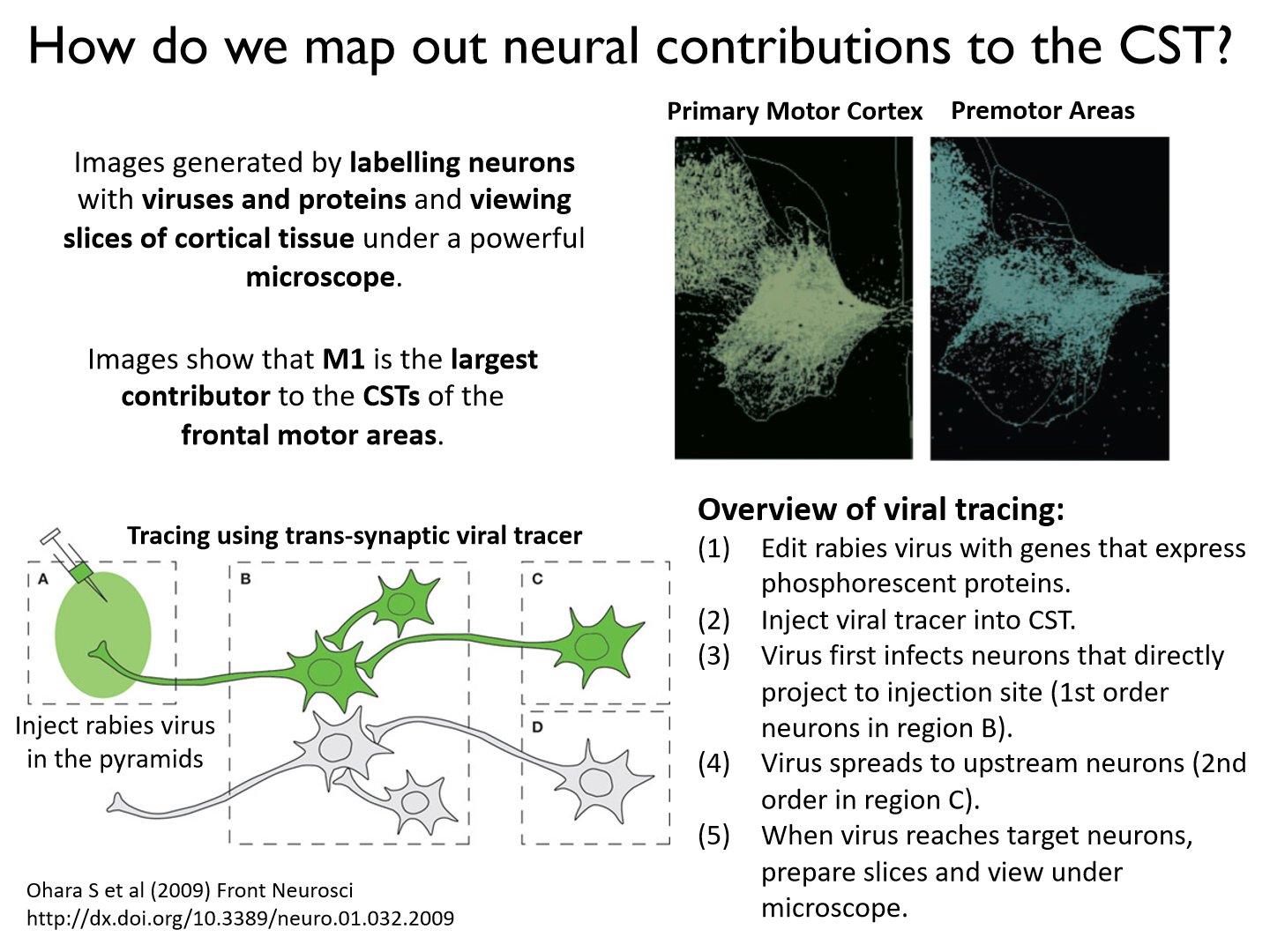
(1) Edit rabies virus with genes that express phosphorescent proteins.(2) Inject viral tracer into CST.(3) Virus first infects neurons that directly project to injection site (1st order neurons in region B).(4) Virus spreads to upstream neurons (2nd order in region C).(5) When virus reaches target neurons, prepare slices and view under microscope.
Pyramidotomy:
A surgical procedure where all descending fibers of the pyramidal tract are severed or otherwise ablated, preventing motor commands from travelling from the brain to the spinal cord or muscles.
* can't do fine motor movements
*prevents information being transmitted to the spinal cord via the corticospinal tracts
Where do corticomotorneural (CM) cells originate?
in M1 along anterior bank of central sulcus
What do CM cells control?
The CM cells that control a single hand muscle are widely distributed throughout the arm motor map and there is extensive overlap in their representations.
What is a source of CM cells?
M1 is a source of CM cells. They originate on the anterior bank of the central sulcus and synapse directly on spinal motor neurons (alpha and gamma motoneurons) that innervate muscles of the contralateral upper arm, forearm and hand.
How do CM cells permit fine control of the hand?
The axon of a single CM cell can synapse with the spinal motor neurons of many different muscles. The connectivity of CM cells permits fine control of the hand.
What are the 3 critical environments that police officers face?
- learning
- testing
- criterion
Is linear pedagogy of self defense training in the police best?
NO! we want to shift towards a nonlinear pedagogy
What are some characteristics of a great police officer?
- rapid cognition
- goal focus
- cue recognition
- visuomotor control
- attentional control
- emotional regulation
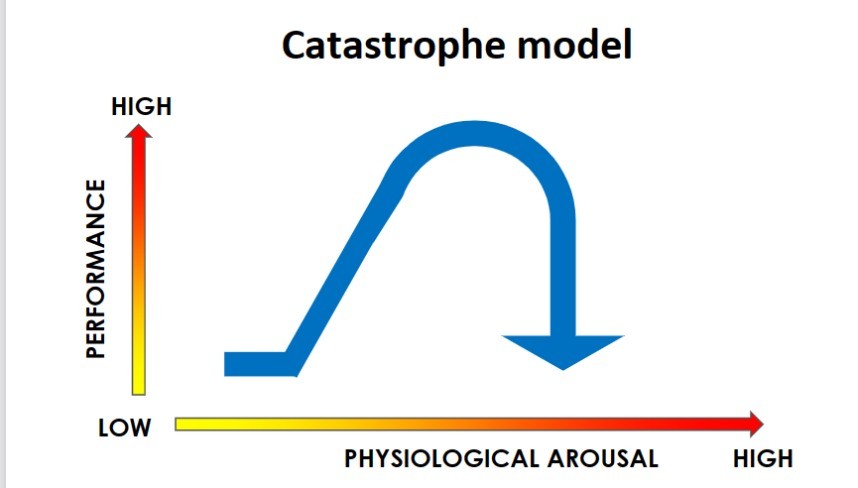
Catastrophe model
Dr. Melis Yilmax Balban
Created a device that monitors stress levels in police and send shock/vibrations when they are too high
Where do we usually see optimal learning?
Moderate stress

Where do expert police look in this scene:
- 1st scan was face
- 2nd scan was hands
- 3rd scan was environment
- 4th scan was hands
**Tactical officers know where to put their attention
Satisficing
Maybe not chosing the best option, but the first one
What are the two systems that work together to direct our decisions?
1. Subconscious: fast, intuitive, emotional, involuntary
2. Conscious: slow, logical, rational, analytical
When in crisis what system is in charge?
system 1, subconscious
- take the first not the best
Hebb's rule
spike timing dependent plasticity
- neurons that fire together, wire together
**non-contextual, siloed, closed repetition builds myelated implicit motor programs, which results in training scars