What are hair cells and what do they detect? (7)
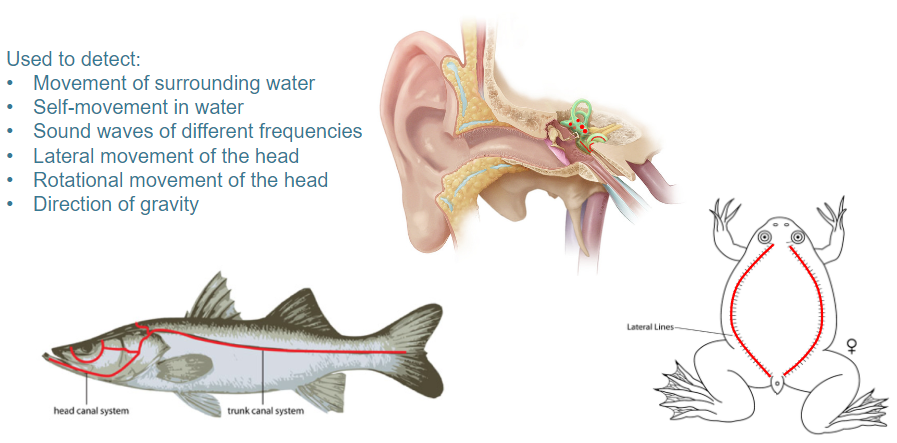
Hair cells are motion-detecting mechanoreceptors that are responsible for detecting:
Movement of surrounding water
Self-movement in water
Sound waves of different frequencies
Lateral movement of the head
Rotational movement of the head
Direction of gravity
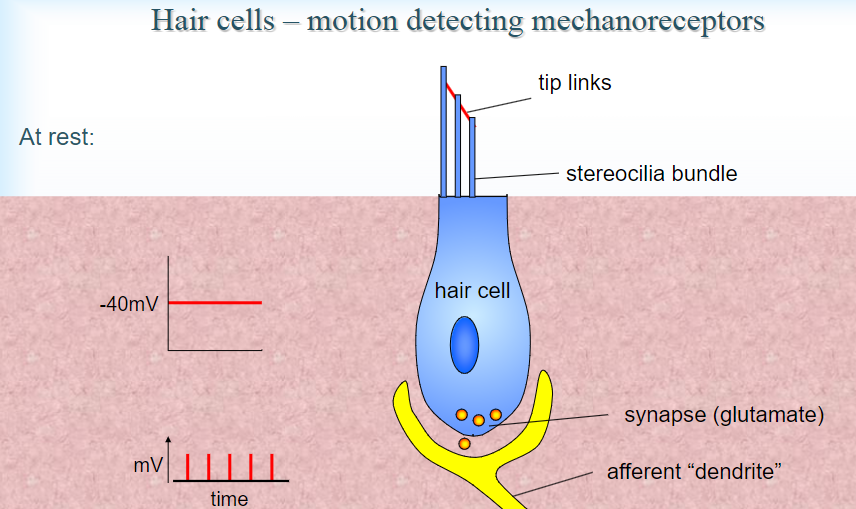
Picture demonstrating Hair cells – motion detecting mechanoreceptors:
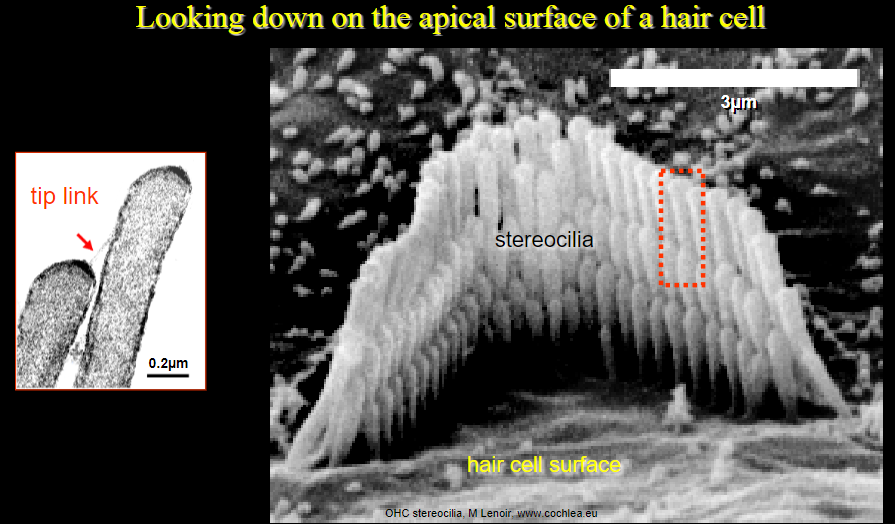
Picture demonstrating Looking down on the apical surface of a hair cell:
How do hair cells function as motion-detecting mechanoreceptors at rest? (4)
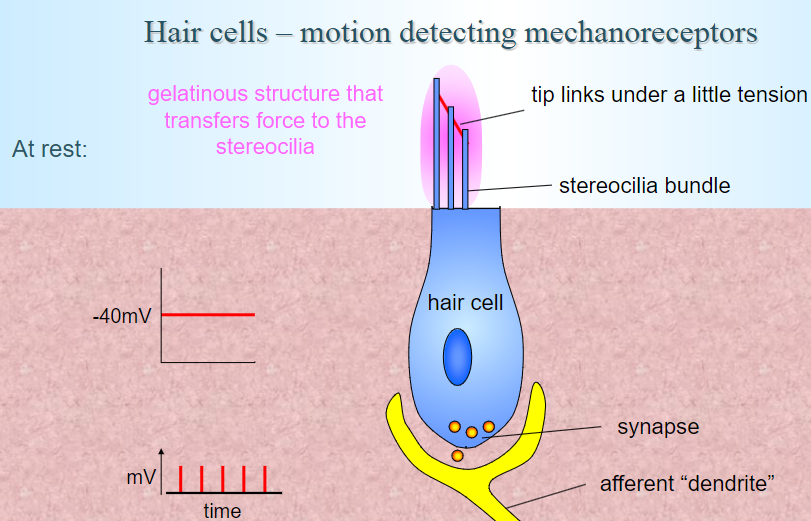
Tip links: Under a slight tension, these connect the stereocilia bundles.
Gelatinous structure: Transfers force to the stereocilia.
Resting membrane potential: The hair cell has a resting potential of around -40mV.
Synapse activity: The synapse connects to an afferent "dendrite," which is involved in transmitting signals to the brain.
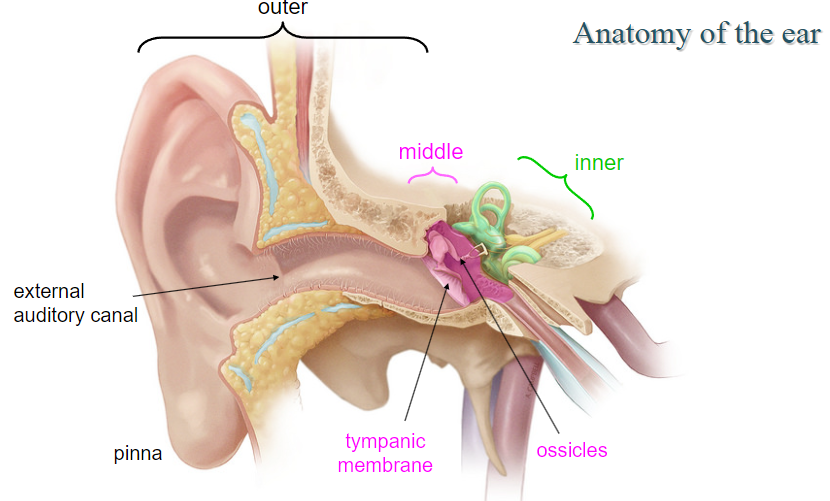
Picture demonstrating the anatomy of the ear:
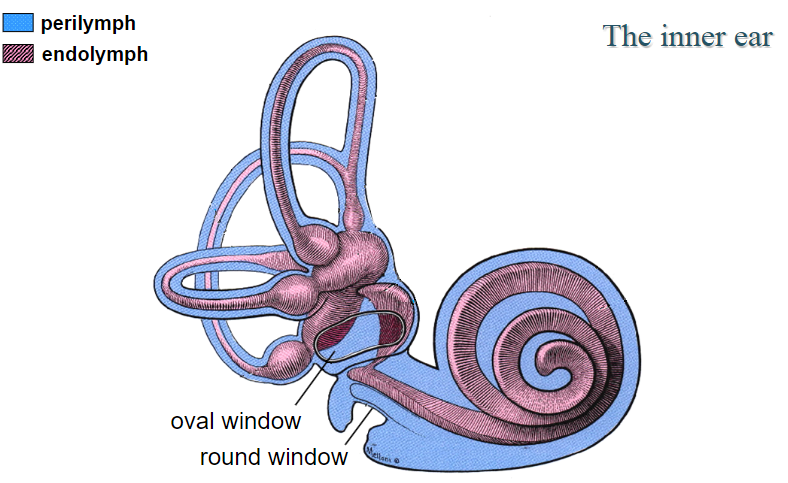
Picture demonstrating the anatomy of the inner ear:
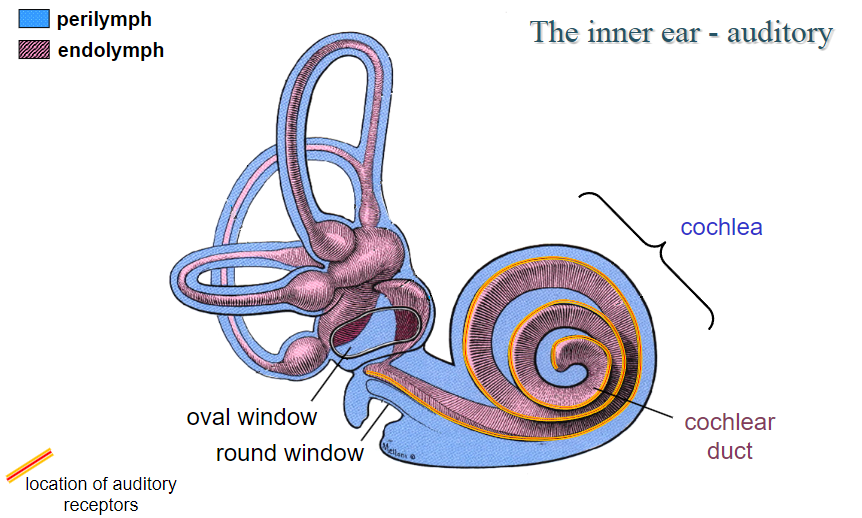
Picture demonstrating the anatomy of the inner ear (auditory picture 1):
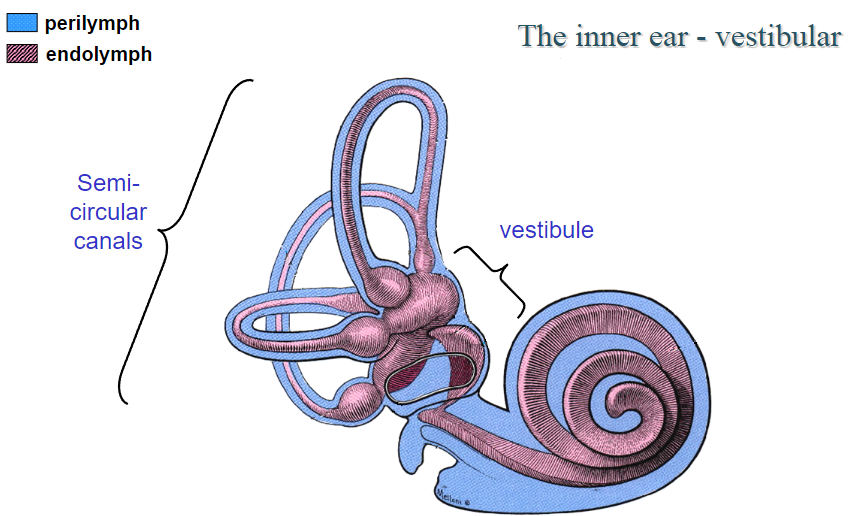
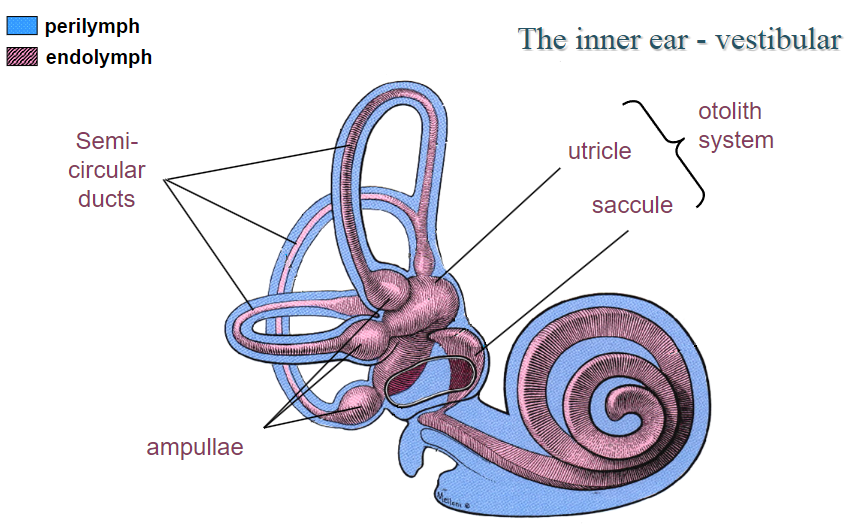
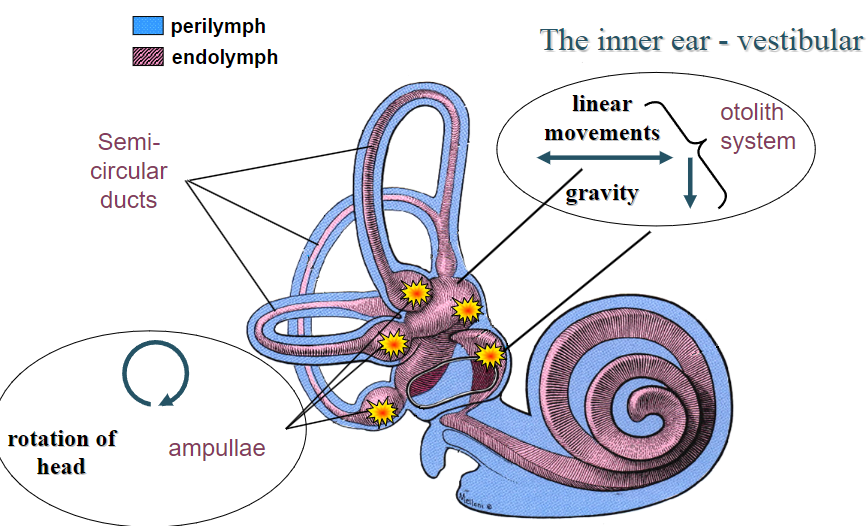
Picture demonstrating the anatomy of the inner ear (vestibular picture 1):
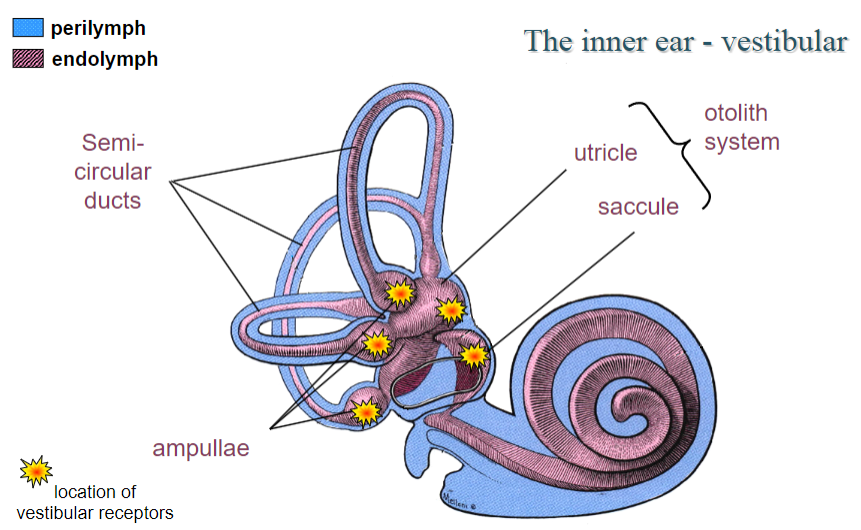
Picture demonstrating the anatomy of the inner ear (vestibular picture 2):
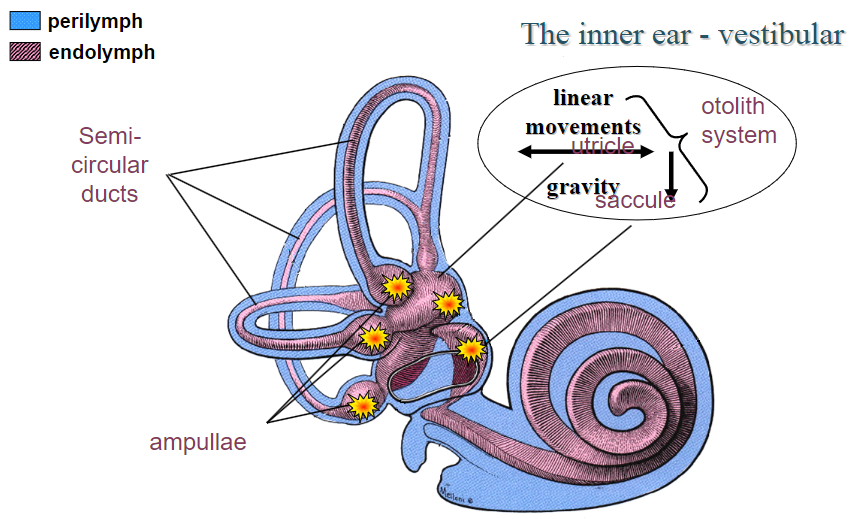
Picture demonstrating the anatomy of the inner ear (vestibular picture 3):
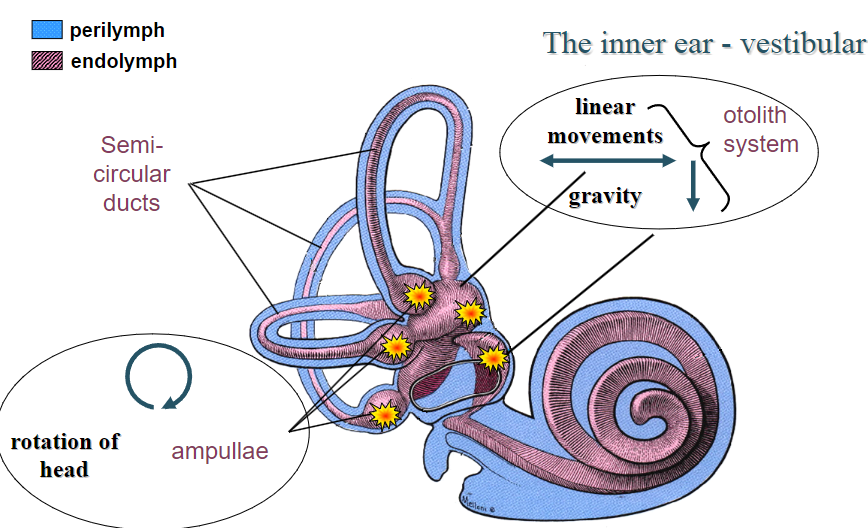
Picture demonstrating the anatomy of the inner ear (vestibular picture 4):
Picture demonstrating the anatomy of the inner ear (vestibular picture 5):
Picture demonstrating the anatomy of the inner ear (vestibular picture 6):
What are the components of the auditory system and their roles? (5)
Pinna: Collects sound waves and directs them into the ear canal.
Tympanic membrane (eardrum): Vibrates in response to sound waves.
Oval window: Vibrations from the tympanic membrane transfer to the inner ear.
Ossicles (malleus, incus, stapes): Amplify sound vibrations.
Cochlea: Converts sound vibrations into neural signals.
What is conductive hearing loss? (2)
Definition: A blockage or damage that prevents sound waves from reaching the oval window.
Common causes: Blockage in the ear canal, fluid in the middle ear, otitis media, or damage to ossicles.
What structures are located in the inner ear and their functions? (6)
Cochlea: Contains auditory receptors and is responsible for converting sound waves into neural signals.
Perilymph: Fluid surrounding the cochlear duct.
Endolymph: Fluid inside the cochlear duct.
Cochlear duct: Location of the auditory receptors.
Round window: Helps dissipate sound pressure.
Cochlear branch of the vestibulocochlear nerve: Transmits auditory information from the cochlea to the brain.
What is the structure and function of the spiral organ (organ of Corti)? (7)
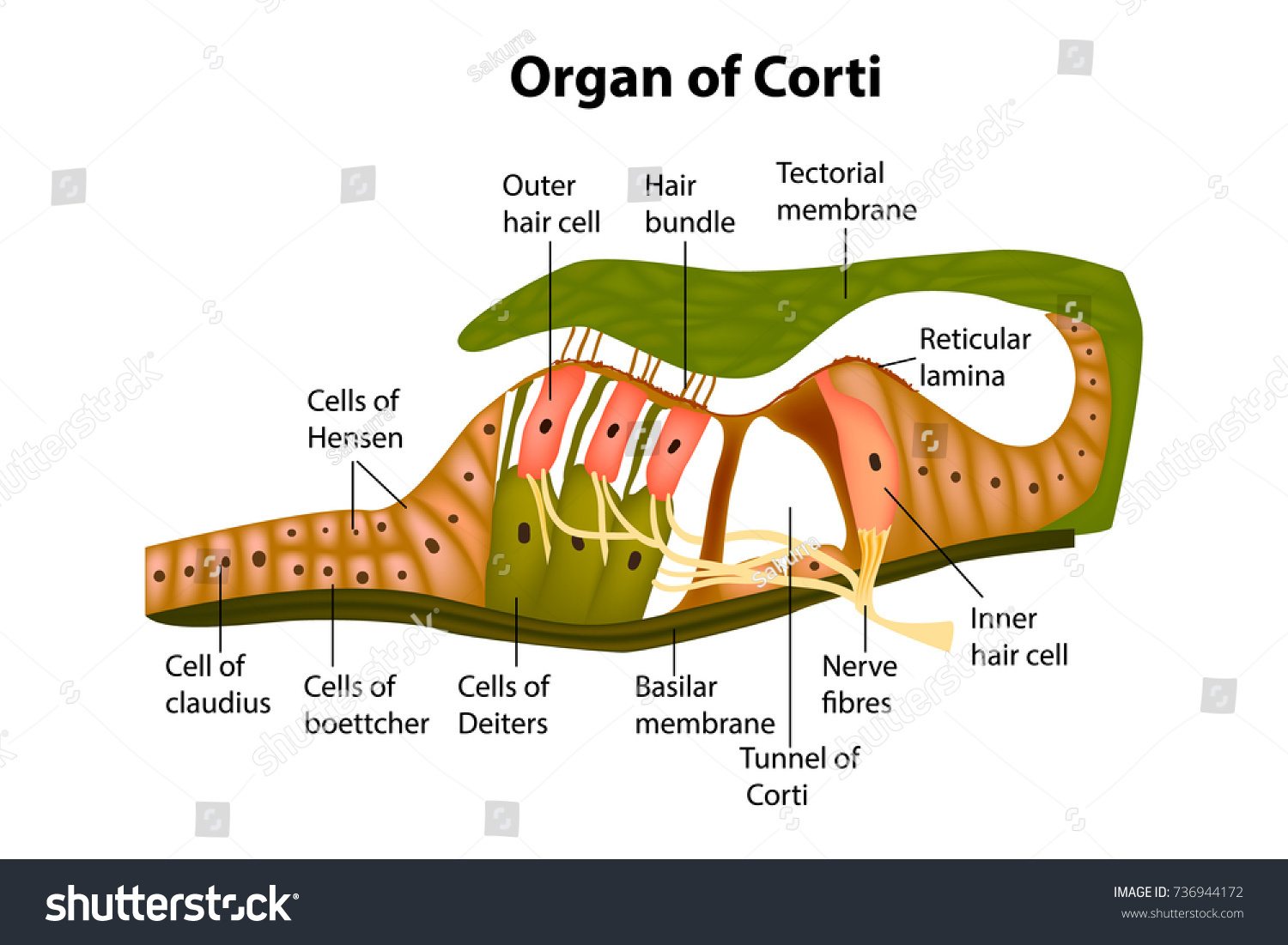
Basilar membrane: Supports hair cells and vibrates in response to sound.
Tectorial membrane: Provides support for stereocilia.
Stereocilia: Hair-like projections that detect sound vibrations.
Inner hair cells: Convert sound vibrations into electrical signals.
Outer hair cells: Amplify sound vibrations through mechanical feedback.
Support cells: Help maintain the structure of the organ.
Vestibular membrane: Separates the cochlear duct from the scala vestibuli.
What is the place code in the cochlea? (3)
Frequency encoding: Different parts of the basilar membrane vibrate at different frequencies.
Base of cochlea: Narrow and stiff, responds to high frequencies (~20kHz).
Apex of cochlea: Broad and flexible, responds to low frequencies (~20Hz).
How does the auditory system encode different qualities of sound? (4)
Frequency: Encoded by the place code (location of hair cells on the basilar membrane).
Loudness: Encoded by the firing rate of action potentials (more firing = louder sound).
Timing: Preserved by fast axons and synapses, essential for detecting the timing of sounds.
Origin: Encoded by the superior olivary nuclei which compare sound input from both ears.
How do the medial and lateral superior olivary nuclei contribute to sound localization? (2)
Medial superior olivary nuclei: Compare the timing of sounds reaching both ears (important for localizing low-frequency sounds).
Lateral superior olivary nuclei: Compare the loudness of sounds in both ears (important for localizing high-frequency sounds).
What is the pathway for sound localization? (5)
Cochlear nuclei: Receive input from the cochlear nerve.
Superior olivary nuclei: Process sound information for localization.
Inferior colliculus: Integrates auditory information and assists in sound localization.
Medial geniculate nucleus: Relays sound information to the auditory cortex.
Primary auditory cortex: Processes sound information in the temporal lobe.
What is the role of outer hair cells in the cochlea? (3)
Amplify sound: Outer hair cells amplify sound vibrations through mechanical feedback.
Electromotility: Outer hair cells change their length in response to sound, enhancing the movement of the basilar membrane.
Improve sensitivity: Outer hair cells increase the cochlear sensitivity to quiet sounds.
What are some conditions that can damage hair cells? (3)
Loud sounds: Can cause mechanical damage to hair cells.
Genetic conditions: Some genetic disorders can lead to the loss of hair cells.
Age-related hearing loss: Over time, hair cells naturally degrade.
What are cochlear implants and when are they used? (3)
Cochlear implants: Devices that bypass damaged hair cells and directly stimulate the auditory nerve.
Used for: Severe sensorineural hearing loss, particularly when hair cells in the cochlea are non-functional.
Benefit: Restores hearing by converting sound into electrical signals that stimulate the auditory nerve.
How do vibrations in the cochlea affect the hair cells? (2)
Vibration of the basilar membrane: Causes tilting of the stereocilia on hair cells.
Depolarization: When the stereocilia bend, ion channels open, leading to depolarization of the hair cells and triggering action potentials.
What is the role of afferent fibers in the auditory system? (2)
Transmit signals: Afferent fibers carry electrical signals from the inner hair cells to the brain.
Essential for hearing: The brain interprets these signals to perceive sound.
What is the tonotopic organization of the auditory cortex? (3)
Tonotopic mapping: Different frequencies are processed in different regions of the auditory cortex.
High frequencies: Processed in the anterior part of the cortex.
Low frequencies: Processed in the posterior part of the cortex.
What is the vestibular system and its primary components? (2)
The vestibular system is responsible for detecting changes in head position and movement to help maintain balance and coordinate eye movements.
Primary components: Perilymph, endolymph, utricle, saccule, otolith system, semi-circular canals, ampullae, and hair cells.
What are the functions of the perilymph and endolymph in the vestibular system? (2)
Perilymph: Found in the space between the bony labyrinth and membranous labyrinth; provides structural support.
Endolymph: Found within the membranous labyrinth; aids in the transduction of mechanical movements into neural signals.
What are otolith organs and their role in the vestibular system? (4)
Otolith organs (utricle and saccule) detect linear acceleration and the direction of gravity.
They contain hair cells embedded in a gelatinous membrane (otolithic membrane) with otoconia (crystals) that provide mass and inertia.
The macula of the utricle and saccule detect changes in the head's linear movements.
The otolith system helps maintain upright posture and compensates for externally induced movements.
Describe the macula of the otolith system. (3)
The macula contains hair cells that are oriented in different directions to detect changes in head position.
Each hair cell is activated by linear movements, either in the utricle or saccule.
Hair cells project afferent signals to the vestibular nuclei and via the vestibulospinal tract to motor neurons.
How do otolith organs detect linear acceleration and gravity? (3)
During linear acceleration, the otoliths lag behind movement due to inertia.
As the head decelerates, the otoliths continue to move due to inertia.
The direction of gravity is detected when the otoliths shift in response to the head tilting.
What is the role of the vestibulospinal tract in the vestibular system? (2)
The vestibulospinal tract carries afferent signals from the otolith organs to motor neurons controlling the trunk and legs.
It helps maintain postural stability, particularly in response to changes in body position.
What is the function of the semi-circular canal system? (3)
The semi-circular canals detect angular acceleration of the head in three dimensions (anterior, posterior, and horizontal canals).
They consist of hair cells located in the ampulla, surrounded by endolymph and perilymph.
The canals help detect rotational movements by measuring the delay of endolymph fluid movement in response to head turns.
Describe the structure of the semi-circular canal ampulla. (3)
The ampulla is a swelling at the end of each semi-circular canal.
It contains the crista ampullaris, a structure with hair cells embedded in a gelatinous membrane called the cupula.
The movement of the endolymph during head rotation causes deflection of the hair cells, leading to neural activation.
How do movements of the head activate the hair cells in the semi-circular canal? (3)
When the head rotates, the endolymph fluid inside the canals lags behind.
This causes the cupula (gelatinous membrane) to bend, which deflects the hair cells.
The bending of hair cells alters the firing rate of afferent nerves, signaling the direction and velocity of head movement.
How is the direction of movement encoded in the semi-circular canal system? (2)
Each semi-circular canal detects rotation along a specific axis (anterior, posterior, or horizontal).
The arrangement of the canals allows for the detection of all possible rotational movements of the head.
What are the main outputs of the vestibular system in terms of motor control? (4)
The vestibular system projects afferent signals via the vestibulospinal tracts to control posture and movement.
It regulates eye movements through the vestibulo-ocular reflex (VOR) to stabilize the gaze.
It coordinates the movements of neck and shoulder muscles to maintain head stability.
It helps control the movement of limbs by adjusting posture in response to changes in head position.
What is the vestibulo-ocular reflex (VOR)? (3)
The VOR helps maintain stable vision during head movements by coordinating eye movements in the opposite direction of head rotation.
The VOR involves the oculomotor (CN III), abducens (CN VI), and vestibular nuclei.
It ensures that the gaze remains steady and compensates for head movements, contributing to visual stability.
What are conjugate eye movements and their connection to the vestibular system? (3)
Conjugate eye movements, such as smooth pursuit, are coordinated movements of both eyes in the same direction.
The vestibular system helps guide smooth pursuit movements through signals sent from the vestibular nuclei to the extraocular muscles.
These eye movements are critical for maintaining visual stability during head or body movements.
How does the vestibular system contribute to eye movement control? (4)
The vestibular system ensures the stability of gaze during head movements through the vestibulo-ocular reflex.
It controls the extraocular muscles via the vestibular nuclei and medial longitudinal fasciculus.
It coordinates movements of both eyes to maintain visual focus.
It helps adjust the speed and direction of eye movements, such as during smooth pursuit or saccades.
What is the role of the medial longitudinal fasciculus in the vestibular system? (2)
The medial longitudinal fasciculus is a neural pathway that connects the vestibular nuclei with the oculomotor and abducens nuclei, which control eye movements.
It ensures the coordination of eye movements with head movements for stable vision, and its dysfunction can lead to issues like nystagmus or double vision.
What is the relationship between the vestibular system and multiple sclerosis? (2)
The pathways involved in the vestibular system require rapid conduction and are heavily myelinated.
Damage to the myelinated pathways, such as in multiple sclerosis, can impair vestibular function and affect balance, coordination, and eye movement stability.
What are the effects of head stability and visually-guided movements on the vestibular system? (3)
The vestibular system helps maintain head stability by compensating for head and body movements, ensuring that the visual field remains steady.
It adjusts the activity of eye muscles to keep the gaze focused during head movements.
It plays a key role in coordinating visually-guided movements, allowing smooth and accurate tracking of objects in space.
What is a receptor and its significance? (2)
A protein complex that binds to and is activated by a signaling molecule.
A nerve cell that detects external stimuli and converts it into a receptor potential.
What is a primary afferent? (1)
The first cell in the sensory pathway that transmits sensory signals from the sensory apparatus to the cerebral cortex.
What is threshold and its different types? (3)
Action potential threshold: The depolarization level necessary to trigger an action potential (approximately -50mV).
Minimum sensory input threshold: The least sensory input needed to activate a receptor.
Perceptual threshold: The minimum sensory input required for conscious perception, dependent on both receptor activation and attention.
What is sensitivity and how does it relate to sensory systems? (2)
The relative responsiveness of a sensory system to stimuli.
High sensitivity correlates with lower response thresholds and larger responses to stimuli.
What is specificity in sensory systems? (1)
The ability of a system to differentiate between similar stimuli.
What is receptor adaptation and why is it important? (3)
The process where receptors adjust their responses to constant stimuli.
Some adapt quickly (e.g., Pacinian corpuscles), others slowly (e.g., cone photoreceptors).
Helps extend dynamic range and save energy.
What is lateral inhibition and its purpose in sensory systems? (2)
A mechanism where excitation of one part of a pathway inhibits its neighbors.
Enhances contrast and allows small differences in stimuli to be detected.
What is dynamic range? (1)
The range of stimulus strengths a sensory system can respond to, extended through receptor sensitivity and adaptation.
What is saturation in sensory systems? (1)
The point at which a sensory system reaches its maximum response, beyond which it can't distinguish stronger stimuli.
What is synaptic plasticity and how does it function? (2)
Changes in synaptic strength due to activity patterns.
Long-term potentiation (LTP) increases synapse strength by enhancing transmitter availability and receptor effectiveness.
What is a specific circuit/pathway? (1)
A neural circuit involved in processing sensory, motor, or cognitive information.
What is a modulatory pathway? (2)
Neural inputs that adjust a cell's response to sensory or motor input.
Crucial for regulating sleep, attention, mood, and emotions, impacting motor and cognitive functions.