Define anxiety and its severity levels. (2)
A feeling of unease, such as worry or fear.
Can range from mild to severe.
How can anxiety be a beneficial adaptive response? (2)
Anxiety serves as a learned response to avoid harmful experiences (e.g., not touching a hot stove).
Acts as an innate response to threatening stimuli, enhancing alertness and defensive behaviours.
What are the components of an innate fear response? (4)
Defensive behaviours.
Autonomic reflexes.
Increased alertness.
Innate and species-specific fears.
Can fear responses occur without stimuli? (2)
Yes, fear can be anticipatory.
Fear responses are not always appropriate to the situation.
When does anxiety become a problem? (6)
Anxiety becomes a problem when it is:
Chronic and irrational.
Linked to social disturbances.
Causes avoidance behaviours.
Accompanied by incessant worry.
Leads to concentration or memory problems.
Intense and disproportionate to its source.
What is anxiety, and what are its symptoms? (11)

Psychological: Anxiety involves feelings of unease, worry, or fear.
Physiological: Symptoms include:
Tachycardia
Shortness of breath
Excessive sweating
Trembling or shaking
Headache and dizziness
Pins and needles
Gastrointestinal disturbances
Nausea
Fatigue
Insomnia
What types of food and drink can trigger symptoms of anxiety? (2)

Sugar
Caffeine
How can physical and mental health problems contribute to anxiety? (2)

Physical health problems, such as chronic conditions, can trigger or exacerbate anxiety.
Mental health conditions, such as depression, can also trigger or worsen anxiety.
How can past experiences contribute to anxiety? (1)

Difficult experiences in childhood, adolescence, or adulthood are common triggers for anxiety.
How can everyday life and habits contribute to anxiety? (1)

Current issues or problems in daily life can lead to anxiety.
How can alcohol and drugs contribute to anxiety symptoms? (2)

Recreational drugs of abuse (e.g. psychostimulants) can trigger anxiety symptoms via mechanisms specific to each drug or class of drugs.
Alcohol, as a CNS depressant, increases GABAergic neurotransmission and blocks glutamatergic neurotransmission, disrupting the balance between GABA and glutamate in the brain.
How does the imbalance between GABA and glutamate contribute to anxiety when alcohol is consumed? (2)
Alcohol disrupts the balance between GABA and glutamate, which is crucial for optimal brain function.
The brain adapts to counteract this imbalance, leading to low levels of GABA and high levels of glutamate, which can trigger anxiety symptoms.
How can genetics contribute to the symptoms of anxiety? (2)
Research has linked genetic factors to several anxiety disorders (e.g. panic disorder) (Na et al., 2011).
Anxiety disorders are not based on a single gene but likely have a complex genetic basis, which can be affected by environmental factors.
What is the pathophysiology of anxiety? (6)
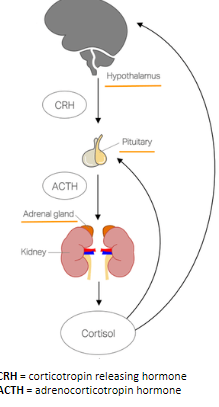
The hallmark of anxiety disorders is an inappropriate stress response, either when a stressor is not present or not immediately threatening.
The stress response is the coordinated reaction to threatening stimuli and is regulated by the hypothalamus-pituitary-adrenal (HPA) axis.
The HPA axis regulates the release of cortisol (a glucocorticoid), which contributes to the body’s physiological response to stress.
The activation of CRH (corticotropin releasing hormone) in the hypothalamus plays a key role in regulating the stress response:
Overexpressing CRH in rodent models leads to increased anxiety-like behaviors.
Knocking out CRH receptors in rodent models leads to fewer anxiety-like behaviors.
What is the role of the amygdala and hippocampus in the pathophysiology of anxiety? (6)

Amygdala:
Plays a key role in emotion and the fear response.
Stimulates the HPA axis to promote cortisol release.
Amygdala hyperactivity is linked to anxiety disorders.
Hippocampus:
Plays a key role in learning and memory.
Suppresses the HPA axis to prevent excessive cortisol release.
Hippocampus underactivity is linked to anxiety disorders.
What are the main categories of anxiety disorders in the DSM-5 2013 classification? (3)
Anxiety disorders
Obsessive-compulsive disorders
Trauma and stressor-related disorders
What are the anxiety disorders in the DSM-5 2013 classification? (4)
Generalized anxiety disorder (GAD)
Specific phobias
Social phobias
Panic disorder
What other anxiety disorders are included in the DSM-5 2013 classification? (2)
Substance/medication-induced anxiety disorder
Anxiety disorder due to a medical condition
What are the obsessive-compulsive disorders in the DSM-5 2013 classification? (1)
Obsessive-compulsive disorder (OCD)
What other obsessive-compulsive disorders are included in the DSM-5 2013 classification? (3)
Body dysmorphic disorder
Hoarding disorder
Trichotillomania (hair-pulling disorder)
What are the trauma and stressor-related disorders in the DSM-5 2013 classification? (1)
Post-traumatic stress disorder (PTSD)
What are the key features of Generalized Anxiety Disorder (GAD)? (5)
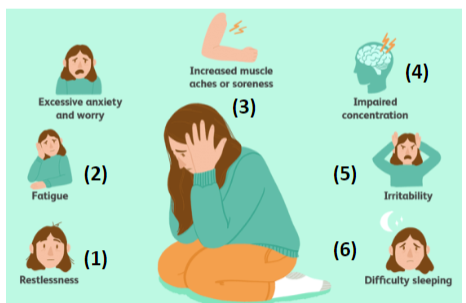
Excessive anxiety and worry occurring for at least six months, which is difficult to control and impairs activities of daily living.
Associated with three or more of six symptoms (unspecified in the prompt).
Symptoms are not attributable to a substance or medical condition.
Symptoms are not better explained by another type of anxiety disorder.
GAD sufferers' symptoms are likely to differ from one person's experience to another.
What are the key features of specific phobias? (4)

Extreme fears or anxieties provoked by exposure to a particular situation or object, often leading to avoidance behaviors.
The phobic object or situation almost always provokes immediate fear or anxiety, out of proportion to the actual danger.
Phobia is persistent, typically lasting at least six months, impairing activities of daily living.
Symptoms are not attributable to a substance or medical condition and are not better explained by another type of anxiety disorder.
What are some examples of specific phobias? (5)

Acrophobia (fear of heights)
Ornithophobia (fear of birds)
Trypanophobia (fear of needles)
Nomophobia (fear of being without a mobile phone)
Triskaidekaphobia (fear of the number 13)
What are the key features of social phobias? (4)
Significant anxiety provoked by exposure to certain types of social or performance situations.
Social situations almost always provoke immediate fear or anxiety, out of proportion to the actual danger.
The phobia is persistent, typically lasting at least six months, impairing activities of daily living.
Symptoms are not attributable to a substance or medical condition and are not better explained by another type of anxiety disorder.
What types of social situations may trigger social phobia? (3)
Social interactions
Performing in front of others
Being observed
What are the key features of panic disorder? (7)
Recurring panic attacks without a clear cause or trigger.
A panic attack is an abrupt surge of intense fear or discomfort, reaching a peak within minutes.
Associated with four or more of thirteen symptoms as per the DSM-5, including:
Increased heart rate
Sweating
Trembling/shaking
Shortness of breath
Fear of dying
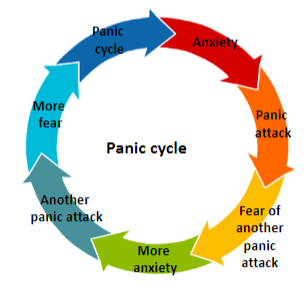
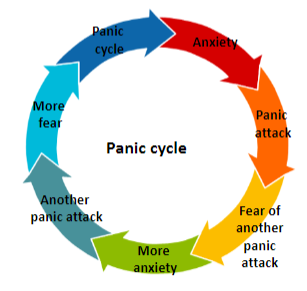
What is the panic cycle in panic disorder? (4)
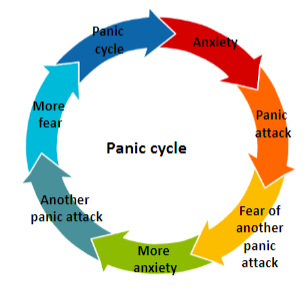
Anxiety
Panic attack
Fear of another panic attack
More anxiety leading to another panic attack, and so on, continuing the cycle.
When can panic attacks occur in panic disorder? (2)
Panic attacks can occur spontaneously.
Panic attacks can also be a feature of other anxiety disorders.
What are the key features of obsessive-compulsive disorder (OCD)? (4)
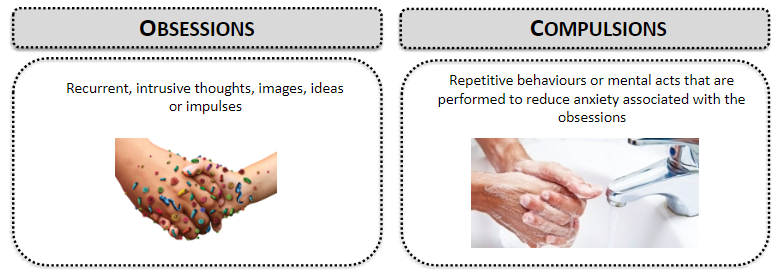
OCD is characterized by compulsive, ritualistic behavior driven by irrational anxiety.
Obsessions and compulsions are time-consuming, typically taking over an hour per day, impairing activities of daily living.
OCD is not attributable to a substance or medical condition and is not better explained by another type of anxiety disorder.
Recurrent, intrusive thoughts, images, ideas, or impulses are typical of obsessions.
What are obsessions in OCD? (1)
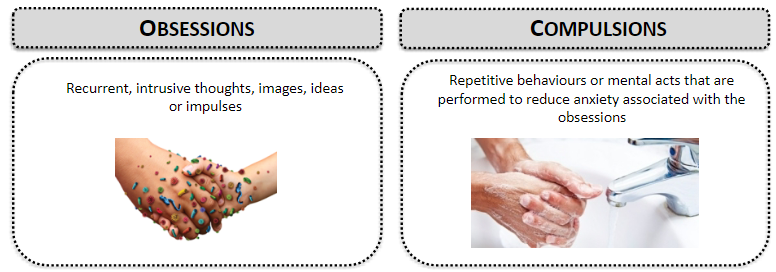
Recurrent, intrusive thoughts, images, ideas, or impulses.
What are compulsions in OCD? (1)
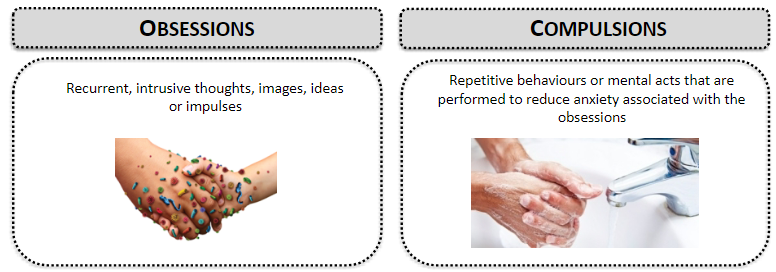
Repetitive behaviors or mental acts performed to reduce anxiety associated with the obsessions.
What are the key features of post-traumatic stress disorder (PTSD)? (4)
PTSD is characterized by distress triggered by the recall of past traumatic experiences.
Disturbances persist for at least one month, impairing activities of daily living.
PTSD is not attributable to a substance or medical condition.
Triggered by exposure to certain situations, such as actual or threatened death, serious injury, or sexual violence. Exposure may be direct, as a witness, or by learning that a close family member or friend experienced the traumatic event.
What are the intrusion symptoms associated with PTSD? (4)
Recurrent intrusive memories
Nightmares
Dissociative reactions (e.g., flashbacks)
Psychological and physiological distress at exposure to cues resembling the traumatic event.
What are the two main categories of treatment for anxiety disorders? (2)
Psychological: Cognitive behavioural therapy (CBT)
Pharmacological: Anxiolytics
What are the main classes of anxiolytic drugs? (3)
Benzodiazepines
5-HT1A receptor agonists
b -noradrenergic receptor antagonists
What is the role of Benzodiazepines in treating anxiety? (1)
Benzodiazepines act as GABAA receptor modulators, enhancing the effects of the neurotransmitter GABA to reduce anxiety.
What is the role of 5-HT1A receptor agonists in treating anxiety? (1)
5-HT1A receptor agonists target serotonin receptors, helping to regulate mood and anxiety.
What is the role of b -noradrenergic receptor antagonists in treating anxiety? (1)
b -noradrenergic receptor antagonists work by blocking certain noradrenergic receptors, helping to reduce the physiological symptoms of anxiety.
What is the GABAA receptor and its role in anxiolytic drugs? (1)
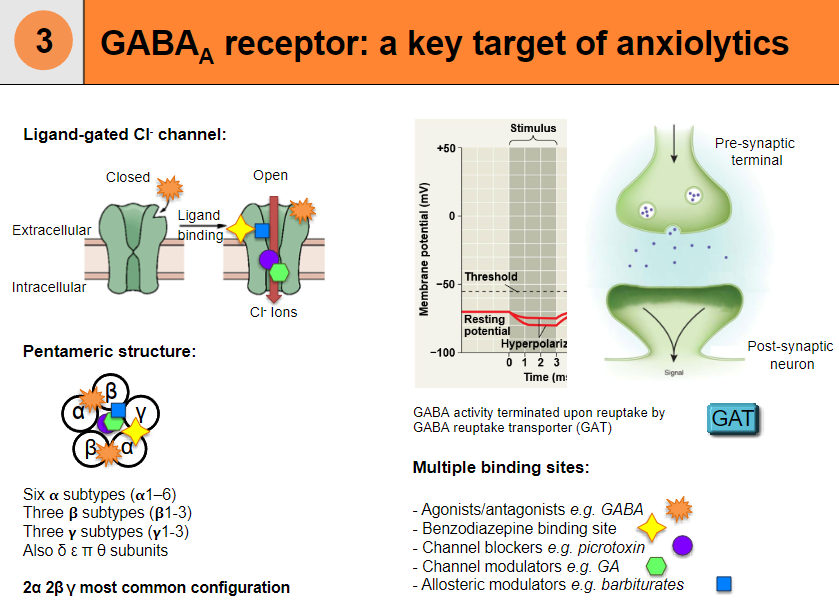
GABAA receptor is a ligand-gated chloride (Cl-) channel, and it is a key target for anxiolytic drugs, which modulate its activity to reduce anxiety.
What is the structure of the GABAA receptor? (3)
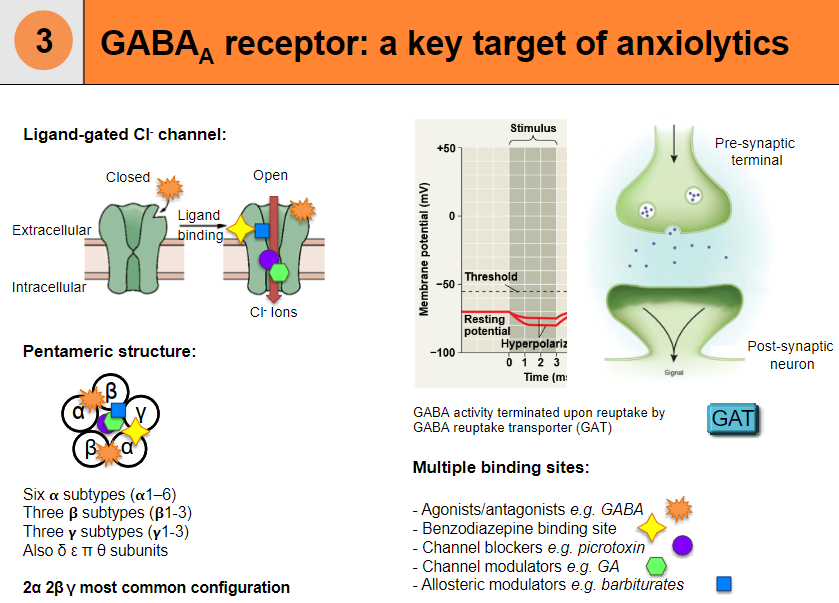
The receptor has a pentameric structure with six ᵷ subtypes (ᵷ 1-6).
It typically includes two α subunits, two β subunits, and one γ subunit, which is the most common configuration.
Other subunits include δ, ε, π, and θ.
What are the types of binding sites on the GABAA receptor? (5)
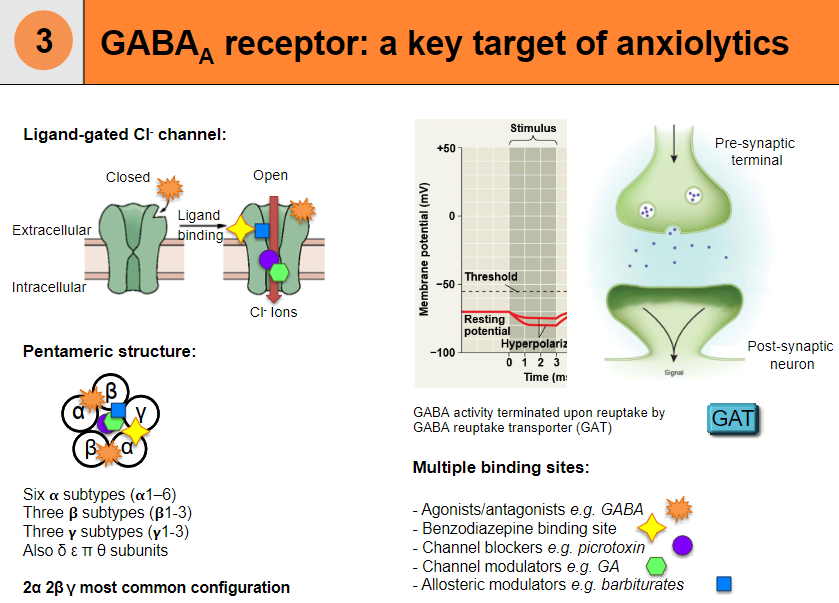
Agonist/antagonist binding site, e.g., GABA.
Benzodiazepine binding site.
Channel blockers binding site, e.g., picrotoxin.
Channel modulators binding site, e.g., GA.
Allosteric modulators binding site, e.g., barbiturates.
How is GABA activity terminated in the GABAA receptor? (1)
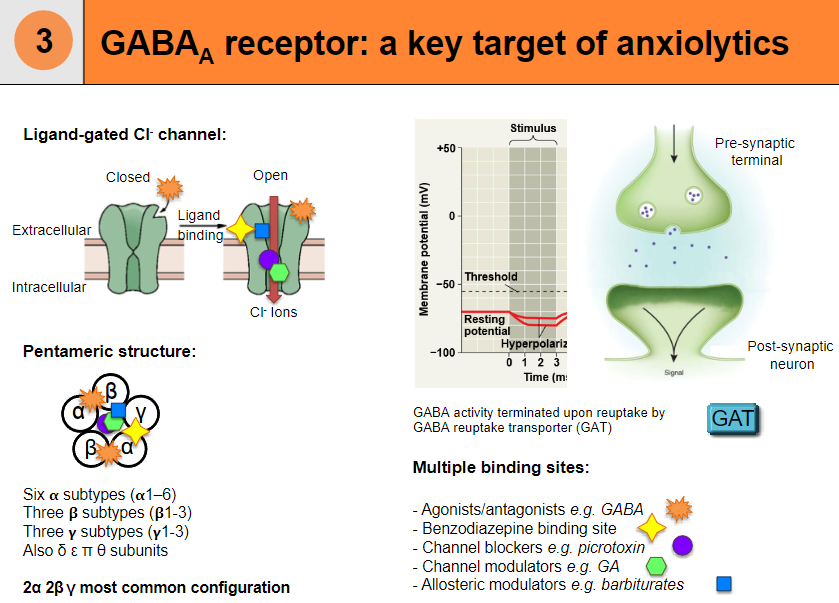
GABA activity is terminated upon reuptake by the GABA reuptake transporter (GAT).
What are benzodiazepines and their role as GABAA receptor modulators? (1)
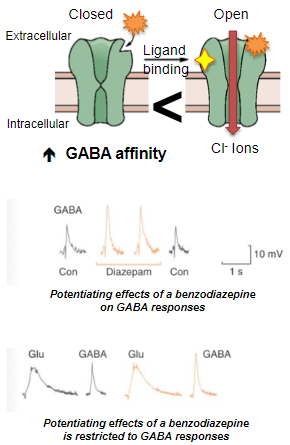
Benzodiazepines are a class of positive allosteric modulators of the GABAA receptor.
How do benzodiazepines interact with GABAA receptors? (2)
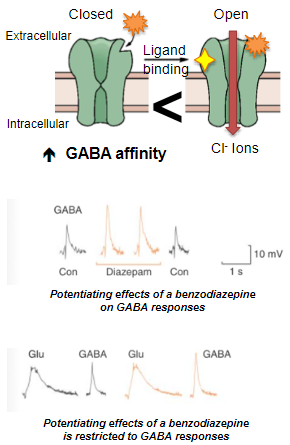
Benzodiazepines bind to a distinct regulatory site on GABAA receptors.
They stabilize the GABAA receptor in the open configuration, increasing GABA affinity.
What is the effect of benzodiazepines on GABA? (2)
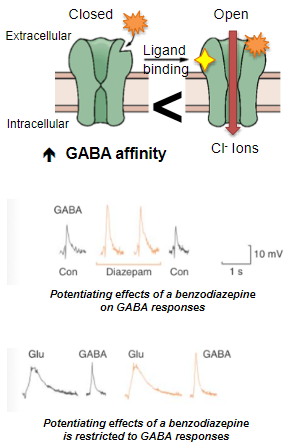
Benzodiazepines increase GABA affinity for its binding site.
This results in the potentiation of GABA responses, enhancing its neuroinhibitory actions.
Why are benzodiazepines considered "cleaner" compounds compared to barbiturates? (1)
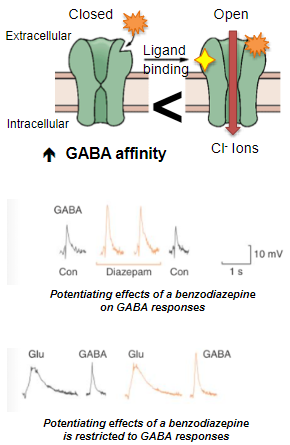
Benzodiazepines are considered "cleaner" because they do not activate other receptors, such as glycine or glutamate receptors, unlike barbiturates.
What is the duration of action and main use of Midazolam? (2)
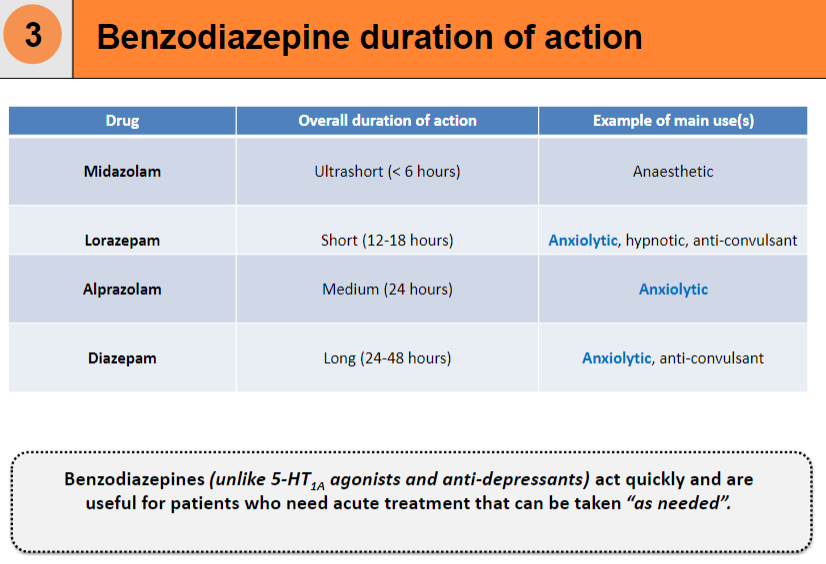
Duration of action: Ultrashort (< 6 hours).
Main use(s): Anaesthetic.
What is the duration of action and main use of Lorazepam? (2)
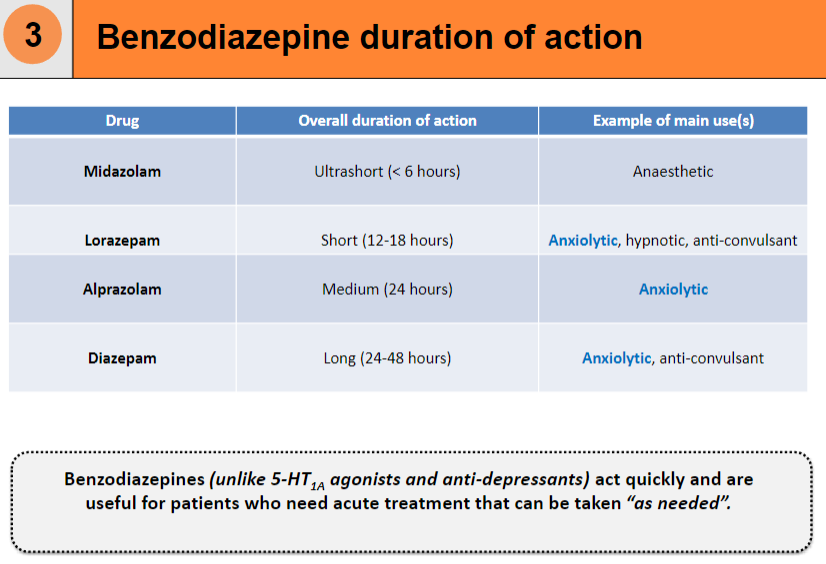
Duration of action: Short (12-18 hours).
Main use(s): Anxiolytic, hypnotic, anti-convulsant.
What is the duration of action and main use of Alprazolam? (2)
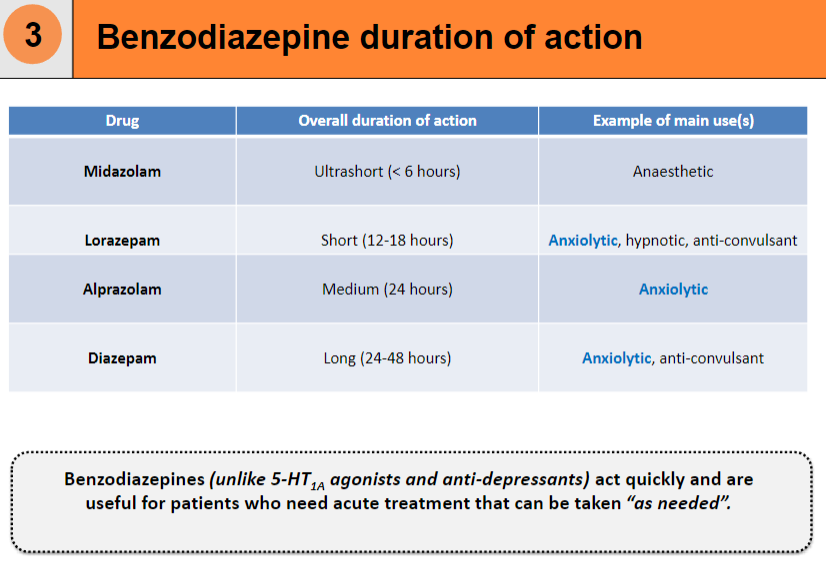
Duration of action: Medium (24 hours).
Main use(s): Anxiolytic.
What is the duration of action and main use of Diazepam? (2)
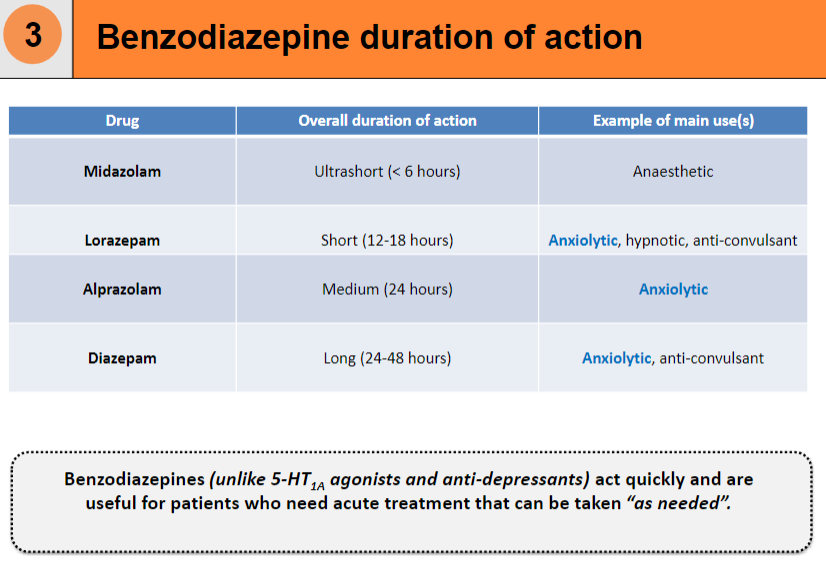
Duration of action: Long (24-48 hours).
Main use(s): Anxiolytic, anti-convulsant.
How do benzodiazepines compare to 5-HT1A agonists and anti-depressants in terms of onset? (1)
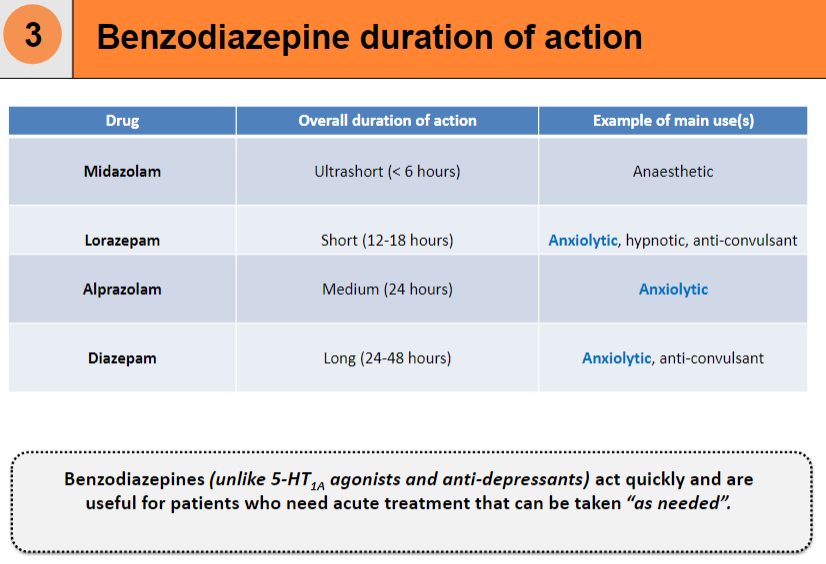
Benzodiazepines act quickly and are useful for acute treatment that can be taken “as needed”, unlike 5-HT1A agonists and anti-depressants, which take longer to take effect.
What are the potential issues associated with barbiturates and benzodiazepines in terms of side effects and dependency? (2)
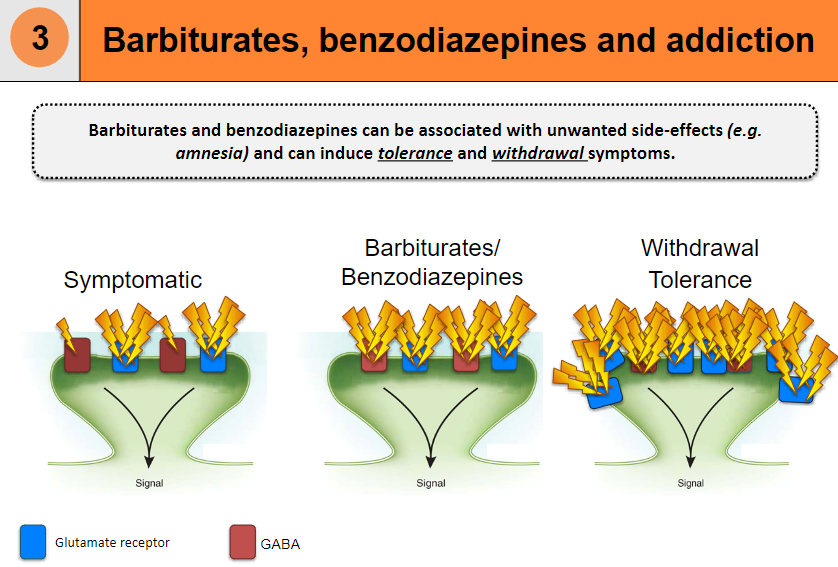
Unwanted side-effects: Amnesia and other cognitive impairments.
Addiction-related issues: Tolerance and withdrawal symptoms can develop with prolonged use.
What is an overview of serotonin (5-HT) and its function? (3)
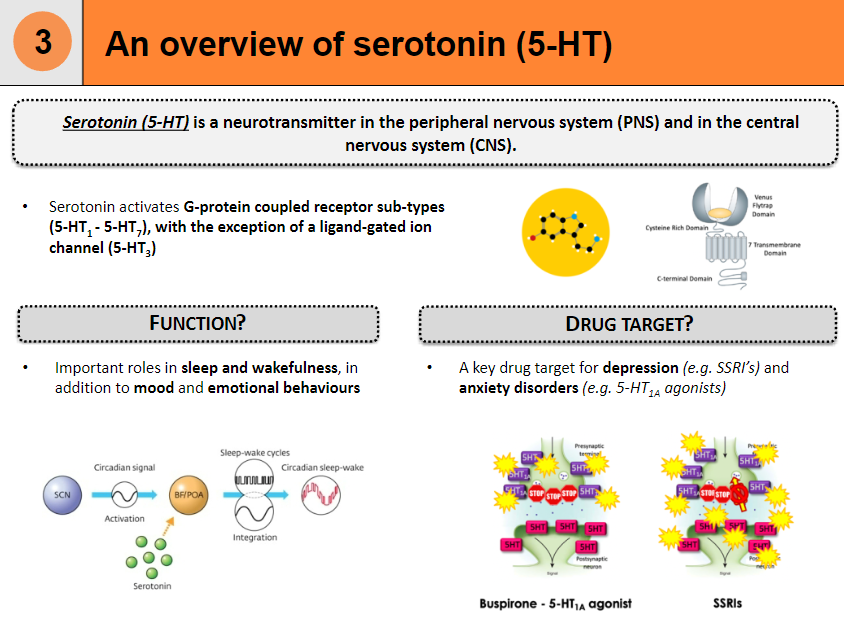
Neurotransmitter: Found in the peripheral nervous system (PNS) and central nervous system (CNS).
Receptor activation: Activates G-protein coupled receptor sub-types (5-HT1 - 5-HT7), except for 5-HT3, which is a ligand-gated ion channel.
Drug target: Plays a key role in treating depression (e.g. SSRIs) and anxiety disorders (e.g. 5-HT1A agonists), with roles in mood, sleep, and emotional behaviors.
What are 5-HT1A receptor agonists and their effects? (4)
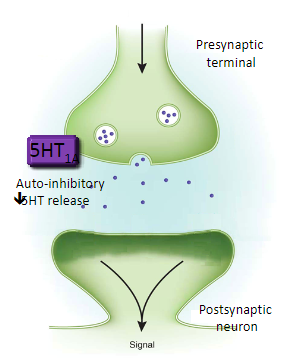
Buspirone is an example of a 5-HT1A receptor agonist, primarily used to treat generalised anxiety disorder (GAD).
Side effects: Less troublesome than benzodiazepines, but may include dizziness, nausea, and headache.
Delayed effect: Anxiolytic effects take several days to be seen.
Mechanism:
Activates 5-HT1A auto-receptors, inhibiting serotonin (5-HT) release.
Inhibits noradrenergic neurons, decreasing arousal reactions.
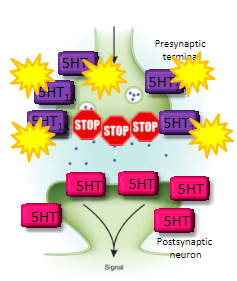
How does buspirone and selective serotonin re-uptake inhibitors (SSRIs) differ in their treatment of anxiety, specifically for generalised anxiety disorder (GAD)? (4)
Buspirone activates 5-HT1A auto-receptors, which decreases serotonin (5-HT) release. It is used for generalised anxiety disorder (GAD) and has delayed effects.
Selective serotonin re-uptake inhibitors (SSRIs) work by blocking the serotonin re-uptake transporter (SERT), leading to more serotonin (5-HT) being available in the brain.
SSRIs are more commonly used for long-term treatment of anxiety and depression.
Both medications affect serotonin but in different ways to manage anxiety disorders.
What is the mechanism of action of buspirone in treating generalised anxiety disorder (GAD)? (5)
Buspirone is a 5-HT1A receptor agonist, meaning it binds to and activates 5-HT1A receptors in the brain.
Initially, the 5-HT1A receptors are auto-inhibitory, so when buspirone activates them, it inhibits serotonin (5-HT) release from serotonergic neurons.
With prolonged use, the brain desensitizes these auto-inhibitory receptors and downregulates the 5-HT1A receptors, meaning they become less sensitive to the effects of serotonin.
This process leads to heightened excitation of serotonergic neurons, resulting in increased serotonin release over time.
This mechanism helps reduce anxiety and alleviate symptoms of generalized anxiety disorder (GAD). However, buspirone is not effective for phobias.
What are the functions of noradrenaline and its role in anxiety? (4)
Noradrenaline is the major neurotransmitter of the sympathetic nervous system, influencing cardiovascular tone.
It also plays a role in attention, arousal, and sleep-wake cycles.
Noradrenaline activates G-protein coupled receptor subtypes, including α- and β-noradrenergic receptors.
As a drug target, α-noradrenergic receptor antagonists can be used to treat the peripheral manifestations of anxiety.
What are β-noradrenergic receptor antagonists (e.g. propranolol) and their role in treating anxiety? (5)
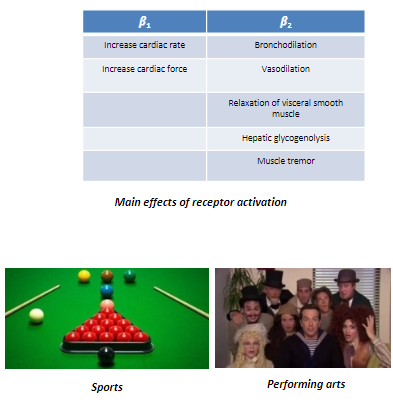
β-noradrenergic receptor antagonists (e.g. propranolol) are used to treat some anxiety forms.
Propranolol is non-selective between β1 and β2 receptors.
Effects of receptor activation: Increased heart rate, force, bronchodilation, vasodilation, and muscle tremor.
They reduce peripheral anxiety symptoms like tachycardia, sweating, and tremors.
Effectiveness is due to blocking peripheral sympathetic responses rather than central effects, aiding in sports (reduces tremor) and performing arts (reduces stage fright).
What are anxiety disorders and how are they characterized? (2)
Anxiety disorders involve significant feelings of anxiety (worry about future events) and fear (reaction to current events).
These feelings can cause physical symptoms, such as fast heart rate and shakiness.
What is panic disorder and its key features? (3)
Panic disorder is characterized by recurring panic attacks.
A panic attack involves sudden intense fear with symptoms like palpitations, sweating, shaking, and shortness of breath.
These attacks often occur unexpectedly.
What is agoraphobia and how is it characterized? (2)
Agoraphobia is an extreme or irrational fear of places where escape may be difficult.
This condition can limit one's ability to be in certain environments.
What is obsessive-compulsive disorder (OCD) and its main characteristics? (3)
Obsessive-compulsive disorder (OCD) involves excessive orderliness, perfectionism, and attention to details.
Individuals with OCD may feel a need for control in their relationships and daily activities.
This can impair functioning and cause distress.
What is post-traumatic stress disorder (PTSD) and its main features? (3)
Post-traumatic stress disorder (PTSD) occurs due to severe psychological shock or injury.
It leads to persistent mental and emotional stress, including vivid memories and sleep disturbances.
Individuals may experience dulled responses to others and the outside world.
What are benzodiazepines and how are they used? (2)
Benzodiazepines are a class of drugs used as short-term anxiolytics.
They are commonly prescribed for anxiety relief but can be habit-forming if used long-term.