Heart Failure Presentation
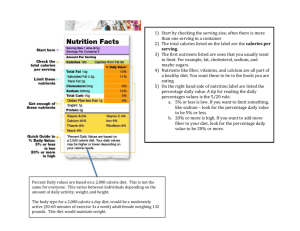
advertisement

Heart Failure Jerri Lamar Learning Objectives Understand classification of heart failure, along with the signs and symptoms. Identify heart failure stages for the development of diagnosis, intervention and patient-centered goals. Definitions Heart muscle is unable to pump enough blood through to meet the body’s needs for blood and oxygen Healthy Heart: Pumps 50% of the blood in the ventricle in one beat Failing Heart: 40% or less of the blood in the ventricle in one beat Further categorization Systolic failure vs Diastolic failure Heart is unable pump all the blood it receives= excess fluids can back up into the lungs and other parts of the body Pulmonary congestion or peripheral edema Compensation Mechanisms Heart: Enlarges Increases muscle mass Pumps faster Stimulate kidneys to conserve sodium and water Body: Blood vessels narrow Sending blood to most vital organs Public Health Problem Affects more than 5 million Americans 500,000 new cases diagnosed each year 10 per 1,000 population after the age of 65 Highest rates: Black women, followed by Black men, MexicanAmerican men, White men, White women, and MexicanAmerican women Medical Diagnosis and Management Medical history and symptoms Treatment of Underlying Conditions Physical Exam: Hypertension Blood pressure Dyslipidemia Weight Thyroid disorders Listen to heart and lungs Arrhythmias Blood test: Sodium, Potassium, albumin, and creatinine Chest X-Rays EKG: Electrocardiogram Echocardiography Exercise Stress Test Nutrition Assessment Anorexia Nausea, abdominal pain and feeling of fullness Constipation Malabsorption Malnutrition Cardiac cachexia Hypomagnesemia Hyponatremia Signs and Symptoms Shortness of breath Fatigue Fluid Retention Persistent coughing or wheezing Lack of appetite, nausea Confusion/memory loss Increased heart rate Anxiety Insomnia Syncope and Headache Stages of Heart Failure Classifications Risk Factors Conditions: Smoking Coronary heart disease Overweight Past MI Diet high in fat and Abnormal heart valves cholesterol Heart muscle disease or Physical inactivity inflammation Excessive alcohol Heart defects present at consumption birth Male sex Severe lung disease Lower education Hypertension Dyslipidemia Diabetes Sleep Apnea Diagnosis: PES Statement Food and nutrition knowledge deficit related to no previous nutrition education as evidenced by the consumption of and inability to identify high sodium foods. Excessive sodium intake related to frequent use of convenience and fast foods as evidenced by diet history. Intervention: Therapeutic Diet Small, frequent meals Lifestyle changes Low in saturated fat, trans fat, cholesterol Increase physical activity Increase: whole grains, F&V Manage stress Restricted sodium diet- <2 gm/day (DASH diet) Get adequate rest Lose or maintain appropriate weight Limit fluid to 2 L per day Develop support Severely decompensated, 1000-1500 mL daily Supplementation: Magnesium, Thiamin Ensure adequate: B6, B12 and folate in diet. Avoid: tobacco, alcohol Education Salt alternatives Label Reading Herbs, Botanicals, and Supplements L-arginine- reduces endothelin (protein that causes blood vessel constriction) Chromium- dyslipidemia Coenzyme Q10- repletion may prevent oxidative stress and further myocardial damage Omega-3 fatty acids in fish oil capsules- lower elevated triglyceride levels, prevent atrial fibrillation, and possibly reduce mortality rates Vitamin D- may improve inflammation Avoid: Grapefruit juice Niacin Vitamin E Energy and Protein Needs Energy Severe HF= energy needs increased by 30-50% more than basal level due to increased energy expenditure of the heart and lungs 31-35 kcal/kg of body weight Cardiac cachexia- 1.6-1.8 times the REE Protein Research: 1.12 g protein/kg Preserve actual body composition Limit effects of hypercatabolism Medications ACE inhibitors Decrease sodium and water retention Benazepril, Captopril, Enalapril Angiotensin receptor blockers Aldosterone blockers Warfarin, heparin Antiplatelet Agents Eplerenone, Spironolactone Anticoagulants Candesartan, Eprosartan Reduce cardiac output Acebutolol, Atenolol, Betaxolol Norvasc, Cardizem Digoxin (Lanoxin) Diuretics Plavix, Reopro Beta-blockers Calcium Channel Blockers Vasodilators Bumetanide, Chlorothiazide Hydralazine, Isordil Statins Lipitor, crestor Medical Treatment Percutaneous coronary intervention (PCI) Coronary artery bypass Valve replacement Defibrillator implantation Left ventricular assist device (LVAD) Heart transplant References Congestive Heart Failure. American Heart Association Web site. http://www.heart.org/HEARTORG/Conditions/CongenitalHeartDefects/TheImpactofCongeni talHeartDefects/Congestive-Heart-Failure_UCM_307111_Article.jsp. Accessed February 9, 2014. Escott-Stump S. Heart Failure. Nutrition and Diagnosis-Related Care. 6th ed. Lippincott Williams & Wilkins; 2007: 333-338. Heart Disease and Congestive Heart Failure. WebMD Web site. http://www.webmd.com/heartdisease/guide-heart-failure. Accessed February 9, 2014. Heart Failure. Mayo Clinic Web site. http://www.mayoclinic.org/diseases-conditions/heartfailure/basics/definition/CON-20029801. Last updated Aug. 16, 2013. Assessed February 13, 2014. Heart Failure. National Institute of Health Web Site. http://www.nlm.nih.gov/medlineplus/heartfailure.html. Accessed February 10, 2014. Mahan KL, Escott-Stump S, Raymond JL, Krause MV. Heart Failure. In: Alexopoulos Y, ed. Krause's Food & the Nutrition Care Process. 13th ed. St. Louis, MO: Elsevier/Saunders; 2012:769-777. Pasini E, Opasich C, Pastoris O, Aquilani R. Inadequate Nutritional Intake for Daily Life Activity of Clinically Stable Patients with Chronic Heart Failure, Am J Cardiol. 2004, 93 (Suppl): 41A43A. Vieth R, Kimball S: Vitamin D in congestive heart failure, Am J Clin Nutr 2006; 83:731-732.