The Treatment of Sepsis: Early Goal Directed Therapy and Beyond
advertisement

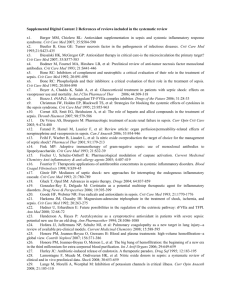
The Treatment of Sepsis: Early Goal Directed Therapy and Beyond Anthony J. Hericks, D.O. South Dakota ACP Scientific Meeting September 13th, 2013 A clinician, armed with the sepsis bundles, attacks the three heads of severe sepsis: hypotension, hypoperfusion and organ dysfunction. Crit Care Med 2004; 320(Suppl):S595-S597 Surviving Sepsis Campaign Sponsoring Organizations American Association of Critical-Care Nurses American College of Chest Physicians American College of Emergency Physicians Australian and New Zealand Intensive Care Society Asia Pacific Association of Critical Care Medicine American Thoracic Society Brazilian Society of Critical Care(AIMB) Canadian Critical Care Society Emirates Intensive Care Society European Respiratory Society European Society of Clinical Microbiology and Infectious Diseases European Society of Intensive Care Medicine European Society of Pediatric and Neonatal Intensive Care Infectious Diseases Society of America Indian Society of Critical Care Medicine Japanese Association for Acute Medicine Japanese Society of Intensive Care Medicine Latin American Sepsis Institute Pan Arab Critical Care Medicine Society Pediatric Acute Lung Injury and Sepsis Investigators Society for Academic Emergency Medicine Society of Critical Care Medicine Society of Hospital Medicine Surgical Infection Society World Federation of Critical Care Nurses World Federation of Societies of Intensive and Critical Care Medicine German Sepsis Society Surviving Sepsis Campaign (SSC) Guidelines for Management of Severe Sepsis and Septic Shock Dellinger RP, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med 2004, 32:858-873. Dellinger RP, et al. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock: 2008 Crit Care Med 2008, 36:296-327. Levy MM, et al. Surviving Sepsis Campaign: Results of an international guidelines performance improvement program targeting severe sepsis. Crit Care Med 2010, 38:367-374. Dellinger RP, et al. Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock: 2012. Crit Care Med 2013, 41(2):580-637. Angus DC, et al. Severe Sepsis and Septic Shock. NEJM 2013; 369(9): 840-851 Surviving Sepsis Campaign Conclusions Strong agreement among a large cohort of international experts Many level 1 recommendations Significant number of recommendations with relatively weak recommendations Evidence-based recommendations are the foundation of improved outcomes Dellinger RP, CCM 2013 Grading of Recommendations (Grading of Recommendations Assessment, Develop and Evaluation – GRADE) A 82 year old white female present to the emergency department with complaints of dysuria, frequency and urgency. Her temperature is 100.4 F, HR 92, RR 21 and BP 122/86. What should she be classified as? 1. 2. 3. 4. 5. Systemic Inflammatory Response Syndrome Sepsis Severe Sepsis Septic Shock Multi-Organ Dysfunction/Failure Syndrome A 82 year old white female present to the emergency department with complaints of dysuria, frequency and urgency. Her temperature is 100.4 F, HR 92, RR 21 and BP 122/86. What should she be classified as? 1. 2. 3. 4. 5. Systemic Inflammatory Response Syndrome Sepsis Severe Sepsis Septic Shock Multi-Organ Dysfunction/Failure Syndrome Identification of Sepsis: Definitions Systemic Inflammatory Response (SIRS) Sepsis Severe Sepsis Septic Shock Multi-Organ Failure Syndrome (MOFS) Death SIRS Heart Rate > 90 Respiratory Rate > 20 WBC > 12K or < 4K Temp > 38 C (100.4 F) or < 36 C (96.8 F) Any two of the above Very nonspecific Sepsis SIRS + signs of a suspected or known infection – WBC’s in normally sterile fluid – Infiltrate on chest x-ray – Bacteria in normally sterile fluid Diagnostic Criteria for Sepsis Severe Sepsis Sepsis + sepsis-induced tissue hypoperfusion or organ dysfunction Sepsis Induced Hypotension SBP < 90 mmHg OR MAP < 70 mmHg OR SBP > 40 mmHg < 2 SD below the nml for age Septic Shock Severe Sepsis or sepsis-induced hypoperfusion persistent despite: – Adequate/initial fluid challenge/resuscitation – Lactate > 4 mmol – Addition of pressors Sepsis-induced hypoperfusion = infection- induced hypotension, elevated lactate or oliguria MOFS Altered organ function, involving two or more organs, in an acutely ill patient requiring medical intervention to achieve homeostasis Death The permanent the cessation of all vital functions in an individual who has sustained either (1) irreversible cessation of circulatory and respiratory functions, or (2) irreversible cessation of all functions of the entire brain, including the brain stem Severe Sepsis/Septic Shock mortality = ~30-46% Consideration for Limitation of Support “We recommend that the goals of care and prognosis be discussed with patients and families and these be incorporated into the patients treatment along with end-of-life care planning and utilizing palliative care principles.” Grade 1B – Re-address goals as earlier as feasible, but no later than 72 hours of admit Grade 2C Incidence of Severe Sepsis Estimated to be: – 2% of all patients admitted to the hospital – 10% of all patients in the ICU – < 750,000 cases per year and rising – Mortality rate of 20-30% NEJM 369(9): 840-851 Pathophysiology of Sepsis Figure B, page 948, reproduced with permission from Dellinger RP. Cardiovascular management of septic shock. Crit Care Med 2003;31:946-955. Based on Dr. Rivers article re: Early Goal Directed Therapy, what is the ultimate goal in the first 6 hours? 1. 2. 3. 4. 5. CVP of 8-12 unventilated/12-15 ventilated MAP >65 Cardiac Output > 8 LPM Hemoglobin > 10 gm/dL ScvO2 > 70% Based on Dr. Rivers article re: Early Goal Directed Therapy, what is the ultimate goal in the first 6 hours? 1. 2. 3. 4. 5. CVP of 8-12 unventilated/12-15 ventilated MAP >65 Cardiac Output > 8 LPM Hemoglobin > 10 gm/dL ScvO2 > 70% Initial Resuscitation: Goals of Early Goal Directed Therapy CVP 8-12 cmH2O – 12-15 cmH2O on the ventilator MAP > 65 mmHg – May need to be higher in patients with HTN UOP > 0.5 mL/Kg /hour ScvO2 > 70% – SvO2 > 65% Grade 1C Goal: Normalize lactate Grade 2C Goal in the first 6 hours after diagnosis 16-17% decrease in mortality Rivers E. N Engl J Med 2001; 345:1368-77 Central Venous Pressure Crystalloid or Colloid? Volume? Goal? Crystalloid or Colloid SAFE Study – Crystalloid (NS) = Colloid (4% Albumin) Less volume, more PRBC’s, higher CVP and Albumin – No difference in mortality (p = 0.87) Trend for increased risk of death in Trauma (0.06) Trend for decreased risk of death in Severe Sepsis (0.09) Grade 1B Finfer S. N Engl J Med 2004; 350:2247–2256 SSC Recommendations Crystalloids Albumin Grade 1B Grade 2C – If substantial fluid is required Hydroxyethyl Starch (HES) Increased risk of acute kidney injury and death in sepsis – Variable findings depending on studies Schortgen G. Lancet 2001; 357:911-916. Sakr Y. Br J Anaesth 2007; 98:216-224. Brunkhorst FM. N Engl J Med 2008; 358: 125-139. Perner A. N Engl J Med 2012; 367:124-134. Risk and no benefit, HES should not be used!!! Grade 1B Fluid Volume 30 mL/Kg crystalloid Grade 1C – A portion may be an albumin equivalent – More rapid administration or larger amounts may be needed Continue fluid administration as long as there appears to be hemodynamic improvement Grade UG Volume Responsiveness CVP > 8 cmH2O Grade 1C – > 12 cmH2O on the vent Swan-Ganz Catheter – PCWP – Cardiac output Non-invasive Monitors – PiCCO Catheter – FloTrac – Pulse Pressure Variation IVC via Echo MAP and Heart Rate Grade 1D CVP Spontaneous Breathing > 8 cmH2O Ventilatory Breathing > 12 cmH2O Primarily based on expert opinion – Dellinger RP. Crit Care Med 2004; 32:858–873 – Rivers E. N Engl J Med 2001; 345:1368–1377 – Practice parameters for hemodynamic support of sepsis in adult patients with sepsis. Crit Care Med 1999; 27:639–660 Pulmonary Capillary Wedge Pressure PCWP < 12 mmHg predicts a fluid bolus with increase cardiac output with a PPV of only 54% However the “Gold Standard” for “volume responsiveness” may be a increase in cardiac output of > 15% after a fluid challenge Osman D. Crit Care Med 2007; 35:64–68 Non-invasive Monitoring PPV PPV PPV CVP PCWP Echocardiography Does volume overload contribute to morbidity and mortality? 1. True 2. False Does volume overload contribute to morbidity and mortality? 1. True 2. False Avoid Volume Overload Tolerated as long as volume responsive – Fluid challenges usually required for the initial 24-48 hours Finfer S. N Engl J Med 2004; 350:2247–2256 Decrease the rate when no longer volume responsive Grade 1D Volume Overload, Cont’d Independent predictor of mortality – Boyd JH. Crit Care Med 2011; 39(2):259-265 – Vincent JL. Crit Care Med 2006; 34:344–353 – Uchino S. Crit Care Med 2006; 10:R174 Prolonged mechanical ventilation – Upadya A. Intensive Care Med 2005; 31:1643–1647 ARDS – – – – Humphrey H. Chest 1990; 97:1176–1180 Simmons RS. Am Rev Respir Dis 1987; 135:924–929 Mitchell JP. Am Rev Respir Dis 1992; 145:990–998 Wiedemann HP. N Engl J Med 2006; 354:2564–2575 Sepsis – Alsous F. Chest 2000; 117:1749–1754 – Rivers E. N Engl J Med 2001; 345:1368–1377 Abdominal compartment syndrome – Malbrain ML. Crit Care Med 2005; 33:315–322 – McNelis J. Arch Surg 2002;137:133–136 Cerebral edema and herniation – Uchino S. Crit Care 2006; 10:R174 MAP MAP 65 mm Hg 75 mm Hg 85 mm Hg F/LT Urinary output (mL) 49 +18 56 + 21 43 +13 .60/.71 Capillary blood flow (mL/min/100 g) 6.0 + 1.6 5.8 + 11 5.3 + 0.9 .59/.55 0.42 + 0.06 0.44 +016 0.42 + 0.06 .74/.97 Pico2 (mm Hg) 41 + 2 47 + 2 46 + 2 .11/.12 Pa-Pico2 (mm Hg) 13 + 3 17 + 3 16 + 3 .27/.40 Red Cell Velocity (au) Adapted from Table 4, page 2731, with permission from LeDoux, Astiz ME, Carpati CM, Rackow ED. Effects of perfusion pressure on tissue perfusion in septic shock. Crit Care Med 2000; 28:2729-2732 Grade 1C What is the pressor of choice for a patient in septic shock? 1. Dopamine 2. Norepinephrine (Levophed) 3. Vasopressin 4. Phenylephrine (Neosynephrine) 5. All the above What is the pressor of choice for a patient in septic shock? 1. Dopamine 2. Norepinephrine (Levophed) 3. Vasopressin 4. Phenylephrine (Neosynephrine) 5. All the above Vasopressors Norepinephrine Dopamine Vasopressin Epinephrine Phenylephrine Norepinephrine vs Dopamine No significant difference in mortality (p = 0.10) – Trend for less death in the ICU (p = 0.07) – No difference at hospital discharge or 1 yr Increased rate of adverse events with Dopamine – Arrhythmias (p = < 0.001) Atrial Fibrillation Ventricular Tachycardia Ventricular Fibrillation – Skin Ischemia (trend; p = 0.09) DeBacker D. N Engl J Med 2010; 362:779-789 Norepinephrine vs Dopamine, Cont’d Norepinephrine should be the first line Grade 1B vasopressor Dopamine is an alternative to Norepinephrine – Only in highly selected patients with low risk of: Tachyarrhythmias Absolute or relative bradycardia Grade 2C Vasopressin Adding Vasopressin to Norepinephrine showed no mortality benefit compared to Norepinephrine alone (p = 0.26) – Did lower Norepinephrine requirements – May have other potential physiologic benefits Should not be used as a single agent Grade UG Russel JA. N Engl J Med 2008; 358:877-887 Epinephrine First line in pts poorly responsive to Norepinephrine and Dopamine – No evidence of worse outcomes Increased risk of: – Tachycardia – Elevated lactate – Decreased splanchnic circulation Add to or instead of Norepinephrine Grade 2B Phenylephrine Not recommended!!! – Except: Norepinephrine induced arrhythmias Cardiac output is high Persistently low BP Salvage therapy Decreases cardiac output Grade 1C Hemodynamic Equations DaO2 = CO x Hgb x SaO2 – Oxygen delivery VO2 = CO x Hgb x (SaO2 - SvO2) – Oxygen consumption O2 ER= VO2/DaO2 – Oxygen extraction ratio ~ 0.2 to 0.3 VO2 > DaO2 OR DaO2 < VO2 = Dysoxia – Dysoxia = lactic acidosis = organ failure = death Venous Oxygen Saturation Physiology Adapted from: http://ht.edwards.com/resourcegallery/products/swanganz/pdfs/svo2edbook.pdf ScvO2/SvO2 Goal > 70%/65% respectively – Normal or shunt physiology < 70%/65% respectively – Transfuse to a Hgb > 10 OR – Start Dobutamine No specific cardiac output/index Grade 1C ScvO2 = subclavian vein SvO2 = pulmonary artery Ionotropic Therapy Dobutamine: – Max dose 20 mcg/Kg/min Titrate to NO pre-defined CO Grade 1B – Used in states with: Elevated cardiac filling pressures Low cardiac output ScvO2 < 70% OR SvO2 < 65% Grade 1C RBC Transfusion Therapy Only if the Hgb < 10 with EGDT Only if the Hgb < 7.0 g/dL in other ICU patients Grade 1B – Target 7 to 9 g/dL – Consider earlier for myocardial ischemia/ischemic coronary disease, severe hypoxemia, acute hemorrhage, cyanotic heart disease or lactic acidosis No EPO Grade 1B Napolitano LM. Crit Care Med 2009; 37(12): 3124-3157 FFP Transfusion Therapy No FFP to reverse coagulopathy in the absence of bleeding or invasive procedures Grade 2D No high-dose Antithrombin – Studies had revealed that a subgroup with severe sepsis and high risk of death = better survival Grade 1B Platelet Transfusion Therapy < 10,000 – prophylactically in absence of bleeding < 20,000 - significant risk of bleeding > 50,000 – active bleeding, surgery or invasive procedures Grade 2D Other Investigation Therapy Immunoglobulins – No use Grade 2B Selenium – Antioxidant – No use Grade 2C Diagnostic Testing Lactate level – Within 3 hours Cultures – Prior to antibiotic administration Grade 1D Do not delay resuscitation for antibiotic administration > 50% of cases of severe sepsis and septic shock will be culture negative – Minimum 2 blood cultures One peripheral and one from each vascular access device Imaging – If not too unstable Grade 1C Diagnostic Testing, Cont’d Serologies: – – – – Strep pneumo and Legionella Urine Ag Mycoplasma IgM 1,3 B-D-glucan Grade 2B Mannan and anti-mannan Ab’s Procalcitonin – Use low levels to assist with Abx D/C Grade 2C Antibiotic Therapy IV route within the 1st hour – Septic Shock Grade 1B – Severe Sepsis Grade 1C One or more drugs with activity against the likely pathogens Grade 1B – Double cover if MDR pathogens Grade 2B – Combo therapy for neutropenic fever Grade 2B – Beta-lactam and macrolide for Strep pneumonia Grade 2B ABX, Cont’d Reassess routinely Grade 1B De-escalate after >3-5 days Grade 2B Duration of treatment ~7-10 days Grade 2C Stop therapy if the syndrome is not infectious Grade 1D Source Control Seek, diagnose or exclude potential anatomical infections and treat expectantly – Within the first 12 hrs Grade 1C Delay definitive treatment of peripancreatic necrosis until demarcation of tissue has occurred Grade 2B Attempt percutaneous over surgical intervention if possible Grade UG Remove vascular access suspected after other access has been placed Grade UG Corticosteroids Hydrocortisone – 200 mg/day – Only with persistent hypotension/poorly responsive to vasopressor therapy Grade 2C – Consider a continuous infusion Grade 2D – Do not do an ACTH stimulation test Grade 2B No Dexamethasone Grade 2B Fludrocortisone if other steroid than HCT Wean steroids when off pressors Grade 2D Grade 2C Corticosteroids, Cont’d Annane D. JAMA 2002; 288:862–871 – Cosyntropin Stim Test delta < 9 = non-responders – 10% decrease in mortality if treated with steroids – 17% decrease in pressor requirements Sprung CL. N Engl J Med 2008; 358:111-124 – No significant difference in mortality – Shock was reversed more quickly – More episodes of superinfection, including new sepsis and septic shock but not statistically significant CIRCI (Critical Illness Related Corticosteroid Insufficiency) Marik PE. Crit Care Med 2008 Vol. 36 (6): 1937-1949 CIRCI, Cont’d Recombinant Human Activated Protein C (Xigris) Withdrawn from the market 2011 – No benefit Mechanical Ventilation Target tidal volume = 6 mL/Kg Grade 1A Plateau pressure goal < 30 cmH2O Grade 1B Allow permissive hypercapnia Grade 1C Use PEEP to decrease FiO2 Grade 1B – Higher PEEP vs lower Grade 2C Recruitment maneuvers Grade 2C ARDS ARMA Trial – The Acute Respiratory Distress Syndrome Network. N Engl J Med 2000;342:1301-08. Alveoli Trial – Brower RG. N Engl J Med 2004;351:327-36 Mechanical Ventilation, Cont’d Consider prone positioning – P:F ration <100 Grade 2C HOB elevated Grade 1B – Goal > 30-45 Grade 1B NIPPV considered in mild ALI/ARDS – Low threshold for intubation Grade 2B Mechanical Ventilation, Cont’d Weaning protocols Grade 1A Selective Oral/Digestive Decontamination – Oral chlorhexidine gluconate – Decreases VAP Grade 2B Avoid pulmonary artery catheters Grade 1A Conservative fluid management (FACTT) – Wiedemann et al. N Engl J Med 2006; 354:2564-2575. Grade 1C Beta-Agonists No recommended for routine use Grade 1B – Nebulized (Ok if concern for bronchospasm) Trend for less vent days Slightly faster heart rates at day #2 Trend for increased mortality – Intravenous (Salbutamol) Increased mortality Sedation, Analgesia and NMB Use Sedation protocol Grade 1B – Minimize intermittent and continuous treatments Use Sedation scales Avoid NMB Grade 1B Grade 1C – Without ARDS – With ARDS (Sepsis-induced and P:F <150) < 48 hours Grade 2C Glucose Control Use intravenous insulin to control blood sugars Grade 2C – If 2 consecutive BS’s > 180 Goal < 180 Grade 1B Grade ? 1A – ? Target range 110-180 mg/dL Avoid hypoglycemia Renal Replacement Therapy CRRT and Intermittent HD are equivalents Grade 2B CRRT should be used if hemodynamically unstable Grade 2D Bicarbonate Therapy Avoid NaHCO3 in patients with a pH > 7.15 and lactic acidemia for the purpose of improving hemodynamics or to reduce vasopressor requirements Grade 2B Thromboembolism Prophylaxis LMWH daily vs Low dose UFH BID LMWH daily vs Low dose UFH TID Grade 1B Grade 2C Dalteparin if creat clearance < 30 mL/min – LMWH Grade 2C or UFH Grade 1A Grade 1A Mechanical prophylaxis if contraindications to heparin products Grade 2C Combo therapy in patients who are high risk – Severe sepsis, history of DVT, or orthopedic surgery Grade 2C Stress Ulcer Prophylaxis If risk of bleeding – H2 blocker Grade 1B – Proton Pump Inhibitor Grade 1B – PPI over H2 Grade 2C No risk of bleeding = no PPI Grade 2B Nutrition Oral or enteral nutrition in the 1st 48 hrs vs complete fasting or just glucose Grade 2C Avoid full caloric feeding for the 1st full week Grade 2B – Low dose feeding up to 500 Kcal/day and advance as tolerated (60-70%) IV glucose and EN vs TPN alone or TPN and EN in the 1st week Grade 2B No specific immunomodulating form Grade 2C Surviving Sepsis Bundles Bundles Point/Counterpoint Editorials – Are the best patient outcomes achieved when ICU bundles are rigorously adhered to? Pros: Dr. Delinger – Not perfect/have flaws, but are based on the best available evidence. Cons: Dr. Marik – Not completely “evidence based” and “cook book” medicine can harm the patient. CHEST 2013; 144(2):372-380 Is there byass/conflict of interest when it comes to the Surviving Sepsis Campaign Guidelines and Early Goal Directed Therapy? 1. Yes 2. No Is there byass/conflict of interest when it comes to the Surviving Sepsis Campaign Guidelines and Early Goal Directed Therapy? 1. Yes 2. No Benefits of the Surviving Sepsis Campaign Surviving Sepsis Campaign Improvement Program – Resuscitation Bundle - First 6 hours Compliance increase linearly from 10.9% to 31.3% over two years ( p = 0.0001) – Management Bundle - First 24 hours Compliance increase linearly from 18.4% to 36.1% over two years ( p = 0.008) – Unadjusted odds ratio for hospital mortality decreased from 37% to 30.8% over two years (p = 0.001) THE END ?? QUESTIONS ??