Treating Allergic Reactions
advertisement

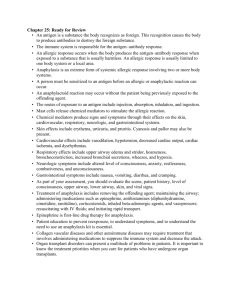
Epinephrine Auto-Injector Training Program Authored and Editied by… Ian Malik, NREMT-B, Captain, Hopewell Valley Emergency Services Jennifer Morris, EMT-B, Mount Laurel EMS Robin Plumer, DO; Medical Director, Mount Laurel EMS Stephen Vetrano, DO, EMT-B; Chair, BLS Subcommittee, MICU Advisory Council Disclaimer This presentation was created to assist in the education of EMTs in epinephrine auto injector administration. This presentation is available for public use and copying/distribution is encouraged. It is the intent that this program may serve as the lecture based portion of a BLS medical director’s epinephrine auto injector program. A practical program is also encouraged. The creators and staff of OEMS recognize that an individual medical director may modify any or all of this presentation to serve his/her organization’s needs. The OEMS policy may not be changed under any circumstances Objectives Identify the common causes of an allergic reaction. Review the pathophysiology of an allergic reaction. Identify signs and symptoms of severe allergic reactions (anaphylaxis). Review differential diagnosis of anaphylaxis. Review pharmacology of epinephrine. Identify protocols for administration of epinephrine autoinjector. Identify proper storage, handling, and disposal techniques for the epinephrine auto-injector. Review documentation and regulatory requirements. What this program is… A review of pathophysiology you already know A review of a skill you already know New State Policy New State Policy • • • December 13, 2006 Epinephrine auto injectors can be stocked on approved emergency service vehicles (not required) MUST be an EMT-B to administer Squad Must Register with OEMS • Must have a physician medical director MEDICAL PRACTICE ACT State legislation that defines scope and role of EMS personnel Local modifications authorized by medical oversight physician or board Usually based on Department of Transportation (DOT) National Standard Curricula for each EMT level New State Policy No change in indications – allergic reaction & anaphylaxis ONLY! MEDICAL DIRECTION LIABILITY Respondent superior- an individual supervising a borrowed servant is ultimately liable for the acts and omissions of the borrowed servant while that individual remains under his supervision MEDICAL DIRECTION LIABILITY Borrowed servant- a servant directed or permitted by his master to perform services for another may become the servant of such other in performing the service (i.e. delegated practice) MEDICAL DIRECTION LIABILITY Borrowed servant- a servant directed or permitted by his master to perform services for another may become the servant of such other in performing the service (i.e. delegated practice) NJ Regulation Epinephrine Auto Injector Interim Policy Found at www.state.nj.us/health/ems/documents/epi_ policy.pdf May be made more stringent by the Medical Director Applicable to EMT’s • Medics and MICN’s/RN’s have the knowledge base • Should be familiar with the policy Allergic Reaction Allergic reaction – hypersensitivity to a given antigen. A reaction more pronounced than would occur in the general population. • Acquired hypersensitivity, an individual must first be exposed or sensitized to the antigen; the body forms antibodies to fight the allergen. Subsequent exposure to the antigen results in an allergic reaction. • Allergen – an antigen that results in the release of IgE, resulting in a hypersensitive reaction. Anaphylaxis – an acute, generalized, and violent antigen-antibody reaction that can be rapidly fatal. Causes of Allergic Reactions Insects (bees, wasps) Foods (nuts, eggs, shrimp) Plants (poison ivy, oak, summac) Medications (antibiotics, NSAIDS) Other allergens (dust, chemicals, foreign proteins, hormones, preservatives, X-ray contrast) Pathophysiology Sensitization – initial exposure to an antigen (allergen). Usually asymptomatic or very mild reaction, immune system forms antibodies to recognize this antigen. Delayed Hypersensitivity – cellular immunity that does not involve antibodies. Different from anaphylaxis. Usually occurs in hours and days post exposure and commonly manifests as a skin rash. The rash associated with poison ivy exposure is an example of delayed hypersensitivity. Immediate Hypersensitivity – is commonly referred to by the public as an allergy. Pathophysiology (cont) When an individual who has been previously sensitized to an allergen comes in contact with that allergen the immune system responds by releasing the antibody immunoglobulin E (IgE). IgE attaches to basophiles and mast cells, when the allergen binds to IgE attached to basophiles and mast cells histamine and heparin are released (degranulation). Sensitization Stage Antigen (allergen) exposure Antigen Plasma cells produce IgE antibodies against the allergen Plasma cell IgE IgE antibodies attach to mast cells and basophils Mast cell with fixed IgE antibodies Granules containing histamine Anaphylactic Reaction More of same allergen invades body Allergen combines with IgE attached to . mast cells and basophils, which triggers degranulation and release of histamine and other chemical mediators Antigen • • • •• • • • • • • • •• • • • •• • • • •• • • • • • •• • • • •• • • • • •• • • • •• • • • • • •• • • • • •• • • • • •• • • • • • • •• • • • • •• • • •• • • • • • • • • •• • • •• • • •• • • • •• •• • • • • •• •• •• • • • • • •• •• • • • • • •• • • • • • • • • •• • • • •• • • • • • • • • • • • • • •• • • • • • • • •• •• • • •• • • • • • • • •• • • • • •• • • • •• • • • • • • • • • • • • • • •• • • • • • • •• • • • • • • •• • • • • • • • • • •• • • • •••• •• •• • • • • • • • • • • •• • Mast cell granules release contents after antigen binds with IgE antibodies • Histamine and other mediators Pathophysiology (cont) Histamine is the principal chemical mediator of an allergic reaction. Histamine acts on H1 and H2 receptors resulting in; • Bronchiochonstriction; • Increased intestinal mobility; • Vasodilatation; • Increased vascular permeability; • Increased secretion of gastric acids. The action of histamine is the bodies attempt to minimize exposure to the antigen. Anaphylaxis Massive amounts of histamine and other substances are released resulting in peripheral vasodilatation as well as increased vascular permeability. Massive amounts of plasma may leak out of capillaries resulting in hypotension. Release of slow-reacting substance of anaphylaxis (SRA) causes spasm of the smooth muscle surrounding the bronchioles resulting in an asthma like attack. Clinical Presentation of Allergies and Anaphylaxis Skin • • • • • Flushed Itching (pruritus) Hives (urticaria) Swelling Cyanosis Respiratory System • Respiratory difficulty • • • • • Asthmatics, particularly poorly controlled, have increased risk of fatality Sneezing, coughing Wheezing, stridor Laryngeal edema Laryneospasm Bronchospasm Clinical Presentation of Allergies and Anaphylaxis Cardiovascular System • Vasodilatation • Increased heart rate • Decreased blood pressure Gastrointestinal System • Nausea and vomiting • Abdominal cramping • Diarrhea Nervous System • • • • Dizziness Headache Convulsions Tearing Clinical Spectrum of Allergic Reaction Mild Severe Nasal Congestion Hives Itching Watery & Itchy Eyes Cardiovascular Collapse Respiratory Failure Some define anaphylaxis as involvement Of at least TWO organ systems!!! Common Allergens Insect Bite Reactions • Large local reactions, without SYSTEMIC hives or other involvement of another body system other than skin, do not raise the risk of anaphylaxis on next exposure • Does NOT require treatment with Epi-Pen Common Allergens Large Allergen Exposure • People who may not have pre-existing allergy, but get an overwhelming amount of exposure • May develop anaphylaxis Common Allergens Kissing & Peanut Allergies • A 15 year old girl with a severe peanut allergy died after she kissed her boyfriend, who had eaten peanut butter • Recommended to wait up to 5 hours after eating peanuts to be peanut-free Common Allergens Deaths from anaphylaxis in the US Radiographic Meds Meds Food Items Insect Stings Latex - 900/yr 400-800/yr 100-200/yr 40-100/yr 3/yr Clinical Manifestations of Anaphylaxis Signs/symptoms Incidence (%) Urticaria and angioedema Upper airway edema* Dyspnea and wheezing Flush* Dizziness, syncope, and hypotension Gastrointestinal symptoms Rhinitis* Headache* Substernal pain* Itch without rash* Seizure* *Symptom or sign not reported in all four series 88 56 47 46 33 30 16 15 6 4.5 1.5 Signs and Symptoms Common Presentation of Anaphylaxis Onset of 30 to 60 seconds following exposure, may be delayed over an hour. Sense of impending doom; Flushed skin; Pruritus (generalized itching); Increase heart rate; Often urticaria (hives). Signs and Symptoms Remember – The more rapidly a reaction develops, the more potentially severe it can be!!! Another way of looking at it… 1. Acute onset of an illness with involvement of skin/mucus membranes AND EITHER • Dyspnea • Hypotension Notice no mention of allergen! Another way of looking at it… OR 2. Two or more of the following that occur rapidly after exposure to a likely allergen for that patient • Mucus Membrane/skin involvement • Dyspnea • Hypotension • Persistant GI symptoms Another way of looking at it… OR 3. Hypotension after exposure to known allergen Putting it simply…. Anaphylaxis is either…. • Allergy involving 2 or more systems • Hypotension following exposure to a known allergen Signs and Symptoms Hives • Can be a single symptom of an allergic reaction or the beginning of a cascade. • Use of epinephrine for hives alone is NOT warranted. • Ice packs can be used to relieve itching. Differential Diagnosis History of exposure to an antigen that is an identifiable trigger, in the presence of signs and symptoms of anaphylaxis is a reliable indicator of an anaphylactic reaction. However, signs and symptoms of allergy/anaphylaxis may present without the history! Differential Diagnosis In the absence history of exposure, the following should be considered in the differential diagnosis: • • • • • • • • • • • • • respiratory difficulty, wheezing, stridor circulatory collapse, including vasovagal reactions asthma foreign body obstruction pulmonary embolism epiglottitis myocardial infarction hypoglycemia seizures overdose of medication cold urticaria sulfite or monosodium glutamate ingestion Niacin ingestion Conditions that Mimic Asthma • Similar s/s: wheezing Foreign Body Obstruction - Similar s/s: SOB, altered mental status Respiratory Distress - Similar s/s: SOB, altered mental status Conditions that Mimic Acute M.I. • Similar s/s: chest tightness, SOB, shock CHF • Similar s/s: SOB, altered mental status, shock Pharmacology Epinephrine Auto-Injector • Liquid Medication administered by an automatically injectable needle and syringe system. Medication Name • Generic: Epinephrine • Trade: Adrenalin ™ • EpiPen® or EpiPen Jr. ® Pharmacology Epi-pen exposed! Pharmacology Twinject • A two dose system 2nd dose SQ inject Not for EMT use • Anakit Old kit No longer made in US Being d/c’d in Canada Also beyond scope Pharmacology Indications • Signs and symptoms of severe allergic reaction. Contraindications • None in a life threatening scenario-caution in pts with CAD Action • Bronchodilation – Dilation of airways. • Vasoconstriction – constriction of blood vessels. Side Effects •Increase in heart rate •Pallor •Dizziness •Chest Pain •Headache •Nausea •Vomiting •Anxiety, Excitement Administration Protocol Perform scene size-up and initial patient assessment. Do not delay transport; Administer 100% oxygen using a non-rebreather mask at a flow rate of 12-15 lpm, unless the patient is unable to tolerate the mask, in which case use a nasal cannula at a flow rate of 1-6 lpm; Request advanced life support services; Obtain baseline vital signs and obtain the SAMPLE history. "SAMPLE history" means the present and past medical history of a patient, so called because the elements of the history begin with the letters of the word sample: Signs/Symptoms, Allergies, Medications, Pertinent past history, Last oral intake, and Events leading to the injury or illness; Conduct the focused assessment and physical exam. Apply high-concentration oxygen. Assessing Allergic Reactions Request ALS Take baseline vital signs. Obtain SAMPLE history. Assessing Allergic Reactions Any history of allergies? What was patient exposed to? How was the patient exposed? What signs and symptoms does the patient have? Assessing Allergic Reactions Any progression of the signs and symptoms? Have any interventions been performed on the patient? Administration Protocol Initiate treatment with the appropriate epinephrine auto injector if a patient prsents with clinical evidence of allergic reaction/anaphylaxis that may include the following symptoms: • A chief complaint of respiratory distress. • Respiratory arrest; • Signs and symptoms of shock (hypoperfusion) with an increased heart rate. Look for the following indications: Heart rate of greater than 180 bpm for an infant (0-12 months) and/or blood pressure less than 60 mmHg for an infant (0-12 months); Heart rate of greater than 140 bpm for a child (1-12 years) and/or blood pressure less than 70 mmHg for a child (1-12 years); Heart rate of greater than 120 bpm for an adult (older than 12 years) and/or blood pressure less than 80 mmHg for an adult (older than 12 years); Administration Protocol • A tightening feeling in the chest and/or throat; • Wheezing or stridor; • Altered appearance with restlessness and/or agitation, seizure, unconsciousness; • Swelling of the face/tongue/lips or generalized urticaria; Administration Protocol If the patient possesses his/her own prescribed Epinephrine auto injector, use theirs if readily available. If the patient does not possess his/her own prescribed Epinephrine auto injector, use the appropriate Epinephrine auto injector from your vehicle's stock. • For patients under 4 years of age, use the pediatric epinephrine auto injector (0.15 mg). • For patients 4 years of age or older, use the adult epinephrine auto injector (0.3 mg). Estimating Patient Age & Weight Pedi-Wheel Broselow Tape • A tool for determining the correct dosage of medications and equipment sizes for children, based on their length. Broselow Tape Broselow Tape Broselow Tape Broselow Tape Broselow Tape Administration Protocol Administer the appropriate Epinephrine auto injector as follows: • Check the color of the medication (if able to view) and the manufacturer's expiration date. If the medication is discolored (yellowed) or beyond the expiration date, do not use; • Carefully remove the safety cap from the auto injector; Remove safety cap. Administration Protocol • Place the auto injector firmly against the lateral portion of the patient's thigh, midway between the waist and the knee. Firm pressure will activate the spring loaded mechanism in the auto injector and force the needle through the patient's clothing and into the thigh muscles; Administration Protocol • Hold the auto injector in place for at least 10 seconds to ensure that the medication is injected; • Dispose of the auto injector in a biohazard sharps container or the product container on a temporary basis; • Record the location of the injection site, time, dose, medication name, vital signs and any changes in the patient's condition after administration of medication on a patient care report. Hold firmly in place for ten seconds, then remove. Massage the area of injection AI 17© Administration Protocol Continuously monitor the patient (level of consciousness, level of distress, respiratory rate and quality, pulse rate and quality, blood pressure, temperature, etc.). Maintain normal body temperature. Notify the receiving hospital if ALS is not available. Treating Allergic Reactions If patient’s condition IMPROVES: Continue oxygen Treat for shock (preventative) Treating Allergic Reactions If patient’s condition WORSENS: Treat for shock Be prepared to use CPR/AED. Treating Allergic Reactions No Second Stick!!! Per NJ OEMS Policy Treating Allergic Reactions Exception – If patient gives Epi-Pen to themselves prior to squad arrival, or you assist with their epi pen… And there is no change in symptoms … Wait 10 MINTUES! (before giving EMS dose) Administration Protocol Carefully monitor patient for respiratory and/or circulatory failure. If condition deteriorates, patient may experience cardiac arrest. • Respiratory failure Provide ventilation at a rate of • Adult 10 to 12 breaths per min. • Child/Infant 12 t0 20 breaths per min. • Cardiac Arrest If witnessed immediate AED if available If unwitnessed or asphyxial 2 min. CPR then AED Compression Ratio • 30:2 Adults and 1 rescuer child/infant • 15:2 two rescuer child/infant Treating Allergic Reactions The patient’s condition may be stable initially but deteriorate to the point where he/she needs aggressive airway management. Call ALS/Do not delay tranport! Best you can do: oral/nasal airways Administration Protocol Leave a copy of the patient care report at the receiving hospital. Deliver a copy of the patient care report to the physician medical director. The medical director shall review all instances of the use of epinephrine auto injectors for quality assurance. Provide agency specific notifications to ensure appropriate reporting to OEMS. • 72 hours verbal, 45 days written • Have ED diagnosis and disposition when possible Treating Allergic Reactions Recurrent Anaphylaxis • Reappearance of allergic symptoms following complete resolution of original reaction, and WITHOUT re-exposure to the offending allergen • May involve mild or severe symptoms, may be = or more severe than initial reaction in severity Treating Allergic Reactions Recurrent Anaphylaxis cont. • Can occur in up to 20% of cases, up to 72 initial event. • Large antigen load • Repeat internal exposure (i.e. insect venom) hours after Treating Allergic Reactions Accidental Auto-Injection of Epi-Pen • Most often occurs to a finger • Potentially can cause local tissue death • Often can be treated with application of heat, local massage, topical nitrates. • Requires IMMEDIATE ED visit! Storage Must be kept btwn 59-74 degrees F Thermos Bottle to insulate Medical grade IV fluid warmers or incubators Commercial 12-volt heater/cooler containers Don’t mix food and stored meds!