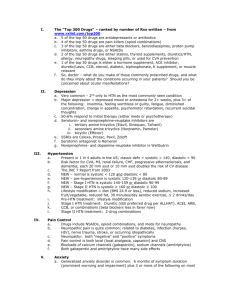
hypertension - University of Washington
advertisement
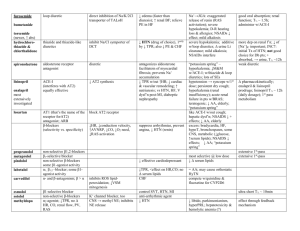
HYPERTENSION Detection, Evaluation and Non-pharmacologic Intervention Misbah Keen, MD, FAAFP Act. Asst. Professor Family Medicine University of Washington School of Medicine Seattle WA Problem Magnitude Hypertension( HTN) is the most common primary diagnosis in America. 35 million office visits are as the primary diagnosis of HTN. 50 million or more Americans have high BP. Worldwide prevalence estimates for HTN may be as much as 1 billion. 7.1 million deaths per year may be attributable to hypertension. Definition A systolic blood pressure ( SBP) >139 mmHg and/or A diastolic (DBP) >89 mmHg. Based on the average of two or more properly measured, seated BP readings. On each of two or more office visits. Accurate Blood Pressure Measurement The equipment should be regularly inspected and validated. The operator should be trained and regularly retrained. The patient must be properly prepared and positioned and seated quietly for at least 5 minutes in a chair. The auscultatory method should be used. Caffeine, exercise, and smoking should be avoided for at least 30 minutes before BP measurement. An appropriately sized cuff should be used. BP Measurement At least two measurements should be made and the average recorded. Clinicians should provide to patients their specific BP numbers and the BP goal of their treatment. Follow-up based on initial BP measurements for adults* www.nhlbi.nih.gov *Without acute end-organ damage Classification www.nhlbi.nih.gov Prehypertension SBP >120 mmHg and <139mmHg and/or DBP >80 mmHg and <89 mmHg. Prehypertension is not a disease category rather a designation for individuals at high risk of developing HTN. Pre-HTN Individuals who are prehypertensive are not candidates for drug therapy but Should be firmly and unambiguously advised to practice lifestyle modification Those with pre-HTN, who also have diabetes or kidney disease, drug therapy is indicated if a trial of lifestyle modification fails to reduce their BP to 130/80 mmHg or less. Isolated Systolic Hypertension Not distinguished as a separate entity as far as management is concerned. SBP should be primarily considered during treatment and not just diastolic BP. Systolic BP is more important cardiovascular risk factor after age 50. Diastolic BP is more important before age 50. Frequency Distribution of Untreated HTN by Age Isolated Systolic HTN Systolic Diastolic HTN Isolated Diastolic HTN Hypertensive Crises Hypertensive Urgencies: No progressive target-organ dysfunction. (Accelerated Hypertension) Hypertensive Emergencies: Progressive end-organ dysfunction. (Malignant Hypertension) Hypertensive Urgencies Severe elevated BP in the upper range of stage II hypertension. Without progressive end-organ dysfunction. Examples: Highly elevated BP without severe headache, shortness of breath or chest pain. Usually due to under-controlled HTN. Hypertensive Emergencies Severely elevated BP (>180/120mmHg). With progressive target organ dysfunction. Require emergent lowering of BP. Examples: Severely elevated BP with: Hypertensive encephalopathy Acute left ventricular failure with pulmonary edema Acute MI or unstable angina pectoris Dissecting aortic aneurysm Types of Hypertension Primary HTN: also known as essential HTN. accounts for 95% cases of HTN. no universally established cause known. Secondary HTN: less common cause of HTN ( 5%). secondary to other potentially rectifiable causes. Causes of Secondary HTN Common Intrinsic renal disease Renovascular disease Mineralocorticoid excess Sleep Breathing disorder Uncommon Pheochromocytoma Glucocorticoid excess Coarctation of Aorta Hyper/hypothyroidism Secondary HTN-Clues in Medical History Onset: at age < 30 yrs ( Fibromuscular dysplasi) or > 55 (athelosclerotic renal artery stenosis), sudden onset (thrombus or cholesterol embolism). Severity: Grade II, unresponsive to treatment. Episodic, headache and chest pain/palpitation (pheochromocytoma, thyroid dysfunction). Morbid obesity with history of snoring and daytime sleepiness (sleep disorders) Secondary HTN-clues on Exam Pallor, edema, other signs of renal disease. Abdominal bruit especially with a diastolic component (renovascular) Truncal obesity, purple striae, buffalo hump (hypercortisolism) Secondary HTN-Clues on Routine Labs Increased creatinine, abnormal urinalysis ( renovascular and renal parenchymal disease) Unexplained hypokalemia (hyperaldosteronism) Impaired blood glucose ( hypercortisolism) Impaired TFT (Hypo-/hyper- thyroidism) Secondary HTN-Screening Tests www.nhlbi.nih.gov Renal Parenchymal Disease Common cause of secondary HTN (2-5%) HTN is both cause and consequence of renal disease Multifactorial cause for HTN including disturbances in Na/water balance, vasodepressors/ prostaglandins imbalance Renal disease from multiple etiologies. Renovascular HTN Atherosclerosis 75-90% ( more common in older patients) Fibromuscular dysplasia 10-25% (more common in young patients, especially females) Other • • • • • • Aortic/renal dissection Takayasu’s arteritis Thrombotic/cholesterol emboli CVD Post transplantation stenosis Post radiation Complications of Prolonged Uncontrolled HTN Changes in the vessel wall leading to vessel trauma and arteriosclerosis throughout the vasculature Complications arise due to the “target organ” dysfunction and ultimately failure. Damage to the blood vessels can be seen on fundoscopy. Target Organs CVS (Heart and Blood Vessels) The kidneys Nervous system The Eyes Effects On CVS Ventricular hypertrophy, dysfunction and failure. Arrhithymias Coronary artery disease, Acute MI Arterial aneurysm, dissection, and rupture. Effects on The Kidneys Glomerular sclerosis leading to impaired kidney function and finally end stage kidney disease. Ischemic kidney disease especially when renal artery stenosis is the cause of HTN Nervous System Stroke, intracerebral and subaracnoid hemorrhage. Cerebral atrophy and dementia The Eyes Retinopathy, retinal hemorrhages and impaired vision. Vitreous hemorrhage, retinal detachment Neuropathy of the nerves leading to extraoccular muscle paralysis and dysfunction Retina Normal and Hypertensive Retinopathy A B C Normal Retina Hypertensive Retinopathy A: Hemorrhages B: Exudates (Fatty Deposits) C: Cotton Wool Spots (Micro Strokes) Stage I- Arteriolar Narrowing Arteriolar Narrowing Stage II- AV Nicking AV AVNicking Nicking AV Nicking AV Nicking Stage III- Hemorrhages (H), Cotton Wool Spots and Exudats (E) H E Stage IV- Stage III+Papilledema Patient Evaluation Objectives (1) To assess lifestyle and identify other cardiovascular risk factors or concomitant disorders that may affect prognosis and guide treatment (2) To reveal identifiable causes of high BP (3) To assess the presence or absence of target organ damage and CVD (1) Cardiovascular Risk factors Hypertension Cigarette smoking Obesity (body mass index ≥30 kg/m2) Physical inactivity Dyslipidemia Diabetes mellitus Microalbuminuria or estimated GFR <60 mL/min Age (older than 55 for men, 65 for women) Family history of premature cardiovascular disease (men under age 55 or women under age 65) (2) Identifiable Causes of HTN Sleep apnea Drug-induced or related causes Chronic kidney disease Primary aldosteronism Renovascular disease Chronic steroid therapy and Cushing’s syndrome Pheochromocytoma Coarctation of the aorta Thyroid or parathyroid disease (3) Target Organ Damage Heart Left ventricular hypertrophy Angina or prior myocardial infarction Prior coronary revascularization Heart failure Brain Stroke or transient ischemic attack Chronic kidney disease Peripheral arterial disease Retinopathy History Angina/MI Stroke: Complications of HTN, Angina may improve with b-blokers Asthma, COPD: Preclude the use of b-blockers Heart failure: ACE inhibitors indication DM: ACE preferred Polyuria and nocturia: Suggest renal impairment History-contd. Claudication: May be aggravated by bblockers, atheromatous RAS may be present Gout: May be aggravated by diuretics Use of NSAIDs: May cause or aggravate HTN Family history of HTN: Important risk factor Family history of premature death: May have been due to HTN History-contd. Family history of DM : Patient may also be Diabetic Cigarette smoker: Aggravate HTN, independently a risk factor for CAD and stroke High alcohol: A cause of HTN High salt intake: Advice low salt intake Examination Appropriate measurement of BP in both arms Optic fundi Calculation of BMI ( waist circumference also may be useful) Auscultation for carotid, abdominal, and femoral bruits Palpation of the thyroid gland. Examination-contd. Thorough examination of the heart and lungs Abdomen for enlarged kidneys, masses, and abnormal aortic pulsation Lower extremities for edema and pulses Neurological assessment Routine Labs EKG. Urinalysis. Blood glucose and hematocrit; serum potassium, creatinine ( or estimated GFR), and calcium. HDL cholesterol, LDL cholesterol, and triglycerides. Optional tests urinary albumin excretion. albumin/creatinine ratio. Goals of Treatment Treating SBP and DBP to targets that are <140/90 mmHg Patients with diabetes or renal disease, the BP goal is <130/80 mmHg The primary focus should be on attaining the SBP goal. To reduce cardiovascular and renal morbidity and mortality Benefits of Treatment Reductions in stroke incidence, averaging 35–40 percent Reductions in MI, averaging 20–25 percent Reductions in HF, averaging >50 percent. Lifestyle modifications www.nhlbi.nih.gov Lifestyle Changes Beneficial in Reducing Weight Decrease time in sedentary behaviors such as watching television, playing video games, or spending time online. Increase physical activity such as walking, biking, aerobic dancing, tennis, soccer, basketball, etc. Decrease portion sizes for meals and snacks. Reduce portion sizes or frequency of consumption of calorie containing beverages. DASH Diet Dietary approaches to Stop Hypertension As effective as one medication JNC 7 Summary Joint National Commission 7th Report PDF File on website 50 page document Other JNC 7 Resources Software for use with Palm and Pocket PC JNC 7 Reference Card Other Resources Chronic Kidney Disease Information GFR Calculator www.nephron.com Hyperlipedemia Information Adult Treatment Panel 3 Guidelines www.nhlbi.nih.gov/guidelines/cholesterol/index.htm Questions mkeen@fammed.washington.edu