Controlled Drugs Dayton July 2015
advertisement

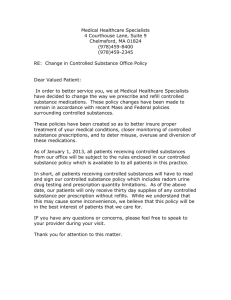
From Dosing to Destruction: Best Practices - Controlled Medications Rob Shulman R.Ph. CGP FASCP Director of Consulting Services Remedi SeniorCare William M. Vaughan, RN Vice President, Education and Clinical Affairs Remedi SeniorCare Disclosure / Contact • Rob Shulman has no relevant disclosures • William Vaughan is a shareholder at Remedi SeniorCare, a consultant to CMS currently working on QAPI and on the advisory board of the Institute for Safe Medication Practices’ long-term care newsletter • Rob.Shulman@Remedirx.com • William.Vaughan@Remedirx.com Objectives • Address best practices related to the prescribing, administration, monitoring, and storage of controlled substances from both a clinical and regulatory perspective. • Provide an overview of the Drug Enforcement Agency's final rule on disposal of controlled substances and its potential implications for long term care communities Diversion Case Studies • • • • Vomiting Phenobarbital The case of the “weak” foil Some drugs will surprise you Its often those who you would least expect Regulatory Pearls – Controlled Drugs Federal Nursing Home Regulations: (what about assisted living facilities?) • Acknowledge diversion policy/procedures • Include pharmacist in development / ongoing review • Consistency: pharmacy/facility • Consistency: log/MAR • “The facility must provide separately locked, permanently affixed compartments for storage of controlled drugs … other drugs subject to abuse …” (F 431) • Permanently affixed intent • Other drugs proactively define • Medical Director, Consultant Pharmacist, NIDA Regulatory Pearls – Controlled Drugs • Drug diversion: Duty to report to survey agency? • Neglect = failure to provide goods and services necessary to avoid physical harm, mental anguish, or mental illness • Misappropriation of Resident Property = The deliberate misplacement, exploitation, or wrongful, temporary or permanent use of a resident’s belongings or money without the resident’s consent. (Ref: CMS S&C-05-09) • Drug diversion: Duty to report to law enforcement? • The Affordable Care Act requires reporting of “any reasonable suspicion of a crime” to local law enforcement: • • Serious bodily injury 2 hours, otherwise within 24 hours Reference: CMS S&C: 11-30-NH Regulatory Pearls – Controlled Drugs “Counting” Liquid Medications • Deficiency Allegation: “… the facility failed to ensure narcotic medications for Resident #25 were properly secured and accounted for …” • Narcotic medication = Morphine Sulfate (100 mg/5ml) Regulatory Pearls – Controlled Drugs • Surveyor observes 30 mls. • Narcotic reconciliation record = 28 mls • DON estimates between 29 and 30 mls “Failure to properly account for narcotic medications” Regulatory Pearls – Controlled Drugs • • • • • • Informal Dispute Resolution Minimal volume administered via dropper (.25ml) Bottle calibrated in 1-5 ml increments Manufacturers routinely overfill by up to 10% (label = 30 mls, actual volume 31-33 mls) Removing morphine each shift creates more risk Staff was estimating the amount … just like the surveyor Intent F 431: “Identification of loss or diversion of controlled medications so as to minimize the time between actual loss or diversion and the detection and determination of the extent of loss or diversion” Controlled Substance Diversion Diversion of drugs: Unlawful channeling of regulated pharmaceuticals, including the misuse of prescription medications • Symptom of the disease of addiction • Addiction is a treatable disease Healthcare Professionals and Drug Abuse: Healthcare Professions with higher rates of drug use: • Nurses • Dentists • Pharmacists • Anesthesiologists • Veterinarians Preferred Medications: • Benzodiazepines • Opiates Healthcare Professionals and Drug Abuse: Types of drugs preferred: • • • • • 60% use an opiate 45% use a benzodiazepine 11% use sedatives 3.5% use amphetamines 1.9% use inhalants Early intervention is vital for both patient care concerns and health care employee professional recovery A visible program is a major deterrent to diversion (Lillibridge, Cox & Cross, 2002) Drug Diversion Issues: Nursing Staff • 10 –20% of nurses have substance abuse issues • ANA estimates approximately 6% to 8% of nurses are practicing while impaired • Substance abuse is the number one reason named by state boards of nursing for disciplinary action • Recidivism rates by nurses from diversion and rehabilitation programs are lower when compared with the general population (Griffith, 1999); (Trinkoff& Storr, 1998) (Sullivan & Decker, 2001). Staff Risk Factors: In the workplace: • Stress • Belief in medications • Caregiver burnout • “Nurses’ knowledge can ward off substance abuse” • Access to controlled substances At high risk : Nurses who administer drugs daily and perceive poor to non-existent workplace controls have 2 x the risk of drug misuse Physical Signs of Use/Withdraw • Physical signs of use or withdrawal: • • • • • • Hand tremors Headache Diaphoresis Abdominal/muscle cramps Nausea/ Diarrhea Irritability or Restlessness • Signs may disappear with use • Non-descript: can also be signs of psychological problems. • Behaviors impair clinical judgment and put residents at risk (Smith et al., 1998). Drug Diversion: Staff Indicators Staff Behavioral Indicators: Isolates self from others, eats meals alone, avoids staff social events Frequent, unexplained disappearances during shift Often shows up on days off to finish work or retrieve forgotten items Frequently volunteers to work extra shifts Volunteer to hold the narcotics keys/ perform count Frequently spills or wastes narcotics Chaotic home/personal life Refuses to comply with narcotic diversion investigational procedures implausible excuses for behavior or become defensive Drug Diversion: Staff Indicators Resident Care Indicators: Inconsistent or incorrect charting Displays inconsistent work quality with times of high and low efficiency Offers to medicate other nurses’ patients on a regular basis Obtains larger dose of narcotics when the ordered dose is available, documents the remaining amount as wasted Requests to care for specific patients His/her patients reveal consistent pain scale patterns or complain that narcotics are not effective only on that shift Prevention and Recognition of Diversion and Drug Use/Abuse Early intervention is vital for both patient care concerns and health care employee professional recovery A visible program is a major deterrent to diversion To prevent drug diversion: • Adequate controls in place- Policies & Procedures • Use proactive approach for early detection and intervention • Discourage diversion through education and awareness • Intervene as appropriate • Rapid closure on diversion cases Preventing Drug Diversion: Best Practices Staff Prevention Strategies: • • • • • • • • • • Only remove medications for your assigned patients Only remove current dose of medication for your patient Properly document medication administration and pain scores All wastes of medications must have a documented witness Don’t be a “virtual witness” to medication wasting Don’t loan your ID badge or pass-codes to anyone Return unused medications according to procedure Report medication discrepancies promptly to pharmacy (on-line reporting available) Report attempted inappropriate access to medications to pharmacy Report witnessed or suspected medication diversion to pharmacy Preventing Drug Diversion: Best Practices Policies, Procedures and Controls • Procurement • Storage and security What areas need the most reinforcement with Administration and Staff? • Prescribing • Preparation/Administration of CDS • Handling wastage • Documentation • Follow-up if diversion is suspected What do you do if diversion is suspected, or if CDS are missing? Policies & Procedures Addressing Drug Disposition Examples of procedures addressing the disposition of medications include: • • • • • • • • Controlled substance receipt/ reconciliation Shift counts/ongoing accountability Timely identification and removal of medications Identification of storage method for medications awaiting final disposition Control and accountability of medications awaiting final disposition Documentation of actual disposition of medications Method of destruction consistent with applicable state and federal requirements Procedures for discrepancies, theft or loss Drug Diversion Investigation Rapid internal investigation and closure of diversion incidents Reasons to contact pharmacy: • Unresolved discrepancies • Questionable resolutions • Tampered syringes or vials • Misplaced narcotics • Missing narcotics • Records of dispensing, refills Investigation Checklist Controlled Substance Drug Disposal In Ohio… For every unintentional opiod overdose death in 2010, there were 733 non-medical users. ER visits from pharmaceutical abuse with no other type of drug or alcohol involvement doubled between 2004-2010. 70% of younger people using Rx drugs get them from family or friends. One in four teens admit to having used Rx drugs More Americans abuse Rx drugs than the number of cocaine, hallucinogen methamphetamine and heroin users combined OhioPMP.gov Cocktail Hour… Opiate + Benzo + Muscle relaxant “Trinity” = hydrocodone + alprazolam + carisoprodol “Holy Trinity” = oxycodone + alprazolam + carisoprodol Hydrocodone, prior to becoming a C-II was #1 drug of abuse in Ohio OhioPMP.gov OARRS Ohio Automated Rx Reporting System All controlled dispensing data on one website Researched by patient name Detects multiple prescribers Checked by Prescribers prior to writing for CDS Checked by Pharmacies prior to filling Rx for a CDS (OAC 4729-5-20) – prospective DUR Ohio Board of Pharmacy “Deter & Detect” Drug destruction at the facility : • Witnessed by the DON or Administrator and a Pharmacist Complete and accurate record of the drugs destroyed shall be made: • Record of destruction shall be signed and dated by the persons witnessing the destruction • Maintained at LTCF for a period of two years. • Copy goes to Board of Pharmacy White House Office of National Drug Control Policy (ONDCP) Federal Guidelines for the Proper Disposal of Prescription Drugs Take your prescription drugs out of their original containers: • Mix drugs with an undesirable substance, such as cat litter or used coffee grounds • Put this mixture into a disposable container with a lid or into a sealable bag. • Place the sealed container with the mixture, and the empty drug containers, in the trash. Food and Drug Administration DEA- Disposal of Controlled Substances Safe and Secure Drug Disposal Act of 2010 allows DEA to develop regulations to allow non-DEA registrants to dispose of unused controlled medications. • Mail-back programs • Take-back events • Secured on-site receptacles . Centers for Medicare and Medicaid Services Centers for Medicare and Medicaid Services F-Tag 425 Policies and procedures for disposal of medications. • Timely identification and removal of medications for disposition • Identification of storage method for medications awaiting final disposition • Control and accountability of medications awaiting final disposition consistent with standards of practice • Documentation of actual disposition of medications • Method of disposition consistent with applicable state and federal requirements and standards of practice Destruction of Fentanyl Patches: Additional Guidance CMS: “The remaining fentanyl in a used patch is a potential vehicle of abuse and warrants implementation of adequate disposal policies” • Staff should dispose of fentanyl patches in the same manner as wasting of any other controlled substances, particularly because the active ingredient is still accessible. • Wasting must involve a secure and safe method, so diversion and/or accidental exposure are minimized. Occupational Safety and Health Administration (OSHA) In verbal discussions with OSHA, ASCP was told that OSHA has no guidance about medication disposal other than to say medications (in particular Fentanyl patches) should not be put into sharps containers. Cactus “Smart Sink” 2014 Drug Diversion: DEA Final Rule Disposal of Controlled Substances The Disposal Act amendment to the Controlled Substances Act • 9/9/14 - Expands the entities to which ultimate users may transfer unused/unwanted/expired pharmaceutical CDS for disposal. • Expands the methods by which CDS may be collected. • Encourage public and private entities to develop a variety of methods of collection • Voluntary * 21 CFR Parts 1300, 1301, 1304, 1305, 1307, and 1317 DEA Final Rule : Disposal Options Who can collect: Manufacturers, distributors, reverse distributors, narcotic treatment, hospital pharmacies, retail pharmacies How: • Mail-back Programs • Take-Back Events • Collection Receptacles: - At DEA registrant’s location - Hospitals/ clinics and retail pharmacies may also maintain collection receptacles at longterm care facilities. Drug Destruction: “Ultimate User” “Ultimate User” : “A person who has lawfully obtained, and who possesses, a CDS for his own use /for the use of a member of his household “ Voluntary options for “ultimate user” disposal: (1) Take-back events (2) Mail-back programs (3) Collection receptacles Exceptions: “Ultimate User” Destruction Exceptions: (1) Individuals lawfully entitled to dispose of an ultimate user decedent’s property are authorized to dispose of the ultimate user’s pharmaceutical controlled substances by utilizing any of the three disposal options. (2) LTCFs may dispose of pharmaceutical controlled substances on behalf of an ultimate user who resides, or has resided, at that LTCF. Operational Challenges- Structure A collection receptacle shall be located in a secured area regularly monitored by LTCF employees. • Securely fastened to a permanent structure • Securely locked, substantially constructed container with a permanent outer container and a removable inner liner • Outer container shall include a small opening that allows contents to be added to the inner liner, but does not allow removal of the inner liner's contents. • Small opening in the outer container shall be locked when the collection receptacle is not being regularly monitored by long-term care facility employees. Operational Challenges- Coordination • When disposing into a collection receptacle, disposal shall occur no longer than three business days after the discontinuation of use by the ultimate user. • Supervisor-level employee of the LTCF (e.g. a charge nurse, supervisor, or similar employee) to install, remove, store, or transfer inner liners with one employee of the collector. • Filled liners may be stored in a securely locked for up to three business days until the liners can be transferred for destruction. • Collectors may not transfer sealed inner liners from LTCFs to their primary registered location (i.e., the pharmacy location). Facility Implications • Take-back programs: • • Touchstone for this disposal method is the individual nature of the disposal activity Institutional facilities such as LTCFs should ensure that the individual patient is the disposer • Release of controlled substances to individuals lawfully entitled to dispose of an ultimate user decedent’s property • Placement of disposal receptacles within a long-term care facility renders the facility a "controlled premises" under the Controlled Substances Act • Cost! Operationalizing Diversion Prevention Ensure your facility has adequate policies, procedures and that they are held accountable for following these guidelines. Audits and observations will ensure ongoing compliance to procedures • MedPass Observations • MedCart Audits • Documentation Audits Controlled Substances: Storage and Access • Drugs listed in Schedules II-V are not to be accessible to other than: • • • • • Licensed nursing personnel Pharmacy personnel Medical personnel Those designated by the facility /as allowed by regulations Note: Medication Aides may have access/administer controlled substances per facility policy if state regulations allow. • All Schedule II controlled substances are to be stored under double lock, separate from other medications. • Depending on state regulations, ALL controlled substances may require a double lock and shift count- Check your state regulations regarding the storage for CIII- V medications. Controlled Substances: Accounting Procedures Declining Inventory sheets must be signed by the accepting nurse upon receipt of the med in the facility Verifying the quantity received matches the quantity sent. Schedule II medications must be counted by an oncoming nurse and an offgoing nurse at the change of each shift Documented on the Shift Count Form for Controlled Substances. Count all medications storage areas, including the refrigerator. Controlled substances other than Schedule II’s may be added to the accounting procedures. The pharmacy can provide the individualized records for Schedule III-V’s upon request if not already provided. Controlled Substances: CII Record Procedures Separate records (individual controlled substance record) need to be maintained on all Schedule II drugs in the form of a declining inventory Pharmacy will provide these individual records for each Schedule II prescription sent. Each record must be accurately maintained and shall include: Name of the resident Name of the prescriber Prescription number Drug name Form of the medication (tablet, capsule, liquid, suppository, etc.) Strength and dose administered Date and time of administration Signature of the person administering the drug Remaining number of doses Controlled Substances: Emergency Supply Staff should only sign-out and remove one (1) dose at a time, at the time you are actually administering the drug. If two (2) doses are due on your shift, you still must sign and remove each dose at designated time of administration. Ensure the MAR and Declining Inventory Sheet match Controlled Substances: Incorrect Count Incorrect Count- What to do? Determine whether the medication was given and not charted. Determine if the medication may have been ‘lost’ or discarded. Document on the individual count form that “count is incorrect” Sign the shift count record in the usual manner, indicating that the count was not correct The nurse on the shift on which the count was identified as being incorrect must fill out an Incident Report indicating the action that was taken to locate the medication Forward the report to the Nursing Office; the DON /Administrator need to be notified (or follow facility policy) Thank You References Narcotic Use and Diversion in Nursing Mandy L. Hrobak, University of Arizona College of Nursing http://juns.nursing.arizona.edu/articles/Fall%202002/hrobak.htm. 1. 2. Nurse Drug Diversion and Nursing Leader's Responsibilities: Legal, Regulatory, Ethical, Humanistic, and Practical Considerations. Tanga, H. JONA's Healthcare Law, Ethics, and Regulation Jan 2011 Vol 13(1) pg 13 –16. http://www.nursingcenter.com/lnc/static?pageid=1193263 . 3. Impaired healthcare professional Marie R. Baldisseri, MD, FCCM. Crit Care Med 2007 Vol. 35, No. 2 (Suppl.) http://www.csamasam.org/sites/default/files/pdf/misc/16_article_Baldisseri_Impaired_healthcare_prof_2007.pdf. 4. A Multidisciplinary Approach to Proactive Drug Diversion Prevention. Jerry Siegel Pharm.D. FASHP The Ohio State University Medical Center Columbus, Ohio, 2009. 5. Disposal of Controlled Substances. Federal Register / Vol. 79, No. 174 / Tuesday, September 9, 2014 / Rules and Regulations