Preoperative Evaluation And Management
advertisement

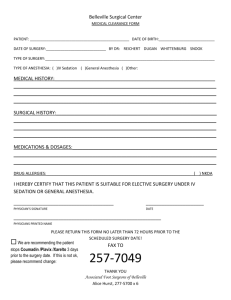
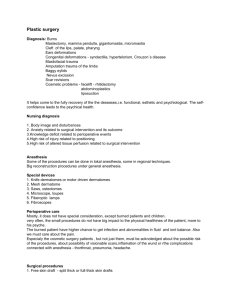
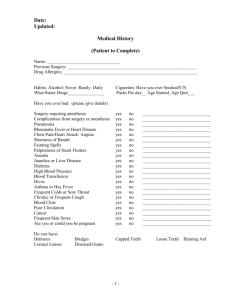
PREOPERATIVE ASSESSMENT Hossam M. Ajabnoor Anesthesia & ICU Asistant Consultant And Lecturer School of Medicine, Taibah University INTRODUCTION Importance 1. Reduce patient risk and morbidity associated with surgery and coexisting diseases 2. Promote efficiency and reduce costs 3. Prepare the patient medically and psychologically for surgery and anesthesia ASA basic standards for preanesthetic care 1. Determining the pt. medical status 2. Developing an anesthetic care plan 3. Reviewing with the pt. or a responsible adult this plan Who should perform the preoperative evaluation? Ideally, the preoperative evaluation is performed by the person who will administer the anesthetic. Goals: 1. Inform the pt. of the risk → informed consent 2. Educate the pt. regarding anesthesia Plan 3. Answer pt. Q.s & reassure the pt. & family 4. Prohibition of ingesting food 5. Instruct the pt. about which medications to take or to stop on the day of surgery PREOPERATIVE EVALUATION • It is important for the evaluation to be complete, accurate, and clear, not only to allow the information to be relayed to others who may care for the patient perioperatively, but also for medico legal purposes COMPONANTS • • • • • • HISTORY PHYSICAL EXAMINATION LAB TESTS CONSULTATIONS (if needed) PLAN DISCUSSION WITH PATIENT HISTORY 1. State of health of pt. especially their • exercise tolerance • Present illness 2. Mental status 3. Medication and substances use(e.g., cigarettes, alcohol) 4. Previous anesthesia and any complications 5. Drug allergies and family Hx of MH 6. review of medical records SPECIFIC AREAS IN Hx CNS Strokes - seizures CVS Angina - old MI – HTN – rheumatic fever – claudication – arrhythmias PULMONARY SOB – cough/sputum – asthma – smoking – recent UTI – pneumonia GI GERD – alcohol – hepatitis KIDNEYS Dialysis – ch. Renal impairment MUSCULOSKELETAL Arthritis – osteoporosis – weakness ENDOCRINE DM – thyroid/adrenal dysfunction COAGULATION History of DVT/PE – bleeding tendency PREGNANCY? DENTITION PHYSICAL EXAMINATION 1. 2. 3. 4. Vital signs CNS (LOC – evidence of S/M weakness) Airway CVS (heart sounds – BP – peripheral edema peripheral pulses – veins) 5. Lungs (rales – wheezes – breathing pattern) AIRWAY • • • • • • • • Cervical spine mobility Short thick neck Temporomandibular mobility Large tongue Prominent central incisors Diseased or artificial teeth Thyromental distance and tissue compliance Ability to visualize the uvula (Mallampati classification) Mallampati classification Mallampati found a correlation between higher oropharyngeal class and decreased glottic exposure at laryngoscopy. A higher oropharyngeal class combined with a mental space < 2 fingerbreadths may better predict increased difficulty with intubation Performed by having patients in sitting position with their mouth widely open and protruding the tongue completely forward. (A tongue depressor is not used) DIRECT VISUALIZATION, PATIENT SEATED class I → soft palate, fauces, uvula, and pillars class II → soft palate, fauces, and a portion of the uvula class III → soft palate and base of the uvula class IV → hard palate only LARYNGOSCOPIC VIEW Entire glottic Posterior commissure Tip of epiglottis No glottal structures LAB TESTS • No evidence supports the use of routine laboratory testing • Use selected laboratory analysis based on the patient's preoperative history, physical examination, and proposed surgical procedure Test Indications Electrocardiogram Cardiac and circulatory disease, respiratory disease, advanced age† Chest radiograph Chronic lung disease, history of congestive heart disease Pulmonary function tests, including blood gas analysis and spirometry Reactive airway disease, chronic lung disease, restrictive lung disease (e.g., scoliosis) Hemoglobin/hematocrit Advanced age,† anemia, bleeding disorders, other hematologic disorders Coagulation studies Bleeding disorders, liver dysfunction, anticoagulants Serum chemistries (Na+, K+, Cl-, CO2, glucose) Endocrine disorders, medications, renal dysfunction Pregnancy test Uncertain pregnancy history, history suggestive of current pregnancy CONSULTATIONS Preoperative consultations fall into two general categories: • Those cases that need more information or expertise to establish or quantify a diagnosis that has implications for anesthetic management. An example is asking a cardiologist to evaluate a 50-year-old man with recent onset of exertional chest pain. • Patients in whom the diagnosis is known, but further evaluation and treatment are needed to optimize their medical condition prior to surgery. Referring patients with poorly controlled diabetes, hypertension, or asthma to an internist are examples. PLAN Type of anesthesia • Awake • Sedation • Local • Regional • General anesthesia Transfer postop • Home • Hospital room (day care / ward) • ICU Pain control postop Discussion With The Pt. Preop 1. Risks related to anesthesia • Nausea and vomiting • Myalgia • Dental injury • Peripheral neuropathy • Cardiac dysrhythmias • Atelectesis • Aspiration • Stroke • Allergic drug reactions • Death (very unlikely) 2. Preop insomnia and its treatment 3. Time, route of administration & effects of preop meds 4. Time of transport to OR 5. Duration of surgery 6. Awakening after surgery in PACU 7. Probable presence of catheters on awakening 8. Time to expected discharge from PACU 9. Magnitude of postop discomfort and it treatment ASA PHYSICAL STATUS CLSSIFICATION Created in 1940 purposes of statistical studies and hospital records It is useful both for outcome comparisons and as a convenient means of communicating the physical status of a patient Unfortunately, it is imprecise, and a patient often may be placed in different classes by different anesthesiologists the higher ASA class only roughly predicts anesthetic risk • Class 1: Healthy patient, no medical problems • Class 2: Mild systemic disease • Class 3: Severe systemic disease, but not incapacitating • Class 4: Severe systemic disease that is a constant threat to life • Class 5: Moribund, not expected to live 24 hours irrespective of operation • An e is added to the status number to designate an emergency operation. An organ donor is usually designated as Class 6. How long should a patient fast before surgery? • Healthy adults with no risk factors for aspiration include no solid food for a minimum of 6 hours, clear liquids up to 2 hours prior to an elective procedure, and oral preoperative medications up to 1-2 hours before anesthesia with sips of water. • Pediatric patients are as follows: clear liquids up to 2 hours preoperatively breast milk up to 4 hours preoperatively solid foods, including nonhuman milk and formula, up to 6 hours preoperatively. How long before surgery must A smoker patient quit smoking? • Carbon monoxide (CO) from cigarette smoking diminishes oxygen delivery to tissues • Nicotine increases heart rate and can cause peripheral vasoconstriction • Within 12-24 hours of discontinuing cigarettes, CO and nicotine levels return to normal • Bronchociliary function improves within 2-3 days of cessation • sputum volume decreases to normal levels within about 2 weeks • However, there may not be a significant decrease in postoperative respiratory morbidity until after 6-8 weeks of abstinence. List the major goals of premedication • • • • Sedation and anxiolysis Analgesia and amnesia Antisialagogue effect To maintain hemodynamic stability, including decrease in autonomic response • To prevent and/or minimize the impact of aspiration • To decrease postoperative nausea and vomiting • Prophylaxis against allergic reaction What factors should be considered in selecting premedication for a patient? • • • • • Patient age and weight Physical status Levels of anxiety and pain Previous history of drug use or abuse History of postoperative nausea or vomiting or motion sickness • Drug allergies • Elective or emergency surgery • Inpatient or outpatient status List the most commonly used preop medications • • • • • • • • • • Diazepam Oral 5-20 Sedation Midazolam IV 2.5-5 Sedation Morphine IM 5-15 Analgesia Meperidine IM 50-150 Analgesia Ranitidine Oral, IV 150 mg and 50 mg, respectively Decrease gastric pH Metoclopramide Oral, IM, IV 5-20 Gastrokinetic Glycopyrrolate IM, IV 0.1-0.3 Weak sedative, antisialagogue Scopolamine IM, IV 0.3-0.6 Sedative, antisialagogue Promethazine IM 25-50 Antiemetic Ketamine IM, oral 1-2 mg/kg and 6 mg/kg, respectively Sedation A 3-year-old child presents for an elective tonsillectomy. His mother reports that for the past 3 days he has had a runny nose. Should you postpone surgery? • Viral URI alters the quality and quantity of airway secretions and increases airway reflexes to mechanical, chemical, or irritant stimulation • Some clinical studies have shown associated intraoperative and postoperative bronchospasm, laryngospasm, and hypoxia • There is evidence that the risk of pulmonary complications may remain high for at least 2 weeks, and possibly 6-7 weeks, after a URI • Infants have a greater risk than older children, and intubation probably confers additional risk • However, as a practical matter, young children can average 5-8 URIs per year, mostly from fall through spring • If a 4- to 7-week symptom-free interval were rigorously followed, an elective surgery might be postponed indefinitely • Therefore, most anesthesiologists distinguish uncomplicated URI with chronic nasal discharge from nasal discharge associated with more severe URI with or without lower respiratory tract infection (LRI) • Chronic nasal discharge is usually noninfectious in origin and caused by allergy or vasomotor rhinitis • An uncomplicated URI is characterized by sore or scratchy throat, laryngitis, sneezing, rhinorrhea, congestion, malaise, nonproductive cough, and temperature > 38°C • More severe URI or LRI may include severe nasopharyngitis, purulent sputum, high fever, deep cough, and associated auscultatory findings of wheezes or rales • It is generally agreed that chronic nasal discharge poses no significant anesthesia risk • In contrast, children with severe URI or LRI almost always have their elective surgery postponed • Probably most anesthesiologists will proceed to surgery with a child with a resolving uncomplicated URI, unless the child has a history of asthma or other significant pulmonary disease THANK YOU